Abstract
Increasing evidence has shown that insulin resistance in omental visceral adipose tissue (OVAT) is a characteristic of gestational diabetes mellitus (GDM). The present study aimed to identify differentially expressed genes (DEGs) and their associated functions and pathways involved in the pathogenesis of GDM by comparing the expression profiles of OVATs obtained from pregnant Chinese women with and without GDM during caesarian section. A total of 935 DEGs were identified, including 450 downregulated and 485 upregulated genes. In the gene ontology category cellular components, the DEGs were predominantly associated with functions of the extracellular region, while receptor binding was predominant in the molecular function category and biological process terms included antigen processing and presentation, extracellular matrix organization, positive regulation of cell-substrate adhesion, response to nutrients and response to dietary excess. Functional enrichment and Kyoto Encyclopedia of Genes and Genomes (KEGG) pathway enrichment were performed and a functional interaction network was constructed. Functions of downregulated genes included antigen processing and presentation as well as cell adhesion molecules, while those of upregulated genes included transforming growth factor (TGF)-β-signaling, focal adhesion, phosphoinositide-3 kinase-Akt-signaling, P53 signaling, extracellular matrix-receptor interaction and regulation of actin cytoskeleton pathway. The five main pathways associated with GDM were antigen processing and presentation, cell adhesion molecules, Type 1 diabetes mellitus, natural killer cell-mediated cytotoxicity and TGF-β signaling. These pathways were included in the KEGG pathway categories of ‘signaling molecules and interaction’, ‘immune system’ and ‘inflammatory response’, suggesting that these processes are involved in GDM. The results of the present study enhanced the present understanding of the mechanisms associated with insulin resistance in OVATs of GDM.
Keywords: expression profile, differentially expressed gene, interaction network, functional enrichment analysis, insulin resistance, gestational diabetes mellitus
Introduction
Insulin resistance is a condition of the body not appropriately responding to circulating insulin; furthermore, insulin resistance in adipose tissue is an important characteristic of gestational diabetes mellitus (GDM) (1). To compensate for the insulin resistance in the adipose tissue, pancreatic β-cells initially produce more insulin; however, beyond a certain limit, β-cell failure and DM occur (2). At the cellular level, the insulin signaling cascade has an important metabolic role, while its disruption may induce insulin resistance and is closely associated with GDM (3). However, to date, the causes of insulin resistance in adipose tissue at the cellular and molecular level have remained elusive. As aberration of gene expression and molecular pathways may be involved in GDM, the present study determined and analyzed the gene expression profiles of adipose tissues from pregnant women with and without GDM. To the best of our knowledge, the present study was the first to show a distinct pattern of differentially expressed genes (DEGs) in omental visceral adipose tissue (OVAT) from Chinese GDM patients by using a whole genome microarray.
While adipose tissue has been regarded as a storage organ, it is likely to have further functions, as it has been convincingly shown to secrete a number of cytokines, which have a fundamental role in causing insulin resistance in GDM (4,5). Adipose tissues in different sites of the body have distinct biochemical properties (6). It has been reported that the accumulation of OVAT is mainly correlated with an increased risk of altered glucose homeostasis and insulin resistance (7).
Microarrays represent a powerful tool for studying the mechanisms of complex diseases and enable for comprehensive analysis of the interaction between multiple genes simultaneously implicated in pathological processes (8–10).
In the present study, the gene expression profiles of OVATs from pregnant women with or without GDM were compared with the aim of identifying DEGs. Functional enrichment analysis was performed to determine the gene ontology (GO) functions and the key signaling pathways in the pathogenetic processes of GDM. Several molecular mechanisms and pathways that may be responsible for the insulin resistance and progression of GDM were identified.
Materials and methods
Patients and tissues
OVATs were obtained from six patients during C-section at the Department of Obstetrics and Gynaecology, the First Affiliated Hospital of Kunming Medical College (Kunming, China) from January 2012 to September 2013, including three cases with normal glucose tolerance and three cases with GDM. The diagnosis of GDM was made by OGTT 75 g, according to the World Health Organization criteria, during the second trimester (24–28 weeks of gestation). Exclusion criteria for participation included multiple gestation, infection, pregnancy with complications, congenital or chromosomal abnormalities of the fetus, a family history of diabetes, and pregnancy with alcohol or drug abuse. Samples were obtained and immediately snap-frozen in liquid nitrogen. Informed consent was obtained prior to caesarean section. The present study was approved by the Ethics Committee of Kunming Medical College (Kunming, China).
RNA extraction and isolation
Adipose tissues from each of the six patients were individually minced with small scissors and total RNA was extracted using TRIzol reagent (Invitrogen; Thermo Fisher Scientific, Inc., Waltham, MA, USA) and purified using the RNeasy Mini kit (Qiagen, Hilden, Germany). The RNA concentration was detected using a 2100 Bioana bioanalyzer (Agilent Technologies, Inc., Santa Clara, CA, USA). RNA purity and integrity were assessed by gel electrophoresis as well as spectrophotometrically using a Nanodrop (Thermo Fisher Scientific, Inc.). The extracted RNA was temporarily stored in a −70°C freezer in 95% ethanol for further analysis.
Microarray assay and data normalization
The whole Human Gene Expression Array (Affymetrix GeneChip® PrimeView™, Homo sapiens; Affymetrix, Santa Clara, CA, USA) was used to screen for gene expression in the OVAT cells of pregnant women according to the manufacturer's instructions.
First, the ribosomal RNA was removed from the total RNA, and the purified mRNA was amplified and reversely transcribed into fluorescent/biotinylated complementary (c)DNA using the ENZO kit (Affymetrix). The cDNA was fragmented and then hybridized to the Affymetrix GeneChip® PrimeView™ containing 36,000 probe-sets representing ~20,000 unique genes. Six microarrays were run for the samples (from the six patients including three cases with normal glucose tolerance and three cases with GDM mentioned above) tested and each array was replicated twice. Subsequently, the arrays were processed on an Affymetrix fluidics station (Affymetrix), where they were subjected to automated washing and staining. The arrays were scanned using an Affymetrix GeneChip scanner 3000 (Affymetrix), raw data were obtained using the Feature Extraction Software 10.7 (Agilent Technologies, Inc.) and normalized using the quantile algorithm with Gene Spring 11.0 (Agilent Technologies, Inc.) to remove background bias with the normalization value set to 1. Systematic bioinformatic analyses of the microarray data were performed by Novel Bioinformatics Co., Ltd. (Shanghai, China).
Differential expression analysis, GO analysis, Kyoto Encyclopedia of Genes and Genomes (KEGG) pathway analysis, gene-gene interaction network (Gene-Act-Net) and pathway-pathway (Path)-Act-Net construction
Genes with fold-changes of ≥2 or <0.5 and P<0.05 were subjected to a secondary selection based on the size of the negative log2 of their P-values, and the thereby selected genes were considered to be DEGs.
To assess the function of the DEGs, they were enriched into terms of the GO categories cellular component (CC), biological process (BP) and molecular function (MF) using the GO chart feature of the Database for Annotation, Visualization and Integrated Discovery.
Significantly enriched pathways of these DEGs were then determined using the KEGG database, and Gene-Act-Net interaction network was constructed with regard to genes, included in the database.
Based on the results of the KEGG enrichment analyses, the Path-Act-Net was constructed. Furthermore, the Gene-Act-Net was constructed based on the DEGs in the GO terms and pathways.
Results
Patient characteristics
Between the patients with and without GDM, no significant differences in age, G1P0 parity, gestational week or height were present. However, the weight and body mass index were significantly higher in the GDM group.
DEGs in OVATS of GDM patients
A total of 935 DEGs were identified, including 450 genes which were downregulated and 485 which were upregulated in the OVATS of pregnant women with GDM compared with those without.
GO analysis of DEGs
In the GO category MF, terms including receptor binding, actin binding, extracellular matrix binding and C-X-C motif chemokine receptor R3 binding were found to be enriched. Moreover, in the category CC, DEGs were enriched in the terms extracellular matrix/region or actin cytoskeleton, while in the category BP, antigen processing and presentation, extracellular matrix organization, positive regulation of cell-substrate adhesion, response to nutrients and response to dietary excess were significantly over-represented.
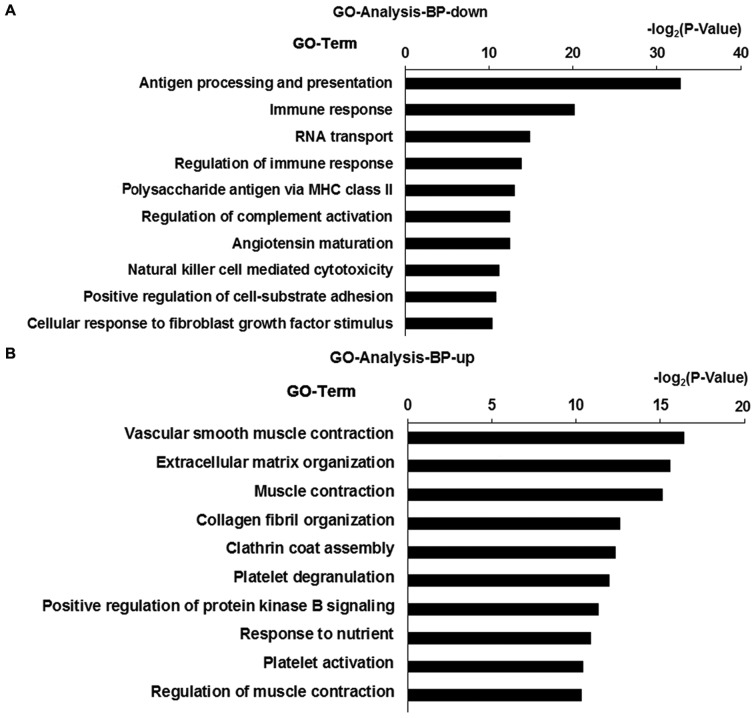
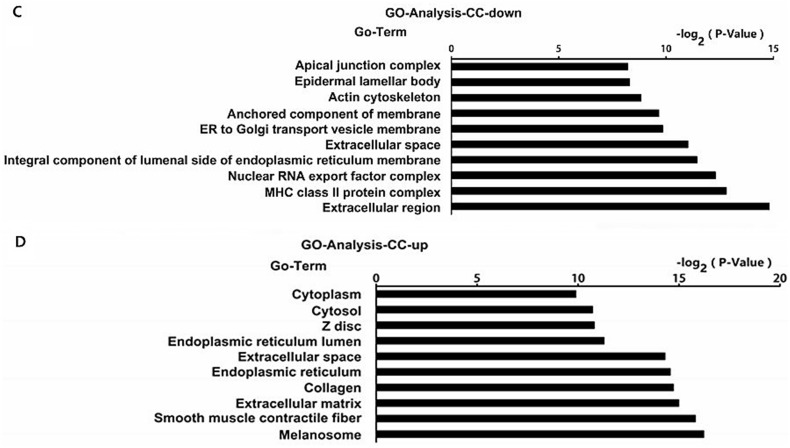
In the BP category, antigen processing and presentation, immune response and regulation of immune response were among the major downregulated GO terms (Fig. 1A), while vascular smooth muscle contraction, extracellular matrix organization and response to nutrients were among the major upregulated GO terms (Fig. 1B). Similarly, the top 10 down- and upregulated GO terms in the CC category are shown in Fig. 1C and D, respectively, and those in the MF category are shown in Fig. 1E and F, respectively.
Figure 1.
Top 10 GO terms in the categories (A and B) MF and (C and D) CC for down- and upregulated DEGs, respectively, in omental visceral adipose tissues of women with gestational diabetes mellitus. The longer the bar, the smaller the P-value. DEGs were rated according to their log2(P-value) using the Database for the Annotation, Visualization and Integrated Discovery (P<0.05). Top 10 GO terms in the categories (E and F) BP for down- and upregulated DEGs, respectively, in omental visceral adipose tissues of women with gestational diabetes mellitus. The longer the bar, the smaller the P-value. DEGs were rated according to their log2(P-value) using the Database for the Annotation, Visualization and Integrated Discovery (P<0.05). GO, gene ontology; DEG, differentially expressed gene; MHC, major histocompatibility complex; BP, biological process; CC, cellular component; MF, molecular function; up, upregulated; down, downregulated; ER, endoplasmic reticulum, MHC, major histocompatibility complex; IgG, immunoglobulin G.
In the CC category, extracellular region, major histocompatibility complex class II and nuclear RNA export factor complex were the major donwnregulated GO terms (Fig. 1C), while melanosome, smooth muscle contractile fiber and extracellular matrix were the major downregulated GO terms (Fig. 1D).
In the MF category, natural killer (NK) cell lectin-like receptor binding, serine-type endopeptidase activity and peptide antigen binding were the top three donwnregulated GO terms (Fig. 1E), while heparin binding, phosphatidylserine binding and phosphatidylinositol-4,5-bisphosphate binding were the top three upregulated GO terms (Fig. 1F). The terms likely to be relevant for GDM were antigen processing and presentation, immune response and response to nutrients.
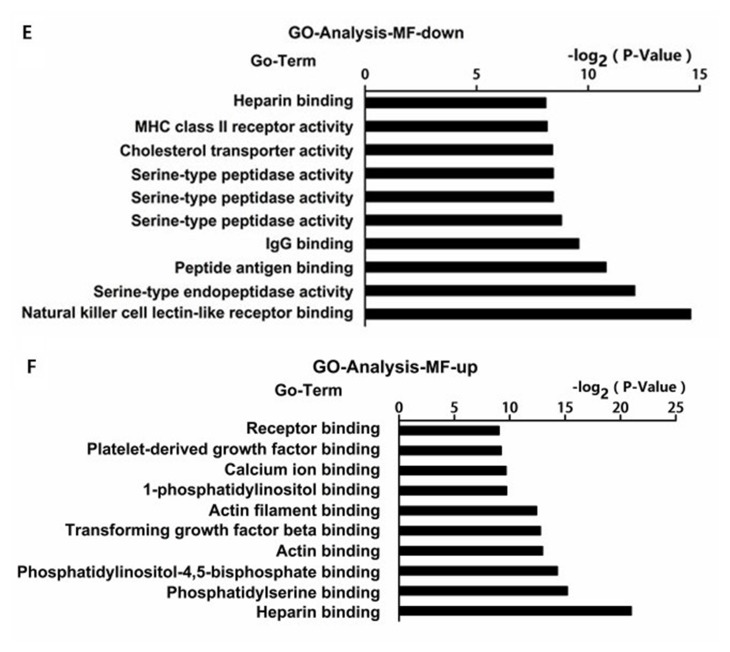
KEGG pathway analysis
To identify the most commonly dysregulated pathways in OVATs of pregnant women with GDM, KEGG pathway analysis was performed. The top six enriched pathways of the DEGs were antigen processing and presentation, viral myocarditis, graft-versus-host disease, phagosome, allograft rejection and type I diabetes mellitus (T1D) (Fig. 2A). With regard to the antigen processing and presentation pathway, 79 genes were represented on the array chips, of which 14 were differentially expressed [transporter 2, ATP-Binding Cassette, Sub-Family B (P=0.0046), LOC100287534 (P=0.0160), major histocompatibility complex, class I, A (HLA-A; P=0.011), killer cell immunoglobulin-like receptor (KIR)2DL4 (P=0.0160), KIR2DL5A (P=0.0161), HLA-DQA1 (P=0.0139), heat shock protein (HSP)A5 (P=0.0189), HLA-E (P=0.0199), HLA-DOA (P=0.0251), HLA-F (P=0.0299), HLA-DMB (P=0.033), HSPA4 (P=0.0379), HSPA6 (P=0.0390), HLA-DPB1 (P=0.0489)].
Figure 2.
KEGG pathway-enrichment analysis for DEGs in omental visceral adipose tissues of women with gestational diabetes mellitus. The longer the bar, the smaller the P-value. Significant enrichment pathways were determined from these DEGs using the KEGG database. Enriched KEGG pathways (A) determined using the Database for the Annotation, Visualization and Integrated Discovery (P<0.05). (B) For upregulated DEGs and (C) for downregulated DEGs with the greatest enrichment score. KEGG, Kyoto Encyclopedia of Genes and Genomes; PPAR, peroxisome proliferator-activated receptor; ECM, extracellular matrix; DEG, differentially expressed gene.
The top five upregulated pathways included focal adhesion, extracellular matrix (ECM)-receptor interaction, proteoglycans in cancer, vascular smooth muscle contraction and the peroxisome proliferator-activated receptor signaling pathway (Fig. 2B). The top four downregulated pathways included graft-versus-host disease, antigen processing and presentation, allograft rejection and NK cell-mediated cytotoxicity (Fig. 2C).
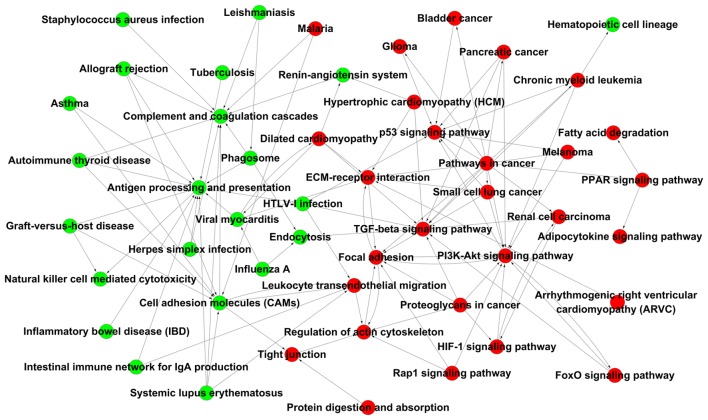
Gene-Act-Net and Pathway-Act-Net
The Gene-Act-Net and the Path-Act-Net were constructed based on the interaction of the DEGs or their enriched pathways, respectively (P<0.05). In the Path-Act-Net, antigen processing and presentation was the top-scoring component identified. Furthermore, complement and coagulation cascades, cell adhesion molecules, the transforming growth factor (TGF)-β, phosphoinositide-3 kinase (PI3K)-Akt and P53 signaling pathways, and regulation of the actin cytoskeleton were high-scoring components in the network, suggesting that immune response and signaling pathways associated with insulin are the major pathways associated with the pathogenesis of GDM. Within the network, antigen processing and presentation as well as cell adhesion molecules were pathways associated with downregulated DEGs with the highest number of connections, while TGF-β signaling, focal adhesion, PI3K-Akt signaling, P53 signaling, ECM-receptor interaction and regulation of the actin cytoskeleton were pathways associated with upregulated DEGs with the highest number of connections (Fig. 3).
Figure 3.
Pathway-pathway network analysis. Pathway-pathway-network based on the enriched pathways of differentially expressed genes between omental visceral adipose tissues of pregnant women with and without gestational diabetes mellitus. Each circle represents a pathway within the interaction network and lines represent the association of the pathways. Upregulated pathways are highlighted in red and downregulated pathways in green. PI3K, phosphoinositide-3 kinase; HTLV-I, human T-lymphotropic virus; PPAR, peroxisome proliferator-activated receptor; IgA, immunoglobulin A; FoxO, forkhead box O; TGF, transforming growth factor; HIF, hypoxia-inducible factor; ECM, extracellular matrix.
In the Gene-Act-Net, the four genes with the highest degree of interaction were integrin subunit β-1 (ITGB1), AKT serine/threonine kinase 3 (AKT3), integrin subunit α V (ITGAV) and fibroblast growth factor receptor (FGFR)3 (≥10 connections) (Table I).
Table I.
Differentially expressed genes with the highest degree of interaction in the gene-gene interaction network.
| Gene ID | Symbol | Description | InDegree | OutDegree | Degree |
|---|---|---|---|---|---|
| 3688a | ITGB1 | Integrin subunit β-1 | 9 | 7 | 16 |
| 10000a | AKT3 | AKT serine/threonine kinase 3 | 2 | 10 | 12 |
| 3685a | ITGAV | Integrin subunit α V | 9 | 1 | 10 |
| 2261b | FGFR3 | Fibroblast growth factor receptor 3 | 8 | 2 | 10 |
| 3105b | HLA-A | Major histocompatibility complex, class I, A | 3 | 5 | 8 |
| 3134b | HLA-F | Major histocompatibility complex, class I, F | 3 | 5 | 8 |
| 3133b | HLA-E | Major histocompatibility complex, class I, E | 3 | 5 | 8 |
| 10398a | MYL9 | Myosin light chain 9 | 6 | 1 | 7 |
| 6385b | SDC4 | Syndecan-4 | 6 | 0 | 6 |
| 4659a | PPP1R12A | Protein phosphatase 1 regulatory subunit 12A | 3 | 3 | 6 |
| 5500a | PPP1CB | Protein phosphatase 1 catalytic subunit β | 3 | 3 | 6 |
| 3479a | IGF1 | Insulin-like growth factor 1 | 3 | 3 | 6 |
| 2257a | FGF12 | Fibroblast growth factor 12 | 3 | 3 | 6 |
| 2259a | FGF14 | Fibroblast growth factor 14 | 3 | 3 | 6 |
| 7410b | VAV2 | VAV2 guanine nucleotide exchange factor | 3 | 3 | 6 |
| 2952a | GSTT1 | Glutathione S-transferase theta-1 | 3 | 3 | 6 |
| 4257a | MGST1 | Microsomal glutathione S-transferase 1, isoform CRA_a | 3 | 3 | 6 |
| 2949a | GSTM5 | Glutathione S-transferase Mu 5 | 3 | 3 | 6 |
| 3111b | HLA-DOA | Major histocompatibility complex, class II, DO α | 3 | 3 | 6 |
| 3109b | HLA-DMB | Major histocompatibility complex, class II, DM β | 3 | 3 | 6 |
| 3115b | HLA-DPB1 | Major histocompatibility complex, class II, DP β 1 | 3 | 3 | 6 |
| 3117b | HLA-DQA1 | cDNA FLJ51239, moderately similar to major histocompatibility complex class II histocompatibility antigen, DQ(W3) α chain | 3 | 3 | 6 |
| 7057a | THBS1 | Thrombospondin 1, isoform CRA_a | 1 | 4 | 5 |
| 21826a | THBS2 | Thrombospondin-2 | 1 | 4 | 5 |
| 998a | CDC42 | Cell division cycle 42, isoform CRA_a | 1 | 4 | 5 |
| 8644a | AKR1C3 | Aldo-keto reductase family 1 member C3 homolog | 4 | 1 | 5 |
| 7363a | UGT2B4 | UDP-glucuronosyltransferase 2 member B4 | 1 | 4 | 5 |
| 7037b | TFRC | Transferrin receptor (p90, CD71) mRNA | 4 | 1 | 5 |
| 1282a | COL4A1 | Collagen type IV α 1 chain | 1 | 3 | 4 |
| 1281a | COL3A1 | Collagen type III α 1 chain | 1 | 3 | 4 |
| 4638a | MYLK | Myosin light chain kinase | 3 | 1 | 4 |
| 1277a | COL1A1 | Collagen type I α-1 chain | 1 | 3 | 4 |
| 3371a | TNC | Tenascin C | 1 | 3 | 4 |
| 57292b | KIR2DL5A | Killer cell immunoglobulin like receptor, two Ig domains and long cytoplasmic tail 5A | 3 | 1 | 4 |
| 3805b | KIR2DL4 | Killer cell immunoglobulin like receptor, two Ig domains and long cytoplasmic tail 4 | 3 | 1 | 4 |
| 6891b | TAP2 | Transporter 2, ATP binding cassette subfamily B member | 0 | 4 | 4 |
| 4192a | MDM2 | E3 ubiquitin-protein ligase Mdm2 | 2 | 1 | 3 |
| 5781a | PTPN11 | Protein tyrosine phosphatase, non-receptor type 11 | 2 | 1 | 3 |
| 1962a | EHHADH | Enoyl-CoA hydratase and 3-hydroxyacyl CoA dehydrogenase | 1 | 2 | 3 |
| 2180a | ACSL1 | Acyl-CoA synthetase long-chain family member 1 mRNA | 1 | 2 | 3 |
| 4773b | NFATC2 | Nuclear factor of activated T-cells 2 | 1 | 1 | 2 |
| 948a | CD36 | CD36 antigen mRNA | 2 | 0 | 2 |
| 4629a | MYH11 | Myosin heavy chain 11 | 1 | 1 | 2 |
| 2316a | FLNA | Filamin-A | 0 | 2 | 2 |
| 94274a | PPP1R14A | Protein phosphatase 1 regulatory subunit 14A | 0 | 2 | 2 |
| 51a | ACOX1 | Acyl-CoA oxidase 1 | 2 | 0 | 2 |
| 7043a | TGFB3 | Transforming growth factor, β 3 | 2 | 0 | 2 |
| 4734b | NEDD4 | Neural precursor cell expressed, developmentally downregulated 4, E3 ubiquitin protein ligase | 1 | 1 | 2 |
| 548596b | CKMT1A | Creatine kinase, mitochondrial 1A | 1 | 1 | 2 |
| 1159b | CKMT1B | Creatine kinase, mitochondrial 1B (EC 2.7.3.2) | 1 | 1 | 2 |
| 10725b | NFAT5 | Nuclear factor of activated T-cells 5, tonicity-responsive, isoform CRA_b | 1 | 0 | 1 |
| 3952a | LEP | Leptin | 0 | 1 | 1 |
| 3563b | IL3RA | Interleukin-3 receptor subunit α | 1 | 0 | 1 |
| 284a | ANGPT1 | Angiopoietin-1 | 0 | 1 | 1 |
| 2034a | EPAS1 | Endothelial PAS domain-containing protein 1 | 0 | 1 | 1 |
| 10332b | CLEC4M | C-type lectin domain family 4, member M, transcript variant 6 mRNA | 0 | 1 | 1 |
| 1759b | DNM1 | Dynamin-1 (EC 3.6.5.5) | 0 | 1 | 1 |
Upregulated genes
downregulated genes.
InDegree, number of inbound gene interactions; OutDegree, number of outbound gene interactions; cDNA, complementary DNA; Ig, immunoglobulin; CoA, coenzyme A.
Discussion
GDM is defined as the first occurrence of glucose intolerance during pregnancy. Although it is a common disorder, its pathophysiology has remained to be fully elucidated. Adipose tissue has been implicated in the development of insulin resistance and excess adipose tissue has been shown to be associated with GDM (11,12).
Adipose tissue can be further classified as sub-cutaneous and visceral adipose tissue. The human body has six visceral fat depots: Perirenal, gonadal, epicardial, retroperitoneal, omental and mesenteric adipose, each of which has distinct characteristics. Human omental adipose tissue exhibits specific mRNA expression profiles. Only few studies have compared the difference in expression profiles in OVATs of pregnant women with and without GDM (13,14). To the best of our knowledge, the present study was the first to assess the DEGs in OVATs from pregnant women with vs. without GDM using the Affymetrix chip due to the difficulty in obtaining OVAT samples during the same period, which are matched with regard to age, gestational age, G1P0 parity and height.
The microarray approach and bioinformatic technologies were combined to perform a comparative gene expression profiling analysis of normal and pathological OVATs. Subsets of DEGs were identified, GO and KEGG pathways were analyzed, and interaction networks were generated.
The DEGs identified between the two groups may represent new candidate genes associated with GDM. In the present study, the top four genes in the Gene-Act-Net with the highest degree of interaction were ITGB1, AKT3, ITGAV (upregulated) and FGFR3 (downregulated), suggesting their function as hub genes with a high regulatory ability. ITGB7 and ITGB1 have been previously reported to be associated with type 1 diabetes and their proteins engage in direct mutual receptor-ligand interactions associated with the homing of T cells from blood to tissues, such as the intestine and pancreas (15). ITGB1 was also found to be involved in the regulation of cell migration associated with numerous pathologies (16–18). AKT3 is activated by growth factors and other extracellular stimuli, including glucose, as well as key upstream regulatory proteins including Ras, PI3K subunits and phosphatase and tensin homolog, which are involved in the regulation of a diversity of biological roles of activated Akt, including the regulation of cell metabolism, survival and proliferation (19,20). ITGAV and FGFR3 are involved in cell migration and proliferation, and have been reported to be associated with the progression and dissemination of cancer (21–24).
GO analysis revealed enrichment of the DEGs in the MF category in terms including receptor binding, extracellular matrix binding and CXCR3, as well as in the BP category in terms including antigen processing and presentation, extracellular matrix organization, positive regulation of cell-substrate adhesion, which were also closely associated with inflammation response or immune response. In addition, the DEGs in the GDM group were enriched in GO terms including vascular smooth muscle contraction (GO:0014829) and muscle contraction (GO:0006936), possibly due to the impaired vasodilation in the GDM group. The function of vascular smooth muscle cells is to regulate blood flow and pressure through contraction and relaxation. The principle complications of GDM are cardiovascular disease, the risk of which is potentiated by obesity, hypertensive disorders of pregnancy. Studies have shown that women with GDM have higher risk of cardiac dysfunction and endothelial dysfunction very soon after pregnancy (25), which may explain for the upregulation of these pathways compared with those in normal women in the same gestational week. Furthermore, preterm delivery is relatively common in women with GDM and birth-associated muscle contractions may be another reason for the enrichment of these pathways in the GDM group (26).
In the present study, KEGG analysis revealed that the DEGs in the OVATs from patients with GDM were enriched in pathways including antigen processing and presentation, cell adhesion molecules, T1D, NK cell-mediated cytotoxicity and TGF-β signaling. These pathways were categorized as ‘signaling molecules and interaction’, ‘immune system’ and ‘inflammatory response’, suggesting that these processes are involved in GDM. Among them, four pathways (antigen processing and presentation, cell adhesion molecules, T1D and NK cell-mediated cytotoxicity) have been previously reported in the blood of Chinese women with GDM (27). Considering that OVAT is composed of several different cell types, including adipocytes, pre-adipocytes, macrophages, vascular cells and other blood cells, it is reasonable to assume that certain significant pathways are similar between OVAT and peripheral blood, and insulin resistance in peripheral blood and adipose tissue may also share certain pathways. A study by Yang et al (28) demonstrated that TGF-β signaling participates in steatohepatitis through the regulation of lipid metabolism and apoptosis in hepatocytes. Considering that the present study used adipose tissues, it is expected that pathways associated with lipid metabolism dysfunction have a marked role in the insulin resistance of patients with GDM. In the present study, DEGs were enriched in pathways including peroxisome proliferator-activated receptor signaling, adipocytokine signaling and fatty acid degradation, which are associated with lipid metabolism.
As for pathways associated with T1D, the results of the present study suggested that GDM is mainly facilitated by autoimmune destruction of insulin-producing pancreatic β-cells. The nine genes found to be involved, HLA-A, HLA-DQA1, granzyme B, HLA-F, HLA-E, perforin 1, HLA-DOA, HLA-DMB and HLA-DPB1, were all downregulated. These results may indicate similarities between GDM and T1D. However, it has been reported that pregnant women have an increased risk of developing T2D. GDM may share common characteristics with T1D, including insulin resistance and the immune response; the findings of the present study are therefore in accordance with those of previous ones, which appeared to have detected autoimmune phenomena in patients with GDM (29). Evangelista et al (30) reported that gene expression signatures of GDM patients were closer to those of T1D patients than to those of T2D patients, which may provide an explanation for the findings of the present study.
In the present study, KEGG analysis also suggested that pathways associated with antigen processing and presentation were dysregulated in the GDM group. The findings highlight a significant role of HLA genes in the adipose tissue of women with GDM. A general downregulation of HLA genes has been observed among placentas and blood samples from women with GDM (31). In general, GDM has been associated with increased anti-HLA-class II antibodies in the maternal circulation and reduced tolerance towards alloantigen through inflammatory activation (32).
In the present study, the relevant terms in which DEGs were enriched were antigen processing and presentation, immune response and response to nutrients. Maternal over-nutrition has been reported to be associated with elevated triglyceride levels, increased inflammatory markers and fatty livers in offspring (33). GDM is reconsidered to be a state of chronic, low-grade inflammation and is, distinct from an acute pro-inflammatory response, primarily triggered by metabolites and nutrients, leading to systemic insulin resistance.
As for NK cell-mediated cytotoxicity pathways, their participation in GDM progression is expected due to the proposed involvement of the NK pathway in T1D (34). It is thought that the NK pathway causes the release of cytotoxic granules, penetration of effector proteins through the cell membrane and subsequent induction of apoptosis. Considering adipose tissue being the main inflammatory organ and highly expressing numerous inflammatory mediators, it is expected that inflammatory pathways are associated with its role in GDM. It has been speculated that cytokine-mediated inflammation leads to metabolic abnormalities by increasing insulin resistance in patients (35). Numerous pre-clinical and clinical studies support the notion that obesity-induced inflammation may be a specific type of inflammation resulting from overnutrition and stress pathways that drive abnormal metabolic homeostasis and lead to insulin resistance (36). It has been widely evidenced that obesity is a major cause of impaired insulin signaling (37–39). However, the precise molecular mechanisms of the obesity-induced inflammation causing insulin resistance have remained to be elucidated.
As for focal adhesion, the present study revealed a hub function in the Path-Act-Net of upregulated DEGs. The focal adhesion pathway is closely associated with the insulin signaling pathway. Focal adhesion proteins are integrin-rich microdomains, which transmit mechanical signals from the ECM to activate signaling pathways inside the cell and structurally link the cytoskeleton to the ECM. Cell adhesion and focal adhesion kinases regulate insulin receptor substrate-1 expression (40). Focal adhesion kinase is a substrate for the insulin and insulin-like growth factor-1 tyrosine kinase receptors (41–43). For instance, Bisht and Dey (43) reported that focal adhesion kinase regulates insulin resistance in skeletal muscle. Zhang et al (44) also reported that the focal adhesion pathway was of high significance in the functional interaction network of DEGs in adipose tissues of patients with insulin resistance.
The results of the KEGG and GO enrichment analyses suggested that antigen processing and presentation was significantly different in OVAT tissues of pregnant women with and without GDM, suggesting that immune responses are involved in GDM. This may be due to the fact that the OVAT tissues are under pathological stress and hypoxia, leading to immune-associated responses, such as the feto-matenal tolerance, innate immunity and inflammation response. Based on the previously suggested involvement of immune responses T1D, it is likely that it is also involved in the development and progression of GDM.
In conclusion, the results of the present study suggested that hub genes of the Gene-Act-Net, including ITGB1, AKT3, ITGAV and FGFR3, in OVAT are associated with GDM. Furthermore, molecular signaling pathways associated with immune responses, inflammatory processes, focal adhesion and signal transduction were identified to be closely associated with GDM in Chinese women. These candidate genes and pathways provided novel insight into the pathogenesis of insulin resistance in OVAT of GDM patents. However, the present study was limited by the low number of study subjects; furthermore, the differential expression of certain genes may have been a result, but not necessarily a cause of GDM. Further experimental studies are therefore required to confirm or expand the conclusions of the present study.
Acknowledgements
The present study was supported by the Natural Science Foundation of China (no. 81360103) and the Application of Basic Research Project of Yunnan Province (no. 2012FB039).
References
- 1.Kjos SL, Buchanan TA. Gestational diabetes mellitus. N Engl J Med. 1999;341:1749–1756. doi: 10.1056/NEJM199912023412307. [DOI] [PubMed] [Google Scholar]
- 2.Kasuga M. Insulin resistance and pancreatic beta cell failure. J Clin Invest. 2006;116:1756–1760. doi: 10.1172/JCI29189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.White MF. Insulin signaling in health and disease. Science. 2003;302:1710–1711. doi: 10.1126/science.1092952. [DOI] [PubMed] [Google Scholar]
- 4.Wójcik M, Chmielewska-Kassassir M, Grzywnowicz K, Woźniak L, Cypryk K. The relationship between adipose tissue-derived hormones and gestational diabetes mellitus (GDM) Endokrynol Pol. 2014;65:134–142. doi: 10.5603/EP.2014.0019. [DOI] [PubMed] [Google Scholar]
- 5.Fasshauer M, Blüher M, Stumvoll M. Adipokines in gestational diabetes. Lancet Diabetes Endocrinol. 2014;2:488–499. doi: 10.1016/S2213-8587(13)70176-1. [DOI] [PubMed] [Google Scholar]
- 6.Ibrahim MM. Subcutaneous and visceral adipose tissue: Structural and functional differences. Obes Rev. 2010;11:11–18. doi: 10.1111/j.1467-789X.2009.00623.x. [DOI] [PubMed] [Google Scholar]
- 7.Insenser M, Montes-Nieto R, Vilarrasa N, Lecube A, Simó R, Vendrell J, Escobar-Morreale HF. A nontargeted proteomic approach to the study of visceral and subcutaneous adipose tissue in human obesity. Mol Cell Endocrinol. 2012;363:10–19. doi: 10.1016/j.mce.2012.07.001. [DOI] [PubMed] [Google Scholar]
- 8.Sun G. Application of DNA microarrays in the study of human obesity and type 2 diabetes. OMICS. 2007;11:25–40. doi: 10.1089/omi.2006.0003. [DOI] [PubMed] [Google Scholar]
- 9.Draghici S, Khatri P, Eklund AC, Szallasi Z. Reliability and reproducibility issues in DNA microarray measurements. Trends Genet. 2006;22:101–109. doi: 10.1016/j.tig.2005.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Allison DB, Cui X, Page GP, Sabripour M. Microarray data analysis: From disarray to consolidation and consensus. Nat Rev Genet. 2006;7:55–65. doi: 10.1038/nrg1749. [DOI] [PubMed] [Google Scholar]
- 11.Guilherme A, Virbasius JV, Puri V, Czech MP. Adipocyte dysfunctions linking obesity to insulin resistance and type 2 diabetes. Nat Rev Mol Cell Biol. 2008;9:367–377. doi: 10.1038/nrm2391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Maassen JA, Romijn JA, Heine RJ. Fatty acid-induced mitochondrial uncoupling in adipocytes as a key protective factor against insulin resistance and beta cell dysfunction: A new concept in the pathogenesis of obesity-associated type 2 diabetes mellitus. Diabetologia. 2007;50:2036–2041. doi: 10.1007/s00125-007-0776-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ma Y, Gao J, Yin J, Gu L, Liu X, Chen S, Huang Q, Lu H, Yang Y, Zhou H, et al. Identification of a Novel Function of Adipocyte Plasma Membrane-Associated Protein (APMAP) in Gestational Diabetes Mellitus by Proteomic Analysis of Omental Adipose Tissue. J Proteome Res. 2016;15:628–637. doi: 10.1021/acs.jproteome.5b01030. [DOI] [PubMed] [Google Scholar]
- 14.Oliva K, Barker G, Rice GE, Bailey MJ, Lappas M. 2D-DIGE to identify proteins associated with gestational diabetes in omental adipose tissue. J Endocrinol. 2013;218:165–178. doi: 10.1530/JOE-13-0010. [DOI] [PubMed] [Google Scholar]
- 15.Evangelou M, Smyth DJ, Fortune MD, Burren OS, Walker NM, Guo H, Onengut-Gumuscu S, Chen WM, Concannon P, Rich SS, et al. A method for gene-based pathway analysis using genomewide association study summary statistics reveals nine new type 1 diabetes associations. Genet Epidemiol. 2014;38:661–670. doi: 10.1002/gepi.21853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhou F, Huang X, Zhang Z, Chen Y, Liu X, Xing J, He X. Functional polymorphisms of ITGB1 are associated with clinical outcome of Chinese patients with resected colorectal cancer. Cancer Chemother Pharmacol. 2015;75:1207–1215. doi: 10.1007/s00280-015-2745-4. [DOI] [PubMed] [Google Scholar]
- 17.Wang L, Zhang Y, Lv W, Lu J, Mu J, Liu Y, Dong P. Long non-coding RNA Linc-ITGB1 knockdown inhibits cell migration and invasion in GBC-SD/M and GBC-SD gallbladder cancer cell lines. Chem Biol Drug Des. 2015;86:1064–1071. doi: 10.1111/cbdd.12573. [DOI] [PubMed] [Google Scholar]
- 18.Fabbri C, Crisafulli C, Gurwitz D, Stingl J, Calati R, Albani D, Forloni G, Calabrò M, Martines R, Kasper S, et al. Neuronal cell adhesion genes and antidepressant response in three independent samples. Pharmacogenomics J. 2015;15:538–548. doi: 10.1038/tpj.2015.15. [DOI] [PubMed] [Google Scholar]
- 19.Eves R, Oldham R, Jia L, Mak AS. The roles of akt isoforms in the regulation of podosome formation in fibroblasts and extracellular matrix invasion. Cancers (Basel) 2015;7:96–111. doi: 10.3390/cancers7010096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Phung TL, Du W, Xue Q, Ayyaswamy S, Gerald D, Antonello Z, Nhek S, Perruzzi CA, Acevedo I, Ramanna-Valmiki R, et al. Akt1 and akt3 exert opposing roles in the regulation of vascular tumor growth. Cancer Res. 2015;75:40–50. doi: 10.1158/0008-5472.CAN-13-2961. [DOI] [PubMed] [Google Scholar]
- 21.Waisberg J, De Souza Viana L, Affonso Junior RJ, Silva SR, Denadai MV, Margeotto FB, De Souza CS, Matos D. Overexpression of the ITGAV gene is associated with progression and spread of colorectal cancer. Anticancer Res. 2014;34:5599–5607. [PubMed] [Google Scholar]
- 22.Denadai MV, Viana LS, Affonso RJ, Jr, Silva SR, Oliveira ID, Toledo SR, Matos D. Expression of integrin genes and proteins in progression and dissemination of colorectal adenocarcinoma. BMC Clin Pathol. 2013;13:16. doi: 10.1186/1472-6890-13-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hosen I, Rachakonda PS, Heidenreich B, de Verdier PJ, Ryk C, Steineck G, Hemminki K, Kumar R. Mutations in TERT promoter and FGFR3 and telomere length in bladder cancer. Int J Cancer. 2015;137:1621–1629. doi: 10.1002/ijc.29526. [DOI] [PubMed] [Google Scholar]
- 24.Guancial EA, Werner L, Bellmunt J, Bamias A, Choueiri TK, Ross R, Schutz FA, Park RS, O'Brien RJ, Hirsch MS, et al. FGFR3 expression in primary and metastatic urothelial carcinoma of the bladder. Cancer Med. 2014;3:835–844. doi: 10.1002/cam4.262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Noctor E, Crowe C, Carmody LA, Kirwan B, O'Dea A, Glynn LG, McGuire BE, O'Shea PM, Dunne FP. ATLANTIC-DIP: Prevalence of metabolic syndrome and insulin resistance in women with previous gestational diabetes mellitus by International Association of Diabetes in Pregnancy Study Groups criteria. Acta Diabetol. 2015;52:153–160. doi: 10.1007/s00592-014-0621-z. [DOI] [PubMed] [Google Scholar]
- 26.Koning SH, Hoogenberg K, Scheuneman KA, Baas MG, Korteweg FJ, Sollie KM, Schering BJ, van Loon AJ, Wolffenbuttel BH, van den Berg PP, et al. Neonatal and obstetric outcomes in diet- and insulin-treated women with gestational diabetes mellitus: A retrospective study. BMC Endocr Disord. 2016;16:52. doi: 10.1186/s12902-016-0136-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zhao YH, Wang DP, Zhang LL, Zhang F, Wang DM, Zhang WY. Genomic expression profiles of blood and placenta reveal significant immune-related pathways and categories in Chinese women with gestational diabetes mellitus. Diabet Med. 2011;28:237–246. doi: 10.1111/j.1464-5491.2010.03140.x. [DOI] [PubMed] [Google Scholar]
- 28.Yang L, Roh YS, Song J, Zhang B, Liu C, Loomba R, Seki E. Transforming growth factor beta signaling in hepatocytes participates in steatohepatitis through regulation of cell death and lipid metabolism in mice. Hepatology. 2014;59:483–495. doi: 10.1002/hep.26698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mauricio D, de Leiva A. Autoimmune gestational diabetes mellitus: A distinct clinical entity? Diabetes Metab Res Rev. 2001;17:422–428. doi: 10.1002/dmrr.237. [DOI] [PubMed] [Google Scholar]
- 30.Evangelista AF, Collares CV, Xavier DJ, Macedo C, Manoel-Caetano FS, Rassi DM, Foss-Freitas MC, Foss MC, Sakamoto-Hojo ET, Nguyen C, et al. Integrative analysis of the transcriptome profiles observed in type 1, type 2 and gestational diabetes mellitus reveals the role of inflammation. BMC Med Genomics. 2014;7:28. doi: 10.1186/1755-8794-7-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Binder AM, LaRocca J, Lesseur C, Marsit CJ, Michels KB. Epigenome-wide and transcriptome-wide analyses reveal gestational diabetes is associated with alterations in the human leukocyte antigen complex. Clin Epigenetics. 2015;7:79. doi: 10.1186/s13148-015-0116-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Steinborn A, Saran G, Schneider A, Fersis N, Sohn C, Schmitt E. The presence of gestational diabetes is associated with increased detection of anti-HLA-class II antibodies in the maternal circulation. Am J Reprod Immunol. 2006;56:124–134. doi: 10.1111/j.1600-0897.2006.00408.x. [DOI] [PubMed] [Google Scholar]
- 33.Oben JA, Mouralidarane A, Samuelsson AM, Matthews PJ, Morgan ML, McKee C, Soeda J, Fernandez-Twinn DS, Martin-Gronert MS, Ozanne SE, et al. Maternal obesity during pregnancy and lactation programs the development of offspring non-alcoholic fatty liver disease in mice. J Hepatol. 2010;52:913–920. doi: 10.1016/j.jhep.2009.12.042. [DOI] [PubMed] [Google Scholar]
- 34.Dotta F, Fondelli C, Falorni A. Can NK cells be a therapeutic target in human type 1 diabetes? Eur J Immunol. 2008;38:2961–2963. doi: 10.1002/eji.200838851. [DOI] [PubMed] [Google Scholar]
- 35.Hauguel-de Mouzon S, Guerre-Millo M. The placenta cytokine network and inflammatory signals. Placenta. 2006;27:794–798. doi: 10.1016/j.placenta.2005.08.009. [DOI] [PubMed] [Google Scholar]
- 36.Lee BC, Lee J. Cellular and molecular players in adipose tissue inflammation in the development of obesity-induced insulin resistance. Biochim Biophys Acta. 2014;1842:446–462. doi: 10.1016/j.bbadis.2013.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lumeng CN, Saltiel AR. Inflammatory links between obesity and metabolic disease. J Clin Invest. 2011;121:2111–2117. doi: 10.1172/JCI57132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hursting SD, Dunlap SM. Obesity, metabolic dysregulation, and cancer: A growing concern and an inflammatory (and microenvironmental) issue. Ann N Y Acad Sci. 2012;1271:82–87. doi: 10.1111/j.1749-6632.2012.06737.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Balsan GA, Vieira JL, Oliveira AM, Portal VL. Relationship between adiponectin, obesity and insulin resistance. Rev Assoc Med Bras 1992. 2015;61:72–80. doi: 10.1590/1806-9282.61.01.072. [DOI] [PubMed] [Google Scholar]
- 40.Lebrun P, Baron V, Hauck CR, Schlaepfer DD, Van Obberghen E. Cell adhesion and focal adhesion kinase regulate insulin receptor substrate-1 expression. J Biol Chem. 2000;275:38371–38377. doi: 10.1074/jbc.M006162200. [DOI] [PubMed] [Google Scholar]
- 41.Gupta A, Dey CS. PTEN, a widely known negative regulator of insulin/PI3K signaling, positively regulates neuronal insulin resistance. Mol Biol Cell. 2012;23:3882–3898. doi: 10.1091/mbc.E12-05-0337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gupta A, Bisht B, Dey CS. Focal adhesion kinase negatively regulates neuronal insulin resistance. Biochim Biophys Acta. 2012;1822:1030–1037. doi: 10.1016/j.bbadis.2012.02.011. [DOI] [PubMed] [Google Scholar]
- 43.Bisht B, Dey CS. Focal Adhesion Kinase contributes to insulin-induced actin reorganization into a mesh harboring Glucose transporter-4 in insulin resistant skeletal muscle cells. BMC Cell Biol. 2008;9:48. doi: 10.1186/1471-2121-9-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Zhang L, Cui Y, Fu F, Li Z, Pan X, Li H, Li L. An insight into the key genes and biological functions associated with insulin resistance in adipose tissue with microarray technology. Mol Med Rep. 2015;11:1963–1967. doi: 10.3892/mmr.2014.2909. [DOI] [PubMed] [Google Scholar]