Abstract
Women with alcohol use disorders (AUD) experience high rates of co-occurring conditions, such as depression and post-traumatic stress disorder (PTSD), which can complicate treatment engagement and response. Therefore, identifying factors that underlie alcohol use, depression, and PTSD symptoms in women with AUD has important treatment implications. The current study investigated emotion regulation as one such underlying factor. We tested a model that examined the extent to which changes in emotion regulation during treatment predicted women’s depression and PTSD symptom severity at treatment completion and subsequent alcohol use following treatment. The study included 48 participants enrolled in a randomized controlled trial of Interpersonal Psychotherapy (IPT) versus usual care for women with co-occurring alcohol dependence and major depression. Assessments were conducted at baseline, post-treatment (16 weeks), and follow-up (24 weeks). Descriptive statistics of baseline data revealed heightened levels of emotion dysregulation in this sample, which were related to fewer days abstinent from alcohol, more negative consequences from alcohol, and greater PTSD symptom severity. Women’s lower depressive symptoms at the end of treatment were found to mediate the relationship between improved emotion regulation during the treatment period and greater abstinence following treatment. Post-treatment PTSD symptoms, however, were not found to mediate that relationship. These results suggest that improvements in depressive symptoms during treatment are associated with emotion regulation at the end of treatment, which may contribute to greater abstinence from alcohol following treatment.
Keywords: Women, Alcohol, Emotion Regulation, Depression, Post-traumatic Stress
The rate of alcohol use disorders (AUD) among women has been continually rising (Ruiz & Oscar-Berman, 2013; White et al., 2015), and research has demonstrated significant physical, social, and emotional risks associated with women’s alcohol misuse (Stewart, Gavric & Collins, 2009). Additionally, women with AUD experience high rates of co-occurring mental health disorders. Depressive disorders are especially prevalent within this population, with 48.5% of women with lifetime AUD also reporting lifetime episodes of major depression (Kessler et al., 1997). Within a clinical sample of alcohol-dependent women [in the National Epidemiological Survey on Alcohol and Related Conditions (NESARC)], 62% were diagnosed with a comorbid mood disorder (major depression, dysthymia, or bipolar disorder). Furthermore, even after adjusting for sociodemographic characteristics and other psychiatric disorders, AUD women had an odds ratio of 1.5 to be diagnosed with major depression when compared to women without any AUD (Goldstein, Dawson, Chou & Grant, 2012). Additionally, there is a 16.9% lifetime prevalence of post-traumatic stress disorder (PTSD) in women with lifetime alcohol dependence (Goldstein, Dawson, Chou & Grant, 2012), a finding that is not surprising given that women with AUD have often experienced more traumatic life events when compared to the general population (World Health Organization, 2013).
Identifying correlates of alcohol use in women with AUD and co-occurring depression and/or PTSD has important treatment implications, as many of these women have been shown to experience difficulties engaging in and completing traditional substance use disorder treatments. While the relationship between co-occurring conditions and treatment outcome in women with AUD is somewhat complicated by moderating factors, the presence of co-occurring conditions has been found in many studies to complicate treatment retention and/or long-term outcomes (Greenfield et al., 2007). One particular way in which co-occurrence affects treatment is that, when women with co-occurring conditions do enter specialized treatment for AUD, treatment programs may have difficulty addressing both conditions concurrently. This issue is particularly evident in health care systems where substance use treatment and mental health care are siloed in different settings (Flynn & Brown, 2008).
Novel approaches are needed to simultaneously address co-occurring depression or PTSD in AUD treatment. Toward that end, targeting transdiagnostic processes that underlie commonly co-occurring conditions may be helpful (Barlow, Allen, & Choate, 2004; Nolen-Hoeksema & Watkins, 2011). A transdiagnostic process is defined as a construct that manifests across disorders and often varies along a continuum, ranging from adaptive to maladaptive (Nolen-Hoeksema & Watkins, 2011). When considering the population of AUD women with co-occurring depression and/or PTSD, the experience and regulation of negative emotion has been found to be an important, potentially transdiagnostic, factor that contributes to their drinking behavior.
In addition to the high prevalence rates of comorbid AUD and mood disorders as described above, the importance of negative emotion in understanding women’s alcohol use has been supported by research showing negative emotion can act as a momentary trigger for alcohol use (Rubonis et al., 1994) as well as a trigger for relapse after a period of sustained abstinence (Walitzer & Dearing, 2006). A recent study found that women with AUDs had a higher prevalence of anxiety and depression disorders and a higher propensity to drink in negative emotional states compared to men (Karpyak et al., 2016). In a sample of patients with PTSD and alcohol dependence, coping motives (drinking to cope with negative emotion) were significantly associated with average number of drinks per day for female patients. In contrast, coping motives were not associated with average drinks per day in male patients with PTSD and AUD, whereas enhancement motives were (Lehavot, Stappenbeck, Luterek, Kaysen & Simpson, 2014).
Relatedly, research has shown that the regulation of negative emotion is an important factor in alcohol use, depression, and PTSD (Kring & Sloan, 2009), and is perhaps more malleable than the inevitable experience of negative emotion. Full-scale clinical trials have suggested that changes in emotion regulation skills are related to positive treatment outcomes, including decreased alcohol use. Specifically, one study exploring the extent to which emotion regulation skills predicted alcohol use in a group of individuals (men and women) receiving cognitive-behavioral therapy (CBT) for AUD found that deficits in post-treatment emotion regulation skills predicted alcohol use during follow-up, after controlling for symptom severity, cognitive capacities, and level of negative affect (Berking et al., 2011). A separate RCT that tested affect regulation training (ART) as an add-on to CBT for patients with alcohol dependence showed positive effects of ART on drinking outcomes (but, interestingly, not on measured emotion regulation strategies) in patients who received that training (Stasiewicz et al., 2013). These studies were conducted with mixed samples of men and women and did not report results within individuals with co-occurring AUD, PTSD and/or depression. However, Stasiewicz and colleagues conducted their study with individuals with a negative affect drinking profile, who may be more predisposed to co-occurring emotional disorders. It is plausible that in women with AUD and co-occurring depression and/or PTSD symptoms, for whom negative emotion may be particularly linked to drinking, these positive effects of improved emotion regulation on drinking may be even greater.
Furthermore, research has demonstrated the importance of emotion dysregulation in PTSD and depression independently. One study with male Veterans receiving treatment for PTSD found that specific types of emotion regulation strategies were associated with PTSD symptom severity. Specifically, their decreased use of ineffective emotion regulation strategies (i.e., emotional suppression) during treatment was found to predict post-treatment symptom severity (Boden et al., 2013). Studies examining specific emotion regulation strategies among trauma-exposed women have also found significant associations between use of ineffective emotion regulation strategies and higher levels of PTSD and depressive symptoms (Eftekhari, Zoellner, & Vigil, 2009; Moore, Zoellner, & Molenholt, 2008). Indeed, research has examined the association between emotion dysregulation and PTSD or depression to a more specific extent, but has been examined less in samples of individuals who have co-occurring AUD.
Emerging research that has examined emotion regulation in individuals with co-occurring PTSD and substance use disorders (SUD) has primarily used predictive and correlational designs. One study with patients at a SUD residential facility found that individuals with co-occurring SUD-PTSD had greater emotion dysregulation and more impulsive behaviors than those with SUD alone (Weiss, Tull, Viana, Anestis, & Gratz, 2012). Another study that examined PTSD symptoms and substance use (drug and/or alcohol) in young adult women found no direct relationship between PTSD symptoms and overall substance use – however, the symptoms were associated with later use in the context of heightened emotion dysregulation (Tull, Bardeen, DiLillo, & Messman-Moore, 2015). One study, conducted with a highly comorbid, diagnostically heterogeneous sample of men and women at a residential substance use treatment facility, found that emotion dysregulation was uniquely associated with patients’ anxiety, depression, PTSD, and AUD symptom severity. This finding was significant even after controlling for insomnia severity and the shared variance between anxiety, depression, PTSD, and AUD symptoms (Fairholme, Nosen, Nillni, Schumacher, Tull & Coffey, 2013). Although research has demonstrated the saliency of emotion dysregulation to general substance use and co-occurring PTSD, the exact directionality of the relationship is less clear. Research that has examined the directional relationships between emotion regulation, substance use, and co-occurring conditions has primarily examined and found preliminary support for emotion regulation as a mediator between co-occurring conditions (primarily PTSD) and substance use, but has largely used cross-sectional research designs (Weiss, Tull, Viana, Anestis, & Gratz, 2012; Bonn-Miller, Vujanovic, Boden & Gross, 2011; Bornovalova, Ouimette, Crawford, & Levy, 2009; Tull, Bardeen, DiLillo, Messman-Moore, & Gratz, 2015).
Collectively, the aforementioned work suggests that women with AUDs have high rates of co-occurring depression and/or PTSD and may be particularly driven by motives to drink to cope with negative emotion. In addition, a growing body of evidence suggests that emotion regulation is associated with symptom severity and substance-related treatment outcomes in individuals with co-occurring depression and/or PTSD symptoms. As discussed above, we hypothesize that emotion regulation may act as an underlying transdiagnostic mechanism that drives depressive or PTSD symptom intensity and subsequent drinking behavior. While establishing a construct as a transdiagnostic variable is a prolonged and detailed process (Nolen-Hoeksema & Watkins, 2011), our goal was to test a model guided by this concept. Specifically, we sought to examine improved emotion regulation as a proximal factor which may enhance the likelihood of a woman experiencing a number of positive post-treatment outcomes, including depression, PTSD, and alcohol misuse. The current study tested a multiple mediation model by which depression and PTSD symptom severity at the end of treatment mediated the association between changes in emotion regulation over the course of treatment and alcohol consumption at the end of treatment and during follow-up.
Methods
Design and Setting
Data for this study were gathered from a randomized controlled trial (RCT) examining the efficacy of Interpersonal Therapy (IPT) for comorbid alcohol dependence (AD) and major depression (MD) in women. Participants for this study were recruited from a multidisciplinary substance use treatment program for individuals with co-occurring disorders in an outpatient chemical dependency clinic. All women in the study received standard, group-based chemical dependency treatment that was abstinence-oriented. The groups were held three days per week for 1.5 hours in each session. Psychiatric evaluation and medication management were provided on an as-needed basis. Group sessions focused on teaching patients symptom management of co-occurring conditions and alcohol-related coping skills. In addition, women were randomized to receive either eight sessions of IPT or “usual care” individual sessions as clinically indicated. An 8-session adjunctive dose of IPT was selected given that patients were already attending three addiction treatment groups per week. Since the study was conducted in a community outpatient substance abuse treatment center with community therapists (who delivered IPT in this study as part of their usual caseload), individual treatment sessions were typically scheduled on a bi-weekly (versus weekly) basis. Therefore, although there were 8 sessions, therapists delivered the sessions over 16 weeks.
Participants
To be eligible for the study, participants needed to be English-speaking women between 18 and 65 years old. They also needed to meet criteria for current (criteria met in past year) AD and MD according to the Diagnostic and Statistical Manual of Mental Disorders (4th ed.; DSM–IV; APA, 1994). Exclusion criteria included: current or past psychosis, current or past bipolar disorder, moderate or severe mental retardation, acute suicidal intent requiring emergency intervention, or intravenous drug use in the past year. The final sample included 48 women, 25 of whom received adjunctive IPT, 23 of whom received usual care.
Procedure
Female patients who reported symptoms of depression [defined as total scores ≥ 5 on the Patient Health Questionnaire-9 (PHQ-9; Kroenke, Sptizer, & Williams, 2001)] during their initial intake appointments were referred to the study by staff clinicians. Study staff contacted potential participants and invited them to complete a baseline evaluation to determine their eligibility for the study. Written informed consent was obtained from all participants and the University’s Research Subjects Review Board approved all procedures. Eligible participants were assessed at baseline, post-treatment (16-weeks) and post-treatment follow-up (24-weeks). Participants were paid $20 cash for each assessment they completed. 97.9% (n=47) women participated in the 16 week evaluation and 85.4% (n=41) women participated in the 24 week evaluation.
Measures
Psychiatric Research Interview for Substance and Mental Disorders (PRISM; Hasin, Trautman, Miele, Samet, Smith & Endicott, 1996)
The PRISM is a semi-structured, diagnostic interview that assesses DSM-IV Axis I and II diagnoses. It was administered to establish current (criteria met within the past year) diagnoses of AD and MD, as well as to assess co-morbid drug dependence, PTSD, and borderline personality disorder (BPD). The PRISM also reliably distinguishes between depressive symptoms that are the expected result of intoxication or withdrawal from those that constitute MD, and allows for further classification of MD into primary and substance-induced subtypes. One interviewer conducted all the PRISM interviews, which were then reviewed by the study’s principal investigator (SG).
Difficulties in Emotion Regulation Scale (DERS; Gratz & Roemer, 2004)
The DERS is a 36-item questionnaire comprised of six subscales assessing different aspects of emotion dysregulation, including (1) non-acceptance of emotions (e.g., “When I’m upset, I feel like I am weak”), (2) difficulties engaging in goal-directed behaviors (e.g., “When I’m upset, I have difficulty concentrating”), (3) impulse control difficulties (e.g., “When I’m upset, I feel out of control”), (4) limited access to effective regulatory strategies (e.g., “When I’m upset, it takes me a long time to feel better”), (5) reduced emotional clarity (e.g., “I am confused about how I feel”), and (6) lack of emotional awareness (e.g., “I am attentive to my feelings”, reverse-scored). Participants rate each statement on a 5-point scale ranging from 1 “almost never” to 5 “almost always”. Higher scores reflect greater difficulty in regulating emotions, with a potential range of total score between 36 and 170. For this study, we used the total score (Cronbach’s alpha = .89 at week 16; .90 at baseline), which reflects a continuous measure of the participant’s overall severity of emotion dysregulation.
Beck Depression Inventory-II (BDI-II; Beck, Steer, & Brown, 1996)
This 21-item measure is commonly included in depression treatment trials (Keller, 2003) and has been used to detect changes in depression severity among AD-MD patients (Brown, Evans, Miller, Burgess & Mueller, 1997). The BDI-II assesses the severity of depression symptoms, with each item being rated on a scale from 0 (non-presence of symptom) to 3 (worst severity of symptom) and total score ranging from 0–63. Participants are asked to rate each item as it describes their mood over the past two weeks. The Cronbach’s alpha in the current sample was .89 at baseline and .93 at week 16.
Modified PTSD Symptom Scale (MPSS; Falsetti, Resnick, Resick, & Kilpatrick, 1993)
The MPSS is a 17-item self-report measure of PTSD symptoms over the past two weeks (e.g., “Have you had repeated or intrusive upsetting thoughts or recollections of the event?”). Each item is rated in terms of frequency (“not at all” to “5 or more times per week”), and severity (“not at all distressing” to “extremely distressing”). A total score is calculated by summing all frequency and severity scores, with a total score of 71 or greater and severity score of 47 or higher indicating clinical levels of PTSD symptoms. Cronbach’s alpha = .87, .90, and .94 at baseline and .89, .92, and .95 at week 16 for frequency, severity, and total scales, respectively. The severity subscale of the MPSS was used in the mediation model as it provides a more detailed assessment of the extent to which participants were experiencing symptoms of PTSD.
The Drinker Inventory of Consequences (DrInC; Miller, Tonigan, & Longabaugh, 1995)
The DrInC is a 50-item self-report measure of individuals’ consequences related to alcohol use, independent of an AUD diagnosis. The questions query about potential consequences from drinking over the past 3 months. It includes five subscales representing different areas of consequences, including (1) physical (e.g., “My physical health has been harmed by my drinking”), (2) social responsibility (e.g., “The quality of my work has suffered because of my drinking”), (3) intrapersonal (e.g., “I have felt bad about myself because of my drinking”), (4) impulse control (e.g., “I have taken foolish risks when I have been drinking”), and (5) interpersonal (e.g., “My family has been hurt by my drinking”). Participants rate the frequency with which they have experienced various consequences from drinking, on a 4-point scale ranging from 0 (“never”) to 3 (“daily or almost daily”). Cronbach’s alpha for the subscales ranged from .86 (physical and social responsibility subscales) to .92 (intrapersonal subscale) in this sample. A total consequences score is calculated by summing scores of each subscale (Cronbach’s alpha = .96). Consequences from drinking were used in our analyses as a measure of problem drinking severity in this highly comorbid sample already diagnosed with AD and MD.
Timeline Follow-back Interview (TLFB; Sobell & Sobell, 1996)
The TLFB uses a calendar and other memory aids to determine an individual’s drinking over a specified time period. Using data derived from the TLFB, we calculated each participant’s percent days abstinent (PDA)—a reliable measure of drinking frequency (Babor et al., 1994). At baseline, participants were interviewed about their drinking during the 90 days prior to treatment entry. At 16 weeks, they were interviewed about their drinking during the 16 weeks of treatment. At 24 weeks, participants reported on their drinking during the 8 weeks between the end of treatment and the follow-up interview. The TLFB has excellent reliability (Sobell & Sobell, 1978) and validity for assessing individuals’ alcohol use over time (Sobell, Maisto, Sobell & Cooper, 1980).
Data Analytic Plan
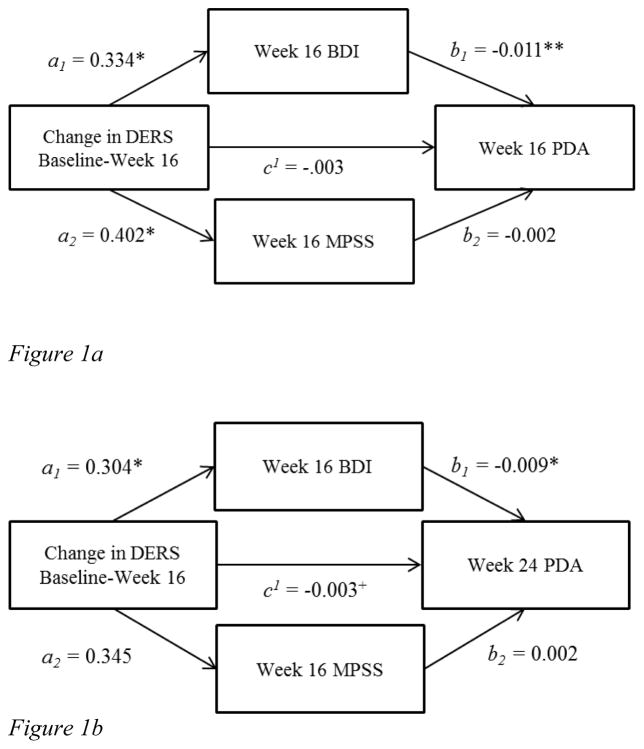
We first ran descriptive statistics in order to examine the rates and nature of comorbidity within this sample, and to examine their level of emotion regulation as a group. Second, we used bivariate correlation analyses to examine the association between emotion regulation, drinking quantity and frequency, alcohol-related consequences, and severity of co-occurring post-traumatic stress and depression. We additionally conducted paired-sample t-tests to examine overall change in our constructs of interest during the treatment period and independent t-tests to compare change between conditions. Two multiple mediation models were run in PROCESS (Hayes, 2012) using IBM SPSS Statistics Version 20. PROCESS provides bootstrapped 95% confidence intervals (95 % CI) for the ab products that are generated in the hypothesized multiple mediation models. Bootstrapped CIs are preferable given (1) the smaller sample size, (2) assumed non-normal distribution of ab products, and (3) the clinical nature of our sample (Hayes, 2013). While normal hypothesis testing assumes that the ab term (the interaction term that is estimated and tested in mediation analyses) is normal, bootstrapping provides an estimated sample distribution which is then used to test significance of the current sample’s data (see Hayes, 2013 for further discussion). The model in Figure 1 was tested, with change in DERS total score from baseline to week 16 as the independent variable (note, lower/negative score represents an improvement in emotion regulation), BDI total score and MPSS severity score as mediating variables, and PDA at week 16 then week 24 as the outcome variable (i.e., the two models differed only in the week of PDA used as the outcome variable). We controlled for treatment condition and baseline scores of PDA, BDI and MPSS. Given the association between emotion regulation and other substance use, and the high rates of co-occurring substance use disorders (SUD, including nicotine) in our sample, we also controlled for co-occurring SUD in these analyses.
Figure 1.
Figure 1a. Results from Mediation Model, Week 16 PDA
Figure 1b. Results from Mediation Model, Week 24 PDA
Note: DERS = Difficulties in Emotion Regulation Scale; BDI = Beck Depression Inventory; MPSS = Modified PTSD Symptom Severity Scale; PDA = Percent Days Abstinent on Timeline Follow-Back; *reflects p<.05; ** p<.01; + reflects significant 95% CI, used to test indirect (mediation) effect
Results
Descriptive Statistics
To examine the presence and severity of co-occurring mental health symptoms and the extent to which emotion dysregulation is heightened in this sample, we first conducted descriptive statistics (see Table 1 for descriptive statistics and demographics). Within this sample of women diagnosed with both AD and MD, there were high percentages of additional comorbid disorders (PTSD, BPD, and additional substance dependence). Seventy-five percent of the sample met criteria for at least one additional diagnosis on the PRISM beyond the MD and AD required for study inclusion. In examining symptom severity of depression and PTSD, at baseline the mean BDI score was 32.6 (SD=10.7) and the mean MPSS severity score was 27.8 (SD=15.6). At 16 weeks, mean BDI was 21.1 (SD=11.5) and MPSS severity score was 22.1 (18.1). With regard to the distribution of self-reported emotion dysregulation, the DERS total score was normally distributed within this sample. However, statistics demonstrated a restricted range and higher average score in this sample (M=97.2, SD = 10.37, range 76–127) when compared to other samples, including healthy college students, at-risk young adult women, and male and female residential substance use treatment patients (Tull, Bardeen, DiLillo, Messman-Moore, & Gratz, 2015; Roemer et al., 2009; Whiteside et al., 2007; Weiss, Tull, Viana, Anestis, & Gratz, 2012; see discussion for details).
Table 1.
Patient Demographics and PRISM diagnoses (n= 48)
| Age [years: mean, (sd)] | 37.4 (11.5) |
| Race [n(%)] | |
| White/Caucasian | 30 (62.5) |
| Black/African American | 15 (31.3) |
| Multiple racial identities | 3 (6.3) |
| Family Status [n(%)] | |
| Never married | 28 (58.3) |
| Married or living with someone | 7 (14.6) |
| Separated or divorced | 13 (27.1) |
| Education [years, mean, (sd)] | 13.4 (2.3) |
| Employment [n(%)] | |
| Unemployed | 37 (77.1) |
| Employed at least part-time or full-time student | 11 (22.9) |
| Household Income [US dollars, median] | $11840.00 |
| Co-occurring conditions [n(%)] | |
| Posttraumatic Stress Disorder | 37 (68.5) |
| Primary Major Depression | 34 (63.0) |
| Substance-Induced Depression | 14 (25.9) |
| Borderline Personality Disorder | 38 (70.4) |
| Current Cannabis, Cocaine, or Opioid Dependence (all same n) | 12 (22.2) |
| Current Nicotine Dependence | 27 (50.0) |
Bivariate Correlations of Baseline Variables of Interest
We then examined bivariate correlations at baseline between emotion dysregulation, drinking variables, and co-occurring PTSD and depression symptoms (Table 2). First, within this sample, higher scores on the DERS (greater emotional dysregulation) were associated with one particular subscale of the DrInC – greater interpersonal consequences. Second, emotion dysregulation was associated directly with drinking frequency, with lower PDA (percent days abstinent) correlating with higher total DERS score. Third, emotion dysregulation was positively associated with severity of mental health symptoms. Total DERS score correlated positively and significantly with PTSD symptoms (total MPSS score and severity subscale), and was marginally associated with depression severity (total BDI score, p=.09). Taken together, results showed that participants’ self-reported high levels of emotion dysregulation, which was associated with a higher frequency of drinking days, more interpersonal consequences from drinking, and more severe PTSD symptoms.
Table 2.
Correlations between variables of interest at baseline (n=48)
| 1 | 2a | 2b | 2c | 3 | 4 | 5 | 5a | 5b | 5c | 5d | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| (1) DERS total | |||||||||||
| (2) MPSS subscales: | |||||||||||
| (a) frequency | .28 | ||||||||||
| (b) severity | .34* | .91** | |||||||||
| (c) total | .32* | .97** | .98** | ||||||||
| (3) BDI | .25 | .20 | .36* | .30* | |||||||
| (4) PDA | −.31* | 0.14 | .05 | .09 | −.21 | −.37* | |||||
| (5) DrInC subscales: | |||||||||||
| (5a) intrapersonal | −.01 | .40** | .48** | .46** | .21 | −.07 | .06 | ||||
| (5b) control | −.03 | .03 | .03 | .03 | .11 | −.14 | −.21 | .42** | |||
| (5c) interpersonal | .38** | .21 | .20 | .20 | −.13 | .32* | −.18 | .23 | .10 | ||
| (5d) physical | −.07 | .32* | .34* | .34* | .12 | −.14 | −.01 | .80** | .56** | .07 | |
| (5e) social responsibility | −.05 | .37* | .38** | .38** | .04 | −.11 | −.04 | .78** | .53** | .17 | .85** |
significant at p<.05,
significant at p<.01;
Note: DERS = Difficulties in Emotion Regulation Scale; MPSS = Modified PTSD Symptom Scale; BDI = Beck Depression Inventory; PDA = Percent days abstinent from alcohol; DrinC = Drinker Inventory of Consequences Scale. See Methods section for more details.
We conducted paired-samples t-tests using bootstrapping to assess mean change in these constructs during treatment (from baseline to week 16). While there was a significant decrease in BDI score (t=6.024, p=.000, 95% CI = (8.30, 15.52) and increase in PDA (t=-5.94, p=.000, 95% CI = (−.35, −.18), there were not significant changes in MPSS total score or in DERS total score. Additionally, independent t-tests examining mean change in the variables (emotion regulation, depression, PTS, and PDA) did not reveal any significant group differences between the two treatment conditions (p>0.05) from baseline to post-treatment.
Multiple Mediation Models
In predicting PDA at week 16, the overall mediation model was significant, R2=.44, F(8, 31)=3.08, p=.01, with 44% of variance in PDA at week 16 accounted for by the proposed predictors (change in emotion regulation over treatment, and depression and PTSD severity scores at week 16). Coefficients for pathways a1, a2, b1, and b2 can be seen in Figure 1a. The change in DERS score during treatment was significantly associated specifically with BDI score at week 16 (a1; p=.01), which was significantly associated with PDA at week 16 (b1; p=.01). The independent mediating effect of depression was significant [95% CI = (−.010, −.001)]. The association between change in DERS score during treatment and MPSS severity score at week 16 was also significant (a2; p=.046), but there was no significant association between MPSS at week 16 and PDA at week 16 (b2; p=.52). These results demonstrate a significant mediating effect of depression score on the relationship between change in emotion regulation and abstinence from alcohol. Although depression was an independently significant mediator, the mediators’ (depression and PTS symptom severity) overall effect was marginally significant, with c1=−.003, [95% CI= −.010, .001)], again suggesting that depression was the significant mediator in this model. For every unit improvement in DERS score over treatment, women were estimated to have a significant .4% increase in their PDA at week 16 via their improved depression and PTSD symptoms (although this effect was primarily accounted for by improved depression). Women who did experience an improvement in emotion regulation over treatment ranged from 1 unit improvement on the DERS (and estimated .4% increase in percent days abstinent at week 16) to 36 unit improvement (with an estimated 14% increase in PDA at week 16). Additionally, the direct effect of change in DERS score on PDA, independent of the effect of the proposed mediators, was a non-significant c’=−.003. This finding reflects that the association between changing emotion regulation and alcohol use was due only to the mediating influences, and primarily the influence of improved depression at week 16.
Because PDA at week 16 coincided with the timeframe for our mediator (i.e., BDI and MPSS scores at week 16) we tested the mediation model reversing the mediator variables (BDI and MPSS scores) and outcome variable (PDA at week 16) to examine whether a change in modeled directionality would affect overall model significance (Hayes, 2013). Results showed that, when PDA at week 16 was entered as the mediator of the relationship between change in emotion regulation and either week 16 MPSS or BDI, the pathway coefficients needed to demonstrate mediation (a1, a2, b1, and b2) were no longer significant. The overall model for the alternative 16 week model switching PDA and MPSS scores was significant, p=.01, but the indirect/mediation effect was not significant (95% CI=−.05, .57). In switching PDA at 16 week and BDI at 16 week, the overall model for the alternative 16 week model was significant, p=.00, but the indirect/mediation effect was not significant (95% CI=−.27, .07)
This finding was further supported by a mediation model with PDA at week 24 as the outcome variable. The overall model was not significant, R2=.32, F(8, 28)=1.63, p=.16, with 32% of variance in PDA at week 24 being accounted for by the predictors (change in emotion regulation, BDI and MPSS scores at week 16). Given that we were particularly interested in the independent mediating effect of each of our variables, we then examined each mediator to test for significance (Hayes, 2013). Coefficients for pathways a1, a2, b1, and b2 can be seen in Figure 1b. The change in DERS score during treatment was significantly associated specifically with BDI score at week 16 (p=.03), which was subsequently significantly associated with PDA at week 24 (p=.02). Change in DERS score during treatment was not significantly associated with MPSS severity score at week 16 (p=.08), and there was no significant association between MPSS at week 16 and PDA at week 24 (p=.56). These findings replicated the results with PDA at week 16 as the outcome; the relationship between change in emotion regulation and PDA at week 24 was significantly mediated by depression at week 16 but not PTSD symptom severity.
The indirect effect of change in emotion regulation through BDI score at week 16 showed that one unit in change on DERS was estimated to differ by .3% PDA at week 24, with those who experience more improvement having greater PDA during follow-up. The indirect effect of BDI alone was a significant mediator of changing DERS score on PDA at week 24 [95% CI = (−.010, −.0001)] and the overall indirect effect of the mediation model was significant [95% CI = (−.013, −.0001)]. Additionally, the direct effect of change in emotion regulation on PDA at week 24 without accounting for the mediators was non-significant (c1 =.001). Thus, results from this second mediation model replicated the findings from the first mediation model, demonstrating that the association between changing emotion regulation and abstinence from alcohol is mediated by co-occurring symptoms, primarily through post-treatment depressive symptoms.
For exploratory reasons, because 26% of the sample had substance-induced major depression, we additionally ran analyses among only those participants with primary depression. Results showed similar results with the 16 week data (overall model p=.02). The independent mediating effect of depression was significant [95% CI = (−.019, −.001)], but that of MPSS severity score was not [95% CI = (−.015, .002)]. Results with 24 week were non-significant [overall model p=.095; independent mediating effect of depression 95% CI = (−.018, .001); independent mediating effect of MPSS severity score 95% CI = (−.001, .014).
Discussion
The goal of this research was to explore the extent to which emotion dysregulation underlies changes in co-occurring depression and PTSD symptom severity and, subsequently, women’s alcohol consumption. We additionally sought to examine the presence and severity of emotion regulation and its association with alcohol use, alcohol-related consequences, and co-occurring symptoms (PTSD and depression symptoms) in a sample of women with co-occurring conditions. Emotion dysregulation, as measured by self-report on the well-validated DERS measure, was significantly higher in this sample when compared with other samples of women and with other individuals with substance use disorders; however this sample also had a more restricted range of scores than other samples. The average score on the DERS in this sample (M=97.2, SD=10.4) was significantly higher than several other samples in which the DERS has been used (t-tests comparing our sample to these others all reflected p<.05): young adult women in a community sample at risk for sexual victimization (M=69.5, SD =21.8; Tull, Bardeen, DiLillo, Messman-Moore, & Gratz, 2015); college students (M=82.12, SD =22.2, Roemer et al., 2009, and M=81.5, SD =20.3, Whiteside et al., 2007); and patients with substance use disorders in residential treatment (M=86.3, SD =26.3, Weiss, Tull, Viana, Anestis, & Gratz, 2012). These other studies had large sample sizes (n range from 106–695) and age ranges (from 18 to 61). Only the first study (Tull et al., 2015) reflects DERS scores in a sample of women only. Therefore, the current sample of women reported greater-than-typical difficulties regulating their negative emotion and demonstrated a more restricted range of emotion dysregulation, in comparison to other clinical and non-clinical samples. This heightened level of emotion dysregulation was undoubtedly influenced by the high percentages of co-occurring mental health conditions – particularly depression and PTSD - conditions with which emotion dysregulation has been associated in past research. Indeed, the high rates of these diagnoses within this sample of women seeking treatment for their alcohol use and co-occurring depression is consistent with what is known of the larger population (e.g., with up to 62% of women with AUDs having a co-occurring mood disorder diagnosis), which helped guide conceptualization of the current study.
Furthermore, varying levels of emotion dysregulation among these women at baseline were directly related to their drinking frequency (percent of days abstinent), number of alcohol-related interpersonal consequences, and severity of PTSD symptoms. The lack of a significant association between emotion dysregulation and depression severity was surprising, as was its non-significant association with other types of alcohol-related consequences. The associations between emotion dysregulation and depression in particular trended toward significance, however, and likely would have been significant in a larger sample. The specific association of emotion dysregulation with interpersonal consequences from alcohol extends prior findings that implicate interpersonal conflict as an especially salient relapse trigger in women with AUD (Lutz, 1991; Greenfield et al., 2007). It is possible that the cyclical effect of alcohol use on interpersonal conflict and vice versa is intensified by poor emotion regulation skills. Women with poorer ability to regulate their emotions after interpersonal conflict in particular may have a harder time controlling their alcohol use. This idea is consistent with research on the importance of emotion regulation in interpersonal contexts (Hofmann, 2014). Emotion dysregulation may be a proximal factor associated not only with PTSD, depression, and alcohol use, but interpersonal functioning as well – independently and as a function of its potentiating effect for the development of co-occurring symptoms such as PTSD and depression.
Results also supported our hypothesis that co-occurring symptoms of depression at the end of treatment (week 16) would mediate the relationship between change in emotion regulation over treatment (from baseline to week 16) and drinking at end of treatment (week 16) and follow-up (percent days abstinent at week 24). While the analyses with depression at week 16 did overlap with the change in emotion regulation variable (only suggesting mediation), the analyses at week 24 are more consistent with a mediation model. The analyses that tested both time points and tested the possibility of a bi-directional relationship between the mediators and outcome drinking provided support that the change in emotion regulation leads to alcohol abstinence through the co-occurring depression symptoms, and not vice versa (that emotion regulation leads directly to alcohol abstinence, which then improves depression symptom severity). More specifically, the effect of emotion regulation changes on depression had the significant mediating impact on drinking, whereas PTSD symptom severity was not a significant predictor when entered with depression as an additional mediator. The results from these analyses are consistent with research that suggests a strong relationship between negative emotion/depression and drinking in women. Research has found mixed results regarding a direct relationship between PTSD and drinking in women, and it has been suggested that the PTSD-alcohol use association may itself be mediated by the depression and negative emotion associated with PTSD (Creech & Borsari, 2014). This is an area for further research. The findings from this study lend support to the association between emotion dysregulation, depression, and alcohol use in women and are consistent with our knowledge of this population so far. Future research on the relationship between emotion dysregulation, PTSD, and alcohol use is needed.
Results of the exploratory mediation models with primary depression only showed similar results with the 16 week data, but the 24 week data showed non-significant results. Research on the therapeutic implications of primary vs. substance-induced depression has not yet fueled definitive conclusions. Research has found that a diagnosis of substance-induced MDD posed a strong risk for relapse after treatment for co-occurring conditions (Samet et al., 2013). Other research has shown that a reduction in drinking during treatment is associated with lower depression regardless of whether it is primary or secondary (Foulds et al., 2015), and that residual depression after treatment is a risk factor for relapse in general (Hasin et al., 2002). We are cautious about interpreting the results of the exploratory analyses, given the unclear implications of primary vs. substance-induced depression, as well as the small sample size after removing participants with substance induced depression; however, these exploratory analyses may be informative for future research on this important topic. The results from this mediation analysis provide support for the idea that emotion dysregulation may be an important construct that evokes change in co-occurring disorders as well as alcohol use.
While research has consistently shown the association between negative emotion and women’s alcohol use, traditional AUD treatment does not directly target regulation of negative emotion and rather focuses on regulating cravings and managing alcohol-related situations. These results suggest that directly targeting co-occurring symptoms and improving emotion regulation skills may have beneficial impact on both co-occurring depressive symptoms as well as decreasing drinking behavior. While not tested in the current study in a detailed fashion, the model was guided by the concept of a transdiagnostic variable - a proximal factor (i.e., emotion dysregulation) that underlies commonly co-occurring conditions of alcohol use and depression and/or PTSD. The current study, despite its limitations as described below, provides preliminary support for the role of emotion dysregulation as a factor that underlies depression and alcohol misuse in women.
Limitations
The results of this study must be considered in light of its limitations. First, this study was conducted with a highly comorbid sample of women and therefore the findings may not apply to other populations including men and/or women with less severe clinical presentations. We also used self-report measures of our constructs of interest, which could be enhanced by additional methods of measurement in future studies. Additionally, we did not explicitly manipulate women’s use of emotion regulation skills so we cannot determine causality, although the longitudinal nature of the project lends some support on this issue.
It is also possible that the non-significant finding for the mediating effect of PTSD symptoms may have been related to the fact that all women in the current study were diagnosed with Major Depression, whereas about 69% were diagnosed with PTSD. In addition, the results could potentially have been impacted by the emphasis of therapy (particularly IPT) on depression. Women did show improvement (albeit, non-significant) in the severity of their PTSD symptoms even though it was not necessarily directly targeted in treatment, and the improvement in emotion regulation was found to predict PTSD symptoms at 16 weeks. Therefore, there were some women who improved in the severity of their PTSD symptoms over the course of the study, which allows us to assess the mediating effect of these symptoms. Additionally, all women received relatively intense treatment as usual (3 times per week), which targeted alcohol misuse and comorbid conditions more generally (including anxiety/PTSD), and not just depression. Since the mediation analyses modeled the effect of changing emotion regulation on depression and PTSD (as opposed to the effect of depression and PTSD as the initial variables in the model), any “unfair advantage” given by the IPT to the significance of depression as a mediator (versus PTSD) may be minimized. The non-significant mediating effect of PTSD found in this study, however, is an area for further research.
Although the results of this study demonstrated significant effects, research would benefit from replication with larger samples. It is important not to over-state our findings especially given our small sample size and significant but small effect sizes. However, post-hoc power analyses did show that our analyses had sufficient power, with the power for our mediation for 16 week at .99 and for the 24 week at .95. Furthermore, while the population of women with AUDs is steadily increasing in size and experiences quite significant disability from their alcohol use, they are less often the focus of research and are more difficult to identify clinically and engage in research. Therefore, despite the smaller sample size, these findings help build on the existing literature on women with AUD and co-occurring conditions.
Conclusions
These results suggest that emotion dysregulation may be an appropriate area for future research in terms of its relevance for treatment of alcohol use in women with significant co-occurring conditions. Indeed, emotion dysregulation is targeted in various treatment approaches, most notably dialectical behavior therapy (DBT, Linehan, 1993) for individuals (primarily women) with BPD. DBT has begun to more directly target substance use behaviors (e.g., Dimeff & Linehan, 2008); however, emotion dysregulation is less frequently directly targeted in treatment for AUDs. Cognitive behavioral therapies (CBT) more broadly have been identified as effective treatments for AUDs (Longabaugh et al., 2005), but it has been argued that current CBT coping and emotion regulation skills are too generic, especially for a comorbid population (Conrod et al., 2000) and may benefit from more elicit focus on regulation of emotion. Such treatments often focus on coping with cravings for alcohol to a greater extent than coping with or regulating negative emotion. Treatment development has begun to focus on efforts to treat co-occurring diagnoses in women (Najavits & Hein, 2013), and the integration of emotion regulation interventions may be an important element of such treatment. Additionally, further experimental research that clarifies the role of emotion regulation in women’s alcohol use would guide development of specific interventions that can be integrated into treatment development efforts.
Table 3.
Regression Coefficients (Coeff), Standard Errors, and Model Summary Information for the Multiple Mediation Model with Week 16 Percent Days Abstinent (PDA) as Outcome Variable
| Antecedent | Consequent | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||
| M1 (BDI wk 16) | M2 (MPSSs wk 16) | Y (PDA wk 16) | Y (PDA wk 16) indirect effect | |||||||||
|
| ||||||||||||
| Coeff | SE | p | Coeff | SE | p | Coeff | SE | p | Coeff | SE | 95% CI | |
| X (Change in DERS) | .334 | .129 | .01 | .402 | .194 | .05 | .004 | .003 | .15 | −.003 | .003 | −.010, .010 |
| M1 (BDI) | -- | -- | -- | -- | -- | -- | −.011 | .004 | .01 | −.004 | .002 | −.010, −.001 |
| M2 (MPSSs) | -- | -- | -- | -- | -- | -- | −.002 | .003 | .52 | −.001 | .001 | −.005, .001 |
| Constant | 15.00 | 8.18 | .08 | −3.86 | 12.32 | .76 | .829 | .174 | .00 | -- | -- | -- |
| R2=.33 | R2=.35 | R2= .44 | ||||||||||
| F(6,33)=2.74, p=.03 | F(6,33)=3.01, p=.02 | F(8,31)=3.08, p=.01 | ||||||||||
Note: DERS = Difficulties in Emotion Regulation Scale; BDI = Beck Depression Inventory; MPSSs = Modified PTSD Symptom Severity Scale; PDA = Percent Days Abstinent on Timeline Follow-Back; Model controlling for Baseline PDA, BDI, MPSS, condition, and Other Substance Use Diagnoses
Table 4.
Regression Coefficients (Coeff), Standard Errors, and Model Summary Information for the Multiple Mediation Model with Week 24 Percent Days Abstinent (PDA) as Outcome Variable
| Antecedent | Consequent | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||
| M1 (BDI wk 16) | M2 (MPSSs wk 16) | Y (PDA wk 24) | Y (PDA wk 24) indirect effect | |||||||||
|
| ||||||||||||
| Coeff | SE | p | Coeff | SE | p | Coeff | SE | p | Coeff | SE | 95% CI | |
| X(Change in DERS) | .304 | .130 | .03 | .345 | .194 | .08 | .000 | .003 | .96 | −.003 | .003 | −.013, −.0001 |
| M1 (BDI) | -- | -- | -- | -- | -- | -- | −.009 | .004 | .02 | −.003 | .002 | −.010, −.0001 |
| M2 (MPSSs) | -- | -- | -- | -- | -- | -- | .002 | .002 | .56 | .005 | .001 | −.001, .005 |
| Constant | 15.34 | 9.16 | .10 | −10.26 | 13.60 | .46 | .736 | .184 | .00 | -- | -- | -- |
| R2= .37 | R2= .40 | R2=.32 | ||||||||||
| F(6,30)=2.90, p=.02 | F(6,30)=3.29, p=.01 | F(8,28)=1.63, p=.16 | ||||||||||
Note: DERS = Difficulties in Emotion Regulation Scale; BDI = Beck Depression Inventory; MPSSs = Modified PTSD Symptom Severity Scale; PDA = Percent Days Abstinent on Timeline Follow-Back; Model controlling for Baseline PDA, BDI, MPSS, condition, treatment condition, and Other Substance Use Diagnoses
Acknowledgments
This study was supported by Grant K23AA017246 from the National Institute on Alcohol Abuse and Alcoholism (NIAAA). The ideas and data appearing in this manuscript have not been previously presented or posted.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. Vol. 4. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- Babor TF, Longabaugh R, Zweben A, Fuller RK, Stout RL, Anton RF, Randall CL. Issues in the definition and measurement of drinking outcomes in alcoholism treatment research. J Stud Alcohol Drugs. 1994;12:S101–S111. doi: 10.15288/jsas.1994.s12.101. [DOI] [PubMed] [Google Scholar]
- Barlow DH, Allen LB, Choate ML. Toward a unified treatment for emotional disorders. BehaviorTherapy. 2004;35:205–230. doi: 10.1080/16506073.2012.748090. [DOI] [Google Scholar]
- Beck AT, Steer RA, Brown GK. Beck Depression Inventory-II (BDI-II) San Antonio, TX: The Psychological Corporation; 1996. [Google Scholar]
- Berking M, Margraf M, Ebert D, Wupperman P, Hofmann S, Junghanns K. Deficits in emotion-regulation skills predict alcohol use during and after cognitive behavioral therapy for alcohol dependence. J Consult Clin Psychol. 2011;79(3):307–318. doi: 10.1037/a0023421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boden MT, Westermann S, McRae K, Kuo J, Alvarez J, Kulkarni MR, Gross JJ, Bonn-Miller MO. Emotion regulation and posttraumatic stress disorder: A prospective investigation. Journal of Social and Clinical Psychology. 2013;32:296–314. doi: 10.1521/jscp.2013.32.3.296. [DOI] [Google Scholar]
- Bonn-Miller MO, Vujanovic AA, Boden MT, Gross JJ. Posttraumatic stress, difficulties in emotion regulation, and coping-oriented marijuana use. Cognitive Behavior Therapy. 2011;40(1):34–44. doi: 10.1080/16506073.2010.525253. [DOI] [PubMed] [Google Scholar]
- Bornovalova MA, Ouimette P, Crawford AV, Levy R. Testing Gender Effects on the Mechanisms Explaining the Association between Post-Traumatic Stress Symptoms and Substance Use Frequency. Addictive Behaviors. 2009;34(8):685–692. doi: 10.1016/j.addbeh.2009.04.005. http://doi.org/10.1016/j.addbeh.2009.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown RA, Evans DM, Miller IW, Burgess ES, Mueller TI. Cognitive-behavioral treatment for depression in alcoholism. J Consulting & Clinical Psychology. 1997;65:715–726. doi: 10.1037//0022-006x.65.5.715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conrod PJ, Stewart SH, Pihl RO, Cote S, Fontaine V, Dongier M. Efficacy of brief coping skills interventions that match different personality profiles of female substance abusers. Psychology of Addictive Behaviors. 2000;14(3):231–242. doi: 10.1037//0893-164x.14.3.231. [DOI] [PubMed] [Google Scholar]
- Creech SK, Borsari B. Alcohol use, military sexual trauma, expectancies, and coping skills in women veterans presenting to primary care. Addictive Behaviors. 2014;39(2):379–385. doi: 10.1016/j.addbeh.2013.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dimeff LA, Linehan MM. Dialectical Behavior Therapy for Substance Abusers. Addiction Science & Clinical Practice. 2008;40:39–47. doi: 10.1151/ascp084239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eftekhari A, Zoellner LA, Vigil SA. Patterns of emotion regulation and psychopathology. Anxiety, Stress & Coping: An International Journal. 2009;22:571–586. doi: 10.1080/10615800802179860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fairholme CP, Nosen EL, Nillni YI, Schumacher JA, Tull MT, Coffey SF. Sleep Disturbance and Emotion Dysregulation as Transdiagnostic Processes in a Comorbid Sample. Behaviour Research and Therapy. 2013;51(9):540–546. doi: 10.1016/j.brat.2013.05.014. http://doi.org/10.1016/j.brat.2013.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Falsetti SA, Resnick HS, Resick PA, Kilpatrick DG. The Modified PTSD Symptom Scale: A brief self-report measure of posttraumatic stress disorder. The Behavior Therapist. 1993;16(6):161–162. [Google Scholar]
- Flynn PM, Brown BS. Co-Occurring Disorders in Substance Abuse Treatment: Issues and Prospects. Journal of Substance Abuse Treatment. 2008;34(1):36–47. doi: 10.1016/j.jsat.2006.11.013. http://doi.org/10.1016/j.jsat.2006.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- GolFoulds JA, Sellman JD, Adamson SJ, Boden JM, Mulder RT, Joyce PR. Depression outcome in alcohol dependent patients: An evaluation of the role of independent and substance-induced depression and other predictors. Journal of Affective Disorders. 2015;174:503–510. doi: 10.1016/j.jad.2014.11.052. [DOI] [PubMed] [Google Scholar]
- Goldstein RB, Dawson DA, Chou SP, Grant BF. Sex differences in prevalence and comorbidity of alcohol and drug use disorders: Results from wave 2 of the National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Studies on Alcohol and Drugs. 2012;73:938–950. doi: 10.15288/jsad.2012.73.938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gratz KL, Roemer L. Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the Difficulties in Emotion Regulation Scale. Journal of Psychopathology and Behavioral Assessment. 2004;26(1):41–54. doi: 10.1023/B:JOBA.0000007455.08539.94. [DOI] [Google Scholar]
- Greenfield SF, Brooks AJ, Gordon SM, Green CA, Kropp F, McHugh RK, … Miele GM. Substance abuse entry, retention, and outcome in women: A review of the literature. Drug and Alcohol Dependence. 2007;86:1–21. doi: 10.1016/j.drugalcdep.2006.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasin D, Trautman K, Miele G, Samet S, Smith M, Endicott J. Psychiatric Research Interview for Substance and Mental Disorders (PRISM): reliability for substance users. American Journal of Psychiatry. 1996;153:1195–1201. doi: 10.1176/ajp.153.9.1195. [DOI] [PubMed] [Google Scholar]
- Hasin D, Liu X, Nunes E. Effects of major depression on remission relapse of substance dependence. Archives of General Psychiatry. 2002;59(4):375–380. doi: 10.1001/archpsyc.59.4.375. [DOI] [PubMed] [Google Scholar]
- Hayes AF. PROCESS: A versatile computational tool for observed variable mediation, moderation, and conditional process modeling (White paper) 2012 Retrieved from http://www.afhayes.com/public/process2012.pdf.
- Hayes AF. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach. New York: The Guilford Press; 2013. [Google Scholar]
- Hofmann SG. Interpersonal Emotion Regulation Model of Mood and Anxiety Disorders. Cognitive Therapy and Research. 2014;38(5):483–492. doi: 10.1007/s10608-014-9620-1. http://doi.org/10.1007/s10608-014-9620-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karpyak VM, Biernacka JM, Geske JR, Abulseoud OS, Brunner MD, Chauhan M, … Mrazek DA. Gender-specific effects of comorbid depression and anxiety on the propensity to drink in negative emotional states. 2016 doi: 10.1111/add.13386. E-pub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keller MB. Past, present, and future directions for defining optimal treatment outcome in depression: remission and beyond. JAMA. 2003;289:3152–3160. doi: 10.1001/jama.289.23.3152. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Crum RM, Warner LA, Nelson CB, Schulenberg J, Anthony JC. Lifetime co-occurrence of DSM-III-R alcohol abuse and dependence with other psychiatric disorders in the national co-morbidity survey. Archives General Psychiatry. 1997;54:313–321. doi: 10.1001/archpsyc.1997.01830160031005. [DOI] [PubMed] [Google Scholar]
- Kring AM, Sloan DM. Emotion Regulation and Psychopathology: A Transdiagnostic Approach to Etiology and Treatment. New York, NY: Guilford Press; 2009. [Google Scholar]
- Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. Journal General Internal Medicine. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lehavot K, Stappenbeck CA, Luterek JA, Kaysen D, Simpson TL. Gender differences in relationships among PTSD severity, drinking motives, and alcohol use in a comorbid alcohol dependence and PTSD sample. Psychology of Addictive Behaviors. 2014;28(1):42–52. doi: 10.1037/a0032266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linehan MM. Cognitive Behavioral Treatment of Borderline Personality Disorder. New York: Guilford Press; 1993. [Google Scholar]
- Longabaugh R, Donovan DM, Karno MP, McCrady BS, Morgenstern J, Tonigan JS. Active ingredients: How and why evidence-based alcohol behavioral treatment interventions work. Alcoholism: Clinical and Experimental Research. 2005;29(2):235–247. doi: 10.1097/01.alc.0000153541.78005.1f. [DOI] [PubMed] [Google Scholar]
- Lutz ME. Sobering decisions: are there gender differences? Alcoholism Treatment Quarterly. 1991;8:51–64. [Google Scholar]
- Miller WR, Tonigan JS, Longabaugh R. The Drinker Inventory of Consequences (DrInC): an instrument for assessing adverse consequences of alcohol abuse. Vol. 4. Rockville, MD: National Institute on Drug Abuse; 1994. (DHHS Publication No 95-3991) Project MATCH Monograph Series. [Google Scholar]
- Moore SA, Zoellner LA, Mollenholt N. Are expressive suppression and cognitive reappraisal associated with stress-related symptoms? Behaviour Research and Therapy. 2008;46:993–1000. doi: 10.1016/j.brat.2008.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Najavits LM, Hien D. Helping vulnerable populations: A comprehensive review of the treatment outcome literature on substance use disorder and PTSD. Journal of Clinical Psychology. 2013;S69:433–479. doi: 10.1002/jclp.21980. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S, Watkins ER. A heuristic for developing transdiagnostic models of psychopathology: explaining multifinality and divergent trajectories. Perspectives on Psychological Science. 2011;66(6):589–609. doi: 10.1177/1745691611419672. [DOI] [PubMed] [Google Scholar]
- Roemer L, Lee JK, Salters-Pedneault K, Erisman SM, Orsillo SM, Mennin DS. Mindfulness and emotion regulation difficulties in generalized anxiety disorder: Preliminary evidence for independent and overlapping contributions. Behavior Therapy. 2009;40(2):142–154. doi: 10.1016/j.beth.2008.04.001. http://doi.org/10.1016/j.beth.2008.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubonis AV, Colby SM, Monti PM, Rohsenow DJ, Gulliver SB, Sirota AD. Alcohol cue reactivity and mood induction in male and female alcoholics. Journal of Studies on Alcohol. 1994;55:487–494. doi: 10.15288/jsa.1994.55.487. [DOI] [PubMed] [Google Scholar]
- Ruiz SM, Oscar-Berman M. Closing the gender gap: The case for gender-specific alcoholism research. Alcoholism & Drug Dependence. 2013;1(6):e106. doi: 10.4172/2329-6488.1000e106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Samet S, Fenton MC, Nunes E, Greenstein E, Aharonovich E, Hasin D. Effects of independent and substance-induced major depressive disorder on remission and relapse of alcohol, cocaine, and heroin dependence. Addiction. 2013;108(1):115–123. doi: 10.1111/j.1360-0443.2012.04010.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB. Timeline followback user’s guide: a calendar method for assessing alcohol and drug use. Toronto, Ontario, Canada: Addiction Research Foundation; 1996. [Google Scholar]
- Sobell LC, Sobell MB. Validity of self-reports in three populations of alcoholics. Journal of Consulting and Clinical Psychology. 1978;46:901–907. doi: 10.1037//0022-006x.46.5.901. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Maisto SA, Sobell MB, Cooper AM. Reliability of alcohol abusers’ self-reports of drinking behavior. Behavior Research and Therapy. 1980;17:157–160. doi: 10.1016/0005-7967(79)90025-1. [DOI] [PubMed] [Google Scholar]
- Stasiewicz PR, Bradizza CM, Schlauch RC, Coffey SF, Gulliver SB, Gudleski GD, Bole CW. Affect regulation training (ART) for alcohol use disorders: Development of a novel intervention for negative affect drinkers. Journal of Substance Abuse Treatment. 2013;45:433–443. doi: 10.1016/j.jsat.2013.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stewart SH, Gavric D, Collins P. Women, Girls, and Alcohol. In: Brady KT, Black SE, Greenfield SF, editors. Women and Addiction: A Comprehensive Handbook. New York: Guilford; 2009. pp. 341–380. [Google Scholar]
- Tull MT, Bardeen JR, DiLillo D, Messman-Moore T, Gratz K. A prospective investigation of the relation between posttraumatic stress symptoms and substance use severity. Journal of Anxiety Disorders. 2015;29:52–60. doi: 10.1016/j.janxdis.2014.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walitzer KS, Dearing RL. Gender differences in alcohol and substance use relapse. Clinical Psychology Review. 2005;26:128–148. doi: 10.1016/j.cpr.2005.11.003. [DOI] [PubMed] [Google Scholar]
- Weiss NH, Tull MT, Viana AG, Anestis MD, Gratz KL. Impulsive behaviors as an emotion regulation strategy: examining associations between PTSD, emotion dysregulation, and impulsive behaviors among substance dependent inpatients. Journal of Anxiety Disorders. 2012;26(3):453–458. doi: 10.1016/j.janxdis.2012.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White A, Castle IJ, Chen CM, Shirley M, Roach D, Hingson R. Converging Patterns of Alcohol Use and Related Outcomes Among Females and Males in the United States, 2002 to 2012. Alcoholism: Clinical and Experimental Research. 2015;39(9):1712–26. doi: 10.1111/acer.12815. [DOI] [PubMed] [Google Scholar]
- Whiteside U, Chen E, Neighbors C, Hunter D, Lo T, Larimer M. Difficulties regulation emotions: Do binge eaters have fewer strategies to modulate and tolerate negative affect? Eating Behaviors. 2007;8:162–169. doi: 10.1016/j.eatbeh.2006.04.001. [DOI] [PubMed] [Google Scholar]
- World Health Organization. Gender disparities in mental health. 2013 Retrieved from http://www.who.int/mental_health/prevention/genderwomen/en/#.