Abstract
Cranioplasty is an in evitable operation conducted after decompressive craniectomy (DC). The primary goals of cranioplasty after DC are to protect the brain, achieve a natural appearance and prevent sinking skin flap syndrome (or syndrome of the trephined). Furthermore, restoring patients' functional outcome and supplementing external defects helps patients improve their self-esteem. Although early cranioplasty is preferred in recent year, optimal timing for cranioplasty remains a controversial topic. Autologous bone flaps are the most ideal substitute for cranioplasty. Complications associated with cranioplasty are also variable, however, post-surgical infection is most common. Many new materials and techniques for cranioplasty are introduced. Cost-benefit analysis of these new materials and techniques can result in different outcomes from different healthcare systems.
Keywords: Cranioplasty, Cost-Benefit analysis, Complications, Cosmetics, Outcome
Introduction
Decompressive craniectomy (DC) is a traditional, classic and evidence-based surgical method for intractable increased intracranial pressure not responding to medical treatments. Cranioplasty after DC with a patient's autologous skull flap is a worldwide practice.5,54) The increase of DC leads to an increase of cranioplasty.12)
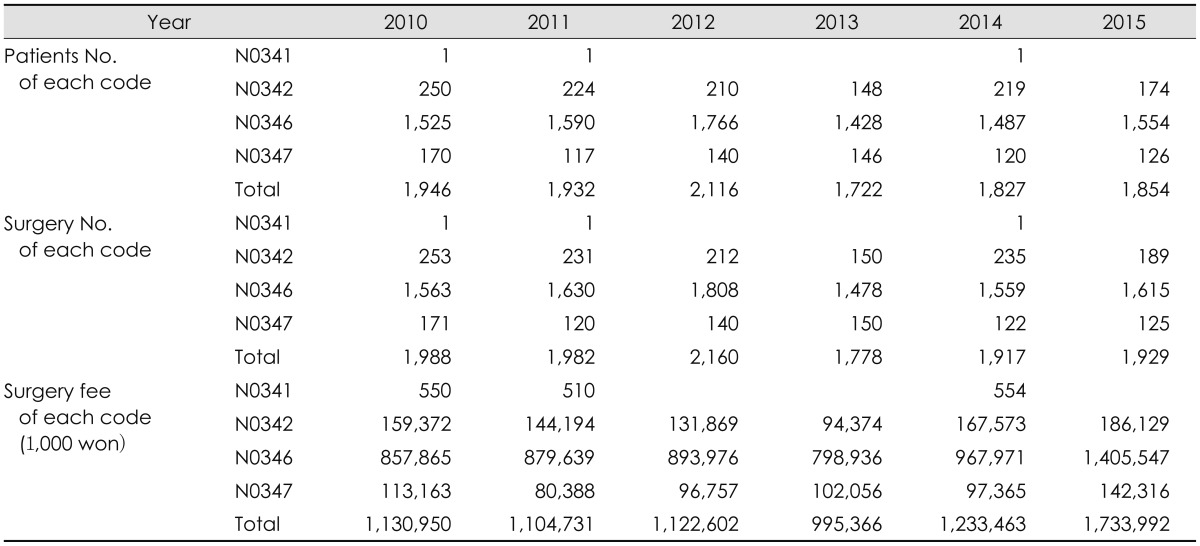
According to the open data from Healthcare Big Data Hub, which is provided from Health Insurance Review and Assessment Service of Republic of Korea, approximately 1,900 patients have received cranioplasty annually between 2010 and 2015 (Table 1).
TABLE 1. Open data of cranioplasty from Healthcare Bigdata Hub which is provided from Health Insurance Review and Assessment Service, Republic of Korea. Cranioplastys for craniosynostosis are excluded. Code N0341 means simple cranioplasty limited in skull, N0342 means cranioplasty including duroplasty, N0346 means relatively simple cranioplasty and N0347 means relatively complex cranioplasty. Surgical fee was increased with phase-out of the selective medical fee in 2014 Jul in Repubic of Korea.
There are many reports about cranioplasty in literatures such as case series, case-control study, cohort studies, clinical trials and complications data. Major topics on cranioplasty are such as complications, surgical timing, surgical technique, free flap preservation methods, new materials and cost-effectiveness. In a few references, there are efforts to provide and support biological basis for cryopreserved bone flaps.7,19,28,41)
In this report, we want to review current information on cranioplasty from the purpose of cranioplasty to the cost-effectiveness of new materials and techniques.
Objectives of Cranioplasty
The reason we should perform cranioplasty after DC is to protect the brain, achieve a natural appearance and prevent sinking skin flap syndrome (or syndrome of the trephined). Furthermore, cranioplasty may improve neuronal function. Many literatures report cranioplasty enhances cerebral glucose metabolism, cerebrovascular reserve capacity, postural blood flow regulation and cerebrospinal fluid circulation.11,12,17)
Optimal Timing of Cranioplasty
The optimal timing for cranioplasty remains a controversial topic.11) One author reported 390.4 days as the mean time between craniectomy and cranioplasty in 2015.39) Some authors have defined “early cranioplasty” as cranioplasty less than 91 days after craniectomy.37,56) In Korea, if the patient's condition is favorable, the timing of cranioplasty can be shortened to less than six weeks following DC.14,53) Optimal timing of cranioplasty is thought to be related with cranioplasty complications. The most important complication of cranioplasty is postoperative infection. There are several risk factors such as operation time exceeding 90 minutes, early cranioplasty, patient's age older than 20 years, female patient, and so on.12) In the past, delayed cranioplasty was considered the optimal timing because it showed a lower infection rate.43) Many authors reported cranioplasty before six months after craniectomy was associated with poor outcomes.43) Tasiou et al.51) reported delayed cranioplasty preference is associated with efforts to decrease postoperative infection, especially for traumatic brain injuries. Recently, several reports recommend early cranioplasty, because it was found that cranioplasty improved clinical outcomes.36,42,47) In the aspect of postoperative infection, multinational prospective designed study says no difference exists of the infection rates between early and delayed cranioplasty.42) In meta-analysis, there was no difference in the chances of developing postoperative infection between early and late cranioplasty.37)
Autologous Skull Flap
Autologous bones are cost-efficient and cosmetically natural.34) In general brain surgeries, skull flaps are usually re-inserted and strong bony fusions between bone flaps is achieved. This is natural because osteogenic, osteoinductive and osteoconductive materials are rich in fresh bone flaps.
Transplanted bone flaps undergo complex healing processes to fuse with surrounding bones.45) Capillary invasion and osteoblasts migration from surrounding bones are important for the bone flap's survival. After re-implantation, no blood is supplied to the bone flap, leading to ischemia. The bone flap is surrounded by blood and an inflammatory response is initiated. Capillaries from surrounding bone, dura and periosteum initiate angiogenesis to the bone flap. As granulation tissue proliferates, capillaries invade the flap. Through the capillary, primitive mesenchymal cells migrate and bone remodeling occurs. Necrotic bone is gradually reabsorbed. If this functional contact between the transplanted flap and surrounding bone is poor, the transplanted flap will be absorbed.45) In animal studies, free skull flaps showed a 50% reduction in volume after re-implantation.18) Similarly, an experimental study on particulate bone on-lay cranioplasty also showed that half of the on-lay graft was resorbed.15)
Fresh skull flaps should be preserved sterilely after DC. There are two methods to make autologous skull flap sterile for cranioplasty: subcutaneous layer placing or cryopreservation.1,4,27,32,38)
As the deep-freezer freezing technique developed, cryopreservation became a more economic and practical method.16) However, there is not a lot of information on how to cryopreserve skull flaps. Bhaskar et al.8) reported 96% of 25 neurosurgical centers in Australia used cryopreserved autologous bone flaps for cranioplasty. In his report, 88% of institutions used double or triple gabbed under dry, sterile conditions for packing bone flaps. The bone flaps were cryopreserved at temperatures between -18℃ and -83℃.8) Biomechanical studies reveal that freezing and thawing have little effect on the mechanical properties of the human skull.54) Sometimes, autoclave or ethylene oxide gas sterilization techniques were used for preventing postoperative infection.26,38,46) However, biological evidence of cryopreserved cranioplasty is obscure. There are few reports on the osteogenic potential of cryopreserved skull flaps. It has been reported that osteoblasts were not cultured from skulls cryopreserved for more than 6 months.7)
Bone Substitute for Cranioplasty
If a skull flap was suspected of contamination, the bone flap would be disposed of. Traumatic brain injuries with a severely contaminated wound or a bacteria-infected wound should undertake delayed cranioplasty with synthetic materials. The ideal synthetic material should be easy to shape and should accurately fit skulls with a cranial defect. The material should be radiolucent enough to avoid formation of artifacts on images and biocompatible to lessen immune response or inflammation. It should be firm and stable, resistant to infection, heat and cold. Finally, it should be economical.3,29)
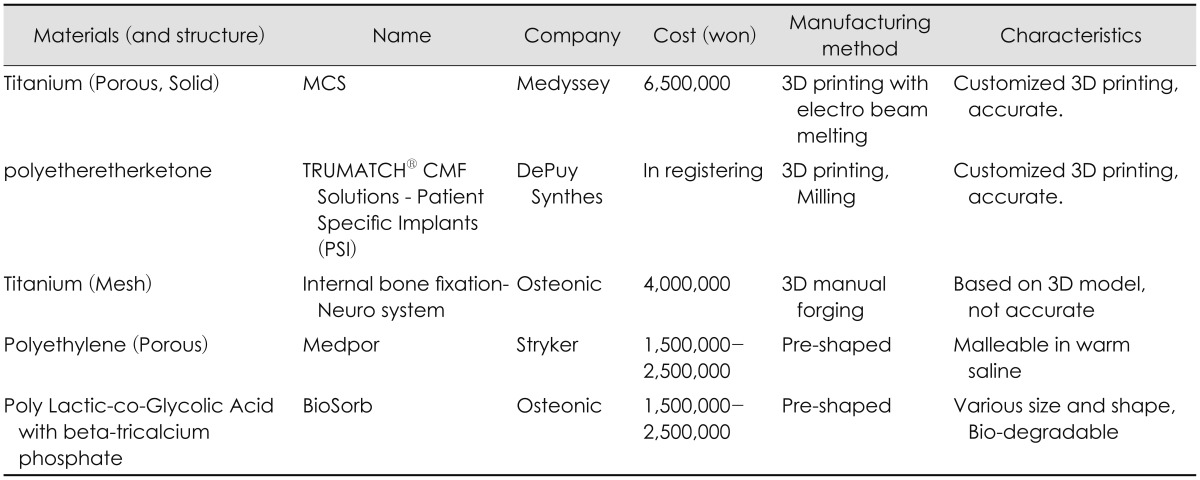
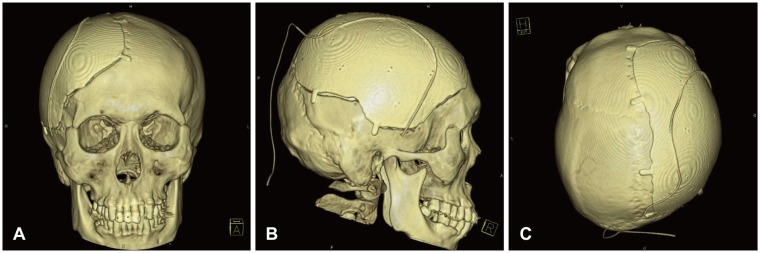
Various materials are used as synthetic materials such as metals (titanium, tantrum etc.), ceramics (calcium phosphate, hydroxyapatite etc.) and polymers (Polymethyl methacrylate [PMMA], polyethylene, poly-ether-ether ketone, poly-ether-ketone-ketone, etc.), bioactive fiber-reinforced composite, demineralized bone matrix and so on.3,9,34,35,39,40) Recently, custom-made prostheses for cranioplasty printed with three-dimensional printers are on market (Table 2, Figure 1).48)
TABLE 2. New materials for cranioplasty available in Korea market.
MCS: microthread collar structure, CMF: craniomaxillofacial, 3D: three-dimensional
FIGURE 1. Brain computed tomography (CT) three-dimensional (3D) reconstructions after cranioplasty with Titanium skull flap. Bone flap is made by 3D printing with electron beam melting technique. Pre-craniectomy brain CT and pre-cranioplasty CT were used for tailored flap. Subgaleal drain catheter is seen above metal flap. (A) Frontal view, (B) Right lateral view, and (C) Apical view.
Special Surgical Considering for Periosteal-dura Mater Dissection
Dissecting the dura mater and the scalp-muscle flap is a difficult process during cranioplasty. Temporalis muscle injury may result in pain and dysfunction of masseteric action. For this reason, some authors support early cranioplasty within one month before adhesion becomes firm. Some authors recommend using anti-adhesives like artificial dura mater or film to facilitate dissection, and some authors recommend new dissection plane.14,21,22)
Antibiotics on Surgical Field
Antibiotics preventing post-cranioplasty infection were used clinically. However, PMMA impregnated with antibiotics, preoperative prophylactic vancomycin for Methicillin-resistant Staphylococcus aureus (MRSA) and prophylactic vancomycin ointment at the cranioplasty site shows low grade evidence.25,43,44,55)
Complications after Cranioplasty
The overall complication rate for cranioplasty after DC was 10% to 40%.2,53) These complications include infections, reoperations, intracranial hemorrhage, extra-axial fluid collection, hydrocephalus, seizures and bone resorptions.37)
The most well-known complications are postoperative surgical infection and bone flap resorption.49) The bone flap infection rate after cranioplasty was 2% to 20%.2,53) Risk factors include long operative times (>120 min), craniectomy with temporalis muscle resection, and presence of preoperative subgaleal fluid collection(s), and postoperative wound disruption.30) Fever, scalp swelling and local inflammations were presented. Imaging study shows extra-axial fluid collection, subgaleal fluid collection, galea swelling, cerebritis, osteomyelitis, and so on.6) In bone flap culture during surgery, primary skin flora such as P. acnes, coagulase-negative staphylococci and S. aureus were cultured.13) However, P. acnes, Escherichia coli, MRSA and S. aureus are among the pathogens identified in surgical site infection (SSI) after cranioplasty.49) Generally, patients that developed SSI were treated with antibiotics following antimicrobial susceptibility testing for 4 to 8 weeks after removal of the implanted bone.
Bone resorption indicates bone tissue resorption by osteoclast, which breaks down bone tissue and releases minerals from bone tissue to the blood.52) Resorption after cranioplasty means decreased bone volume or bone mineral density after autologous cranioplasty. The reported rates were between 2.7% and 44.4%. Computer tomography was used for bone resorption diagnosis. There is a report using computed tomography house field unit scores for resorption diagnosis. Children and large skull flaps, long cryopreservation periods, fragmented flaps and Glasgow Outcome Scale at the time of cranioplasty were reported as risk factors.10,33,37)
Cost Effectiveness of Autologous Skull Flap in Korea
Many researchers emphasize the economic merit of cranioplasty with autologous bone flaps.23,34,35) There are many reports about new substitutes. The difference of the clinical outcome between synthetic materials and autologous bone graft in cranioplasty is very small.34,35,39,40,48) Some authors report lower complication with synthetic materials.8,25,26,27,28) Some reports say the total cumulative cost, including complication risks and treatments, was not significantly different between titanium and autologous bone flaps in United States of America & Canada.24,50) The total average cost of cranioplasty was $25,000 to $29,000 at Canada, reported in 2015.20) The medical environment of each country is different. The surgical fee of cranioplasty and the cost of synthetic materials are also different, even in Korea (Table 1). Following the development of science and industry, the total cost also is becoming more variable.
Up to this time, autologous cryopreserved bone flaps are the most ideal substitute for cranioplasty. Autologous bone flaps are valuable in two aspects. First, biologically cryopreserved skull flaps are the best scaffold for autologous osteoblasts. In the concept of tissue-engineered constructs, cryopreserved skull flaps are filled with osteoconductive and osteoinductive materials, which were completely matched immunologically with the recipient.31) Second, skull flaps are economic; there are no further costs.
Conclusion
Cranioplasty after DC is a familiar surgical process to neurosurgeons. It is an essential surgery not only to satisfy patients' external defects, but also to improve patients' functional outcome. It is probable that many complications will arise because patients are in an immune-compromised state. New synthetic materials and techniques are introduced, and surgical results will also be improved clinically.
Footnotes
This study was supported by BioGreen21 Program (PJ01121401) of Rural Development Administration of ROK. This work was supported by a grant from Hallym University Medical Center Research Fund (HURF 2015-42). We are thankful to Noah Kim who provided expertise that greatly assisted the research.
The authors have no financial conflicts of interest.
References
- 1.Abbott KH. Use of frozen cranial bone flaps for autogenous and homologous grafts in cranioplasty and spinal interbody fusion. J Neurosurg. 1953;10:380–388. doi: 10.3171/jns.1953.10.4.0380. [DOI] [PubMed] [Google Scholar]
- 2.Acciarri N, Palandri G, Cuoci A, Valluzzi A, Lanzino G. Cranioplasty in neurosurgery: is there a way to reduce complications? J Neurosurg Sci. doi: 10.23736/S0390-5616.16.03843-1. [epub ahead of print, 2016.] [DOI] [PubMed] [Google Scholar]
- 3.Arun Kumar KV, Singla NK, Gowda ME, Kumar D, Legha VS. Current Concepts in Restoring Acquired Cranial Defects. J Indian Prosthodont Soc. 2014;14:14–17. doi: 10.1007/s13191-014-0368-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Asano Y, Ryuke Y, Hasuo M, Simosawa S. Cranioplasty using cryopreserved autogenous bone. No To Shinkei. 1993;45:1145–1150. [PubMed] [Google Scholar]
- 5.Barthélemy EJ, Melis M, Gordon E, Ullman JS, Germano IM. Decompressive craniectomy for severe traumatic brain Injury: A systematic review. World Neurosurg. 2016;88:411–420. doi: 10.1016/j.wneu.2015.12.044. [DOI] [PubMed] [Google Scholar]
- 6.Bhaskar IP, Inglis TJ, Lee GY. Clinical, radiological, and microbiological profile of patients with autogenous cranioplasty infections. World Neurosurg. 2014;82:e531–e534. doi: 10.1016/j.wneu.2013.01.013. [DOI] [PubMed] [Google Scholar]
- 7.Bhaskar IP, Yusheng L, Zheng M, Lee GY. Autogenous skull flaps stored frozen for more than 6 months: do they remain viable? J Clin Neurosci. 2011;18:1690–1693. doi: 10.1016/j.jocn.2011.02.046. [DOI] [PubMed] [Google Scholar]
- 8.Bhaskar IP, Zaw NN, Zheng M, Lee GY. Bone flap storage following craniectomy: a survey of practices in major Australian neurosurgical centres. ANZ J Surg. 2011;81:137–141. doi: 10.1111/j.1445-2197.2010.05584.x. [DOI] [PubMed] [Google Scholar]
- 9.Bonda DJ, Manjila S, Selman WR, Dean D. The recent revolution in the design and manufacture of cranial implants: modern advancements and future directions. Neurosurgery. 2015;77:814–824. doi: 10.1227/NEU.0000000000000899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Brommeland T, Rydning PN, Pripp AH, Helseth E. Cranioplasty complications and risk factors associated with bone flap resorption. Scand J Trauma Resusc Emerg Med. 2015;23:75. doi: 10.1186/s13049-015-0155-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Carvi Y, Nievas MN, Höllerhage HG. Early combined cranioplasty and programmable shunt in patients with skull bone defects and CSF-circulation disorders. Neurol Res. 2006;28:139–144. doi: 10.1179/016164106X98008. [DOI] [PubMed] [Google Scholar]
- 12.Chaturvedi J, Botta R, Prabhuraj AR, Shukla D, Bhat DI, Devi BI. Complications of cranioplasty after decompressive craniectomy for traumatic brain injury. Br J Neurosurg. 2016;30:264–268. doi: 10.3109/02688697.2015.1054356. [DOI] [PubMed] [Google Scholar]
- 13.Chiang HY, Steelman VM, Pottinger JM, Schlueter AJ, Diekema DJ, Greenlee JD, et al. Clinical significance of positive cranial bone flap cultures and associated risk of surgical site infection after craniotomies or craniectomies. J Neurosurg. 2011;114:1746–1754. doi: 10.3171/2011.1.JNS10782. [DOI] [PubMed] [Google Scholar]
- 14.Chun HJ, Yi HJ. Efficacy and safety of early cranioplasty, at least within 1 month. J Craniofac Surg. 2011;22:203–207. doi: 10.1097/SCS.0b013e3181f753bd. [DOI] [PubMed] [Google Scholar]
- 15.Clune JE, Mulliken JB, Glowacki J, Arany PR, Kulungowski AM, Rogers GF, et al. Autologous cranial particulate bone graft: an experimental study of onlay cranioplasty. J Craniofac Surg. 2011;22:319–323. doi: 10.1097/SCS.0b013e3181f7e0e2. [DOI] [PubMed] [Google Scholar]
- 16.Elliott H, Scott HJ. The bone-bank in neurosurgery. Br J Surg. 1951;39:31–34. doi: 10.1002/bjs.18003915305. [DOI] [PubMed] [Google Scholar]
- 17.Erdogan E, Duz B, Kocaoglu M, Izci Y, Sirin S, Timurkaynak E. The effect of cranioplasty on cerebral hemodynamics: evaluation with transcranial Doppler sonography. Neurol India. 2003;51:479–481. [PubMed] [Google Scholar]
- 18.Fukuta K, Har-Shai Y, Collares MV, Herschman BR, Persiani RJ, Jackson IT. The viability of revascularized calvarial bone graft in a pig model. Ann Plast Surg. 1992;29:136–142. doi: 10.1097/00000637-199208000-00007. [DOI] [PubMed] [Google Scholar]
- 19.Georgiou K, Fan C, Ng Y, Shandala T, King T, Scherer M, et al. Do cryopreserved autogenous cranial bone flaps remain viable at cranioplasty? Bone. 2010;47:S387–S388. [Google Scholar]
- 20.Gilardino MS, Karunanayake M, Al-Humsi T, Izadpanah A, Al-Ajmi H, Marcoux J, et al. A comparison and cost analysis of cranioplasty techniques: autologous bone versus custom computer-generated implants. J Craniofac Surg. 2015;26:113–117. doi: 10.1097/SCS.0000000000001305. [DOI] [PubMed] [Google Scholar]
- 21.Gordon CR, Fisher M, Liauw J, Lina I, Puvanesarajah V, Susarla S, et al. Multidisciplinary approach for improved outcomes in secondary cranial reconstruction: introducing the pericranial-onlay cranioplasty technique. Neurosurgery. 2014;10(Suppl 2):179–189. doi: 10.1227/NEU.0000000000000296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Griessenauer CJ, He L, Salem M, Chua M, Ogilvy CS, Thomas AJ. Epidural bovine pericardium facilitates dissection during cranioplasty: A technical note. World Neurosurg. 2015;84:2059–2063. doi: 10.1016/j.wneu.2015.08.009. [DOI] [PubMed] [Google Scholar]
- 23.Hayward RD. Cranioplasty: don't forget the patient's own bone is cheaper than titanium. Br J Neurosurg. 1999;13:490–491. [PubMed] [Google Scholar]
- 24.Honeybul S, Morrison DA, Ho KM, Lind CR, Geelhoed E. A randomized controlled trial comparing autologous cranioplasty with custom-made titanium cranioplasty. J Neurosurg. 2017;126:81–90. doi: 10.3171/2015.12.JNS152004. [DOI] [PubMed] [Google Scholar]
- 25.Ikeda H, Kurisu K, Kihira K. Vancomycin ointment for MRSA infection at a cranioplasty site. Ann Pharmacother. 2004;38:70–72. doi: 10.1345/aph.1D178. [DOI] [PubMed] [Google Scholar]
- 26.Jho DH, Neckrysh S, Hardman J, Charbel FT, Amin-Hanjani S. Ethylene oxide gas sterilization: a simple technique for storing explanted skull bone. Technical note. J Neurosurg. 2007;107:440–445. doi: 10.3171/JNS-07/08/0440. [DOI] [PubMed] [Google Scholar]
- 27.Joaquim AF, Mattos JP, Chaddad F, de Oliveira E. Bone flap management in neurosurgery. Rev Neurociências. 2009;17:133–137. [Google Scholar]
- 28.Kaku M, Koseki H, Kojima S, Sumi H, Shikata H, Kojima S, et al. Cranial bone regeneration after cranioplasty using cryopreserved autogenous bone by a programmed freezer with a magnetic field in rats. Cryo Letters. 2014;35:451–461. [PubMed] [Google Scholar]
- 29.Khader BA, Towler MR. Materials and techniques used in cranioplasty fixation: A review. Mater Sci Eng C Mater Biol Appl. 2016;66:315–322. doi: 10.1016/j.msec.2016.04.101. [DOI] [PubMed] [Google Scholar]
- 30.Kim H, Sung SO, Kim SJ, Kim SR, Park IS, Jo KW. Analysis of the factors affecting graft infection after cranioplasty. Acta Neurochir (Wien) 2013;155:2171–2176. doi: 10.1007/s00701-013-1877-8. [DOI] [PubMed] [Google Scholar]
- 31.Kuleshova LL, Gouk SS, Hutmacher DW. Vitrification as a prospect for cryopreservation of tissue-engineered constructs. Biomaterials. 2007;28:1585–1596. doi: 10.1016/j.biomaterials.2006.11.047. [DOI] [PubMed] [Google Scholar]
- 32.Lee BS, Min KS, Lee MS, Kim YG, Kim DH. Comparison with subcutaneous abdominal preservation and cryoconservation using autologous bone flap after decompressive craniectomy. Korean J Neurotrauma. 2012;8:21–25. [Google Scholar]
- 33.Lee SH, Yoo CJ, Lee U, Park CW, Lee SG, Kim WK. Resorption of autogenous bone graft in cranioplasty: Resorption and reintegration failure. Korean J Neurotrauma. 2014;10:10–14. doi: 10.13004/kjnt.2014.10.1.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lemée JM, Petit D, Splingard M, Menei P. Autologous bone flap versus hydroxyapatite prosthesis in first intention in secondary cranioplasty after decompressive craniectomy: a French medico-economical study. Neurochirurgie. 2013;59:60–63. doi: 10.1016/j.neuchi.2012.10.138. [DOI] [PubMed] [Google Scholar]
- 35.Lethaus B, Bloebaum M, Koper D, Poort-Ter Laak M, Kessler P. Interval cranioplasty with patient-specific implants and autogenous bone grafts--success and cost analysis. J Craniomaxillofac Surg. 2014;42:1948–1951. doi: 10.1016/j.jcms.2014.08.006. [DOI] [PubMed] [Google Scholar]
- 36.Liang W, Xiaofeng Y, Weiguo L, Gang S, Xuesheng Z, Fei C, et al. Cranioplasty of large cranial defect at an early stage after decompressive craniectomy performed for severe head trauma. J Craniofac Surg. 2007;18:526–532. doi: 10.1097/scs.0b013e3180534348. [DOI] [PubMed] [Google Scholar]
- 37.Malcolm JG, Rindler RS, Chu JK, Grossberg JA, Pradilla G, Ahmad FU. Complications following cranioplasty and relationship to timing: A systematic review and meta-analysis. J Clin Neurosci. 2016;33:39–51. doi: 10.1016/j.jocn.2016.04.017. [DOI] [PubMed] [Google Scholar]
- 38.Osawa M, Hara H, Ichinose Y, Koyama T, Kobayashi S, Sugita Y. Cranioplasty with a frozen and autoclaved bone flap. Acta Neurochir (Wien) 1990;102:38–41. doi: 10.1007/BF01402184. [DOI] [PubMed] [Google Scholar]
- 39.Piitulainen JM, Kauko T, Aitasalo KM, Vuorinen V, Vallittu PK, Posti JP. Outcomes of cranioplasty with synthetic materials and autologous bone grafts. World Neurosurg. 2015;83:708–714. doi: 10.1016/j.wneu.2015.01.014. [DOI] [PubMed] [Google Scholar]
- 40.Plum AW, Tatum SA. A comparison between autograft alone, bone cement, and demineralized bone matrix in cranioplasty. Laryngoscope. 2015;125:1322–1327. doi: 10.1002/lary.25158. [DOI] [PubMed] [Google Scholar]
- 41.Prolo DJ, Burres KP, McLaughlin WT, Christensen AH. Autogenous skull cranioplasty: fresh and preserved (frozen), with consideration of the cellular response. Neurosurgery. 1979;4:18–29. doi: 10.1227/00006123-197901000-00005. [DOI] [PubMed] [Google Scholar]
- 42.Quah BL, Low HL, Wilson MH, Bimpis A, Nga VD, Lwin S, et al. Is there an optimal time for performing cranioplasties? Results from a prospective multinational study. World Neurosurg. 2016;94:13–17. doi: 10.1016/j.wneu.2016.06.081. [DOI] [PubMed] [Google Scholar]
- 43.Rish BL, Dillon JD, Meirowsky AM, Caveness WF, Mohr JP, Kistler JP, et al. Cranioplasty: a review of 1030 cases of penetrating head injury. Neurosurgery. 1979;4:381–385. doi: 10.1227/00006123-197905000-00002. [DOI] [PubMed] [Google Scholar]
- 44.Ronderos JF, Wiles DA, Ragan FA, Dempesy CW, Culicchia FC, Fontana CJ, et al. Cranioplasty using gentamicin-loaded acrylic cement: a test of neurotoxicity. Surg Neurol. 1992;37:356–360. doi: 10.1016/0090-3019(92)90003-6. [DOI] [PubMed] [Google Scholar]
- 45.Shaffrey ME, Persing JA, Shaffrey CI. Craniofacial reconstruction. In: Apuzzo MLJ, editor. Brain surgery: Complication avoidance and management. New York, NY: Churchill Livingstone; 1993. pp. 1373–1398. [Google Scholar]
- 46.Son S, Park CW, Kim EY, Kim JM, Yoo CJ. Bone resorption of autologous cranioplasty following decompressive craniectomy in children: case report. J Korean Neurotraumatol Soc. 2009;5:118–123. [Google Scholar]
- 47.Songara A, Gupta R, Jain N, Rege S, Masand R. Early cranioplasty in patients with posttraumatic decompressive craniectomy and its correlation with changes in cerebral perfusion parameters and neurocognitive outcome. World Neurosurg. 2016;94:303–308. doi: 10.1016/j.wneu.2016.07.003. [DOI] [PubMed] [Google Scholar]
- 48.Stefini R, Zanotti B, Nataloni A, Martinetti R, Scafuto M, Colasurdo M, et al. The efficacy of custom-made porous hydroxyapatite prostheses for cranioplasty: evaluation of postmarketing data on 2697 patients. J Appl Biomater Funct Mater. 2015;13:e136–e144. doi: 10.5301/jabfm.5000211. [DOI] [PubMed] [Google Scholar]
- 49.Sundseth J, Sundseth A, Berg-Johnsen J, Sorteberg W, Lindegaard KF. Cranioplasty with autologous cryopreserved bone after decompressive craniectomy: complications and risk factors for developing surgical site infection. Acta Neurochir (Wien) 2014;156:805–811. doi: 10.1007/s00701-013-1992-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Takeuchi H, Higashino Y, Hosoda T, Yamada S, Arishima H, Kodera T, et al. Long-term follow-up of cryopreservation with glycerol of autologous bone flaps for cranioplasty after decompressive craniectomy. Acta Neurochir (Wien) 2016;158:571–575. doi: 10.1007/s00701-015-2679-y. [DOI] [PubMed] [Google Scholar]
- 51.Tasiou A, Vagkopoulos K, Georgiadis I, Brotis AG, Gatos H, Fountas KN. Cranioplasty optimal timing in cases of decompressive craniectomy after severe head injury: a systematic literature review. Interdiscip Neurosurg. 2014;1:107–111. [Google Scholar]
- 52.Teitelbaum SL. Bone resorption by osteoclasts. Science. 2000;289:1504–1508. doi: 10.1126/science.289.5484.1504. [DOI] [PubMed] [Google Scholar]
- 53.The Korean Neurosurgical Society. Neurosurgery. ed 4th. Seoul: The Korean Neurosurgical Society; 2012. [Google Scholar]
- 54.Torimitsu S, Nishida Y, Takano T, Koizumi Y, Hayakawa M, Yajima D, et al. Effects of the freezing and thawing process on biomechanical properties of the human skull. Leg Med (Tokyo) 2014;16:102–105. doi: 10.1016/j.legalmed.2013.11.005. [DOI] [PubMed] [Google Scholar]
- 55.Worm PV, do Nascimento TL, do Couto Nicola F, Sanches EF, Dos Santos Moreira CF, Rogerio LP, et al. Polymethylmethacrylate imbedded with antibiotics cranioplasty: An infection solution for moderate and large defects reconstruction? Surg Neurol Int. 2016;7:S746–S751. doi: 10.4103/2152-7806.193725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Xu H, Niu C, Fu X, Ding W, Ling S, Jiang X, et al. Early cranioplasty vs. late cranioplasty for the treatment of cranial defect: A systematic review. Clin Neurol Neurosurg. 2015;136:33–40. doi: 10.1016/j.clineuro.2015.05.031. [DOI] [PubMed] [Google Scholar]