Summary
Introduction.
Obesity is a major risk factor for type 2 diabetes mellitus (T2DM). Clinical evidence indicates a stronger association of diabetes with central obesity than general obesity. The present study aimed to compare the association between type 2 diabetes mellitus and different anthropometric measurements and evaluate the usefulness of these measurements in clinical practice.
Methods.
A case-control study was done among 102 individuals; of whom 51 cases included diagnosed T2DM (≥ 20 years age) patients attending the Medicine out-patient consultation of a tertiary care hospital and 51 controls who were screen negative for T2DM and recruited from the local community. Various anthropometric measurements were used according to standard World Health Organization (WHO) protocols. Data was entered and analyzed using Statistical Package for Social Sciences (SPSS) version 15.
Results.
The proportion of cases with Body Mass Index (BMI) ≥ 25 kg/m2 was 55% as compared to 22% of controls and this association was statistically significant (p < 0.05). The proportion of cases with high waist circumference cut-offs (WC) was 74.5% as compared to 45.1% healthy individuals and this association was also statistically significant (p < 0.05, OR = 3.56). A Receiver Operating Characteristic (ROC) curve for both gender revealed highest area under the curve for body mass index (area = 0.787). Body mass index had the best discriminatory power. Waist to hip ratio was not a sensitive marker especially for females.
Conclusions.
A strong association between obesity indices and diabetes was identified. BMI and WC could be used in clinical practice for suggesting life style modifications.
Key words: Type 2 diabetes mellitus, Obesity, Body mass index, Waist circumference, Case control study, ROC curve
Introduction
Diabetes is a major global health problem which the world is facing today. India is regarded as the diabetic capital of the world [1]. The emergence of type 2 diabetes mellitus (T2DM) in India, coinciding with the country's rapid economic development in the past several decades, is often characterized as a modern epidemic resulting directly from westernization [2]. The severity of the present situation in the Indian context can be judged from the alarming figures wherein, diabetes was directly responsible for 109,000 deaths, 1,157 years of life lost and 2,263 disability adjusted life years, in the year 2004 [3]. One of the major risk factor for T2DM is obesity. Clinical evidence indicates a stronger association of diabetes with central obesity than general obesity [4]. There are 380 million people in the world expected to have diabetes by 2025 [5]. In spite of a relatively lower rate of obesity as defined by Body Mass Index (BMI) cut points, South Asians tend to have larger waist measurements and waist-to-hip ratios (WHR), indicating a greater degree of central body obesity [6]. This is associated with a characteristic metabolic profile with higher insulin levels, a greater degree of insulin resistance, and a higher prevalence of diabetes [6]. Over the next 10 years in India deaths from chronic disease will increase by 18% - most markedly, deaths from diabetes will increase by 35% [7]. Simple anthropometric measurements have been used as surrogate measurements of obesity and have more practical value in both clinical practice and for large-scale epidemiological studies [8]. BMI is a simple method which is used to calculate the prevalence of overweight and obesity in the population. Waist circumference (WC) is the best measure of both intra-abdominal fat mass and total fat [8]. But BMI can be misleading, such as in individuals with a high proportion of lean muscle mass [9]. WC, a more accurate measure of the distribution of body fat, has been shown to be more strongly associated with morbidity and mortality [9]. Recently, the waist-to-stature ratio (WSR) has been proposed as a better screening tool than WC and BMI for adult metabolic risk factors [10]. The present study is aimed to compare the association between T2DM and different anthropometric measurements and evaluate the practicability and usefulness of these measurements in clinical practice and public health.
Methods
This was a case control study comprising of 51 cases prospectively recruited from the hospital and 51 controls also recruited prospectively from the local community (Case control in the ratio of 1:1). Institutional ethical committee clearance was obtained (IEC 123/2014) before the initiation of the study. Written informed consent was obtained from all the study subjects. Information pertaining to socio-demographic characteristics and anthropometric measurements was collected by personal interviews using a pre-designed questionnaire.
CASES: PATIENTS WITH TYPE 2 DIABETES MELLITUS - HOSPITAL
Cases were recruited from a tertiary care referral hospital in South India. Cases were the patients diagnosed with T2DM attending the tertiary care referral hospital. Inclusion criteria for cases was, age ≥ 20 years of both gender diagnosed with T2DM at least since two years, willing to participate and attending the Out Patient Department (OPD) clinic of Department of Medicine at the tertiary care referral hospital. Patients of T2DM having severe co-morbidities like stroke, chronic renal diseases and chronic lung diseases at the time of recruitment into the study; referred patients to the medicine OPD who came to the hospital due to other illness and pregnant females were excluded from the study. Cases were interviewed in the hospital and additional details about investigations, complications, etc. were obtained from OPD patient records for cases.
CONTROLS: SCREEN NEGATIVE FOR DIABETES - COMMUNITY
Controls were the individuals not having T2DM, selected from the community in the field practice area of Department of Community Medicine. Controls were defined as individuals' ≥ 20 years of both gender, willing to participate and who were not suffering from type 2 diabetes mellitus. Diabetes was ruled out by screening the participants at the time of enrolment into the study by random blood glucose (RBS) estimation using a glucometer (Accu-Chek Active Blood Glucose Monitoring System). Subjects with RBS < 7.8 mmol/l [11] were eligible to be included as controls. Controls were approached by house to house survey in the field practice area of Department of Community Medicine, Kasturba Medical College, Manipal, which is operational for the last 50 years, and covers a population of 50,000.
Blood pressure was measured for all subjects in the study using a standardized mercury sphygmomanometer in the right arm in sitting posture. If the recorded blood pressure is ≥ 140/90 mm Hg (18.6/11.9 KPa), repeat blood pressure reading was taken after five minutes.
STATISTICAL ANALYSIS
Data was entered and analysed using Statistical Package for Social Sciences (SPSS) version 15 (SPSS Inc, Chicago, IL, USA) for Windows. Sample size was calculated by anticipating standard deviation of 0.09 and difference of 0.05 in WHR to be significant for power of 80% and 95% confidence interval, 51 cases and 51 controls (1:1 ratio) were recruited, group matched for gender.
All the variables were measured according to World Health Organization (WHO) guidelines and quality control was maintained during collection of data [12]. All the measurements were taken over light clothing. Weight was measured by mechanical weighing scale in kilograms to the nearest 0.5 kg, without footwear with the scale being placed on a firm flat surface. Height was measured by a measuring tape against a flat vertical surface and recorded in centimetres, to the nearest 0.1 cm. Waist circumference was measured by a measuring tape and recorded in centimetres, to the nearest 0.1 cm, at the mid-point between coastal margin and iliac crest. Hip circumference was measured by a measuring tape and recorded in centimetres, to the nearest 0.1 cm, at the level of maximum circumference of the ischial tuberosity of the participant.
The following ratios were calculated:
WHR: waist circumference (cm)/hip circumference (cm);
WSR: waist circumference (cm)/Height (cm);
BMI: weight (kg)/height (m2).
CRITERIA FOR DEFINING OBESITY
BMI ≥ 25 kg/m2 - overweight and BMI ≥ 30 kg/m2 - obese [13].
WSR ≥ 0.90 for males and ≥ 0.85 for females (truncal obesity) [14].
WC > 90 cm in males and > 80 cm in females (central/ abdominal obesity) [14].
WSR > 0.5 [10].
Blood pressure was classified according to Joint National Committee VII (JNC VII) criteria [15].
Results
The study included 51 cases and 51 controls. Socio-demographic details of cases and controls were similar as depicted in Table I. The cases and controls were group matched by gender. Nearly 70% of cases belonged to age group of 40-59 years, while controls constituted 45% in the same age bracket. Hinduism being the predominant faith followed in the entire country is reflected in the study area too. Nearly one third of the population (37.3%) was illiterate among the cases, while control population in the community was more literate (86%).
Tab. I.
Socio-demographic characteristics of the study population.
| Demographic characteristics |
Cases (n = 51) n (%) |
Controls (n = 51) n (%) |
|---|---|---|
| Age group (years) 20-39 40-59 ≥ 60 |
1 (2) 35 (68.6) 15 (29.4) |
19 (37.2) 23 (45.1) 9 (17.6) |
| Gender Male Female |
25 (49) 26 (51) |
26 (51) 25 (49) |
| Religion Hindu Sikh Christian |
48 (94.1) 0 (0) 3 (5.9) |
50 (98.0) 1 (2) 0 (0) |
| Education Graduate and above Elementary (1st to 12th Class) Illiterate |
6 (11.8) 26 (50.9) 19 (37.3) |
1 (2) 43 (84.3) 7 (13.7) |
| Occupation Professional/White collared Business Skilled Semiskilled Coolie/Unskilled Not currently employed |
1 (2) 2 (3.9) 13 (25.5) 2 (3.9) 2 (3.9) 31 (60.8) |
1 (2) 8 (15.7) 14 (27.5) 1 (2) 1 (2) 26 (51) |
| Marital Status Married Unmarried |
51 (100) 0 (0) |
48 (94.1) 3 (5.9) |
| Socio-economic status Low Middle High |
16 (31.4) 30 (58.8) 5 (9.8) |
12 (23.5) 39 (76.5) 0 (0) |
The distribution of various occupation categories among cases and controls was similar. Over half of the study population belonged to the middle socio-economic category as per the modified Udai-Parikh scale used for socio- economic status assessment. The scale uses a scoring pattern based on household possessions, education and occupation of the eldest member of the family.
Among 75% of the subjects, the duration of diabetes was less than ten years. Among the cases, 63% were being treated only by oral hypoglycaemic agents while 31% were both on insulin and oral hypoglycaemic agents. Hypertension (37%) was the most common co-morbidity among the cases as documented in the records. None of the diabetic subjects had their blood glucose levels within the suggested normal limits, as per the tests-fasting blood sugar (FBS), post prandial blood sugar (PPBS), random blood sugar (RBS) and glycated haemoglobin (HbA1c) mentioned in the patient records.
According to BMI categories (Tab. II) the proportion of cases with BMI ≥ 25 kg/m2 among cases was 55% as compared to controls among whom only 21.6% individuals had BMI ≥ 25 kg/m2 and this association was found to be statistically significant, with the odds being highest when BMI was ≥ 30 (p < 0.05).
Tab. II.
Association between anthropometric variables among cases and controls.
| Anthropometric variables | Cases n (%) |
Controls n (%) |
Chi-square value |
p value | Odds ratio | 95%CI |
|---|---|---|---|---|---|---|
| BMI category (Kg/m2) Underweight (< 18.5) Normal (18.5-24.99) Overweight (≥ 25) Obese (≥ 30) |
3 (5.9) 20 (39.2) 14 (27.5) 14 (27.5) |
14 (27.5) 26 (51) 8 (15.7) 3 (5.9) |
16.65 |
0.001 |
0.27 1.00 2.27 6.06 |
0.07-1.10 0.79-6.47 1.53-24.03 |
| WC Normal Abnormal (M ≥ 90 cm) (F ≥ 80 cm) |
13 (25.5) 38 (74.5) |
28 (54.9) 23 (45.1) |
9.18 |
0.002 |
1.00 3.56 |
1.54 -8.22 |
| WHR Normal Abnormal (M ≥ 0.90) (F ≥ 0.85) |
9 (17.6) 42 (82.4) |
10 (19.6) 41 (80.4) |
0.06 |
0.799 |
1.00 1.14 |
0.42-3.08 |
| WSR Normal Abnormal (> 0.5) |
6 (11.8) 45 (88.2) |
18 (35.3) 33 (64.7) |
7.84 |
0.005 |
1.00 4.09 |
1.46-11.42 |
The proportion of cases with more than normal waist circumference (Tab. II) was 74.5% as compared to 45.1% healthy individuals and this association was also found to be statistically significant (p < 0.05). Statistically significant association was also noted with WSR, but not with waist hip ratio (Tab. III).
Tab. III.
Cut-off values, sensitivity and specificity for different anthropometric measures.
| Anthropometric measure | Cut-off value | Sensitivity | Specificity |
|---|---|---|---|
| BMI | 21.85 | 82% | 65% |
| WC | 89.75 | 70% | 65% |
| WHR | 0.94 | 60% | 53% |
| WSR | 0.54 | 74% | 57% |
BMI and WC were identified to have good sensitivity and specificity irrespective of gender (Tabs. IV, V).
Tab. IV.
Cut-off values, sensitivity and specificity for different anthropometric measures among males
| Anthropometric measure | Cut-off value | Sensitivity | Specificity |
|---|---|---|---|
| BMI | 22.07 | 76% | 66% |
| WC | 91.25 | 76% | 74% |
| WHR | 0.95 | 72% | 54% |
| WSR | 0.54 | 76% | 62% |
Tab. V.
Cut-off values, sensitivity and specificity for different anthropometric measures among females.
| Anthropometric measure | Cut-off value | Sensitivity | Specificity |
|---|---|---|---|
| BMI | 22.28 | 80% | 68% |
| WC | 83.5 | 73% | 60% |
| WHR | 0.94 | 46% | 48% |
| WSR | 0.54 | 73% | 56% |
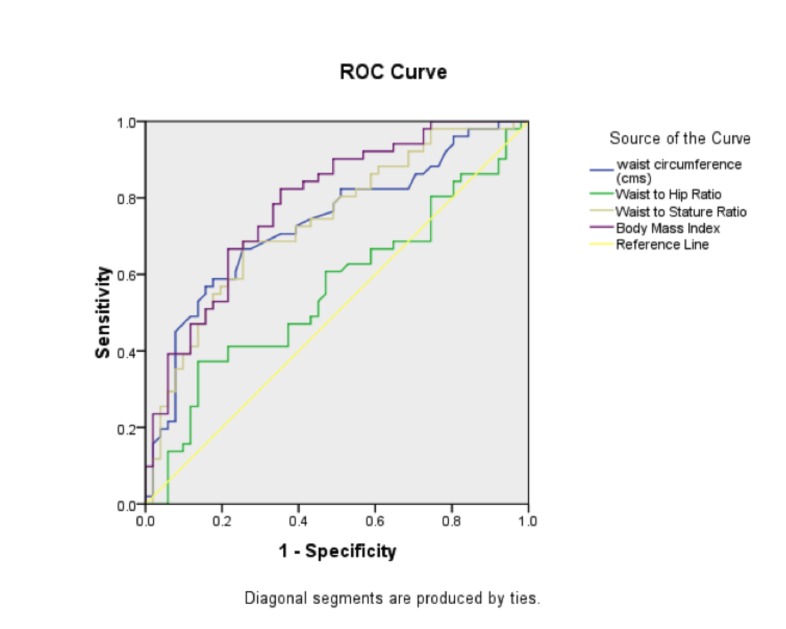
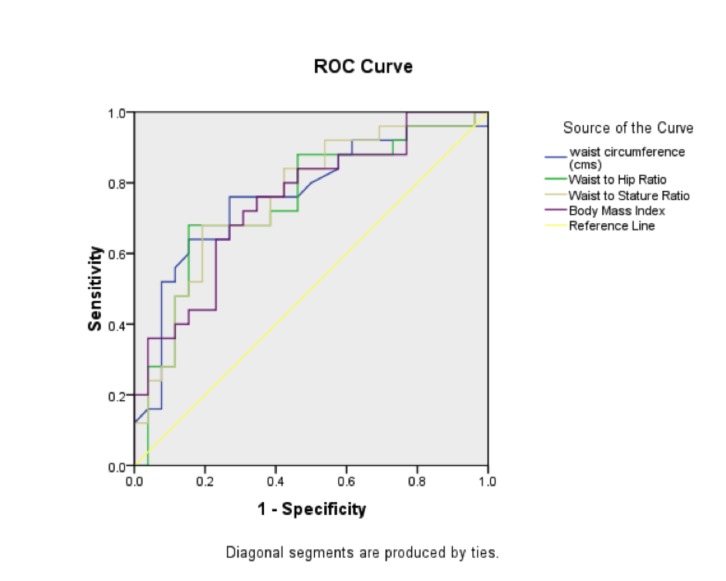
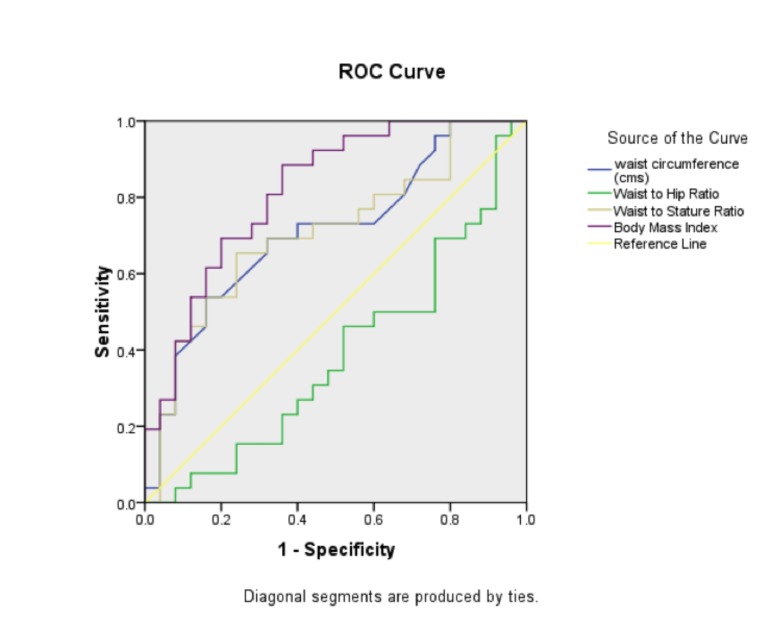
The area under the curve for BMI, WC and WSR was 0.787, 0.734 and 0.737 respectively (Fig. 1) as per the Receiver Operator Characteristics (ROC) curve analysis for both gender. Among males (Fig. 2) all the anthropometric measures were found to have similar sensitivity, while among the females (Fig. 3) BMI was found to be the most sensitive marker fo rT2DM (Area = 0.818). WC and WSR were also good in assessing the risk of diabetes. WHR was not found to be suitable marker for T2DM among females.
Fig. 1.
ROC curve for both gender.
Fig. 2.
ROC curve for males.
Fig. 3.
ROC curve for females.
Discussion
The present study identified WC, WSR and BMI to be associated with T2DM than WHR. The odds of a diabetic individual having high waist circumference was 3.56 times more as compared to a non-diabetic individual.
Different anthropometric cut-off values for various ethnic groups and populations, always makes comparisons difficult and limits generalizability. In most of the studies BMI performed poorly as an anthropometric predictor for T2DM which was in contrast to the present study where BMI was found to be the sensitive marker for diabetes and especially among females. In the Uppsala study [16] they concluded that overweight (BMI 25- 30 kg/m2) or obese men (BMI 30 kg/m2) without metabolic syndrome were at increased risk for diabetes which were comparable with our results. In the present study, WHR was not a sensitive marker for T2DM. But there are contrasting views on this anthropometric measure in literature [1, 17].
WC was found to be a significant predictor of T2DM in a systematic review [18] and a prospective cohort study [19] which was concurring with the present study findings. Results from a systematic review [10] and a multi ethnic cohort study [20] identified WSR to be a more useful clinical screening tool similar to the present study.
The present study was an effort to identify the discriminatory power of various anthropometric measures and its association with T2DM, using hospital cases and community controls. Despite the small sample size, undisputedly waist circumference may be endorsed as the single most convenient, feasible measure that could be used across communities for its significant association with T2DM.
Generalizability of the results is a limitation of the study because of the smaller sample size and due to disparities in various cut-offs used to define obesity in the available literature. Assessment of glycaemic control was intended to be assessed using investigation reports available from patient's files, but could not be done satisfactorily due to discrepancies in data records. A cohort study with a larger sample size is recommended to determine the optimal cut-off points for the various anthropometric measurements specific for the Indian population.
Conclusions
Among the various anthropometric measurements, BMI was found to have the best discriminatory power. WC and WSR were also found to be sensitive markers. WHR was not a sensitive marker especially for females. So, waist circumference as a single measure could be advocated due to simplicity of measurement and usage either in hospital or community settings.
ACKNOWLEDGMENTS
Heads of Department of Community Medicine and Internal Medicine, Kasturba Medical College, Manipal University, Manipal, Dr Asha Kamath for statistical analysis.
Funding by Indian Council of Medical Research Short Term Studentship Program-2014 (STS-Reference ID 2014-02454).
No potential conflicts of interest. The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
- 1.Rama Lakshmi G, Bandyopadhyay SS, Bhaskar LVKS, Sharma M, Rao RV. Appraisal of risk factors for diabetes mellitus type 2 in central Indian population: a case control study. Antrocom Online J Anthropol. 2011;7:103–110. Available at: http://www.antrocom.net/upload/sub/antrocom/070111/09-Antrocom.pdf [Accessed on 25/07/2014] [Google Scholar]
- 2.Ramachandran A, Snehalatha C. Current scenario of diabetes in India. J Diabetes. 2009;1:18–28. doi: 10.1111/j.1753-0407.2008.00004.x. doi: 10.1111/j.1753- 0407.2008.00004.x. [DOI] [PubMed] [Google Scholar]
- 3.Venkataraman K, Kannan AT, Mohan V. Challenges in diabetes management with particular reference to India. Int J Diabetes Dev Ctries. 2009;29:103–109. doi: 10.4103/0973-3930.54286. doi:10.4103/0973-3930.54286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kamath A, Shivaprakash G, Adhikari P. Body mass index and waist circumference in type 2 diabetes mellitus patients attending a diabetes clinic. Int J Biol Med Res. 2011;2:636–638. Available at: http://www.biomedscidirect.com/journalfiles/IJBMRF2011210/body_mass_index_and_waist_circumference_in_type_2_diabetes_mellitus_patients_attending_a_diabetes_clinic.pdf. Accessed on 20/06/ 2014. [Google Scholar]
- 5.Spollett GR. Diabetes: treating the coming Tsunami. Diabetes Spectrum. 2013;26:58–62. doi: 10.2337/diaspect.26.1.58. [Google Scholar]
- 6.Unnikrishnan R, Anjana RM, Mohan V. Diabetes in South Asians: Is the phenotype different? Diabetes. 2014;63:53–55. doi: 10.2337/db13-1592. doi: 0.2337/db13-1592. [DOI] [PubMed] [Google Scholar]
- 7. The impact of chronic disease in India. Available at: http://www.who.int/chp/chronic_disease_report/media/india.pdf. Accessed on 15/01/2014.
- 8.Padaki S, Vijayakrishna K, Dambal A, Ankad R, Manjula R, Surekharani C, Herur A, Patil S. Anthropometry and physical fitness in individuals with family history of type-2 diabetes mellitus: A comparative study. Indian J Endocrinol Metab. 2011;15:327–330. doi: 10.4103/2230-8210.85595. doi: 10.4103/2230-8210.85595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dagan SS, Segev S, Novikov I, Dankner R. Waist circumference vs body mass index in association with cardiorespiratory fitness in healthy men and women: a cross sectional analysis of 403 subjects. Nutr J. 2013;12:12–12. doi: 10.1186/1475-2891-12-12. doi: 10.1186/1475-2891-12-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Browning LM, Hsieh SD, Ashwell M. A systematic review of waist-to-height ratio as a screening tool for the prediction of cardiovascular disease and diabetes: 0·5 could be a suitable global boundary value. Nutr Res Rev. 2010;23:247–269. doi: 10.1017/S0954422410000144. doi: 10.1017/S0954422410000144. [DOI] [PubMed] [Google Scholar]
- 11. International Diabetes Federation , author. IDF Diabetes Atlas. 6th edition. Brussels, Belgium: International Diabetes Federation; 2013. Available at: http://www.idf.org/diabetesatlas [Accessed on 27/07/2014] [Google Scholar]
- 12. STEP wise approach to surveillance (STEPS)-Guide to physical measurements. World Health Organization. Available at: http://www.who.int/chp/steps/Part3_Section3.pdf [Accessed on 15/01/2014].
- 13. WHO expert consultation , author. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363:157–163. doi: 10.1016/S0140-6736(03)15268-3. doi: http://dx.doi. org/10.1016/S0140-673615268-3. [DOI] [PubMed] [Google Scholar]
- 14. Report of a WHO Expert Consultation on waist circumference and waist hip ratio. Available at: http://whqlibdoc.who.int/publications/2011/9789241501491_eng.pdf [Accessed on 23/01/2014].
- 15.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jones DW, Materson BJ, Oparil S, Wright JT, et al. the National High Blood Pressure Education Program Coordinating Committee, author. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: The JNC 7 Report. JAMA. 2003;289:2560–2571. doi: 10.1001/jama.289.19.2560. doi: 10.1001/jama. 289.19.2560. [DOI] [PubMed] [Google Scholar]
- 16.ärnlöv J, Sundström J, Ingelsson E, Lind L. Impact of BMI and the Metabolic Syndrome on the Risk of Diabetes in Middle-Aged Men. Diabetes Care. 2011;34:61–65. doi: 10.2337/dc10-0955. doi:10.2337/dc10-0955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jowitt LM, Lu LW, Rush EC. Migrant Asian Indians in New Zealand;prediction of metabolic syndrome using body weights and measures. Asia Pac J Clin Nutr. 2014;23:385–393. doi: 10.6133/apjcn.2014.23.3.06. doi: 10.6133/apjcn.2014.23.3.06. [DOI] [PubMed] [Google Scholar]
- 18.Freemantle N, Holmes J, Hockey A, Kumar S. How strong is the association between abdominal obesity and the incidence of type 2 diabetes? Int J Clin Pract. 2008;62:1391–1396. doi: 10.1111/j.1742-1241.2008.01805.x. doi: 10.1111/j.1742-1241.2008.01805.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mamtani M, Kulkarni H, Dyer TD, Almasy L, Mahaney MC, Duggirala R, Comuzzie AG, Blangero J, Curran JE. Waist circumference independently associates with the risk of insulin resistance and type 2 diabetes in Mexican American families. PLoS ONE. 2013;8:e59153–e59153. doi: 10.1371/journal.pone.0059153. doi: 10.1371/journal.pone.0059153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.MacKay MF, Haffner SM, Wagenknecht LE, D'Agostino RB, Hanley AJG. prediction of type 2 diabetes using alternate anthropometric measures in a multi-ethnic cohort: the Insulin Resistance Atherosclerosis Study. Diabetes Care. 2009;32:956–958. doi: 10.2337/dc08-1663. doi: 10.2337/dc08-1663. [DOI] [PMC free article] [PubMed] [Google Scholar]