To the Editor,
Pulmonary tumor thrombotic microangiopathy (PTTM) is rare complication of cancer first described in 1990 by von Herbay et al. [1], where they observed PTTM in 3.3% of autopsied patients with malignant tumors. It can have severe clinical manifestations, including hypoxia, pulmonary hypertension, right-side heart failure, and sudden death [2]. The pathology of PTTM is characterized by non-occluding microscopic tumor cell emboli accompanied by marked intimal proliferation in small pulmonary arteries [1]. Pulmonary tumor embolism is a condition related to PTTM, but it lacks intimal proliferation. In PTTM, tumor emboli in the vasculature and the consequent local activation of coagulation and widespread fibrocellular intimal proliferation of small pulmonary arteries and arterioles lead to increased vascular resistance, resulting in marked pulmonary hypertension [3]. The diagnosis and treatment of PTTM in living patients is extremely difficult, and many patients die of right-side heart failure within weeks. Only four PTTM cases have been reported in Korea, but all were diagnosed shortly before or after death, so no useful treatment was attempted. Here, we report a case of PTTM in a patient with breast cancer diagnosed from a lung perfusion scan.
The patient was a 32-year-old woman who was diagnosed with breast adenocarcinoma (invasive ductal carcinoma, well differentiated) based on a biopsy 5 months earlier and she underwent resection of the left breast and axillary lymph node dissection at that time. Subsequently, she received four cycles of adjuvant chemotherapy (docetaxel 75 mg/body surface area [BSA] and cyclophosphamide 600 mg/BSA). She was also given radiation therapy to the left breast and axillary and supraclavicular nodes, with a posterior axillary boost. Thirteen years ago, she underwent autologous stem cell transplantation for subcutaneous panniculitis-like T-cell lymphoma.
She came to the outpatient clinic with a 2-week history of acute progressive dyspnea on exertion with no associated symptoms after receiving 21 doses of radiation therapy. A transthoracic echocardiogram showed normal left ventricular systolic function with right ventricular enlargement with decreased right ventricular contractile function. It also showed the typical findings of acute pulmonary thromboembolism with a D-shaped left ventricle, mild tricuspid regurgitation, and moderate pulmonary hypertension with an estimated right ventricular systolic pressure of 54 mmHg. D-dimer was elevated at 5.21 μg/mL.
On admission, her blood pressure was 105/56 mmHg, heart rate was 130 beats per minute, respiratory rate was 22 breaths per minute, body temperate was 36.7°C, and oxygen saturation was 85% (on room air). An arterial blood gas analysis on room air revealed hypoxemia: pH 7.472, pCO2 24.3 mmHg, pO2 41.7 mmHg, HCO3 17.6 mmol/L, and SaO2 73.4%. Other laboratory tests showed the following: white blood cell count 7,750/mm3 with a normal differential, hemoglobin 13.1 g/dL, platelets 217,000/mm3, total bilirubin 0.7 mg/dL, alanine aminotransferase 46 IU/L, aspartate aminotransferase 29 IU/L, and C-reactive protein 1.08 mg/dL. A chest radiograph showed no definite abnormality. Computed tomography (CT) pulmonary angiography was performed on suspicion of pulmonary thromboembolism and revealed no significant pulmonary thromboembolism. There were centrilobular ground glass opacities throughout both lungs (Fig. 1). A lung perfusion scan showed multiple small segmental perfusion defects (Fig. 2), which is compatible with PTTM. A lung ventilation scan was not performed due to her condition.
Figure 1.
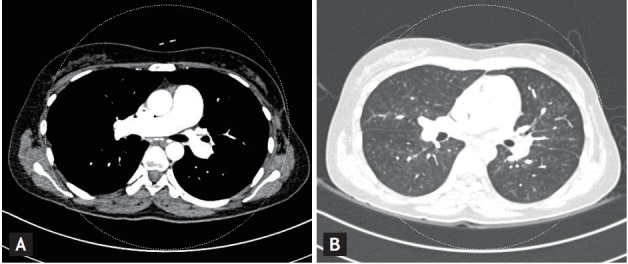
(A) Computed tomography pulmonary angiography revealed no evidence of pulmonary embolism. (B) There were centrilobular ground glass opacities throughout both lungs.
Figure 2.
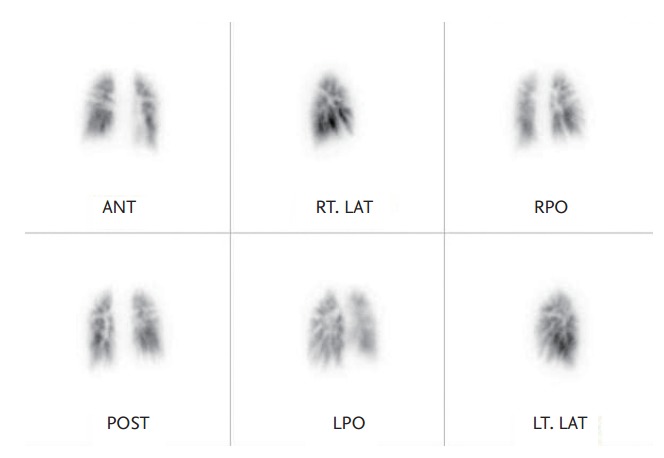
A lung perfusion scan showed multiple small segmental perfusion defects in both lungs. ANT, anterior; RT. LAT, right lateral; RPO, right posterior oblique; POST, posterior; LPO, left posterior oblique; LT. LAT, left lateral.
Anticoagulation therapy with enoxaparin was started and was changed to rivaroxaban after 5 days. She was supported with oxygen (up to 12 L/min via a non-rebreathing mask); the oxygen demand increased gradually over the next 4 days and the oxygen saturation fell below 85%. Therefore, high-flow nasal cannula oxygen therapy was started. The oxygen saturation was maintained satisfactorily until just before her death (Fig. 3). On the 12th day of admission, her general condition deteriorated rapidly and her blood pressure fell. She died despite resuscitation.
Figure 3.
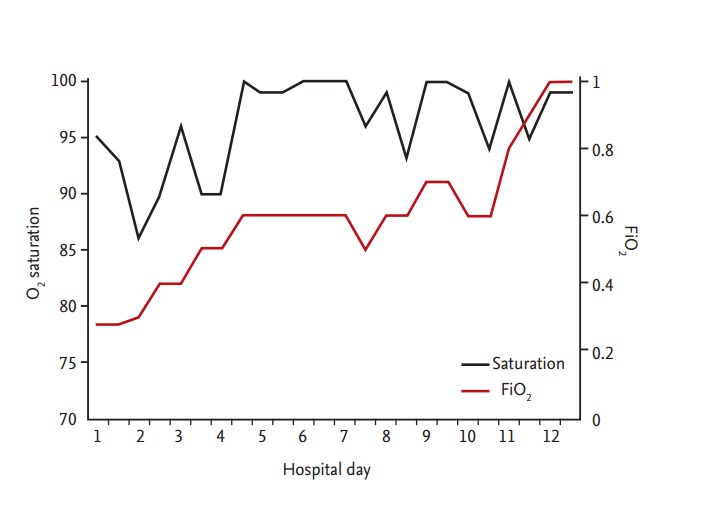
Flowchart of the clinical progress.
PTTM is a fatal, cancer-related pulmonary complication, which is characterized by rapidly progressive dyspnea, pulmonary hypertension and right-sided heart failure, and leads to sudden death [1]. PTTM is seen in 0.8% to 3.3% of autopsied of patients with malignant neoplasms and it is usually associated with adenocarcinoma, especially poorly differentiated gastric adenocarcinoma and adenocarcinoma of the pancreas, breast, liver, colon, lung, and ovary [1,4]. In PTTM, tumor cells metastasize to the pulmonary arterial system and adhere to the vascular endothelium. This activates the coagulation system, which releases inflammatory mediators, resulting in the deposition of platelets and fibrin microthrombi, fibrocellular intimal proliferation, and smooth muscle colonization. These processes induce diffuse narrowing of the pulmonary arteriolar system and increased vascular resistance, resulting in pulmonary hypertension [3].
Antemortem diagnosis of PTTM is difficult and no diagnostic methods have been established for PTTM. CT pulmonary angiography shows no evidence of pulmonary thromboembolism, while a lung ventilation-perfusion scan shows multiple small wedged-shaped perfusion defects [5]. An echocardiogram may show pulmonary hypertension and right-side heart failure. An aggressive bronchoscopic biopsy, transbronchial lung biopsy, or pulmonary microvascular cytology using a wedged pulmonary artery catheter have been suggested as tools for making an antemortem diagnosis of PTTM. However, these procedures cannot be performed in many patients who are already suffering from severe, progressive dyspnea.
In our case, PTTM was confirmed based on four clinical findings. The patient had been diagnosed with breast adenocarcinoma (invasive ductal carcinoma, well differentiated) and PTTM is usually associated with adenocarcinoma. A transthoracic echocardiogram showed normal left ventricular contractile function with an elevated estimated systolic pulmonary artery pressure of 54 mmHg and a D-shaped left ventricle. There was no evidence of pulmonary thromboemboli on CT pulmonary angiography, ruling out a diagnosis of pulmonary thromboembolic disease. A lung perfusion scan showed multiple small segmental perfusion defects compatible with PTTM. The clinical manifestations in this case were all consistent with PTTM.
Although the underlying molecular mechanism of PTTM remains uncertain, platelet-derived growth factor, vascular endothelial growth factor, and osteopontin may play important roles in the pathogenesis of PTTM [3]. There is no standard management for PTTM. In one reported case, PTTM was managed with a combination of anticoagulation, steroid therapy, and anticancer drugs [4]. In a recent case, imatinib, a tyrosine kinase inhibitor of the platelet-derived growth factor receptor, led to the regression of pulmonary hypertension and pulmonary artery remodeling in PTTM [5]. However, the disease usually progresses rapidly and the prognosis is extremely poor. Almost all patients with PTTM die within 2 weeks of the onset of dyspnea [2,3]. Although we tried best-supportive care, our patient died 12 days after the diagnosis was made. The hypoxia is rapidly progressive in PTTM. In our case, we first applied high-flow nasal cannula oxygen therapy to manage hypoxia. With the high-flow nasal cannula oxygen therapy, the oxygen saturation was maintained avoiding endotracheal intubation. However, rapidly progressive circulatory failure eventually developed and the patient died. This demonstrates that the cause of death in PTTM is not respiratory failure, but circulatory failure.
In conclusion, PTTM is a rare pulmonary complication of cancer that is fatal because of its rapid progression. To make an early diagnosis and intervene therapeutically, it is important to include PTTM in the differential diagnosis of cancer patients with rapidly progressing hypoxemia without pulmonary thromboembolism. Although we could not change the clinical outcome using highflow nasal cannula oxygen therapy, we revealed that the cause of death in PTTM is circulatory failure, and not hypoxia. Nevertheless, further studies are needed to elucidate the pathogenesis and treatment of PTTM.
Footnotes
No potential conflict of interest relevant to this article was reported.
REFERENCES
- 1.von Herbay A, Illes A, Waldherr R, Otto HF. Pulmonary tumor thrombotic microangiopathy with pulmonary hypertension. Cancer. 1990;66:587–592. doi: 10.1002/1097-0142(19900801)66:3<587::aid-cncr2820660330>3.0.co;2-j. [DOI] [PubMed] [Google Scholar]
- 2.Hibbert M, Braude S. Tumour microembolism presenting as “primary pulmonary hypertension”. Thorax. 1997;52:1016–1017. doi: 10.1136/thx.52.11.1016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chinen K, Kazomoto T, Ohkura Y, Matsubara O, Tsuchiya E. Pulmonary tumor thrombotic microangiopathy caused by a gastric carcinoma expressing vascular endothelial growth factor and tissue factor. Pathol Int. 2005;55:27–31. doi: 10.1111/j.1440-1827.2005.01783.x. [DOI] [PubMed] [Google Scholar]
- 4.Miyano S, Izumi S, Takeda Y, et al. Pulmonary tumor thrombotic microangiopathy. J Clin Oncol. 2007;25:597–599. doi: 10.1200/JCO.2006.09.0670. [DOI] [PubMed] [Google Scholar]
- 5.Fukada I, Araki K, Minatsuki S, et al. Imatinib alleviated pulmonary hypertension caused by pulmonary tumor thrombotic microangiopathy in a patient with metastatic breast cancer. Clin Breast Cancer. 2015;15:e167–e170. doi: 10.1016/j.clbc.2014.10.008. [DOI] [PubMed] [Google Scholar]


