ABSTRACT
The replication and pathogenicity of influenza A viruses (IAVs) critically depend on their ability to tolerate the antiviral interferon (IFN) response. To determine a potential role for the IAV hemagglutinin (HA) in viral sensitivity to IFN, we studied the restriction of IAV infection in IFN-β-treated human epithelial cells by using 2:6 recombinant IAVs that shared six gene segments of A/Puerto Rico/8/1934 virus (PR8) and contained HAs and neuraminidases of representative avian, human, and zoonotic H5N1 and H7N9 viruses. In A549 and Calu-3 cells, viruses displaying a higher pH optimum of HA-mediated membrane fusion, H5N1-PR8 and H7N9-PR8, were less sensitive to the IFN-induced antiviral state than their counterparts with HAs from duck and human viruses, which fused at a lower pH. The association between a high pH optimum of fusion and reduced IFN sensitivity was confirmed by using HA point mutants of A/Hong Kong/1/1968-PR8 that differed solely by their fusion properties. Furthermore, similar effects of the viral fusion pH on IFN sensitivity were observed in experiments with (i) primary human type II alveolar epithelial cells and differentiated cultures of human airway epithelial cells, (ii) nonrecombinant zoonotic and pandemic IAVs, and (iii) preparations of IFN-α and IFN-λ1. A higher pH of membrane fusion and reduced sensitivity to IFN correlated with lower restriction of the viruses in MDCK cells stably expressing the IFN-inducible transmembrane proteins IFITM2 and IFITM3, which are known to inhibit viral fusion. Our results reveal that the pH optimum of HA-driven membrane fusion of IAVs is a determinant of their sensitivity to IFN and IFITM proteins.
IMPORTANCE The IFN system constitutes an important innate defense against viral infection. Substantial information is available on how IAVs avoid detection by sensors of the IFN system and disable IFN signaling pathways. Much less is known about the ability of IAVs to tolerate the antiviral activity of IFN-induced cellular proteins. The IFN-induced proteins of the IFITM family block IAV entry into target cells and can restrict viral spread and pathogenicity. Here we show for the first time that the sensitivity of IAVs to the IFN-induced antiviral state and IFITM2 and IFITM3 proteins depends on the pH value at which the viral HA undergoes a conformational transition and mediates membrane fusion. Our data imply that the high pH optimum of membrane fusion typical of zoonotic IAVs of gallinaceous poultry, such as H5N1 and H7N9, may contribute to their enhanced virulence in humans.
KEYWORDS: H5N1, H7N9, IFITM, fusion, hemagglutinin, influenza, interferon, restriction
INTRODUCTION
Influenza A viruses (IAVs) are important pathogens with a wide host range and variable pathogenicity. Wild aquatic birds represent the major natural reservoir of IAVs. Transmission and adaptation of aquatic bird viruses to domestic birds and mammals with prolonged circulation of viruses in these species facilitate occasional zoonotic transmissions. Although zoonotic IAVs are not transmitted from human to human, some of them, such as the poultry H5N1 and H7N9 viruses, can cause unusually severe human disease and fatalities (for reviews, see references 1, to ,4). On rare occasions, animal viruses become adapted to humans, initiate global pandemics, and continue to circulate and evolve in humans for decades, causing annual seasonal influenza outbreaks (5, 6). Thus, influenza disease in humans can be caused by seasonal, pandemic, and zoonotic viruses that have distinguishable properties.
Efficient replication of IAVs depends on their ability to evade the antiviral type I and III interferon (IFN) systems (7–9). IFNs secreted by virus-infected cells trigger the upregulation of several hundred IFN-stimulated genes, some of which encode proteins that were found to inhibit different stages of the viral life cycle (reviewed in references 7, 10, and 11). At the earliest step of infection, the IFN-induced transmembrane proteins (IFITMs) IFITM1, IFITM2, and IFITM3 restrict virus entry into cells by inhibiting fusion between viral and cellular membranes (12, 13). Other IFN-induced proteins, such as MxA, 2′,5′-oligoadenylate synthetase/RNase L, ADAR1, APOBEC, PKR, IFITs, and BST2/tetherin, inhibit later steps of viral replication (7, 8, 10, 11).
IAVs counteract the development of the IFN-dependent antiviral state by several mechanisms, including inhibition of IFN induction, disruption of IFN signaling pathways, and inactivation of IFN-induced gene products (reviewed in references 7 to 9). The viral NS1 protein is primarily responsible for these activities (14). The IFN-counteracting measures of IAVs are not 100% efficient, and any IAV has to replicate under the pressure of the IFN-induced antiviral effectors. Mechanisms that allow IAVs to tolerate this pressure are not well understood, but they may be critical for viral host range and pathogenicity. For example, the nucleoprotein (NP) of avian IAVs was found to be more sensitive to restriction by MxA protein than the NP of human IAVs (15), and the emergence of the 1918 and 2009 pandemic viruses required the acquisition of adaptive mutations in the NP that reduced MxA binding (16). These findings highlight the necessity to characterize the roles of different viral proteins in the sensitivity of IAVs to the IFN-induced state.
The hemagglutinin (HA) protein of IAVs has two essential functions early in the viral life cycle (17, 18). It mediates virus attachment to target cells via binding to sialic acid-containing cell surface molecules. After endocytosis, the decreasing pH in the endosomes triggers structural rearrangements of the HA that eventually lead to fusion between viral and endosomal membranes and entry of nucleocapsids into the cytoplasm. Differences in the receptor binding specificity of animal and human viruses and differential expression of sialic acid receptors in the human respiratory tract determine, to a significant extent, differences in viral cell and tissue tropism, transmissibility, and disease severity in humans (reviewed in references 4 and 19 to 21). Furthermore, there is growing evidence that the interval of acidic pH at which HA undergoes a conformational transition and mediates membrane fusion (pH optimum of fusion) also differs between IAVs from different host species (22–24), and these differences in the pH optimum of fusion can affect viral interspecies transmission and pathogenicity (reviewed in references 25 to 27).
Given the critical role of the HA in the early stages of viral infection and significant host- and strain-specific variation of HA receptor binding characteristics and membrane fusion activity, we wished to test whether properties of the HA can modulate the sensitivity of IAVs to IFN-induced antiviral molecules. To test this hypothesis, we generated 2:6 recombinant influenza viruses that contained HAs of representative IAVs from different host species, as well as HAs with single amino acid substitutions, and compared the abilities of these viruses to infect IFN-treated human cells. We found that the pH optimum of viral membrane fusion activity affected the sensitivity of the viruses to the IFN-induced antiviral state and that this phenomenon was determined, at least in part, by the interplay between HA and cellular IFITMs.
RESULTS
Sensitivity of IAVs to the IFN-induced antiviral state depends on the origin of HA and NA and correlates with the viral pH optimum of membrane fusion.
To study potential effects of viral HA on the sensitivity of IAVs to IFN, we generated 2:6 recombinant viruses that shared six gene segments of laboratory strain A/Puerto Rico/8/1934 (PR8) and differed solely by the origin of their HA and NA. The homologous NAs were included together with the HAs to preserve the functional balance between the two glycoproteins, which is known to be essential for efficient viral replication (28). The recombinant viruses contained HA and NA segments of representative viruses from three major natural hosts (virus descriptions and abbreviations are shown in Table 1, group 1 viruses). Non-egg-adapted A/Memphis/14/1996 (H1N1) represented seasonal human IAVs, the H1N1 and H2N2 mallard viruses represented IAVs of wild aquatic birds, and the H5N1 and H7N9 virus isolates from human cases of infection were chosen to represent poultry-adapted IAVs with zoonotic potential. The receptor binding specificities of the HA/NA-donating wild-type viruses were characterized previously (29–33). Thus, A/Memphis/14/1996 preferentially bound to Neu5Ac2-6Gal-terminated receptors, mallard viruses and the H5N1 virus preferentially bound to Neu5Ac2-3Gal-terminated receptors, and the H7N9 virus displayed a dual binding specificity with stronger binding to avian type Neu5Ac2-3Gal-terminated receptors (Table 1). To characterize membrane fusion properties of the recombinant IAVs, we determined the pHs at which the viral HAs underwent an acid-induced conformational transition (pH50-HA) and at which the virus lost infectivity owing to acid-induced inactivation of the HA (pH50-inact). In addition, we compared levels of inhibition of viral infection by the lysosomotropic agent ammonium chloride, which counteracts the acidification of endosomes and lysosomes; a higher sensitivity to NH4Cl reflected a viral requirement for a lower pH during fusion and/or uncoating (24). Collectively, these three assays indicated that the HAs of Mem-H1N1 and the two duck IAVs, mal-H1N1 and mal-H2N2, underwent conformational transition and mediated membrane fusion at a lower pH than the HAs of VN-H5N1 and Sh-H7N9 (Table 1). Thus, the receptor binding properties of the recombinant IAVs and their relative pH optima of membrane fusion well represented typical properties of IAVs from corresponding natural reservoirs (aquatic birds, gallinaceous poultry, and humans) (19–22, 34–39).
TABLE 1.
2:6 recombinant PR8-based viruses used in this study
| Viral group and abbreviation | Source of HA and NA | Receptor binding specificity (reference[s])a | Membrane fusion activity and stabilityb |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Low-pH conformational transition of HA (pH50-HA) |
Loss of infectivity at acidic pH (pH50-inact) |
Inhibition of infection by NH4Cl (IC50, mM) |
|||||||||
| Mean | SD (n) | P valuec | Mean | SD (n) | P valuec | Mean | SD (n) | P valuec | |||
| Group 1f | |||||||||||
| Mem-H1N1 | A/Memphis/14/1996 (H1N1) | α2-6 (29, 30) | 4.7 | 0.14 (12) | 5.2 | 0.06 (8) | 0.48 | 0.16 (12) | |||
| mal-H1N1 | A/mallard/Alberta/119/1998 (H1N1) | α2-3 (29, 30) | 4.9 | 0.12 (12) | <0.001 | 5.3 | 0.13 (7) | 0.77 | 0.20 (8) | <0.01 | |
| mal-H2N2 | A/mallard/New York/6750/1978 (H2N2) | α2-3 (31) | 5.1 | 0.18 (12) | <0.001 | 5.2 | 0.11 (4) | 1.17 | 0.14 (4) | <0.001 | |
| VN-H5N1 | A/Vietnam/1203/2004 (H5N1) | α2-3 (32) | 5.7 | 0.10 (14) | <0.001 | 5.7 | 0.03 (8) | <0.001 | 1.55 | 0.24 (12) | <0.001 |
| Sh-H7N9 | A/Shanghai/2/2013 (H7N9) | α2-3 > α2-6 (33) | 5.6 | 0.11 (6) | <0.001 | 5.6 | 0.01 (2) | <0.001 | 1.36 | 0.20 (4) | <0.001 |
| Group 2g | |||||||||||
| HK-H3N2 | A/Hong Kong/1/1968 (H3N2) | α2-6 > α2-3 (30, 43) | 4.9 | 0.06 (13) | NDd | 0.33 | 0.04 (12) | ||||
| 82T | K822T mutation in HA2 | Same as HK-H3N2e | 5.1 | 0.05 (7) | <0.001 | ND | 0.81 | 0.07 (11) | <0.001 | ||
| 17R | H171R mutation in HA1 | Same as HK-H3N2e | 5.3 | 0.20 (7) | <0.001 | ND | 1.00 | 0.26 (9) | <0.001 | ||
| 17Y | H171Y mutation in HA1 | Same as HK-H3N2e | 4.7 | 0.07 (7) | <0.001 | ND | 0.25 | 0.05 (11) | <0.001 | ||
Virus ability to recognize Siaα2-6Gal-terminated receptors, Siaα2-3Gal-terminated receptors, or both receptor types as described in the references cited. The symbol > indicates stronger binding to the receptor type indicated.
Viral membrane fusion characteristics were studied as described in Materials and Methods. The data are mean values and standard deviations of 2 to 14 biological replicates from two to eight independent experiments performed on different days. Numbers of replicates are shown in parentheses.
P values were calculated with an unpaired two-tailed Student t test. Viruses in groups 1 and 2 were compared with Mem-H1N1 and HK-H3N2, respectively.
ND, not determined.
No differences with respect to HK-H3N2 were detected in two receptor-binding assays described in reference 43.
Viruses with wild-type HA and NA.
Fusion mutants of A/Hong Kong/1/1968.
The viral sensitivity to the IFN-induced antiviral state was studied by stimulation of cells with human IFN-β for 24 h, followed by infection and quantification of the numbers of NP-positive cells after one cycle of viral replication. The single-cycle replication assay allowed us to study the effects of IFN-induced proteins on HA-dependent early stages of infection and exclude potential effects on the late stages of infection, such as assembly and release of viral progeny. We used this approach to facilitate the interpretation of the data. Thus, as all 2:6 recombinant viruses contained identical ribonucleocapsids, any differences in the number of NP-positive cells reflected differences in virus attachment, endocytosis, or intraendosomal membrane fusion.
All viruses were inhibited by IFN in a dose-dependent manner in stimulated A549 cells (Fig. 1a). VN-H5N1 and Sh-H7N9 were inhibited less strongly than the three other viruses, indicating that the sensitivity of IAVs to IFN depends on the origin of the HA and NA. The effect did not correlate with the receptor binding preference of the virus for the type of Neu5Ac-Gal linkage. For example, human and duck viruses displayed opposite linkage preferences but were equally sensitive to inhibition by IFN. At the same time, the reduced inhibition of VN-H5N1 and Sh-H7N9 by IFN compared to the three other viruses tested correlated with the viral pH optimum of membrane fusion, with the less IFN-susceptible viruses having a higher pH optimum than the more susceptible ones.
FIG 1.
Effect of IFN pretreatment on single-cycle viral infection in A549 (a, b) and Calu-3 (c, d) cells. Cell cultures were maintained for 24 h in medium supplemented with various amounts of human IFN-β; control cultures were incubated without IFN. The cells were infected with 200 FFU of virus per culture, fixed after one cycle of viral replication, and immunostained for viral NP. Numbers of NP-positive cells in IFN-treated cultures were determined and are expressed as percentages of those of the control cultures. (a, c) Recombinant viruses with wild-type HA and NA. (b, d) Recombinant HK-H3N2 virus and its fusion mutants. Four (a), five (b), and two (c, d) independent experiments were performed on different days with the same results. The panels show results of representative experiments with two (a, c, d) and four (b) biological replicates for each condition. The data points and error bars depict mean values and standard deviations. Asterisks indicate the statistical significance of differences with respect to Mem-H1N1 (a, c) and HK-H3N2 (b, d), as defined in Materials and Methods.
Fusion-modulating amino acid substitutions in the HA affect viral restriction by IFN.
To further investigate the correlation between the sensitivity of IAVs to IFN and their fusion pH optimum, we decided to exclude potential effects of the HA receptor binding activity and NA-dependent effects by comparing viruses that differed solely by their membrane fusion properties. A large number of fusion-affecting amino acid substitutions in the HA of the H3N2/1968 pandemic influenza virus were characterized by Skehel and colleagues (reviewed in references 17, 26, and 27). On the basis of these studies, we generated a 2:6 recombinant virus containing HA and NA of A/Hong Kong/1/1968 (H3N2) and three variants of this virus with single-point substitutions in the HA, H171Y, H171R, and K822T (Table 1, group 2 viruses HK-H3N2, 17Y, 17R, and 82T, respectively). These substitutions were located in the fusion domain of the HA, far away from the receptor binding site, and were reported to significantly alter the pH optimum of membrane fusion and stability without effects on other properties of the HA (40–42). We verified the differences in the pH optima of fusion of the recombinant viruses generated by using two assays. As expected, compared to the parental HK-H3N2 virus, variants 17R and 82T displayed a higher pH of conformational transition and were less sensitive to inhibition by ammonium chloride during cell entry, whereas variant 17Y displayed the opposite phenotype (Table 1). To assess a potential effect of substitutions on viral receptor binding properties, we compared the viruses for their binding to fetuin preparations carrying either Neu5Ac2-3Gal or Neu5Ac2-6Gal and for their ability to infect partially desialylated Madin-Darby canine kidney (MDCK) cells as described previously (43). As expected from the locations of the substitutions, no differences among the wild-type HK-H3N2, 17R, 17Y, and 82T viruses were detected in these receptor binding assays (data not shown).
The HK-H3N2 and 17Y mutant viruses were inhibited to similar extents in IFN-pretreated A549 cells (Fig. 1b), whereas variant 82T and especially variant 17R showed less inhibition than HK-H3N2 and 17Y. These results formally confirmed that the membrane fusion properties of the HA affect the sensitivity of IAVs to IFN.
The pattern of viral inhibition by IFN in A549 cells was well reproduced in another epithelial cell line of human origin, Calu-3 cells (Fig. 1c and d). Thus, the viruses with a low pH optimum of membrane fusion (Mem-H1N1, mal-H1N1, HK-H3N2, 17Y) were more strongly inhibited by IFN than their counterparts that fused at a relatively high pH (VN-H5N1, 17R).
Viral fusion pH affects the restriction of IAVs by IFITM2 and IFITM3 proteins.
The observation that sensitivity of IAVs to IFN depends on the viral pH optimum of fusion prompted us to test if IFN-inducible proteins of the IFITM family, which are known to inhibit fusion between viral and cellular membranes, contribute to this effect. To this end, we studied the IAV infection of MDCK cells engineered to stably express either IFITM2 or IFITM3. The ability of the viruses to enter the cells and undergo one cycle of replication was impaired to various extents in the cells expressing IFITMs compared to parent MDCK cells (Fig. 2a and b). Thus, Mem-H1N1 and mal-H1N1 were more efficiently restricted by IFITM2 and IFITM3 expression than were VN-H5N1 and Sh-H7N9 (Fig. 2a). Moreover, of the single-point fusion mutants (Fig. 2b), variant 17R was significantly less restricted and variant 17Y was significantly more restricted in both types of IFITM-expressing cells than was the parental HK-H3N2 virus. These results were confirmed when multicycle viral replication was studied by comparing the sizes of the plaques formed by the viruses in MDCK cells and in MDCK cells expressing IFITM2 and IFITM3. In these experiments, Mem-H1N1, mal-H1N1, and HK-H3N2 were significantly more restricted by IFITMs than were VN-H5N1 and Sh-H7N9 (Fig. 2c). Variant 17Y was highly sensitive to both IFITMs and failed to form plaques in MDCK-IFITM2 and MDCK-IFITM3 cells. Conversely, variant 17R was less restricted than the parent HK-H3N2 (Fig. 2d).
FIG 2.
Inhibition of single-cycle infection and plaque formation in MDCK cells stably expressing IFITM2 and IFITM3 proteins. (a, b) Virus titers in MDCK, MDCK-IFITM2, and MDCK-IFITM3 cells were determined with a single-cycle focus formation assay. Titers are expressed in log10 FFU per milliliter, and the graphs depict the calculated reduction of the titers in IFITM-expressing cells with respect to control MDCK cells. Three (a) and four (b) independent experiments were performed on different days with the same results. The panels show results of representative experiments with three biological replicates for each condition. (c, d) The diameters of 40 to 100 plaques formed by the viruses under semisolid overlay medium were measured for each cell type, and percentages with respect to the mean plaque diameter in MDCK cells (control) were calculated. Asterisks indicate the statistical significance of differences with respect to Mem-H1N1 (a, c) and HK-H3N2 (b, d).
Collectively, these studies demonstrated that viruses with a low pH optimum of fusion (Mem-H1N1, mal-H1N1, and HK-H3N2) were more sensitive to inhibition by IFITM2 and IFITM3 than viruses fusing at a higher pH (VN-H5N1 and Sh-H7N9). Furthermore, single fusion-modulating substitutions H171Y and H171R were sufficient to increase and decrease virus restriction by IFITMs, respectively.
Viral pH optimum of membrane fusion affects restriction of influenza viruses by IFN in primary human respiratory epithelial cells.
We next explored whether the observations made with continuous cell lines (A549 and Calu-3) could be reproduced with cultures of primary human tracheobronchial and alveolar epithelial cells, which better mimic the conditions of IAV infection of the human respiratory tract. Given the limited access to these cells, four 2:6 recombinant IAVs, VN-H5N1, Sh-H7N9, HK-H3N2, and its fusion mutant 17R, were chosen for the experiments.
Type II alveolar epithelial cells (AECII) isolated from human lung tissue and cultivated on semipermeable membrane supports were stimulated with 0, 2, or 20 U of IFN-β/ml of culture medium, infected with the viruses, and analyzed as described above for A549 and Calu-3 cells (Fig. 3a). 17R, VN-H5N1, and Sh-H7N9 showed similar levels of inhibition and were significantly less inhibited than HK-H3N2 in cultures stimulated with 2 U of IFN/ml. 17R and VN-H5N1 were also less sensitive than HK-H3N2 at 20 U of IFN/ml.
FIG 3.

Effect of IFN pretreatment on single-cycle viral infection in AECII and HTBE cultures. (a) AECII cultures were pretreated with IFN-β (either 2 or 20 U ml−1) for 24 h; control cultures were incubated without IFN. The cultures were infected with 2 × 104 FFU of the viruses, fixed at 8 h postinfection, and immunostained. Numbers of NP-positive cells per standard area of IFN-treated cultures were determined and are expressed as percentages of those of the corresponding control cultures. The data are mean values and standard deviations from two experiments performed on different days with three replicate cultures each (n = 6). (b) HTBE cultures were pretreated with 20 U ml−1 IFN-β or mock treated for 24 h, infected with 6 × 105 FFU of the viruses, fixed at 8 h postinfection, and immunostained. Numbers of NP-positive cells per standard area of IFN-treated cultures were determined and are expressed as percentages of those of the corresponding control cultures. The data are mean values and standard deviations for three experiments performed on different days with three or four replicate cultures for each condition. In both panels, asterisks indicate the statistical significance of differences with respect to HK-H3N2.
Differentiated cultures of human tracheobronchial epithelial (HTBE) cells were prepared by cultivation of primary human HTBE cells (Lonza) on membrane supports at the air-liquid interface (ALI). The cultures were pseudostratified and polarized; they contained basal, ciliated, and mucus-secreting cells, thus resembling human airway epithelium in vivo (29, 44). We studied how stimulation of the cells with 20 U of IFN-β/ml affected single-cycle viral infection (Fig. 3b). Variant 17R was less strongly inhibited than HK-H3N2 in all three independent experiments. Sh-H7N9 also showed somewhat less sensitivity than HK-H3N2, although the results were not statistically significant in two out of three experiments. VN-H5N1 did not differ from HK-H3N2 in two experiments and was less sensitive in the third one.
Thus, the relative sensitivities of the four viruses tested in A549 and Calu-3 cells to the IFN-induced state were fully reproduced in AECII infections and partially reproduced in experiments with HTBE cultures. Unlike A549, Calu-3, and AECII cells, the HTBE cultures contain several distinctive types of cells and secrete sialic acid-containing mucins; these features could account for the apparent partial inconsistency between the results obtained with HTBE cultures and those obtained with other cells. For example, both cell tropism and neutralization of IAVs by mucins depend on viral receptor binding specificity and neuraminidase activity (28, 29, 45), suggesting that distinctions between these properties (Table 1) may, in addition to the fusion pH, affect the sensitivity of viruses to IFN in HTBE cultures. This concept is supported by the observation that HK-H3N2 and its single-point fusion mutant 17R displayed the same relative sensitivity to IFN in all four types of cultures tested, indicating that, in the absence of other differences in the viral HAs and NAs, a higher pH optimum of fusion universally reduces the IFN-dependent inhibition of IAV entry into human respiratory and alveolar epithelium.
Sensitivity to IFN of natural IAV isolates correlates with their pH optimum of membrane fusion.
Experiments with 2:6 recombinant viruses revealed a lower IFN-mediated restriction of VN-H5N1 and Sh-H7N9 than of Mem-H1N1 and HK-H3N2. To test whether this pattern would be consistent with the IFN sensitivity of the corresponding wild-type zoonotic and human viruses, we studied single-cycle infections of IFN-treated A549 cells by using natural viral isolates. In addition to wild-type A/Memphis/14/1996 (H1N1) and A/Hong Kong/1/1968 (H3N2), the 2009 pandemic influenza virus A/Hamburg/5/2009 (H1N1) was included in this study. Because wild-type A/Vietnam/1203/2004 (H5N1) and A/Shanghai/2/2013 (H7N9) were not available, the closely related zoonotic viruses A/Thailand/KAN-1/2004 (H5N1) and A/Anhui/1/2013 (H7N9) were tested. The HA of the H5N1 virus contained a multibasic cleavage site, permitting proteolytic activation and multicycle replication of the virus in the absence of trypsin in the culture medium. To limit replication to one cycle, all cultures were fixed at 8 h postinfection in this series of experiments.
The 2009 pandemic virus and both zoonotic viruses were less sensitive to IFN than were A/Memphis/1996 and A/Hong Kong/1968 (Fig. 4a). The former three viruses were also less sensitive to inhibition by ammonium chloride during their cell entry (Fig. 4b), which is indicative of their higher pH optimum of fusion. Thus, irrespective of host- and strain-specific differences among the six “internal” gene segments of the wild-type viruses studied, their sensitivity to IFN-induced state correlated with the viral pH optimum of fusion.
FIG 4.
Infection of IFN-treated A549 cells with wild-type influenza viruses (a) and sensitivity of wild-type influenza viruses to inhibition by ammonium chloride in MDCK cells (b). (a) Replicate A549 cultures were maintained in medium supplemented with IFN-β (1, 10, or 100 U ml−1) for 24 h; control cultures were maintained without IFN. The cells were infected with 200 FFU of virus per culture, incubated for 8 h, fixed, and immunostained for NP. Numbers of NP-positive cells in IFN-treated cultures were determined and are expressed as percentages of those of the control cultures. (b) MDCK cells were infected with the viruses in the presence of various concentrations of NH4Cl, incubated for 8 h, fixed, and immunostained for NP. Numbers of infected cells were determined, and IC50s were determined from the dose-response curves by linear interpolation. In both panels, data points show mean values and standard deviations from two experiments performed on different days with three replicate cultures each (n = 6). Asterisks indicate the statistical significance of differences with respect to A/Memphis/14/1996.
Antiviral effects of IFN-α and IFN-λ.
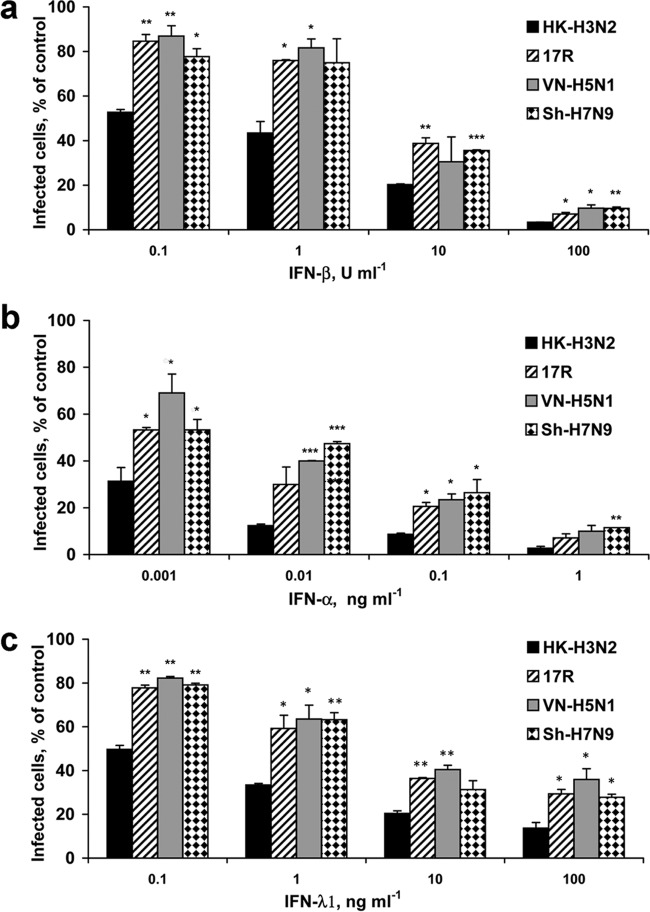
We next assessed whether the differential sensitivities of the viruses to IFN-β will be reproduced with other types of IFN, namely, IFN-α, another type I IFN, and IFN-λ, a type III IFN important for anti-IAV defenses of epithelia (46). Four viruses tested displayed the same relative sensitivity, irrespective of the IFN used, with HK-H3N2 being more efficiently inhibited than 17R, VN-H5N1, and Sh-H7N9 (Fig. 5).
FIG 5.
Effect of pretreatment with human IFN-β (a), IFN-α (b), and IFN-λ1 (c) on single-cycle viral infection of A549 cells. Cell cultures were maintained for 24 h in medium supplemented with various amounts of IFNs. Control cultures were incubated without IFN. The cells were infected with 200 FFU of virus per culture, fixed after overnight incubation, and immunostained for viral NP. Numbers of NP-positive cells in IFN-treated cultures were determined and are expressed as percentages of those of the control cultures. The data points and error bars depict mean values and standard deviations from one experiment with two replicate cultures for each data point (n = 2). Asterisks indicate the statistical significance of differences with respect to HK-H3N2.
Multicycle viral replication in IFN-stimulated cells.
The single-cycle infection experiments performed thus far revealed differences in viral sensitivity to IFN at the early stages of infection. To estimate the combined effects of the IFN-induced antiviral state at the early and late stages of infection, we studied the multicycle growth of six viruses in Calu-3 cells. The titers of HK-H3N2, Mem-H1N1, mal-H1N1, and Sh-H7N9 in the supernatants of IFN-treated cells were reduced, and the reduction was more pronounced at higher concentrations of IFN and at later time points (Fig. 6). In contrast, two other viruses, 17R and VN-H5N1, were significantly less affected by IFN. In particular, 10 U ml−1 IFN had a minor effect, if any, on the titers of these viruses. At 72 h postinfection, 100 U ml−1 IFN had no effect on the titer of VN-H5N1 and caused only a 10-fold reduction in the titer of 17R, whereas the titers of the other four viruses were reduced by 2 to 2.5 orders of magnitude. Thus, sensitivity to IFN during the multicycle replication of five out of six viruses tested correlated with the viral pH optimum of membrane fusion. In contrast, Sh-H7N9 had a high pH optimum of fusion but behaved similarly to viruses fusing at a relatively low pH. It remains unclear whether this discrepancy depends on specific properties of HA, NA, their combination, or some other properties of Sh-H7N9. In any case, comparison of the HK-H3N2 and 17R pair clearly suggested that of two IAVs that only differ by the pH optimum of membrane fusion, the virus with a higher fusion pH will have a growth advantage during its multicycle replication in IFN-activated cells.
FIG 6.
Multicycle viral replication in IFN-treated Calu-3 cells. Cells were stimulated with 0, 10, or 100 U ml−1 IFN-β for 24 h and infected at 2.3 × 103 PFU per culture (multiplicity of infection, ∼0.01) with the recombinant viruses HK-H3N2, 17R, VN-H5N1, Mem-H1N1, mal-H1N1, and Sh-H7N9. At 1 h postinfection, the inocula were removed and replaced with IM containing the same concentrations of IFN that were used for stimulation. Samples of supernatants were collected daily and titrated by focus formation assay in MDCK cells. The data are mean values and standard deviations from two experiments performed on different days with three replicate cultures each (n = 6). Arrows depict four data points for IFN-treated cultures infected with 17R and VN-H5N1 with no significant difference from mock-treated cultures; all other differences between viral titers in IFN-treated cultures and corresponding mock-treated cultures were statistically significant (P < 0.05).
DISCUSSION
Current knowledge of the ability of IAVs to evade the IFN response is biased toward mechanisms that interfere with either virus detection by cellular innate sensors or subsequent development of the IFN-induced antiviral state; less is known about mechanisms that modulate the sensitivity of IAVs to IFN-stimulated antiviral effectors (for reviews, see references 7 to 9, 25, and 47). We demonstrate in this study that the level of inhibition of IAV infection in IFN-stimulated cells depends on the membrane fusion characteristics of the viral HA. Namely, IAVs having a relatively high pH optimum of fusion were found to be less restricted in IFN-treated cell lines and primary human airway and alveolar epithelial cells than IAVs fusing at a lower pH.
The only IFN-induced effector proteins known to inhibit the virus-cell fusion of IAVs are members of the IFITM family. IFITMs are small transmembrane proteins constitutively expressed in many cells of different vertebrate species and strongly upregulated by IFNs. Human IFITM1, IFITM2, and IFITM3 restrict the cell entry of many enveloped viruses and at least one nonenveloped virus in vitro; the level of restriction varies depending on the virus, IFITM species, and cell type (reviewed in references 10, 11, 13, 48, and 49). Importantly, IFITM3 represents one of the IFN-stimulated effectors that have been linked to the pathogenic outcome of IAV infection in vivo. Thus, IFITM3 was shown to reduce the morbidity and mortality of IAV infection in mice (50, 51). In humans, homozygosity for the minor rs12252-C allele in the IFITM3 gene, which encodes a protein with compromised antiviral activity, correlated with an increased risk of IAV infection and/or severity of influenza disease (51–55).
Depletion of IFITM3 in cell culture resulted in a loss of 40 to 70% of IFN-induced anti-IAV activity (12, 56), indicating that IFITMs are major contributors, at least in vitro, to the anti-IAV effect of IFN. In agreement with this notion, we observed a clear correlation between the restriction of different IAVs in IFN-stimulated cells and in MDCK cells stably expressing IFITM2 and IFITM3. We conclude, therefore, that the effects of the membrane fusion pH on the IFN sensitivity of IAVs observed in our experiments are primarily explained by differences in viral inhibition by IFN-induced IFITM2 and/or IFITM3. However, a contribution of other IFN-stimulated effectors to the effects observed cannot be excluded. In addition to IFITM1, cholesterol-25-hydroxylase (CH25H) is a putative candidate, as limited data indicate that CH25H blocks an early step in the infectious cycle, possibly virus-host membrane fusion (11, 57).
The exact mechanisms responsible for inhibition of membrane fusion by IFITMs remain unknown and may vary between viruses. One model suggests that IFITMs localize at the sites of fusion and suppress virus-mediated formation and/or expansion of fusion pores by reducing fluidity and changing the curvature of the cell membranes in which they are located (58, 59). Consistent with this model, IFITM3 is abundant in the membranes of late endosomes and lysosomes, and viruses most affected by IFITM3 (IAVs, filoviruses, flaviviruses, and severe acute respiratory syndrome coronavirus) enter the cells through these compartments, whereas viruses refractory to IFITM3 (arenaviruses and murine leukemia virus) enter at the cell surface or in early endosomes (49, 60). On the basis of this model, a hypothesis was recently put forward by Barclay and colleagues that a high pH optimum of fusion would allow IAV to enter the cell from early rather than late endosomes and by this means reduce the susceptibility of the virus to IFITM3, which mainly resides in the late endosomes (61). Although no evidence exists, to our knowledge, of the entry of IAVs from the early endosomes, this hypothesis matches our finding that the pH optimum of membrane fusion and sensitivity of IAVs to IFITM2 and IFITM3 correlate. In more general terms, one can assume that the pH optimum of membrane fusion modulates IFITM-mediated restriction of IAVs by determining the pattern and duration of virus colocalization with IFITM. In addition to direct effects of membrane-embedded IFITMs at the sites of fusion, IFITM3 can disrupt intracellular cholesterol homeostasis (62) and may thereby alter the fusion competence of cell membranes. It was also shown that IFITMs may interact with and affect the activity of the vacuolar proton ATPase and clathrin, presumably altering the rate or pattern of vesicle acidification and trafficking and/or redirecting viruses to a nonfusogenic pathway (49, 63, 64). It remains to be determined whether these effects of IFITMs on characteristics of intracellular vesicles could contribute to the fusion pH-dependent restriction of IAVs.
The pH optimum of HA-mediated fusion of avian and mammalian IAVs varies depending on the host species and the history of virus evolution, and our study, for the first time, demonstrates that this variation influences viral sensitivity to IFN and IFITMs. Among different IAVs, human viruses typically have the lowest fusion pH optimum (from 5.0 to 5.4), whereas swine viruses and viruses of gallinaceous poultry, including high- and low-pathogenic IAVs of the H5 and H7 subtypes, display relatively high fusion pH optima (5.6 to 6.0) (22, 24, 34–39). IAVs isolated from wild aquatic birds appear to be particularly variable with respect to the fusion pH optimum (from 5.0 to 6.0), although available data are limited (22–24, 37, 38). The optimal membrane fusion pH of IAV is thought to be determined by the interplay between two major host-dependent factors. First, studies of infection of cell cultures suggest that the viral fusion pH has to be compatible with the levels of acidification of the cellular endosomal compartment (37, 65–67). These levels may vary depending on the viral target cells and thus differ in airway epithelial cells of humans and pigs, intestinal epithelial cells of aquatic birds, and various types of cells during systemic infections of various species with highly pathogenic avian IAVs. Second, the fusion pH optimum of the HA affects the environmental stability of IAVs (18, 26, 27), which has to be compatible with ecological and physiological features of the host species and modes of virus transmission (1, 61, 68). For example, studies on the replication and experimental transmission of highly pathogenic H5N1 viruses in ferrets suggested that a relatively high pH optimum of fusion and, hence, reduced stability of these viruses prevented their efficient replication in the upper respiratory tract and transmission by airborne droplets (34, 35, 69).
Infections of humans with most avian and swine IAVs are generally rare and cause only mild, if any, illness (2). In contrast, the avian H5N1 and H7N9 viruses are responsible for the majority of zoonotic IAV infections known to date (856 and 808 cases, respectively), and these infections are associated with unusually high fatality rates (53 and 40%, respectively) (70, 71). Unlike seasonal human IAVs, which mainly replicate in the upper respiratory tract in humans, the H5N1 and H7N9 viruses efficiently replicate in the terminal bronchioles and AECII (72–75), leading to strong infiltration of innate immune cells, induction of high levels of IFN and proinflammatory cytokines, and necrosis of the alveolar epithelium (76, 77). The alveolar tropism and enhanced pathogenicity of the avian H5N1 and H7N9 viruses are believed to be partly associated with the ability of their HAs to bind to Neu5Ac2-3Gal-terminated receptor moieties of type II pneumocytes (reviewed in references 21 and 76). The results of our study, particularly data on viral replication in IFN-treated type II alveolar cells, indicate that the high pH optimum of fusion of the H5N1 and H7N9 viruses reduces their sensitivity to IFN and likely represents another factor contributing to their alveolar tropism, virulence, and increased pathogenicity in humans.
MATERIALS AND METHODS
Cells.
All cells were propagated at 37°C in 5% CO2. MDCK cells, human embryonic kidney 293T cells, human lung adenocarcinoma A549 cells, and human bronchial adenocarcinoma Calu-3 cells were grown in Dulbecco's modified Eagle medium (DMEM; Gibco) supplemented with 10% fetal calf serum (FCS; Gibco), 100 IU ml−1 penicillin and 100 μg ml−1 streptomycin (pen-strep), and 2 mM glutamine.
MDCK cells stably expressing human IFITM2 and IFITM3 (MDCK-IFITM2 and MDCK-IFITM3) were generated by transducing wild-type cells with bicistronic expression plasmids pQCXIP-IFITM2 and pQCXIP-IFITM3, which were described previously (12, 78). Stably transduced cells were selected with puromycin (5 μg ml−1) and passaged as a pool in the MDCK growth medium described above supplemented with puromycin. The expression of IFITM2 and IFITM3 was verified by immunoblot analysis employing a polyclonal IFITM2 antiserum, which is cross-reactive with IFITM3 (12769-1-AP; Proteintech, Chicago, IL, USA). In addition, the antiviral activity of the stably expressed IFITM proteins was confirmed by employing IAV carrying Gaussia luciferase as described elsewhere (78).
Differentiated cultures of primary HTBE cells were prepared as described previously (29, 44). In brief, commercial primary HTBE cells (Lonza) were expanded on plastic and stored in aliquots in liquid nitrogen. Thawed passage 1 cells were used to seed membrane supports (12-mm Transwell-Clear; pore size, 0.4 μm; Corning) in a 1:1 mixture of DMEM and serum-free and hormone- and growth factor-supplemented bronchial epithelial cell growth medium (BEGM; Lonza). After 1 week, the medium was removed from the upper compartment and cells were maintained under ALI conditions by changing the medium in the lower compartment every other day. Fully differentiated 5- to 7-week-old cultures were used for the experiments.
Human lung tissue was obtained from lobectomy specimens distal from tumors after informed written patient consent. Human AECII were isolated as described previously (79). The purity of the cells was assessed by using anti-CD45, anti-CD326/EpCam, and anti-pro-SP-C antibodies (BioLegend, Netherlands; Millipore, Germany). Suspensions with an AECII content of >95% were used to seed 6.5-mm Transwell-Clear membrane supports (pore size, 0.4 μm; Corning) in Ham's F12 medium (Biochrom, Germany) supplemented with 10% FCS and antibiotics. Four to 6 days later, the cells reached confluence and were used in experiments.
Wild-type influenza viruses.
H1N1/2009 pandemic virus A/Hamburg/5/2009 was from the repository of the Institute of Virology, Philipps University, Marburg, Germany. A/Memphis/14/1996 (H1N1) and A/mallard/Alberta/119/1998 (H1N1) were provided by Robert Webster, St. Jude Children's Research Hospital, Memphis, TN, USA. A/Thailand/KAN-1/2004 (H5N1), A/Anhui/1/2013 (H7N9), and A/Hong Kong/1/1968 (H3N2) were provided by Pilaipan Puthavathana, Mahidol University, Bangkok, Thailand; John McCauley, Crick Worldwide Influenza Centre, London, United Kingdom; and Earl Brown, University of Ottawa, Ottawa, Ontario, Canada, respectively. The mallard virus was propagated in 11-day-old embryonated chicken eggs; the other viruses were grown in MDCK cells.
All experiments with the wild-type H5N1 and H7N9 viruses were conducted in a biosafety level 3 (BSL3) laboratory in accordance with German law (Gesetz zur Regelung der Gentechnik and Verordnung über die Sicherheitsstufen und Sicherheitsmaßnahmen bei gentechnischen Arbeiten in gentechnischen Anlagen).
Plasmids and recombinant viruses.
Reverse genetics plasmid pHW2000, pHW2000 plasmids containing six gene segments of PR8, and pHW2000 plasmids containing the HA- and NA-encoding genes of A/Vietnam/1203/2004 (H5N1) were kindly provided by Richard Webby and Robert Webster (St. Jude Children's Research Hospital, Memphis, TN, USA). The HA of the H5N1 virus contained a deletion of the polybasic cleavage site introduced by mutagenesis. The plasmids containing the HA- and NA-encoding genes of A/mallard/New York/6750/1978 (H2N2) were kindly provided by Yoshihiro Kawaoka, University of Wisconsin—Madison, Madison, WI, USA. The HA- and NA-encoding genes of A/Shanghai/2/2013 (H7N9) (Global Initiative on Sharing Avian Influenza Data [GISAID], accession numbers EPI439502 and EPI439500) were synthesized commercially (GenScript Corporation, Piscataway, NJ). The HA- and NA-encoding genes of A/Memphis/14/1996 (H1N1) and A/mallard/Alberta/1998 (H1N1) were amplified from isolated RNA by reverse transcription-PCR with a set of universal primers and ligated into the pHW2000 plasmid as described previously (80). pHW2000 plasmids containing the HA- and NA-encoding genes of A/Hong Kong/1/1968 (H3N2) were prepared previously (30). Mutations were introduced into the HA plasmid of A/Hong Kong/1/1968 with a site-directed mutagenesis kit (QuikChange; Stratagene).
2:6 recombinant viruses were generated by eight-plasmid reverse genetics (80). In brief, pHW2000 plasmids containing the HA- and NA-encoding genes of choice and the remaining six genes of PR8 were transfected into 293T cells by using Lipofectamine 2000 (Invitrogen). After 2 days, rescued viruses were amplified in either MDCK cells (A/Memphis/14/1996-PR8 and A/Vietnam/1203/2004-PR8) or 11-day-old embryonated hen's eggs (all other recombinant viruses), clarified by low-speed centrifugation, and stored in aliquots at −80°C. The identities of the HA- and NA-encoding genes of all viruses were confirmed by sequencing.
Single-cycle focus formation assay.
Viral titers were determined in A549, MDCK, MDCK-IFITM2, and MDCK-IFITM3 cells by infecting the cells in 96-well plates with 0.1-ml volumes of serial 10-fold dilutions of viruses in DMEM containing 0.1% bovine serum albumin (PAA Laboratories), pen-strep, and 2 mM glutamine (infection medium [IM]). No trypsin was added to the medium in order to limit the infection to one replication cycle. The cultures were incubated overnight and fixed. Viruses were titrated in Calu-3 cells by using 24-well plates. As Calu-3 cells support multicycle viral replication in the absence of trypsin (81), the infection time was limited to 8 h. Virus-infected cells were detected in all fixed cultures by immunostaining for viral NP as described previously (30). Numbers of infected cells per well were determined under a microscope for the virus dilutions that produced 30 to 300 infected cells per well and recalculated into numbers of focus-forming units (FFU) per milliliter of undiluted viral suspension.
Low-pH-induced conformational transition of HA.
The assay used to determine the low-pH-induced conformational transition of HA was described previously (43). It determines changes in the HA sensitivity to protease digestion that accompany the conformational transition. In brief, viruses adsorbed to the wells of a microtiter plate were incubated in either phosphate-buffered saline (PBS) or 0.1 M sodium acetate low-pH buffers for 15 min at 37°C and then washed with PBS and incubated with 0.1 mg/ml of proteinase K in PBS for 1 h at 37°C. After washing, the binding of peroxidase-labeled fetuin to the viruses was determined and expressed as percentages of low-pH-exposed virus with respect to the PBS-exposed control. Binding-versus-pH curves were plotted, and pH values that corresponded to 50% HA inactivation (pH50-HA) were determined by linear interpolation.
Inhibition of viral cell entry by ammonium chloride.
The assay used to measure inhibition of viral cell entry by ammonium chloride was described in detail elsewhere (24). In brief, MDCK cells in 96-well plates were infected with the viruses in the presence of various concentrations of NH4Cl, incubated overnight, fixed, and immunostained for viral NP. Numbers of infected cells per culture were determined and were expressed as percentages of those of cultures infected in the absence of NH4Cl. The dose-response curves were plotted, and concentrations of NH4Cl that inhibited infection by 50% (IC50s) were determined by linear interpolation.
Inactivation of viral infectivity at acidic pH.
The assay used to determine the inactivation of viral infectivity at acidic pH was described elsewhere (24). In brief, viral stocks were diluted in morpholineethanesulfonic acid (MES)-buffered saline at pHs ranging from 5.0 to 7.0, incubated for 15 min at 37°C, neutralized, and titrated with a single-cycle assay in MDCK cells. Two technical replicates were used for the titration of each sample, and results were averaged. The titers of low-pH-treated viruses were expressed as percentages of the titers of viruses that were incubated at pH 7. Infectivity-versus-pH curves were plotted, and pH values that corresponded to virus inactivation by 50% (pH50-inact) were determined by linear interpolation.
Single-cycle infection of IFN-treated cells.
Replicate cultures of A549 cells in 96-well plates and Calu-3 cells in 24-well plates were stimulated for 24 h by adding recombinant human IFN-β (Betaferon; Schering) at 0 to 1,000 U/ml of cell growth medium. In one experiment with A459 cells (Fig. 5), recombinant human IFN-α and IFN-λ1 (both from PeproTech, Inc.) were used at concentrations ranging from 0.001 to 100 ng/ml. The IFN-stimulated cells were washed three times with PBS containing Ca2+ and Mg2+ (PBS++), inoculated with dilutions of 2:6 recombinant viruses in IM producing about 200 foci of infected cells per culture, and incubated either for 8 h (Calu-3) or overnight (A549). Infections of A549 cells in experiments with wild-type viruses were limited to 8 h to avoid multicycle replication of A/Thailand/KAN-1/2004 (H5N1), which contained a multibasic cleavage site. Following incubation, the cultures were fixed and immunostained for viral NP, and numbers of infected cells per IFN-treated culture were expressed as percentages of those of the control cultures that were incubated without IFN.
Cultures of AECII were stimulated for 24 h by adding 0, 2, or 20 U/ml IFN-β to fresh growth medium in both the apical and basolateral compartments. The cells were then washed twice with the basal medium (Ham's F12). The apical compartments were inoculated with 2 × 104 FFU of the viruses (based on titers determined in MDCK cells) in 0.1 ml of the basal medium supplemented with 0.1% bovine serum albumin. The same medium without the virus was added to the basolateral compartments (0.5 ml of per culture). The cultures were incubated for 8 h, fixed with 4% paraformaldehyde for 30 min at 4°C, and immunostained for viral NP. The cultures were analyzed en face at a magnification of ×300 with an inverted microscope (IMT-2; Olympus, Japan). The total number of cells expressing viral antigen was determined in the epithelial segment that included all consecutive microscopic views (0.28 by 0.42 mm each) along the diameter of the culture. Three or four segments per culture (technical replicates) were counted by rotating the culture clockwise by 45°, and the data were averaged. Three replicate cultures were used for each condition on the same day. The numbers of infected cells per segment of IFN-treated cultures were expressed as percentages of those of the control cultures that were incubated without IFN.
HTBE cultures were stimulated for 24 h with 20 U ml−1 IFN-β added to the freshly changed growth medium in the basolateral compartments. Control cultures were incubated without IFN. The apical surfaces of the cultures were washed 10 times with PBS++ and inoculated with 6 × 105 FFU of the viruses (based on titers determined in MDCK cells) in 0.2 ml of the growth medium. One hour postinfection, the virus inoculum was removed and cultures were incubated at the ALI for an additional 7 h. The cultures were then fixed, immunostained, and analyzed as described above for AECII cultures. Two replicate experiments were performed with series of HTBE cultures differentiated on different occasions from cells from the same donor. The third experiment was performed with cultures prepared with cells from a different donor.
Plaque assay.
Viruses were titrated in MDCK, MDCK-IFITM2, and MDCK-IFITM-3 cells in six-well plates by plaque assay under semisolid overlay medium with immunostaining as described previously (82). The titers were expressed in PFU per milliliter of viral suspension. Plate wells containing 5 to 50 plaques were scanned with a flat-bed scanner. The plaque diameters were measured with the Ruler Tool of Adobe Photoshop CS3 software version 10.0.1 and expressed as percentages of the mean plaque diameter in MDCK cells.
Multicycle replication in IFN-treated Calu-3 cells.
Replicate cultures of Calu-3 cells in 24-well plates were stimulated with IFN for 24 h as described above for single-cycle infections. The cells were washed two times with PBS++ and inoculated with 2.5 × 103 PFU (based on titers determined in MDCK cells) of 2:6 recombinant viruses in 0.3 ml of IM. After incubation for 1 h at 37°C, the inocula were removed and replaced with 0.8 ml of IM containing the same concentrations of IFN that were used for stimulation. Samples of cell supernatants (0.1 ml) were collected daily, stored frozen at −80°C, and titrated by focus formation assay in MDCK cells.
Statistics.
All data are shown as mean values and standard deviations of biological replicates (the details are explained in the table footnotes and figure legends). The statistical significance of the differences between groups was estimated with a two-tailed unpaired Student t test, and P values are indicated as follows in the figures: *, P < 0.05; **, P < 0.01; ***, P < 0.001.
ACKNOWLEDGMENTS
This study was supported by the German Research Foundation (DFG) (SFB 1021 projects B02, B06, and C05; SFB-TR84 project B2; KFO 309 projects P1, P2, and P8), the Leibniz Foundation (Graduate School for Emerging Infectious Diseases [EIDIS]), and the European Union's Seventh Framework Programme for Research, Technological Development, and Demonstration under grant agreement 278433-PREDEMICS.
We thank Abraham Brass, Earl Brown, John McCauley, Yoshi Kawaoka, Pilaipan Puthavathana, Richard Webby, and Robert Webster for providing viruses and plasmids. We are grateful to Peter Staeheli for stimulating discussions and to Jan Baumann and Markus Eickmann for facilitating experiments conducted in the BSL3 laboratory.
REFERENCES
- 1.Reperant LA, Kuiken T, Osterhaus AD. 2012. Adaptive pathways of zoonotic influenza viruses: from exposure to establishment in humans. Vaccine 30:4419–4434. doi: 10.1016/j.vaccine.2012.04.049. [DOI] [PubMed] [Google Scholar]
- 2.Freidl GS, Meijer A, de Bruin E, de Nardi M, Munoz O, Capua I, Breed AC, Harris K, Hill A, Kosmider R, Banks J, von Dobschuetz S, Stark K, Wieland B, Stevens K, van der Werf S, Enouf V, van der Meulen K, van Reeth K, Dauphin G, Koopmans M, FLURISK Consortium . 2014. Influenza at the animal-human interface: a review of the literature for virological evidence of human infection with swine or avian influenza viruses other than A(H5N1). Euro Surveill 19:20793 http://www.eurosurveillance.org/ViewArticle.aspx?ArticleId=20793. doi: 10.2807/1560-7917.ES2014.19.18.20793. [DOI] [PubMed] [Google Scholar]
- 3.Munoz O, De Nardi M, van der Meulen K, van Reeth K, Koopmans M, Harris K, von Dobschuetz S, Freidl G, Meijer A, Breed A, Hill A, Kosmider R, Banks J, Stark KD, Wieland B, Stevens K, van der Werf S, Enouf V, Dauphin G, Dundon W, Cattoli G, Capua I. 2016. Genetic adaptation of influenza A viruses in domestic animals and their potential role in interspecies transmission: a literature review. Ecohealth 13:171–198. doi: 10.1007/s10393-014-1004-1. [DOI] [PubMed] [Google Scholar]
- 4.Neumann G, Kawaoka Y. 2015. Transmission of influenza A viruses. Virology 479–480:234–246. doi: 10.1016/j.virol.2015.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Taubenberger JK, Kash JC. 2010. Influenza virus evolution, host adaptation, and pandemic formation. Cell Host Microbe 7:440–451. doi: 10.1016/j.chom.2010.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Saunders-Hastings PR, Krewski D. 2016. Reviewing the history of pandemic influenza: understanding patterns of emergence and transmission. Pathogens 5:E66. doi: 10.3390/pathogens5040066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Randall RE, Goodbourn S. 2008. Interferons and viruses: an interplay between induction, signalling, antiviral responses and virus countermeasures. J Gen Virol 89:1–47. doi: 10.1099/vir.0.83391-0. [DOI] [PubMed] [Google Scholar]
- 8.García-Sastre A. 2011. Induction and evasion of type I interferon responses by influenza viruses. Virus Res 162:12–18. doi: 10.1016/j.virusres.2011.10.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Weber-Gerlach M, Weber F. 2016. To conquer the host, influenza virus is packing it in: interferon-antagonistic strategies beyond NS1. J Virol 90:8389–8394. doi: 10.1128/JVI.00041-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schoggins JW. 2014. Interferon-stimulated genes: roles in viral pathogenesis. Curr Opin Virol 6:40–46. doi: 10.1016/j.coviro.2014.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schneider WM, Chevillotte MD, Rice CM. 2014. Interferon-stimulated genes: a complex web of host defenses. Annu Rev Immunol 32:513–545. doi: 10.1146/annurev-immunol-032713-120231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Brass AL, Huang IC, Benita Y, John SP, Krishnan MN, Feeley EM, Ryan BJ, Weyer JL, van der Weyden L, Fikrig E, Adams DJ, Xavier RJ, Farzan M, Elledge SJ. 2009. The IFITM proteins mediate cellular resistance to influenza A H1N1 virus, West Nile virus, and dengue virus. Cell 139:1243–1254. doi: 10.1016/j.cell.2009.12.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bailey CC, Zhong G, Huang IC, Farzan M. 2014. IFITM-family proteins: the cell's first line of antiviral defense. Annu Rev Virol 1:261–283. doi: 10.1146/annurev-virology-031413-085537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ayllon J, García-Sastre A. 2015. The NS1 protein: a multitasking virulence factor. Curr Top Microbiol Immunol 386:73–107. doi: 10.1007/82_2014_400. [DOI] [PubMed] [Google Scholar]
- 15.Dittmann J, Stertz S, Grimm D, Steel J, García-Sastre A, Haller O, Kochs G. 2008. Influenza A virus strains differ in sensitivity to the antiviral action of Mx-GTPase. J Virol 82:3624–3631. doi: 10.1128/JVI.01753-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mänz B, Dornfeld D, Gotz V, Zell R, Zimmermann P, Haller O, Kochs G, Schwemmle M. 2013. Pandemic influenza A viruses escape from restriction by human MxA through adaptive mutations in the nucleoprotein. PLoS Pathog 9:e1003279. doi: 10.1371/journal.ppat.1003279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wiley DC, Skehel JJ. 1987. The structure and function of the hemagglutinin membrane glycoprotein of influenza virus. Annu Rev Biochem 56:365–394. [DOI] [PubMed] [Google Scholar]
- 18.Skehel JJ, Wiley DC. 2000. Receptor binding and membrane fusion in virus entry: the influenza hemagglutinin. Annu Rev Biochem 69:531–569. doi: 10.1146/annurev.biochem.69.1.531. [DOI] [PubMed] [Google Scholar]
- 19.Klenk HD, Garten W, Matrosovich M. 2013. Pathogenesis, p 157–172. In Webster RG. (ed), Textbook of influenza. John Wiley & Sons, Ltd., Chichester, West Sussex, United Kingdom. [Google Scholar]
- 20.Xiong X, McCauley JW, Steinhauer DA. 2014. Receptor binding properties of the influenza virus hemagglutinin as a determinant of host range. Curr Top Microbiol Immunol 385:63–91. doi: 10.1007/82_2014_423. [DOI] [PubMed] [Google Scholar]
- 21.de Graaf M, Fouchier RA. 2014. Role of receptor binding specificity in influenza A virus transmission and pathogenesis. EMBO J 33:823–841. doi: 10.1002/embj.201387442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Galloway SE, Reed ML, Russell CJ, Steinhauer DA. 2013. Influenza HA subtypes demonstrate divergent phenotypes for cleavage activation and pH of fusion: implications for host range and adaptation. PLoS Pathog 9:e1003151. doi: 10.1371/journal.ppat.1003151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Russier M, Yang G, Rehg JE, Wong SS, Mostafa HH, Fabrizio TP, Barman S, Krauss S, Webster RG, Webby RJ, Russell CJ. 2016. Molecular requirements for a pandemic influenza virus: an acid-stable hemagglutinin protein. Proc Natl Acad Sci USA 113:1636–1641. doi: 10.1073/pnas.1524384113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Baumann J, Kouassi NM, Foni E, Klenk HD, Matrosovich M. 2015. H1N1 swine influenza viruses differ from avian precursors by a higher pH optimum of membrane fusion. J Virol 90:1569–1577. doi: 10.1128/JVI.02332-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cauldwell AV, Long JS, Moncorge O, Barclay WS. 2014. Viral determinants of influenza A virus host range. J Gen Virol 95:1193–1210. doi: 10.1099/vir.0.062836-0. [DOI] [PubMed] [Google Scholar]
- 26.Russell CJ. 2014. Acid-induced membrane fusion by the hemagglutinin protein and its role in influenza virus biology. Curr Top Microbiol Immunol 385:93–116. doi: 10.1007/82_2014_393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mair CM, Ludwig K, Herrmann A, Sieben C. 2014. Receptor binding and pH stability—how influenza A virus hemagglutinin affects host-specific virus infection. Biochim Biophys Acta 1838:1153–1168. doi: 10.1016/j.bbamem.2013.10.004. [DOI] [PubMed] [Google Scholar]
- 28.Wagner R, Matrosovich M, Klenk HD. 2002. Functional balance between haemagglutinin and neuraminidase in influenza virus infections. Rev Med Virol 12:159–166. doi: 10.1002/rmv.352. [DOI] [PubMed] [Google Scholar]
- 29.Matrosovich MN, Matrosovich TY, Gray T, Roberts NA, Klenk HD. 2004. Human and avian influenza viruses target different cell types in cultures of human airway epithelium. Proc Natl Acad Sci USA 101:4620–4624. doi: 10.1073/pnas.0308001101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Matrosovich M, Matrosovich T, Uhlendorff J, Garten W, Klenk HD. 2007. Avian-virus-like receptor specificity of the hemagglutinin impedes influenza virus replication in cultures of human airway epithelium. Virology 361:384–390. doi: 10.1016/j.virol.2006.11.030. [DOI] [PubMed] [Google Scholar]
- 31.Matrosovich M, Tuzikov A, Bovin N, Gambaryan A, Klimov A, Castrucci MR, Donatelli I, Kawaoka Y. 2000. Early alterations of the receptor-binding properties of H1, H2, and H3 avian influenza virus hemagglutinins after their introduction into mammals. J Virol 74:8502–8512. doi: 10.1128/JVI.74.18.8502-8512.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gambaryan A, Tuzikov A, Pazynina G, Bovin N, Balish A, Klimov A. 2006. Evolution of the receptor binding phenotype of influenza A (H5) viruses. Virology 344:432–438. doi: 10.1016/j.virol.2005.08.035. [DOI] [PubMed] [Google Scholar]
- 33.Shi Y, Zhang W, Wang F, Qi J, Wu Y, Song H, Gao F, Bi Y, Zhang Y, Fan Z, Qin C, Sun H, Liu J, Haywood J, Liu W, Gong W, Wang D, Shu Y, Wang Y, Yan J, Gao GF. 2013. Structures and receptor binding of hemagglutinins from human-infecting H7N9 influenza viruses. Science 342:243–247. doi: 10.1126/science.1242917. [DOI] [PubMed] [Google Scholar]
- 34.Imai M, Watanabe T, Hatta M, Das SC, Ozawa M, Shinya K, Zhong G, Hanson A, Katsura H, Watanabe S, Li C, Kawakami E, Yamada S, Kiso M, Suzuki Y, Maher EA, Neumann G, Kawaoka Y. 2012. Experimental adaptation of an influenza H5 HA confers respiratory droplet transmission to a reassortant H5 HA/H1N1 virus in ferrets. Nature 486:420–428. doi: 10.1038/nature10831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Linster M, van Boheemen S, de Graaf M, Schrauwen EJ, Lexmond P, Mänz B, Bestebroer TM, Baumann J, van Riel D, Rimmelzwaan GF, Osterhaus AD, Matrosovich M, Fouchier RA, Herfst S. 2014. Identification, characterization, and natural selection of mutations driving airborne transmission of A/H5N1 virus. Cell 157:329–339. doi: 10.1016/j.cell.2014.02.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gabbard JD, Dlugolenski D, van Riel D, Marshall N, Galloway SE, Howerth EW, Campbell PJ, Jones C, Johnson S, Byrd-Leotis L, Steinhauer DA, Kuiken T, Tompkins SM, Tripp R, Lowen AC, Steel J. 2014. Novel H7N9 influenza virus shows low infectious dose, high growth rate, and efficient contact transmission in the guinea pig model. J Virol 88:1502–1512. doi: 10.1128/JVI.02959-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Daidoji T, Watanabe Y, Ibrahim MS, Yasugi M, Maruyama H, Masuda T, Arai F, Ohba T, Honda A, Ikuta K, Nakaya T. 2015. Avian influenza virus infection of immortalized human respiratory epithelial cells depends upon a delicate balance between hemagglutinin acid stability and endosomal pH. J Biol Chem 290:10627–10642. doi: 10.1074/jbc.M114.611327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Okamatsu M, Motohashi Y, Hiono T, Tamura T, Nagaya K, Matsuno K, Sakoda Y, Kida H. 2016. Is the optimal pH for membrane fusion in host cells by avian influenza viruses related to host range and pathogenicity? Arch Virol 161:2235–2242. doi: 10.1007/s00705-016-2902-z. [DOI] [PubMed] [Google Scholar]
- 39.Schrauwen EJ, Richard M, Burke DF, Rimmelzwaan GF, Herfst S, Fouchier RA. 2016. Amino acid substitutions that affect receptor binding and stability of the hemagglutinin of influenza A/H7N9 virus. J Virol 90:3794–3799. doi: 10.1128/JVI.03052-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Rott R, Orlich M, Klenk HD, Wang ML, Skehel JJ, Wiley DC. 1984. Studies on the adaptation of influenza viruses to MDCK cells. EMBO J 3:3329–3332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lin YP, Wharton SA, Martin J, Skehel JJ, Wiley DC, Steinhauer DA. 1997. Adaptation of egg-grown and transfectant influenza viruses for growth in mammalian cells: selection of hemagglutinin mutants with elevated pH of membrane fusion. Virology 233:402–410. doi: 10.1006/viro.1997.8626. [DOI] [PubMed] [Google Scholar]
- 42.Thoennes S, Li ZN, Lee BJ, Langley WA, Skehel JJ, Russell RJ, Steinhauer DA. 2008. Analysis of residues near the fusion peptide in the influenza hemagglutinin structure for roles in triggering membrane fusion. Virology 370:403–414. doi: 10.1016/j.virol.2007.08.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Van Poucke S, Doedt J, Baumann J, Qiu Y, Matrosovich T, Klenk HD, Van Reeth K, Matrosovich M. 2015. Role of substitutions in the hemagglutinin in the emergence of the 1968 pandemic influenza virus. J Virol 89:12211–12216. doi: 10.1128/JVI.01292-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gray TE, Guzman K, Davis CW, Abdullah LH, Nettesheim P. 1996. Mucociliary differentiation of serially passaged normal human tracheobronchial epithelial cells. Am J Respir Cell Mol Biol 14:104–112. doi: 10.1165/ajrcmb.14.1.8534481. [DOI] [PubMed] [Google Scholar]
- 45.Matrosovich MN, Matrosovich TY, Gray T, Roberts NA, Klenk HD. 2004. Neuraminidase is important for the initiation of influenza virus infection in human airway epithelium. J Virol 78:12665–12667. doi: 10.1128/JVI.78.22.12665-12667.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Mordstein M, Neugebauer E, Ditt V, Jessen B, Rieger T, Falcone V, Sorgeloos F, Ehl S, Mayer D, Kochs G, Schwemmle M, Gunther S, Drosten C, Michiels T, Staeheli P. 2010. Lambda interferon renders epithelial cells of the respiratory and gastrointestinal tracts resistant to viral infections. J Virol 84:5670–5677. doi: 10.1128/JVI.00272-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ehrhardt C, Seyer R, Hrincius ER, Eierhoff T, Wolff T, Ludwig S. 2010. Interplay between influenza A virus and the innate immune signaling. Microbes Infect 12:81–87. doi: 10.1016/j.micinf.2009.09.007. [DOI] [PubMed] [Google Scholar]
- 48.Perreira JM, Chin CR, Feeley EM, Brass AL. 2013. IFITMs restrict the replication of multiple pathogenic viruses. J Mol Biol 425:4937–4955. doi: 10.1016/j.jmb.2013.09.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Diamond MS, Farzan M. 2013. The broad-spectrum antiviral functions of IFIT and IFITM proteins. Nat Rev Immunol 13:46–57. doi: 10.1038/nri3344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bailey CC, Huang IC, Kam C, Farzan M. 2012. IFITM3 limits the severity of acute influenza in mice. PLoS Pathog 8:e1002909. doi: 10.1371/journal.ppat.1002909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Everitt AR, Clare S, Pertel T, John SP, Wash RS, Smith SE, Chin CR, Feeley EM, Sims JS, Adams DJ, Wise HM, Kane L, Goulding D, Digard P, Anttila V, Baillie JK, Walsh TS, Hume DA, Palotie A, Xue Y, Colonna V, Tyler-Smith C, Dunning J, Gordon SB, GenISIS Investigators, MOSAIC Investigators, Smyth RL, Openshaw PJ, Dougan G, Brass AL, Kellam P. 2012. IFITM3 restricts the morbidity and mortality associated with influenza. Nature 484:519–523. doi: 10.1038/nature10921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Zhang Y-H, Zhao Y, Li N, Peng Y-C, Giannoulatou E, Jin R-H, Yan H-P, Wu H, Liu J-H, Liu N, Wang D-Y, Shu Y-L, Ho L-P, Kellam P, McMichael A, Dong T. 2013. Interferon-induced transmembrane protein-3 genetic variant rs12252-C is associated with severe influenza in Chinese individuals. Nat Commun 4:1418. doi: 10.1038/ncomms2433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Wang Z, Zhang A, Wan Y, Liu X, Qiu C, Xi X, Ren Y, Wang J, Dong Y, Bao M, Li L, Zhou M, Yuan S, Sun J, Zhu Z, Chen L, Li Q, Zhang Z, Zhang X, Lu S, Doherty PC, Kedzierska K, Xu J. 2014. Early hypercytokinemia is associated with interferon-induced transmembrane protein-3 dysfunction and predictive of fatal H7N9 infection. Proc Natl Acad Sci USA 111:769–774. doi: 10.1073/pnas.1321748111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Yang X, Tan B, Zhou X, Xue J, Zhang X, Wang P, Shao C, Li Y, Li C, Xia H, Qiu J. 2015. Interferon-inducible transmembrane protein 3 genetic variant rs12252 and influenza susceptibility and severity: a meta-analysis. PLoS One 10:e0124985. doi: 10.1371/journal.pone.0124985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.López-Rodríguez M, Herrera-Ramos E, Sole-Violan J, Ruiz-Hernandez JJ, Borderias L, Horcajada JP, Lerma-Chippirraz E, Rajas O, Briones M, Perez-Gonzalez MC, García-Bello MA, Lopez-Granados E, Rodriguez de Castro F, Rodriguez-Gallego C. 2016. IFITM3 and severe influenza virus infection. No evidence of genetic association. Eur J Clin Microbiol Infect Dis 35:1811–1817. doi: 10.1007/s10096-016-2732-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Lin TY, Chin CR, Everitt AR, Clare S, Perreira JM, Savidis G, Aker AM, John SP, Sarlah D, Carreira EM, Elledge SJ, Kellam P, Brass AL. 2013. Amphotericin B increases influenza A virus infection by preventing IFITM3-mediated restriction. Cell Rep 5:895–908. doi: 10.1016/j.celrep.2013.10.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Liu SY, Aliyari R, Chikere K, Li G, Marsden MD, Smith JK, Pernet O, Guo H, Nusbaum R, Zack JA, Freiberg AN, Su L, Lee B, Cheng G. 2013. Interferon-inducible cholesterol-25-hydroxylase broadly inhibits viral entry by production of 25-hydroxycholesterol. Immunity 38:92–105. doi: 10.1016/j.immuni.2012.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Li K, Markosyan RM, Zheng YM, Golfetto O, Bungart B, Li M, Ding S, He Y, Liang C, Lee JC, Gratton E, Cohen FS, Liu SL. 2013. IFITM proteins restrict viral membrane hemifusion. PLoS Pathog 9:e1003124. doi: 10.1371/journal.ppat.1003124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Desai TM, Marin M, Chin CR, Savidis G, Brass AL, Melikyan GB. 2014. IFITM3 restricts influenza A virus entry by blocking the formation of fusion pores following virus-endosome hemifusion. PLoS Pathog 10:e1004048. doi: 10.1371/journal.ppat.1004048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Feeley EM, Sims JS, John SP, Chin CR, Pertel T, Chen LM, Gaiha GD, Ryan BJ, Donis RO, Elledge SJ, Brass AL. 2011. IFITM3 inhibits influenza A virus infection by preventing cytosolic entry. PLoS Pathog 7:e1002337. doi: 10.1371/journal.ppat.1002337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Long JS, Benfield CT, Barclay WS. 2015. One-way trip: influenza virus' adaptation to gallinaceous poultry may limit its pandemic potential. Bioessays 37:204–212. doi: 10.1002/bies.201400133. [DOI] [PubMed] [Google Scholar]
- 62.Amini-Bavil-Olyaee S, Choi YJ, Lee JH, Shi M, Huang IC, Farzan M, Jung JU. 2013. The antiviral effector IFITM3 disrupts intracellular cholesterol homeostasis to block viral entry. Cell Host Microbe 13:452–464. doi: 10.1016/j.chom.2013.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Wee YS, Roundy KM, Weis JJ, Weis JH. 2012. Interferon-inducible transmembrane proteins of the innate immune response act as membrane organizers by influencing clathrin and v-ATPase localization and function. Innate Immun 18:834–845. doi: 10.1177/1753425912443392. [DOI] [PubMed] [Google Scholar]
- 64.Anafu AA, Bowen CH, Chin CR, Brass AL, Holm GH. 2013. Interferon-inducible transmembrane protein 3 (IFITM3) restricts reovirus cell entry. J Biol Chem 288:17261–17271. doi: 10.1074/jbc.M112.438515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Marvin SA, Russier M, Huerta CT, Russell CJ, Schultz-Cherry S. 2017. Influenza virus overcomes cellular blocks to productively replicate, impacting macrophage function. J Virol 91:e01417–. doi: 10.1128/JVI.01417-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Murakami S, Horimoto T, Ito M, Takano R, Katsura H, Shimojima M, Kawaoka Y. 2012. Enhanced growth of influenza vaccine seed viruses in Vero cells mediated by broadening the optimal pH range for virus membrane fusion. J Virol 86:1405–1410. doi: 10.1128/JVI.06009-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Zaraket H, Bridges OA, Duan S, Baranovich T, Yoon SW, Reed ML, Salomon R, Webby RJ, Webster RG, Russell CJ. 2013. Increased acid stability of the hemagglutinin protein enhances H5N1 influenza virus growth in the upper respiratory tract but is insufficient for transmission in ferrets. J Virol 87:9911–9922. doi: 10.1128/JVI.01175-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Stallknecht DE, Brown JD. 2009. Tenacity of avian influenza viruses. Rev Sci Tech 28:59–67. [DOI] [PubMed] [Google Scholar]
- 69.Krenn BM, Egorov A, Romanovskaya-Romanko E, Wolschek M, Nakowitsch S, Ruthsatz T, Kiefmann B, Morokutti A, Humer J, Geiler J, Cinatl J, Michaelis M, Wressnigg N, Sturlan S, Ferko B, Batishchev OV, Indenbom AV, Zhu R, Kastner M, Hinterdorfer P, Kiselev O, Muster T, Romanova J. 2011. Single HA2 mutation increases the infectivity and immunogenicity of a live attenuated H5N1 intranasal influenza vaccine candidate lacking NS1. PLoS One 6:e18577. doi: 10.1371/journal.pone.0018577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.WHO. 2016. Cumulative number of confirmed human cases for avian influenza A(H5N1) reported to WHO, 2003–2016. World Health Organization, Geneva, Switzerland: http://www.who.int/influenza/human_animal_interface/2016_12_19_tableH5N1.pdf?ua=1. [Google Scholar]
- 71.WHO. 2016. Influenza at the human-animal interface. Summary and assessment, 22 November to 19 December 2016. World Health Organization, Geneva, Switzerland: http://www.who.int/influenza/human_animal_interface/Influenza_Summary_IRA_HA_interface_12_19_2016.pdf. [Google Scholar]
- 72.Uiprasertkul M, Puthavathana P, Sangsiriwut K, Pooruk P, Srisook K, Peiris M, Nicholls JM, Chokephaibulkit K, Vanprapar N, Auewarakul P. 2005. Influenza A H5N1 replication sites in humans. Emerg Infect Dis 11:1036–1041. doi: 10.3201/eid1107.041313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Korteweg C, Gu J. 2010. Pandemic influenza A (H1N1) virus infection and avian influenza A (H5N1) virus infection: a comparative analysis. Biochem Cell Biol 88:575–587. doi: 10.1139/O10-017. [DOI] [PubMed] [Google Scholar]
- 74.Weinheimer VK, Becher A, Tonnies M, Holland G, Knepper J, Bauer TT, Schneider P, Neudecker J, Ruckert JC, Szymanski K, Temmesfeld-Wollbrueck B, Gruber AD, Bannert N, Suttorp N, Hippenstiel S, Wolff T, Hocke AC. 2012. Influenza A viruses target type II pneumocytes in the human lung. J Infect Dis 206:1685–1694. doi: 10.1093/infdis/jis455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Knepper J, Schierhorn KL, Becher A, Budt M, Tonnies M, Bauer TT, Schneider P, Neudecker J, Ruckert JC, Gruber AD, Suttorp N, Schweiger B, Hippenstiel S, Hocke AC, Wolff T. 2013. The novel human influenza A(H7N9) virus is naturally adapted to efficient growth in human lung tissue. mBio 4:e00601–. doi: 10.1128/mBio.00601-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Kuiken T, Riteau B, Fouchier RA, Rimmelzwaan GF. 2012. Pathogenesis of influenza virus infections: the good, the bad and the ugly. Curr Opin Virol 2:276–286. doi: 10.1016/j.coviro.2012.02.013. [DOI] [PubMed] [Google Scholar]
- 77.Short KR, Kroeze EJ, Fouchier RA, Kuiken T. 2014. Pathogenesis of influenza-induced acute respiratory distress syndrome. Lancet Infect Dis 14:57–69. doi: 10.1016/S1473-3099(13)70286-X. [DOI] [PubMed] [Google Scholar]
- 78.Eckert N, Wrensch F, Gartner S, Palanisamy N, Goedecke U, Jager N, Pohlmann S, Winkler M. 2014. Influenza A virus encoding secreted Gaussia luciferase as useful tool to analyze viral replication and its inhibition by antiviral compounds and cellular proteins. PLoS One 9:e97695. doi: 10.1371/journal.pone.0097695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Högner K, Wolff T, Pleschka S, Plog S, Gruber AD, Kalinke U, Walmrath HD, Bodner J, Gattenlohner S, Lewe-Schlosser P, Matrosovich M, Seeger W, Lohmeyer J, Herold S. 2013. Macrophage-expressed IFN-beta contributes to apoptotic alveolar epithelial cell injury in severe influenza virus pneumonia. PLoS Pathog 9:e1003188. doi: 10.1371/journal.ppat.1003188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Hoffmann E, Neumann G, Kawaoka Y, Hobom G, Webster RG. 2000. A DNA transfection system for generation of influenza A virus from eight plasmids. Proc Natl Acad Sci USA 97:6108–6113. doi: 10.1073/pnas.100133697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Tumpey TM, Basler CF, Aguilar PV, Zeng H, Solorzano A, Swayne DE, Cox NJ, Katz JM, Taubenberger JK, Palese P, García-Sastre A. 2005. Characterization of the reconstructed 1918 Spanish influenza pandemic virus. Science 310:77–80. doi: 10.1126/science.1119392. [DOI] [PubMed] [Google Scholar]
- 82.Matrosovich M, Matrosovich T, Garten W, Klenk HD. 2006. New low-viscosity overlay medium for viral plaque assays. Virol J 3:63. doi: 10.1186/1743-422X-3-63. [DOI] [PMC free article] [PubMed] [Google Scholar]