Abstract
Background
There are varieties of self-assessment questionnaire used for the evaluation of pain, functional disability, and health related quality of life in individuals with knee osteoarthritis (OA). The present study intended to adapt and translate the oxford knee score into the Arabic and investigated its psychometric properties in adult male with knee OA.
Methods
Ninety-seven adult male (mean age 57.55 ± 11.49 years) with knee OA participated. Patients were requested to complete the adapted Arabic version of the Oxford knee score (OKS-Ar), reduced “Western Ontario and McMaster Universities Index (WOMAC)”, and the Visual analogue scale (VAS). Patients were requested to complete 2nd form of OKS-Ar at least 1 week apart to assess the reproducibility of the score. The OKS was adapted and translated into Arabic by two independent Arabic native speakers (one rehabilitation professional having experience of knee OA patients and another one a trained translator) according to the international guidelines.
Results
All the participants completed the 2nd form of OKS-Ar (Response rate 100%). Reliability and internal consistency was high with an ICC of 0.97, and the Cronbach’s alpha coefficient of 0.987, respectively. A significant relationship between the OKS-Ar and the WOMAC and VAS scores confirmed the construct validity (p < 0.001). The standard error of measurement (SEM) and the minimum detectable change (MDC) were 2.2 and 6.2, respectively.
Conclusions
The adapted Arabic version of the OKS demonstrated acceptable psychometric properties, including reliability, internal consistency, and the validity. The present study indicates that the OKS-Ar is a suitable questionnaire to measure pain and physical function in the Arabic speaking adult male patients with knee OA.
Keywords: Arabic, Osteoarthritis, Knee, Oxford knee score, Validity, Reliability
Background
Knee osteoarthritis (OA) is the commonest degenerative joint disease affecting both men and women, and is represented by pain and impaired physical function that can significantly influence the health related quality of life [1–3]. Previous study reported that approximately 60.9% female and 53.3% male adults aged 30–93 years had shown radiographic evidence of knee OA in the Middle East [4]. Another study reported the prevalence of knee OA in the Saudi Arabia was around 30.8% in the adult aged 46–55 years and 60.6% in the adult aged 66–75 years [5]. The world-wide prevalence of the symptomatic knee OA with the radiographic evidence was about 3.8% in the year 2010 [6]. The prevalence of knee OA was higher in females than males (4.8% vs 2.8%) [6]. In the year 2010, the Asia Pacific high-income nations had highest prevalence of Knee OA, followed by Middle East North Africa (MENA) region [6]. In the year 2010, hip and knee OA was reported to be 11th highest contributor causing global disability world-wide [6].
Patients-rated self-assessment questionnaire are widely used to evaluate the outcomes of various interventions [7–10]. These questionnaires often assess pain, disability, and the quality of life. There are varieties of self-assessment questionnaire used for the evaluation of pain, disability, and quality of life in individuals with knee OA [11–16]. Out of these scales, the Oxford Knee Score (OKS) is a 12 item short self-reported scale designed to evaluate pain and function in individuals undergoing total knee arthroplasty (TKA) [12]. It was reported to be amongst the most sensitive, responsive, reliable, and valid patients-reported knee-specific questionnaire [17]. This questionnaire has been validated into various languages, including Italian [18], Chinese [19], Korean [20], Japanese [21], Swedish [22], Thai [23], Persian [24], Dutch [25], Portuguese [26], German [27], Turkish [28], and French [29].
The original English version and the subsequent adapted and translated versions of the OKS have been validated in individuals with knee OA who were either waiting for or undergoing knee replacement surgery [12, 18–20, 22, 23, 25–27, 29]. A few studies have validated the OKS in patient with knee OA [21, 24, 28, 30]. In addition, there was no validation of OKS in Arabic speaking population, therefore, in order to utilize this scale in Arab nation, a validation of the Arabic version OKS was required. The present study intended to adapt and translate the OKS for the Arabic speaking population and investigated its psychometric properties in adult male with knee OA.
Methods
Participants and criteria
Ninety-seven adult male diagnosed with knee OA as indicated by the criteria given by the “American College of Rheumatology (ACR)” participated in this study [31]. Severity of knee was measured using the “Kellgren and Lawrence scale” [32]. Due to the lack of access to the female patients, only male patients were recruited. Patients aged 40–80 years and who can read and understand Arabic language was participated. Patients were excluded if they had secondary OA, inflammatory joint disease, and trauma to knee joint. Patients with peripheral vascular diseases or cardiac diseases were also excluded. Rehabilitation Research Chair, King Saud University, Riyadh, Saudi Arabia, approved this study. Each patient provided an informed consent before the participation.
Translation and cross-cultural adaptation
The OKS was adapted and translated into Arabic according to the international guidelines [33–36], as per the license of the OKS copyright holder (©Isis Innovation Limited, 1998. All rights reserved. www.isis-innovation.com). The English OKS [12] was translated into Arabic language by two independent Arabic native speakers (one rehabilitation professional having experience of knee OA patients and another one a trained translator). The first draft of the preliminary version was developed after the discussion of the obtained translations in a first consensus panel. The Arabic adapted version was translated back to English by two independent translators, who were unaware with the original variant (Table 1). The second draft of the preliminary version was developed after the discussion of the forward and backward translations in a second consensus panel. This pre-final version was tested by knee OA (n = 10) to identify whether all the items of the questionnaire were easy to understand. They were requested to suggest the word or sentences to replace existing word or sentences, if they find any difficulty to understand any word or sentences. This stage confirmed that the questionnaire was easy to understand and no further changes in the questionnaire were required. Finally, a third consensus panel discussed and developed the final Arabic version of OKS-Ar.
Table 1.
Backward English translation of Arabic Version of the Oxford Knee Score (OKS-Ar)
| PROBLEMS IN YOUR KNEE (put a tick mark only one box of each question) | |
| 1. During the past four weeks …… How will you describe the pain your knee often have? □ None □ Very little □ Little □ Moderate □ Severe 2. During the past four weeks ….. Do you have any problems in washing or drying your entire body because of your knee pain? □ None at all □ Very little difficulty □ Moderate difficulty □ Severe difficulty □ Hard to do this 3. During the past four weeks …….. Do you have any problems in the entry and exit of your car or when using public transport because of your knee ?(Whichever is used) □ None at all □ Very little difficulty □ Moderate difficulty □ Severe difficulty □ Hard to do this 4. During the past four weeks … How long you can be able to walk before it becomes severe knee pain? (With or without a stick) □ No pain (For more than 30 min) □ No pain (for 16–30 min) □ No pain (for 5–15 min) □ No pain (Just around house only) □ There is no time at all without pain/severe pain when walking 5. During the past four weeks … After sitting on the table to eat, how much was the pain that you feel when getting up from the chair because of your knee? □ There is no pain at all □ Little Pain □ Moderate Pain □ Severe Pain □ Worst pain 6. During the past four weeks … Do you feel stumbling when walking because of your knee? □ Rarely/Never □ Sometimes, or just at the beginning □ Often, not only at the beginning □ Most of the time □ All times |
7. During the past four weeks … Are you able to kneel down and after that getup from the kneel down position? □ Yes, easily □ Little difficulty □ Moderate difficulty □ Severe difficulty □ No, it is impossible to do so 8. During the past four weeks … Do you suffer from pain in your knee in bed during the night? □ No nights □ A night or two nights only □ Some nights □ Most nights □ Every night 9. During the past four weeks … How much was the amount of the impact of knee pain on your usual work (including housework)? □ No impact □ Little impact □ Moderate impact □ Considerable impact □ Total impact 10. During the past four weeks … Have you ever felt that perhaps your knees are unstable or may make you fall? □ Rarely/Never □ Sometimes, or just at the beginning □ Often, not only at the beginning □ Most of the time □ All times 11. During the past four weeks… Is it possible for you to do shopping for yourself? □ Yes, easily □ Little difficulty □ Difficulty Medium □ With great difficulty □ No, it is impossible to do so 12. During the past four weeks … Is it possible for you to descend the one step of stairs? □ Yes, easily □ Little difficulty □ Moderate Difficulty □ Severe Difficulty □ No, it is impossible to do so |
| Finally, please check that you have answered all the questions. Thank you so much | |
Psychometric measurements
Patients were asked to complete all the outcome scores including, OKS-Ar, the reduced “Western Ontario and McMaster Universities Osteoarthritis index (WOMAC)” [16, 37], and the visual analogue scale (VAS) [38, 39] at first sessions. A second form of the OKS-Ar was completed at least 1 week apart to evaluate the reproducibility of the score. The construct validity of the OKS-Ar was investigated by testing the hypothesis that the scores of OKS-Ar should correlate with the WOMAC and VAS score.
Statistical analyses
Descriptive data were recorded as mean (standard deviation) and the range (minimum – maximum). Intraclass correlation coefficients (ICC2,1) was applied to determine the reliability. Wilcoxon sign ranked test was used to investigate any systematic differences between two test scores of OKS-Ar. Cronbach’s α coefficient was applied to determine the internal consistency. Absolute reliability was investigated by Bland-Altman plot method [37, 40]. The absolute measurement error was calculated using the standard error of measurement (SEM) and the minimal detectable change (MDC) (MDC =1.96 × √2 × SEM) [41, 42]. Spearman’s correlation coefficient between the OKS-Ar, WOMAC, and the VAS scores was used to assess the construct validity. In all the tests, the p < 0.05 was considered as level of significance. All the statistical analysis was done using the statistical package for the social sciences for Windows version 22 (IBM Inc., Chicago, Illinois, USA).
Results
All the participants were male [n = 97; mean age (standard deviation), 57.55 (11.49) years]. Table 2 presented the participants characteristics and baseline scores of OKS-Ar (test and retest), VAS, WOMAC pain score, WOMAC function score, and the WOMAC total score. All the participants completed the 2nd form of OKS-Ar (Response rate 100%). The results of the OKS-Ar total score indicate no floor (2.1%) or ceiling effect (1%).
Table 2.
Participants’ characteristics and the baseline scores
| N = 97 | |
|---|---|
| Age, years | |
| Mean (SD) | 57.55 (11.49) |
| Range | 40–80 |
| Height, m | |
| Mean (SD) | 1.69 (0.04) |
| Range | 1.58–1.80 |
| Weight, kg. | |
| Mean (SD) | 77.81 (10.91) |
| Range | 55–110 |
| BMI, kg/m2 | |
| Mean (SD) | 27.12 (3.70) |
| Range | 18.8–38.5 |
| OKS-Ar, 1st test | |
| Mean (SD) | 28.28 (12.80) |
| Range | 12–58 |
| OKS-Ar, Re-test | |
| Mean (SD) | 28.47 (13.06) |
| Range | 12–59 |
| VAS | |
| Mean (SD) | 4.61 (3.01) |
| Range | 0–10 |
| WOMAC, pain scale | |
| Mean (SD) | 7.41 (4.19) |
| Range | 0–17 |
| WOMAC, function scale | |
| Mean (SD) | 11.38 (6.62) |
| Range | 0–27 |
| WOMAC, total scale | |
| Mean (SD) | 18.79 (10.64) |
| Range | 0–41 |
SD Standard deviation, BMI Body mass index, OKS-Ar Arabic version of the oxford knee score, VAS Visual analogue scale, WOMAC Western Ontario and McMaster Universities Index
Internal consistency
Table 3 presented the results of internal consistency. The internal consistency of OKS-Ar was excellent with the Cronbach’s alpha (CA) values of 0.98 for total scores. Similarly, the corrected item-total correlations for all the items were high (range, 0.83–0.93]). The CA values did not improve higher than 0.98, if one item deleted.
Table 3.
Internal consistency of the Arabic version of the Oxford Knee Score (OKS-Ar)
| Items | Mean score ± SD | Corrected item-total correlation | Alpha if item deleted |
|---|---|---|---|
| 1 | 3.18 ± 1.16 | .83 | .98 |
| 2 | 2.13 ± 1.06 | .92 | .97 |
| 3 | 2.21 ± 1.04 | .93 | .97 |
| 4 | 2.06 ± 1.11 | .89 | .98 |
| 5 | 2.46 ± 1.08 | .88 | .98 |
| 6 | 2.54 ± 1.37 | .88 | .98 |
| 7 | 2.57 ± 1.18 | .90 | .97 |
| 8 | 2.31 ± 1.21 | .91 | .97 |
| 9 | 2.22 ± 1.12 | .90 | .97 |
| 10 | 2.24 ± 1.17 | .90 | .97 |
| 11 | 2.10 ± 1.22 | .86 | .98 |
| 12 | 2.25 ± 1.23 | .91 | .97 |
SD Standard deviation
Reliability
Table 4 presented the reliability of test-retest scores of OKS-Ar. Mean scores of test and retest assessment of OKS-Ar were 28.28 ± 12.8 and 28.47 ± 13.06, respectively. The ICCs for total score and each item were very high (range, .85–.97). In addition, there were no significant difference between test and retest scores of each item as well as total scores (p > 0.05). Figure 1 showed the Bland – Altman plot indicating most of the scores were within the limits of agreement. The Spearman’s correlation coefficient between the test and retest of OKS-Ar was high (r = 0.973, p < 0.001) (Fig. 2) (Table 5). The calculated SEM and MDC were 2.2 and 6.2, respectively.
Table 4.
Reliability of test-retest scores of the Arabic version Oxford knee score (OKS-Ar)
| Items | 1st Test (Mean ± SD) | Re-test (Mean ± SD) | ICC (95% CI) | a P-value |
|---|---|---|---|---|
| Total | 28.28 ± 12.80 | 28.47 ± 13.06 | .97 (.96–.98) | .84 |
| 1 | 3.18 ± 1.16 | 3.23 ± 1.168 | .85 (.79–.90) | .39 |
| 2 | 2.13 ± 1.06 | 2.14 ± 1.051 | .94 (.91–.95) | .78 |
| 3 | 2.21 ± 1.04 | 2.19 ± 1.024 | .90 (.85–.93) | .65 |
| 4 | 2.06 ± 1.11 | 2.12 ± 1.120 | .91 (.86–.93) | .20 |
| 5 | 2.46 ± 1.08 | 2.48 ± 1.174 | .86 (.81–.91) | .72 |
| 6 | 2.54 ± 1.37 | 2.51 ± 1.363 | .92 (.89–.94) | .56 |
| 7 | 2.57 ± 1.18 | 2.62 ± 1.220 | .91 (.87–.94) | .31 |
| 8 | 2.31 ± 1.21 | 2.31 ± 1.228 | .90 (.85–.93) | .98 |
| 9 | 2.22 ± 1.12 | 2.30 ± 1.165 | .88 (.83–.92) | .16 |
| 10 | 2.24 ± 1.17 | 2.30 ± 1.243 | .90 (.86–.93) | .24 |
| 11 | 2.10 ± 1.22 | 2.12 ± 1.210 | .88 (.82–.91) | .74 |
| 12 | 2.25 ± 1.23 | 2.23 ± 1.254 | .91 (.88–.94) | .68 |
SD Standard deviation
aWilcoxon sign ranked test
Fig. 1.
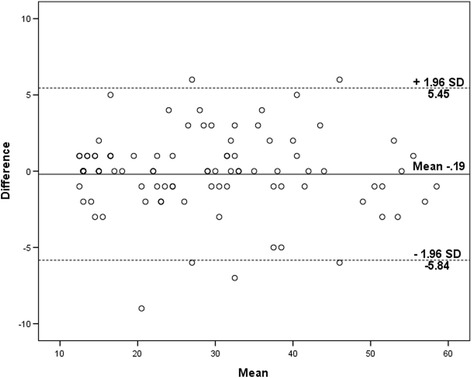
Bland-Altman plot showing reliability of the Oxford Knee Score (OKS-Ar)
Fig. 2.
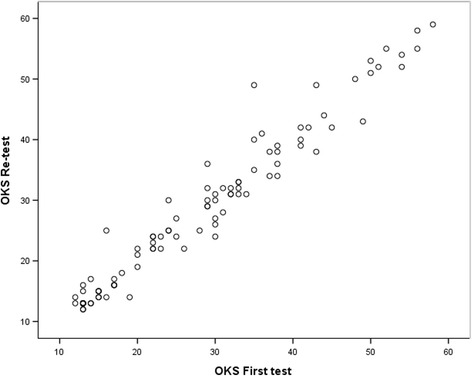
Scatter diagram showing the correlation between first test and re-test of OKS-Ar
Table 5.
Correlations between the Oxford knee score (OKS-Ar) and visual analogue scale (VAS) and the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC)
| Scales | OKS-Ar |
|---|---|
| OKS-Ar (re-test) | .973a |
| WOMAC, pain subscale | .885a |
| WOMAC, function subscale | .883a |
| WOMAC, total scale | .895a |
| VAS | .841a |
aCorrelations p ≤ 0.001
Validity
Table 5 presented the correlations between OKS-Ar and the WOMAC and VAS score. OKS-Ar was significantly associated with the VAS, WOMAC pain score, WOMAC function score, and the WOMAC total score (p < 0.001). The best degree of association was found between the OKS-Ar and the WOMAC total score (r = 0.895) (Fig. 3).
Fig. 3.
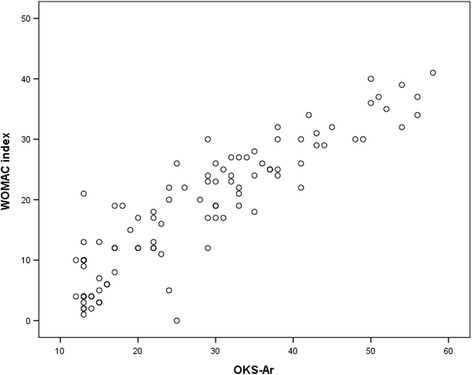
Scatter diagram showing the correlation between the OKS-Ar and the WOMAC index
Discussion
In the present study, the stage of translation and cross-cultural adaptation of the OKS to the Arabic language was described and the psychometric properties including internal consistency, reliability, and validity in adult male patients with knee OA were presented. In the present study, the Arabic version of the OKS demonstrated good psychometric properties including reliability, internal consistency, and validity in a sample of adult male with knee OA. As per literature review, this is the first study validating Arabic version of the OKS in Saudi Arabia.
The original English variant of OKS was designed to evaluate pain and physical function in individuals undergoing TKA [12]. Similarly, the questionnaire has been validated in a various languages and used in knee OA patients who were either waiting for or undergoing knee replacement surgery [18–20, 22, 23, 25–27, 29]. Till date, a few studies have validated the OKS in individuals with knee OA [21, 24, 28, 30]. In the present study, the reliability and the internal consistency of the Arabic version of the OKS were high (ICC 0.97 and CA 0.98). Similarly, previous studies reported high values of reliability (ICC 0.85 to 0.99) and internal consistency (CA 0.90 to 0.95) for different languages of the OKS in patients with knee OA [21, 24, 28]. In contrast, other studies reported a little lower internal consistency (CA 0.80 to 0.87) for different languages of the OKS as well as the original English version [12, 19, 23, 26, 27]. However, in the validation of the OKS, these studies involved knee OA patients who were either waiting for or undergoing knee replacement surgery. While, in the present study, only patients with knee OA with no any surgical intervention participated.
A good correlation between the OKS-Ar and the WOMAC and VAS scores confirmed the construct validity. Similarly, Turkish and Japanese version of the OKS demonstrated a good correlation between the OKS and the WOMAC index [21, 28]. In addition, original English version and the Korean version of the OKS demonstrated a moderate relationship between the OKS and the VAS score [12, 20]. Furthermore, Portuguese version of the OKS demonstrated a weak correlation between the OKS and the VAS score [26].
In addition, the SEM and MDC were calculated for the OKS-Ar in people with knee OA. As per literature review, neither original English version nor the subsequent adapted versions of the OKS have reported the SEM and MDC. Previous studies encouraged using SEM to determine the statistically meaningful change of a health outcome questionnaire [41, 42].
The present study acknowledged some potential limitations. The present study is limited to adult male patients with knee osteoarthritis. Due to the lack of access to the female patients, only male patients were recruited. Further validation with the female patients is recommended. In addition, sample size of the present study was fairly small. Furthermore, the present study did not assess the responsiveness of the Arabic version of the OKS. Further testing with the larger sample is required to complete the evaluation of this important psychometric property.
Conclusions
The adapted Arabic version of the OKS demonstrated acceptable psychometric properties, including reliability, internal consistency, and the validity. The present study indicates that the OKS-Ar is a suitable questionnaire to measure pain and function in the Arabic speaking adult male with knee osteoarthritis.
Acknowledgements
The authors are grateful to the Deanship of Scientific Research, King Saud University for funding through Vice Deanship of Scientific Research Chairs.
Funding
This project was funded by the Deanship of Scientific Research, King Saud University through Vice Deanship of Scientific Research Chairs. The funding body played no role on study design, the writing of the manuscript or the decision to submit the manuscript for publication.
Availability of data and materials
All data generated or analyzed during this study are presented in the manuscript. Please contact the corresponding author for access to data presented in this study.
Authors’ contributions
SA: Corresponding author, participated in the design of the study, participated in the data collection, drafted the manuscript and finished the manuscript. AA: participated in the design of the study, helped in ethics applications and revised the manuscript critically. EA: participated in the design of the study and revised the manuscript critically. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
Ethical approval has been obtained from the institutional review board (IRB), Rehabilitation Research Chair, King Saud University, Riyadh, Saudi Arabia. Each patient provided an informed consent before the participation.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Abbreviations
- MDC
Minimum detectable change
- OA
Osteoarthritis
- OKS
Oxford Knee Score
- SEM
Standard error of measurement
- VAS
Visual analogue scale
- WOMAC
Western Ontario and McMaster Universities Index.
Contributor Information
Ahmad H. Alghadir, Email: aalghadir@hotmail.com
Einas S. Al-Eisa, Email: ealeisa@ksu.edu.sa
Shahnawaz Anwer, Email: anwer_shahnawazphysio@rediffmail.com.
References
- 1.Cho HJ, Chang CB, Kim KW, Park JH, Yoo JH, Koh IJ, et al. Gender and prevalence of knee osteoarthritis types in elderly Koreans. J Arthroplasty. 2011;26(7):994–999. doi: 10.1016/j.arth.2011.01.007. [DOI] [PubMed] [Google Scholar]
- 2.Hochberg MC, Altman RD, Brandt KD, Clark BM, Dieppe PA, Griffin MR, et al. Guidelines for the medical management of osteoarthritis. Part I. Osteoarthritis of the hip. American College of Rheumatology. Arthritis Rheum. 1995;38(11):1535–1540. doi: 10.1002/art.1780381103. [DOI] [PubMed] [Google Scholar]
- 3.Hochberg MC, Altman RD, Brandt KD, Clark BM, Dieppe PA, Griffin MR, et al. Guidelines for the medical management of osteoarthritis. Part II. Osteoarthritis of the knee. American College of Rheumatology. Arthritis Rheum. 1995;38(11):1541–1546. doi: 10.1002/art.1780381104. [DOI] [PubMed] [Google Scholar]
- 4.Al-Arfaj A, Al-Boukai AA. Prevalence of radiographic knee osteoarthritis in Saudi Arabia. Clin Rheumatol. 2002;21(2):142–145. doi: 10.1007/s10067-002-8273-8. [DOI] [PubMed] [Google Scholar]
- 5.Al-Arfaj AS, Alballa SR, Al-Saleh SS, Al-Dalaan AM, Bahabry SA, Mousa MA, et al. Knee osteoarthritis in Al-Qaseem, Saudi Arabia. Saudi Med J. 2003;24(3):291–293. [PubMed] [Google Scholar]
- 6.Cross M, Smith E, Hoy D, Nolte S, Ackerman I, Fransen M, et al. The global burden of hip and knee osteoarthritis: estimates from the global burden of disease 2010 study. Ann Rheum Dis. 2014;73(7):1323–1330. doi: 10.1136/annrheumdis-2013-204763. [DOI] [PubMed] [Google Scholar]
- 7.Beaton DE, Schemitsch E. Measures of health-related quality of life and physical function. Clin Orthop Relat Res. 2003;413:90–105. doi: 10.1097/01.blo.0000079772.06654.c8. [DOI] [PubMed] [Google Scholar]
- 8.Fitzpatrick R, Davey C, Buxton MJ, Jones DR. Evaluating patient-based outcome measures for use in clinical trials. Health Technol Assess. 1998;2(14):i–iv. [PubMed] [Google Scholar]
- 9.Whitehouse SL, Blom AW, Taylor AH, Pattison GT, Bannister GC. The Oxford Knee Score; problems and pitfalls. Knee. 2005;12(4):287–291. doi: 10.1016/j.knee.2004.11.005. [DOI] [PubMed] [Google Scholar]
- 10.Marx RG. Knee rating scales. Arthroscopy. 2003;19(10):1103–1108. doi: 10.1016/j.arthro.2003.10.029. [DOI] [PubMed] [Google Scholar]
- 11.Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15(12):1833–1840. [PubMed] [Google Scholar]
- 12.Dawson J, Fitzpatrick R, Murray D, Carr A. Questionnaire on the perceptions of patients about total knee replacement. J Bone Joint Surg (Br) 1998;80(1):63–69. doi: 10.1302/0301-620X.80B1.7859. [DOI] [PubMed] [Google Scholar]
- 13.Lysholm J, Tegner Y. Knee injury rating scales. Acta Orthop. 2007;78(4):445–453. doi: 10.1080/17453670710014068. [DOI] [PubMed] [Google Scholar]
- 14.Mahler E, Cuperus N, Bijlsma J, Vliet Vlieland T, van den Hoogen F, den Broeder AA, et al. Responsiveness of four patient-reported outcome measures to assess physical function in patients with knee osteoarthritis. Scand J Rheumatol. 2016;45(6):518–527. doi: 10.3109/03009742.2016.1140226. [DOI] [PubMed] [Google Scholar]
- 15.Roos EM, Roos HP, Lohmander LS, Ekdahl C, Beynnon BD. Knee Injury and Osteoarthritis Outcome Score (KOOS) – development of a self-administered outcome measure. J Orthop Sports Phys Ther. 1998;28(2):88–96. doi: 10.2519/jospt.1998.28.2.88. [DOI] [PubMed] [Google Scholar]
- 16.Whitehouse SL, Lingard EA, Katz JN, Learmonth ID. Development and testing of a reduced WOMAC function scale. J Bone Joint Surg (Br) 2003;85(5):706–711. [PubMed] [Google Scholar]
- 17.Garratt AM, Brealey S, Gillespie WJ, Team DT. Patient-assessed health instruments for the knee: a structured review. Rheumatology (Oxford) 2004;43(11):1414–1423. doi: 10.1093/rheumatology/keh362. [DOI] [PubMed] [Google Scholar]
- 18.Padua R, Zanoli G, Ceccarelli E, Romanini E, Bondi R, Campi A. The Italian version of the Oxford 12-item Knee Questionnaire-cross-cultural adaptation and validation. Int Orthop. 2003;27(4):214–216. doi: 10.1007/s00264-003-0453-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Xie F, Li SC, Lo NN, Yeo SJ, Yang KY, Yeo W, et al. Cross-cultural adaptation and validation of Singapore English and Chinese Versions of the Oxford Knee Score (OKS) in knee osteoarthritis patients undergoing total knee replacement. Osteoarthritis Cartilage. 2007;15(9):1019–1024. doi: 10.1016/j.joca.2007.02.013. [DOI] [PubMed] [Google Scholar]
- 20.Eun IS, Kim OG, Kim CK, Lee HS, Lee JS. Validation of the Korean version of the Oxford Knee Score in patients undergoing total knee arthroplasty. Clin Orthop Relat Res. 2013;471(2):600–605. doi: 10.1007/s11999-012-2564-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Takeuchi R, Sawaguchi T, Nakamura N, Ishikawa H, Saito T, Goldhahn S. Cross-cultural adaptation and validation of the Oxford 12-item knee score in Japanese. Arch Orthop Trauma Surg. 2011;131(2):247–254. doi: 10.1007/s00402-010-1185-1. [DOI] [PubMed] [Google Scholar]
- 22.Dunbar MJ, Robertsson O, Ryd L, Lidgren L. Translation and validation of the Oxford-12 item knee score for use in Sweden. Acta Orthop Scand. 2000;71(3):268–274. doi: 10.1080/000164700317411861. [DOI] [PubMed] [Google Scholar]
- 23.Charoencholvanich K, Pongcharoen B. Oxford knee score and SF-36: translation & reliability for use with total knee arthroscopy patients in Thailand. J Med Assoc Thai. 2005;88(9):1194–1202. [PubMed] [Google Scholar]
- 24.Ebrahimzadeh MH, Makhmalbaf H, Birjandinejad A, Soltani-Moghaddas SH. Cross-cultural adaptation and validation of the persian version of the oxford knee score in patients with knee osteoarthritis. Iran J Med Sci. 2014;39(6):529–535. [PMC free article] [PubMed] [Google Scholar]
- 25.Haverkamp D, Breugem SJ, Sierevelt IN, Blankevoort L, van Dijk CN. Translation and validation of the Dutch version of the Oxford 12-item knee questionnaire for knee arthroplasty. Acta Orthop. 2005;76(3):347–352. [PubMed] [Google Scholar]
- 26.Goncalves RS, Tomas AM, Martins DI. Cross-cultural adaptation and validation of the Portuguese version of the Oxford Knee Score (OKS) Knee. 2012;19(4):344–347. doi: 10.1016/j.knee.2011.04.006. [DOI] [PubMed] [Google Scholar]
- 27.Naal FD, Impellizzeri FM, Sieverding M, Loibl M, von Knoch F, Mannion AF, et al. The 12-item Oxford Knee Score: cross-cultural adaptation into German and assessment of its psychometric properties in patients with osteoarthritis of the knee. Osteoarthritis Cartilage. 2009;17(1):49–52. doi: 10.1016/j.joca.2008.05.017. [DOI] [PubMed] [Google Scholar]
- 28.Tugay BU, Tugay N, Guney H, Kinikli GI, Yuksel I, Atilla B. Oxford Knee Score: cross-cultural adaptation and validation of the Turkish version in patients with osteoarthritis of the knee. Acta Orthop Traumatol Turc. 2016;50(2):198–206. doi: 10.3944/AOTT.2015.15.0127. [DOI] [PubMed] [Google Scholar]
- 29.Jenny JY, Diesinger Y. Validation of a French version of the Oxford knee questionnaire. Orthop Traumatol Surg Res. 2011;97(3):267–271. doi: 10.1016/j.otsr.2010.07.009. [DOI] [PubMed] [Google Scholar]
- 30.Xie F, Ye H, Zhang Y, Liu X, Lei T, Li SC. Extension from inpatients to outpatients: validity and reliability of the Oxford Knee Score in measuring health outcomes in patients with knee osteoarthritis. Int J Rheum Dis. 2011;14(2):206–210. doi: 10.1111/j.1756-185X.2010.01580.x. [DOI] [PubMed] [Google Scholar]
- 31.Altman R, Asch E, Bloch D, Bole G, Borenstein D, Brandt K, et al. Development of criteria for the classification and reporting of osteoarthritis. Classification of osteoarthritis of the knee. Diagnostic and Therapeutic Criteria Committee of the American Rheumatism Association. Arthritis Rheum. 1986;29(8):1039–1049. doi: 10.1002/art.1780290816. [DOI] [PubMed] [Google Scholar]
- 32.Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16(4):494–502. doi: 10.1136/ard.16.4.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wild D, Grove A, Martin M, Eremenco S, McElroy S, Verjee-Lorenz A, et al. Principles of Good Practice for the Translation and Cultural Adaptation Process for Patient-Reported Outcomes (PRO) Measures: report of the ISPOR Task Force for Translation and Cultural Adaptation. Value Health. 2005;8(2):94–104. doi: 10.1111/j.1524-4733.2005.04054.x. [DOI] [PubMed] [Google Scholar]
- 34.Acquadro C, Conway K, Hareendran A, Aaronson N, Quality ERI. Literature review of methods to translate health-related quality of life questionnaires for use in multinational clinical trials. Value Health. 2008;11(3):509–521. doi: 10.1111/j.1524-4733.2007.00292.x. [DOI] [PubMed] [Google Scholar]
- 35.Beaton DE, Bombardier C, Guillemin F, Ferraz MB. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine. 2000;25(24):3186–3191. doi: 10.1097/00007632-200012150-00014. [DOI] [PubMed] [Google Scholar]
- 36.Guillemin F, Bombardier C, Beaton D. Cross-Cultural Adaptation of Health-Related Quality-of-Life Measures - Literature-Review and Proposed Guidelines. J Clin Epidemiol. 1993;46(12):1417–1432. doi: 10.1016/0895-4356(93)90142-N. [DOI] [PubMed] [Google Scholar]
- 37.Alghadir A, Anwer S, Iqbal ZA, Alsanawi HA. Cross-cultural adaptation, reliability and validity of the Arabic version of the reduced Western Ontario and McMaster Universities Osteoarthritis index in patients with knee osteoarthritis. Disabil Rehabil. 2016;38(7):689–694. doi: 10.3109/09638288.2015.1055380. [DOI] [PubMed] [Google Scholar]
- 38.Hjermstad MJ, Fayers PM, Haugen DF, Caraceni A, Hanks GW, Loge JH, et al. Studies comparing Numerical Rating Scales, Verbal Rating Scales, and Visual Analogue Scales for assessment of pain intensity in adults: a systematic literature review. J Pain Symptom Manage. 2011;41(6):1073–1093. doi: 10.1016/j.jpainsymman.2010.08.016. [DOI] [PubMed] [Google Scholar]
- 39.Gallasch CH, Alexandre NM. The measurement of musculoskeletal pain intensity: a comparison of four methods. Rev Gaucha Enferm. 2007;28(2):260–265. [PubMed] [Google Scholar]
- 40.Alsanawi HA, Alghadir A, Anwer S, Roach KE, Alawaji A. Cross-cultural adaptation and psychometric properties of an Arabic version of the Shoulder Pain and Disability Index. Int J Rehabil Res. 2015;38(3):270–275. doi: 10.1097/MRR.0000000000000118. [DOI] [PubMed] [Google Scholar]
- 41.Lydick E, Epstein RS. Interpretation of quality of life changes. Qual Life Res. 1993;2(3):221–226. doi: 10.1007/BF00435226. [DOI] [PubMed] [Google Scholar]
- 42.Wyrwich KW, Wolinsky FD. Identifying meaningful intra-individual change standards for health-related quality of life measures. J Eval Clin Pract. 2000;6(1):39–49. doi: 10.1046/j.1365-2753.2000.00238.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed during this study are presented in the manuscript. Please contact the corresponding author for access to data presented in this study.


