Abstract
Background
Telephone consultation and triage are used to limit the workload on emergency departments. Lack of visual cues and clinical tests put telephone consultations to a disadvantage compared to face-to-face consultations increasing the risk of under-triage. Under-triage occurs in telephone triage; however why under-triage happens is not explored yet. The aim of the study was to describe situations of under-triage in context, to assess the quality of under-triaged calls, and to identify communication patterns contributing to under-triage in a regional OOH service in the capital region of Denmark.
Methods
Explanatory simultaneous mixed method with thematic analysis and descriptive statistics was chosen. The study was carried out in an Out-Of-Hours service (OOH) in the Capital Region of Denmark, Copenhagen. Under-triage was defined as Potentially Under-Triaged Calls (PUTC) by specific criteria to an OOH Hotline, and identification by integration of three databases: Medical Hotline database, Emergency number database, including the Ambulance database, and electronic patient records. Distribution of PUTC were carried out using ICD-10 codes to identify diagnosis and main themes identified by qualitative analysis of audio recorded under-triaged calls. Study period was October 15th to November 30th 2014.
Results
Three hundred twenty seven PUTC were identified, representing 0.04% of all calls (n = 937.056) to the OOH. Distribution of PUTC according to diagnoses was: digestive (24%), circulatory (19%), respiratory (15%) and all others (42%). Thematic analysis of the voice logs suggested that inadequate communication and non-normative symptom description contributed to under-triage.
Discussion
The incidence of potentially under-triage is low (0.04%). However, the over-representation of digestive, circulatory, and respiratory diagnoses might suggest that under-triage is related to inadequate symptom description. We recommend that caller and call-handler collaborate systematically on problem identification and negotiate non-normative symptom description.
Conclusion
The incidence of under-triage is low (0.04%). However, the over-representation of digestive, circulatory, and respiratory diagnoses might suggest that under-triage is related to inadequate symptom description. We recommend that caller and call-handler collaborate systematically on problem identification and negotiate non-normative symptom description.
Keywords: Telephone consultation, ICD codes, Out-of-hours medical care, Prehospital acute medicine, Telephone hotline, Triage (under-triage)
Background
Telephone consultation are often chosen over face-to-face consultations in Out Of Hours (OOH) services to ensure cost effectiveness [1], however telephone consultations are associated with uncertainty due to the lack of visual cues [2, 3]. The accuracy of telephone triage has been shown to vary from 49 to 98% [4], suggesting that the issue might affect patient safety. The decision-making process in telephone consultations is influenced by call-handler’s dual task of offering advice (helping the caller) while also acting as gatekeeper [5]. Thus, more knowledge about the pattern of communication that might precipitate under-triage could be used to improve the call-handler/caller interaction. This study aims to describe situations of under-triage in context, to assess the quality of under-triaged calls, and to identify communication patterns contributing to under-triage in a regional OOH service in the capital of Denmark.
Methods
The study had an explanatory simultaneous mixed methods design involving two retrospective datasets [6]. Data consisted of a quantitative strand and a qualitative strand. The qualitative strand was weighted more than the quantitative strand (Fig. 1).
Fig. 1.
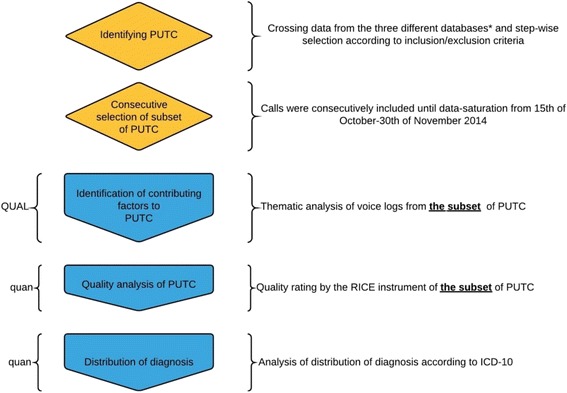
Overview of methods, priority and timing of the quantitative and qualitative strand. Identification of Potentially Under-Triaged Calls were conducted by crossing data from medical hotline 1813, emergency hotline 112, and the electronic patient record “Opus”. PUTC = Potentially Under-Triaged Calls
Setting
The study used data from the OOH service in the Capital Region of Denmark, Copenhagen (hereafter Copenhagen). In this region the OOH is integrated in the Emergency Medical Services and covers a population of 1.7 million citizens (callers) who can contact the OOH Medical Hotline and will be triaged to receive a home visit, scheduled for a consultation at an emergency department or acute care clinic, hospitalised or given advice on self-care, or advised to see their usual GP. The call-handler responding to the call is either a nurse or a physician. Triage and determination of urgency is guided by an electronic decision tool based on the symptoms described by the caller. The triage tool is a detailed guideline to support decision making. The guideline is for nurses a strict protocol where deviations have to be approved by a physician. For physicians the triage tool is a guideline that can be deviated from, however this should be documented. The decision tool is divided into three main sections: somatic illness, somatic injury and psychiatric illness. Emergency calls for potential life-threatening symptoms or injury and request for an ambulance are handled through a different telephone number, 112.
The quantitative study
| Data in the quantitative strand were used to identify Potentially Under-Triaged Calls (PUTCs) and to describe the distribution of diagnoses using the ICD-10 codes. For a call to be identified as a PUTC it had to meet three criteria: BOX: PUTC criteria
1) Caller used the Medical Hotline number, and was NOT offered a home visit and was NOT offered an appointment at an Emergency Department, or hospitalised, AND 2) Caller used the Emergency number 112 for an ambulance within two hours of the first contact, AND 3) Caller was admitted to hospital later by ambulance. |
Data were retrieved from administrative databases “Medical Hotline 1813” (the OOH call system), Emergency Number 112 (the ambulance database), and the electronic patient record used in the regions hospitals (using the ICD-10 code for admission). Inclusion: calls identified as PUTC. Exclusion: calls concerning psychiatric complaints, calls unrelated to the initial somatic complaints (e.g. calls regarding logistics), calls concerning febrile seizures in children.
Data were described calculating percentage of ICD-10 codes and grouping these into sense making clusters.
The qualitative study
The specific aim of the qualitative strand was to identify contributing factors to PUTC, using thematic analysis of audio recorded voice logs.
Data generation
The qualitative sample was a subset of calls (voice logs) to the Medical Hotline 1813 selected by consecutive criterion sampling from October 15th to November 30th, 2014 until data saturation by information redundancy. The criterion sample consisted of calls identified as PUTC in the quantitative strand.
Data analysis
The voice logs were retrieved from an internal database and transcribed verbatim. Initial deductive coding was performed using the four components of the RICE scale [7, 8] to structure the data corpus. The Rice scale is a Dutch assessment tool of call-handlers’ communication skills. The items in the rating scale are structured in accordance with the sequence in telephone triage calls: Reason for calling, Information gathering, Conclusion and Evaluation (RICE) which are sub-divided into 17 items. Inductive thematic analysis was carried out according to the active participant (call-handler vs. caller). The initial codes were clustered into themes, data were systematically reviewed to ensure that name, definition and exhaustive set of data supported the theme. It was verified that the results were representative of the collected calls by re-reading the transcripts and re-assessing the themes. The results were researcher triangulated and discrepancy solved by discussion and consensus [9].
To rule out that under-triage was the result of poor quality communication a quality assessment was made with the RICE instrument, poor quality (RICE < 80%) and good quality (RICE >80%). This criterion was provided by the author of the RICE criteria (personal correspondence).
Results
Quantitative results
The Medical Hotline 1813 received 937 056 calls in 2014 of which approximately 40% were triaged to self-care or GP. Applying the PUTC criterion meant that a total of n = 939 calls were eligible for the study, Fig. 2.
Fig. 2.
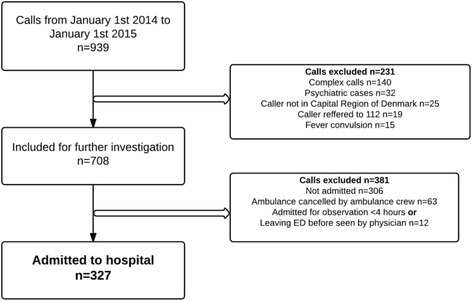
Flowchart of cases included
From the 939 eligible calls, 612 were excluded according to exclusion criteria, leaving 327 for analysis in the study. As such, approx. 35% of the study population were PUTC and included in the description of distribution of diagnosis according to ICD-10, Fig. 3.
Fig. 3.
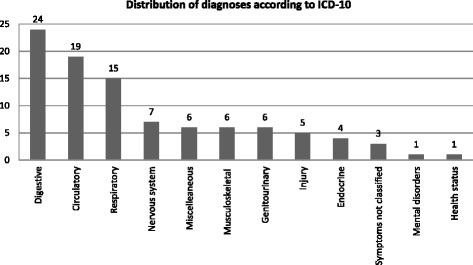
Distribution of PUTC according to diagnosis at admission in ICD-10 codes. *Miscellaneous includes diseases related to pregnancy, childbirth, certain infections, and diseases of eye and skin
Qualitative results
We analysed 31 calls regarding 19 patients from the sample of 327 calls to the Medical Hotline 1813. According to the RICE score, 21 of the 31 calls were of acceptable quality, Table 1.
Table 1.
Demographics of potentially under-triaged calls (PUTC)
| Caller | Patient, Sex/age | OOH hotline problem | Admission diagnosis | RICE rating | Other | |
|---|---|---|---|---|---|---|
| 1 | Patient | Male, 64 | Smoke inhalation | Observation of smoke inhalation | 71% | Admission for social reasons |
| 2 | Patient | Female, 79 | Abdominal pain | Observation of AMI | 86% | n/a |
| 3 | Daughter | Female, 68 | Nose bleed | Defect of septum | 80% (a)a
77% (b) |
n/a |
| 4 | Friend | Female, 40 | Dizziness | Vertigo | 56% | Language difficulties |
| 5 | Mother | male < 1 | Diarrhea and vomiting | Syncope | 89% (a) 82% (b) |
n/a |
| 6 | Mother | Female, 4 | Laryngitis | Epiglottis | 90% (a) 79% (b) 87% (c) |
n/a |
| 7 | Husband | Female, 75 years | Abdominal pain | Missed STEMI | 77% (a) 75% (b) 95% (c) |
n/a |
| 8 | Mother | Female, 8 | Diarrhea and vomiting | Dehydration | 88% | n/a |
| 9 | Patient | Female, 53 | Allergic reaction | Perioral edema | 84% | n/a |
| 10 | Patient | Male, 45 | Abdominal pain | Gallstone | 94% (a) 84% (b) |
n/a |
| 11 | Patient | Female, 81 | Abdominal pain | Gallstone | 89% | n/a |
| 12 | Patient | Female, 17 | Abdominal pain | Abdominal pain | 98% (a) 60% (b) |
n/a |
| 13 | Patient | Female, 45 | Headache/ dizziness |
Chronic post-traumatic headache after SAH | 96% (a) 82% (b) |
Frequent caller |
| 14 | Patient | Male, 64 | Edema of lower extremity | Obs. DVT | 75% | n/a |
| 15 | Spouse | Male, 28 | Fainting | Observation for neurological problem | 88% (a) 92% (b) |
n/a |
| 16 | Spouse | Male, 25 | Hyperglycemia and intoxication | Hyperglycemia | 94% | n/a |
| 17 | Friend | Male, 56 | Fever and abdominal pain | Chronic liver cirrhosis | 83% (a) 58% (b) |
n/a |
| 18 | Patient | Female, 28 | Bleeding after vaginal delivery 5 days earlier | Small post-partum bleeding | 89% (a) 95% (b) |
n/a |
| 19 | Daughter | Male, 52 | Fever and malaise | Sepsis | 29% | n/a |
aThe letter a indicating the first call, b a second call, and c a third call
Inductive coding of the data led to 18 codes related to the call-handler response and 16 codes related to the caller response. The main theme was identified as ‘Co-constructing the problem’ (Table 2).
Table 2.
Codes and themes derived from complete coding
| Participant | Codes | Themes | CO-CONSTRUCTING THE PROBLEM |
| Call-handler response | Clarifying history of problem Acknowledging caller experience Individualized communication Providing advice in blocks Empowering caller Educating caller Agreement of plan |
The professional communication | |
| Condescending, irritated, patronizing communication Ignoring patient perspective, minimizing magnitude of problem |
The non-professional role | ||
| Lack of control with conversation Providing unclear advice Disagreeing with caller Non-individualized communication Unable to collaborate with caller |
The non-professional Communication | ||
| Gate keeper Fixation error Uncharacteristic problem Lack of agreement on problem, urgency and plan |
The difficult decision making | ||
| Caller response | Clear description of problem Clear description of temporal progression of problem Self-evaluation of problem Agreement of plan |
The constructive caller | |
| Vague and/or lengthy description of actual problem Cerebrally impaired Time line Insecurity Talking down symptoms |
The complicated caller | ||
| Lacking problem solving/self-care before calling Contradictive information (+vocal appearance) |
The un-constructive caller | ||
| Caller under the influence Caller is very emotional |
The caller is inebriated/intoxicated | ||
| Calling during GP office hours Unrealistic expectations |
The caller has unrealistic expectations of outcome | ||
| Caller is not patient, caller is not with patient | Proximity to patient (physical/relative) |
Call-handler response
Professional communication
Most importantly the professional communication would enhance collaboration and target individual needs, as well as empowering and educating the caller. As seen in a consultation with the mother of a child with laryngitis: “If it gets any worse or if you think you can’t handle it yourself, call for an ambulance”. The caller was invited to take part in the decision and treatment plan.
Non-professional role
The non-professional role was manifest in blocking and discouraging communication presented by the call-handler as expressions of: Irritation, condescending, or patronizing and characterized by a disagreement of magnitude of the problems and distrust in the described problem. Moreover, the decision making process was impaired by a non-objective approach to the caller. An example of this was the call-handler dismissing the caller or the symptom blocking further information collection. “…and if you call again in 10 min saying that it (the temperature) is 40° Celsius then I won’t believe you”.
Non-professional communication
Factors that contributed to non-professional communication were: Lack of control of conversation in the situations where the caller was under the influence of substances/drugs, fast talking, or continuing to repeat questions and answering themselves, or the very emotional caller. A contributing factor regarding the call-handler was providing unclear advice. The advice could be overly complex making it difficult for the caller to focus on one or two clear pieces of advice. Non-individualized communication was present in a conversation on self-care advice. (Call-handler) “Do you have any baking soda in the cupboard?” (Caller):” no, what is that?” (call-handler): “The chemical formula is bicarbonate of soda”. Nothing was achieved by this explanation and the caller was left without advice.
Complex decision making
Assessment of urgency and plan were potentially complicated by several factors. Problems unrelated to the illness (e.g. uncertainty of address) or non-normative symptoms (non- textbook symptoms) led to complex decision making. Even during professional communication the call-handler might overestimate the self-care ability of the patient or might assume that the problem would be self-limiting. As an example, an elderly woman called with severe abdominal pain, which she compared to her experience with kidney stones. Her breathing was audibly affected. The call-handler’s response to the patient was: “Try taking two paracetamol and go to bed and rest a little and see if it doesn’t resolve … it is probably just a stomach infection”. Later the same patient called for an ambulance and was triaged as chest pain. Complex decision making can be caused by horizontal reasoning, causing the call-handler to fixate on a wrong diagnosis - in this case a stomach infection the call-handler is convinced that the problem is self-limiting and does not evaluate the symptoms and complaints laterally. The last theme; lack on agreement on problem, urgency and plan was seen when the caller and call-handler failed to collaborate and the call was terminated without a clear agreement.
Caller response
The constructive caller
The constructive caller would provide the call-handler with a clear description of the problem and with clear normative symptoms. However, a timeline to the description of the problem could both be an advantage or a barrier to correct triage, e.g. if the caller judged the problem to be self-limiting. This paradox was represented in the example of a young man who called in with uncontrollable jerking: “I have had it like I’m getting a sinus condition but it’s just getting worse and worse. However, in situations when callers minimized the symptoms, the call became complicated and the decision making process compromised. An example was a middle-aged man who called in with severe abdominal pain: “I don’t know, maybe I’m just constipated or I have eaten too much”. The patient was subsequently admitted with a gall stone.
The complex caller
The urgency-estimation could be complicated by a lengthy and unclear description of symptoms. An example was a woman who called complaining of a severe headache. The caller had suffered a non-traumatic brain injury and had acquired a chronic headache. Obtaining the medical history was complicated by the caller’s impaired speech as a result of the injury. Initially the caller declined the offer to be seen at the hospital. Half an hour later she called the emergency Medical Hotline for an ambulance. Some callers appeared insecure when they called, e.g.: “I don’t know if it is a problem that can wait, I just wanted some advice”. The complicated caller failed to communicate a clear problem to the call-handler, and the caller might even disagree on the plan without saying so.
The un-constructive caller
Callers that had not tried to solve their problem on their own received advice from the call-handler (e.g. pain killers, measure temperature) and were asked to call again if the problem did not resolve. In some cases the un-constructive caller could trigger a non-professional response from the call-handler. E.g. a daughter called on behalf of her father who had severe pain passing urine. (Call-handler): “did you call his doctor?” (Caller):” No, he’s closed for the day”. (Call-handler): “Then they will refer you to another number on the answering machine”; “In any case we are not coming home to your father” (Caller):” But it seems acute, and I’m working within health care so I know that he’s ill”. (Call-handler): “in that case you should know what a normal temperature is (referring to earlier in the conversation where the caller asked what a normal temperature was).
The caller is not in control
If the caller did not have emotional self-control or was cognitively impaired due to intoxication, collaboration with the call-handler was made difficult. A woman called on behalf of a friend who had a problem with cirrhosis and vomiting is an example of the caller under the influence of unknown substances. The caller was unable to present a problem, was contradicting herself, and gave a very lengthy and unstructured description of the reason for calling. The call was terminated by the call-handler stating: “this is not a problem for the Hotline!” Shortly thereafter the woman called for an emergency ambulance and the patient was admitted until the following day on social reasons.
The unrealistic caller
Some callers had an unrealistic expectation to the outcome of the telephone consultation. One young woman called the Hotline with complaints of gastroenteritis. She was very emotional and not able to collaborate with the call-handler. She wanted an ambulance to come and give her some medicine and ended the call when this was refused. Because of her emotional state when she called for an emergency ambulance she was brought to the hospital and admitted until the following day. Another example of unrealistic expectations was calling during GP opening hours. It was seen that this could trigger a negative and non-professional response from the call-handler.
The caller’s proximity to patient
Caller proximity to the patient was also seen to contribute to a difficult telephone consultation. This could be due to physical distance, or if the call was made by a proxy who was not closely related to the patient e.g. “my dad is having pain when urinating, he is cursing and feeling really bad”, call-handler; “can I talk to him?” Caller; “No, I’m not with him right now; I talked to my mother, who asked me to phone”. Physical distance where the caller and patient were not at the same location offered a specific barrier to symptom description, and was often resolved with the request to call back when in the presence of the patient.
Discussion
Thematic analysis of the voice logs suggested that non-normative symptom and poor communication description contributed to under-triage. The study demonstrated a generally low incidence of potentially under-triage calls of 0.04%. The most frequent categories of admission diagnoses were related to digestive, circulatory and respiratory symptoms. The use combining quantitative and qualitative methodology in this study helps to illustrate different perspectives of the complex issue of potentially under-triage in low urgency calls in a Danish setting.
Strengths and limitations
The study was conducted during the first year after the re-organization of the OOH service in the Capital Region of Denmark, and thereby included new staff and guidelines. This could have affected the results. The definition of PUTC applied strict criteria to the inclusion of calls. This definition might have been too strict to estimate the actual under-triage, but it did illustrate calls with manifest issues of mis-communication. Moreover, the definition did not take into account the cases that did not make a second call for an emergency ambulance within the time limit, or were admitted by their GP, or even died. Furthermore, the potentially under-triaged calls did not take into consideration that some outcomes could be due to a natural deterioration of the patient. The quality analysis of the calls was performed using the RICE instrument only validated in the Nederland. Application of the instrument enabled a quality assessment of the calls showing that poor communication was not the sole contributing factor to under-triage.
Comparison with existing literature
When dealing with low urgency alternative decision making strategies might be used [2], and internal factors related to the call-handler/caller might confound the triage outcome. The large proportion of abdominal problems in the PUTC, underlines the issue with non-normative symptom description. Abdominal pain is considered to be difficult to evaluate even with lab tests and even when the clinical symptoms are moderately manifest [10], because of many possible differential diagnoses. It is recommended to use clinical decision tools for diagnosis to minimize false positive operative procedures [11]. The medical diagnosis is considered monologic and not dialogic [12], but in absence of the lab tests and clinical observations the co-construction of the problem demands dialog [13], which makes the need for good quality communication even greater. In the present study it was made clear that certain caller characteristics could trigger the call- handler to an un-constructive response. This was seen in the calls where the caller was intoxicated or had unrealistic expectations to the outcome of the call. The stereotype of the intoxicated caller, the caller with limited language proficiency or the un-constructive caller can confound the decision-making process, because the voice utterance is a personal signature [12]. One of the factors that could explain potentially under-triage could be fixation error. Fixation error as term is widely used in emergency medicine for situations where the health professional solely concentrates upon one single aspect of a case to the detriment of other more relevant aspects [14]. There is no simple solution for fixation errors but the introduction of lateral thinking and closed loop communication could alleviate some of the problems and reduce inappropriate gate-keeping [15, 16].
Implications for research and/or practice
The construction of a scale for the callers’ subjective perception of the situation, like the pain scale, could prove valuable in telephone triage. Such a scale could incorporate the callers’ perspective and thereby gaining more information than a non-normative symptom description and bypassing some of the internal factors related to the call-handler.
Conclusion
The incidence of potentially under-triage is low (0.04%). However, the over-representation of digestive, circulatory, and respiratory diagnoses might suggest that under-triage is related to inadequate symptom description. We recommend that caller and call-handler collaborate systematically on problem identification and negotiate non-normative symptom description.
Acknowledgements
Not applicable
Permission was sought and granted from the Danish Data Protection Agency (ref. 2012-58-0004) and the National Board of Health (ref. 3-3013-1175/1)
Funding
The study was not financially funded by a third party. The EMS Copenhagen receives research center support from the Laerdal Foundation for Acute Medicine.
Availability of data and materials
Available upon request/not applicable
Authors’ contributions
HGJ, FL and IR participated in the design of the study. HGJ carried out the datacollection, dataanalysis and drafted the manuscript. IR and FL participated in the data analysis and contributed to the drafting of the manuscript. All authors read and approved the final manuscript.
Competing interests
The authors state no conflict of interest. The study was not financially funded by a third party.
Consent for publication
Not applicable
Ethics approval and consent to participate
Not applicable
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Abbreviations
- GP
General practioner
- OOH
Out-of-hours services
- PUTC
Potentially under-triaged calls
Contributor Information
Hejdi Gamst-Jensen, Email: Hejdi.gamst-jensen.01@regionh.dk.
Freddy K. Lippert, Email: Lippert@regionh.dk
Ingrid Egerod, Email: Ingrid.Egerod@regionh.dk.
References
- 1.Laurant M, Sergison M, Halliwell S, Sibbald B. Evidence based substitution of doctors by nurses in primary care. BMJ. 2000;320(2):1078. [PMC free article] [PubMed] [Google Scholar]
- 2.Leprohon J, Patel VL. Decision-making strategies for telephone triage in emergency medical services. Med Decis Making. 1995;15:240–53. doi: 10.1177/0272989X9501500307. [DOI] [PubMed] [Google Scholar]
- 3.Rothwell E, Ellington L, Planalp S, Crouch B. Exploring challenges to Telehealth communication by specialists in poison information. Qual Health Res. 2012;22(1):67–75. doi: 10.1177/1049732311420446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Huibers L, Smits M, Renaud V, Giesen P, Wensing M. Safety of telephone triage in out-of-hours care: a systematic review. Scand J Prim Health Care. 2011;29(4):198–209. doi: 10.3109/02813432.2011.629150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Holmström I, Höglund AT. The faceless encounter: ethical dilemmas in telephone nursing. J Clin Nurs. 2007;16:1865–71. doi: 10.1111/j.1365-2702.2007.01839.x. [DOI] [PubMed] [Google Scholar]
- 6.Cresswell JW, Clark VLP. Designing and conducting mixed methods research. 2nd ed. Thousand Oaks: Sage Publications; 2011.
- 7.Derkx HP, Rethans J-JE, Maiburg BH, Winkens RA, Muijtjens AM, van Rooij HG, et al. Quality of communication during telephone triage at Dutch out-of-hours centres. Patient Educ Couns. 2009;74(2):174–8. doi: 10.1016/j.pec.2008.08.002. [DOI] [PubMed] [Google Scholar]
- 8.Derkx HP, Rethans JJE, Knottnerus JA, Ram PM. Assessing communication skills of clinical call handlers working at an out-of-hours centre: development of the RICE rating scale. Br J Gen Pract. 2007;57:383–7. [PMC free article] [PubMed] [Google Scholar]
- 9.Malterud K. The art and science of clinical knowledge: evidence beyond measures and numbers. Lancet. 2001;358(9279):397–400. doi: 10.1016/S0140-6736(01)05548-9. [DOI] [PubMed] [Google Scholar]
- 10.Barfod C, Lauritzen MMP, Danker JK, Sölétormos G, Forberg JL, Berlac PA, et al. Abnormal vital signs are strong predictors for intensive care unit admission and in-hospital mortality in adults triaged in the emergency department - a prospective cohort study. Scand J Trauma Resusc Emerg Med. 2012;20:28. doi: 10.1186/1757-7241-20-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Liu JLY, Wyatt JC, Deeks JJ, Clamp S, Keen J, Verde P, et al. Systematic reviews of clinical decision tools for acute abdominal pain. Health Technol Assess. 2006;10(47):1–167. doi: 10.3310/hta10470. [DOI] [PubMed] [Google Scholar]
- 12.Linell P. Rethinking language, mind, and world dialogically. 1. Charlotte, US: Information Age publishing, INC; 2009. [Google Scholar]
- 13.Frank AW. What is dialogical research, and why should we do it? Qual Health Res. 2005;15(7):964–74. doi: 10.1177/1049732305279078. [DOI] [PubMed] [Google Scholar]
- 14.Fioratou E, Flin R, Glavin R. No simple fix for fixation errors: cognitive processes and their clinical applications. Anaesthesia. 2010;65(1):61–9. doi: 10.1111/j.1365-2044.2009.05994.x. [DOI] [PubMed] [Google Scholar]
- 15.Hakimnia R, Holmström IK, Carlsson M, Höglund AT. Exploring the communication between telenurse and caller-a critical discourse analysis. Int J Qual Stud Health Well-being. 2014;9:1–9. doi: 10.3402/qhw.v9.24255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Purc-Stephenson RJ, Thrasher C. Nurses’ experiences with telephone triage and advice: a meta-ethnography. J Adv Nurs. 2010;66:482–94. doi: 10.1111/j.1365-2648.2010.05275.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Available upon request/not applicable


