ABSTRACT
Glutathionylation, the formation of reversible mixed disulfides between glutathione and protein cysteine residues, is a posttranslational modification previously observed for intracellular proteins of bacteria. Here we show that Yersinia pestis LcrV, a secreted protein capping the type III secretion machine, is glutathionylated at Cys273 and that this modification promotes association with host ribosomal protein S3 (RPS3), moderates Y. pestis type III effector transport and killing of macrophages, and enhances bubonic plague pathogenesis in mice and rats. Secreted LcrV was purified and analyzed by mass spectrometry to reveal glutathionylation, a modification that is abolished by the codon substitution Cys273Ala in lcrV. Moreover, the lcrVC273A mutation enhanced the survival of animals in models of bubonic plague. Investigating the molecular mechanism responsible for these virulence attributes, we identified macrophage RPS3 as a ligand of LcrV, an association that is perturbed by the Cys273Ala substitution. Furthermore, macrophages infected by the lcrVC273A variant displayed accelerated apoptotic death and diminished proinflammatory cytokine release. Deletion of gshB, which encodes glutathione synthetase of Y. pestis, resulted in undetectable levels of intracellular glutathione, and we used a Y. pestis ΔgshB mutant to characterize the biochemical pathway of LcrV glutathionylation, establishing that LcrV is modified after its transport to the type III needle via disulfide bond formation with extracellular oxidized glutathione.
KEYWORDS: macrophage, Yersinia pestis, glutathionylation, innate immunity, plague, ribosomal protein S3 (RPS3)
IMPORTANCE
Yersinia pestis, the causative agent of plague, has killed large segments of the human population; however, the molecular bases for the extraordinary virulence attributes of this pathogen are not well understood. We show here that LcrV, the cap protein of bacterial type III secretion needles, is modified by host glutathione and that this modification contributes to the high virulence of Y. pestis in mouse and rat models for bubonic plague. These data suggest that Y. pestis exploits glutathione in host tissues to activate a virulence strategy, thereby accelerating plague pathogenesis.
INTRODUCTION
Glutathione, the predominant low-molecular-weight (LMW) peptide thiol present in all mitochondrial eukaryotes and nearly all Gram-negative bacteria, exists as a redox couple between its reduced (GSH) and oxidized (GSSG) forms and plays a pivotal role in many physiological processes (1). In Escherichia coli, glutathione maintains the proper oxidation state of protein thiols, regulates intracellular potassium levels, detoxifies methylglyoxal and halogenated compounds, and protects bacteria against acidic, oxidative, and osmotic stresses (2). Protein glutathionylation, a posttranslational modification whereby the sulfhydryl of glutathione forms a reversible mixed disulfide with protein cysteine residues, is increased during oxidative stress and protects reactive protein thiols from potentially irreversible oxidation (3). Glutathione in body fluids of vertebrates has been shown to impact the pathogenesis of bacterial infections by regulating the expression of microbial virulence functions or by protecting against oxidative and nitrosative stresses (4–6). A role for extracellular glutathione in modifying the surface of bacterial pathogens has heretofore not been described.
Yersinia pestis, the etiologic agent of plague, has killed more people worldwide than any other infectious agent (7). This bacterium employs a specialized type III secretion system to evade and neutralize the immune responses of its mammalian hosts (8). Particularly significant in this respect is the multifunctional virulence factor LcrV, the plague-protective antigen and needle cap protein of the Yersinia type III secretion machine (9, 10). LcrV is essential for plague pathogenesis (11) as the polypeptide enables the transport of Yersinia effector proteins (Yops) across the eukaryotic plasma membrane, where they exert cytotoxic and immunomodulatory effects within host immune cells (12). Here we report that Y. pestis LcrV is glutathionylated at cysteine residue 273 and that this modification impacts the pathogenesis of plague infections.
RESULTS AND DISCUSSION
LcrV, the cap protein of Y. pestis type III secretion machines, is glutathionylated at Cys273.
LcrVS228 carries a Strep-tag insertion at amino acid 228 that does not affect its function (13). LcrVS228 was purified from the culture supernatant of Y. pestis KLD29 ΔlcrV(pKG48), and the recombinant form of LcrVS228 (rLcrVS228) was purified from extracts of E. coli DH5α(pKG48). Both proteins were analyzed by combined liquid chromatography-electrospray ionization mass spectrometry (LC-ESI-MS) to reveal average masses of 38,594.4 Da (LcrVS228) and 38,284.9 Da (rLcrVS228) (Fig. 1A; see Fig. S1A and B in the supplemental material). Y. pestis LcrVS228 was 309.5 Da heavier than E. coli rLcrVS228 and 314.2 Da heavier than the calculated mass for the 334-amino-acid protein with the initiator methionine (38,280.22 Da). Edman degradation of Y. pestis LcrVS228 released N-terminal amino acids with the sequence NH2-MIRA-CO2H, identical to the predicted protein sequence (11) (Fig. S1C). To locate the site of the modification, reverse-phase-purified Y. pestis LcrVS228 and E. coli rLcrVS228 were treated with trypsin, and overlapping cleavage maps from LC-ESI-MS data were compared (see Table S1 in the supplemental material). These experiments identified peptide 270-284 (NH2-DNNELSHFATTCSDK-CO2H) as the site of the modification in Y. pestis LcrVS228 because its measured monoisotopic mass (1,985.79 Da) was 305.08 Da heavier than that obtained for rLcrVS228 (1,680.71 Da), which is in close agreement with the calculated mass for the predicted peptide (1,680.70 Da) (Table S1). Collisionally induced dissociation of the 1,985.79-Da LcrVS228 peptide generated fragment ions that identified Cys273 as the site of modification (see Table S2 in the supplemental material). Treatment with dithiothreitol (DTT), a disulfide reductant, collapsed the average mass of Y. pestis LcrVS228 to match the mass of rLcrVS228, which was unaffected by DTT treatment (Fig. 1B). DTT treatment of the Y. pestis LcrVS228 tryptic digest resulted in disappearance of the 1,985.79-Da signal, with appearance of a peptide with molecular mass of 1,680.71 Da, which on the basis of high-performance liquid chromatography (HPLC) retention time and molecular mass was indistinguishable from the corresponding rLcrVS228 peptide (Fig. 1B). On the basis of mass concordance, these data suggest that Cys273 of Y. pestis LcrVS228 forms a disulfide with glutathione (calculated residue monoisotopic mass of 305.07 Da). Confirming this conclusion, Y. pestis LcrVS228, but not E. coli rLcrVS228, was recognized by an antibody specific for glutathione (Fig. 1C).
FIG 1 .
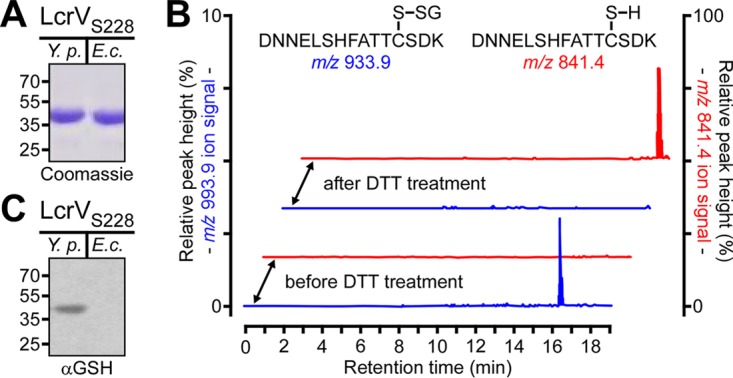
LcrV secreted by Y. pestis is glutathionylated at Cys273. (A) Coomassie-stained SDS-PAGE of LcrVS228 purified via Strep-Tactin affinity chromatography from either the culture supernatant of Y. pestis KLD29(pKG48) (Y.p.) or cell lysates of E. coli DH5α(pKG48) (E.c.). (B) Reconstructed ion traces for the unmodified (m/z 841.4) [(M+2H)2+ ion of 1,680.71] and glutathione-modified (m/z 993.9) [(M+2H)2+ ion of 1,985.79] tryptic peptides from the Y. pestis LcrVS228 protein encompassing Cys273 before and after treatment with dithiothreitol (DTT). The chromatograms show the absence of the unmodified peptides and the presence of the glutathione-modified peptides before treatment and following DTT treatment, the presence of the unmodified peptides, and the absence of the glutathione-modified peptides. (C) LcrVS228 purified from Y. pestis culture supernatants or E. coli extracts (rLcrVS228) was analyzed by immunoblotting with glutathione-specific antiserum (αGSH).
Mass determination and Edman sequencing of LcrVS228. (A and B) Molecular mass spectra of (A) rLcrVS228 purified from cell extracts of E. coli DH5α(pKG48) or (B) LcrVS228 purified from culture supernatants of Y. pestis KLD29 ΔlcrV(pKG48) were reconstructed from the multiply charged ions recorded during combined liquid chromatography-electrospray ionization mass spectrometry (LC-ESI-MS). (A) The representative molecular mass spectrum of E. coli rLcrVS228 reveals a predominate isoform with a measured mass of 38,284.9 ± 1.4 Da, which corresponds to the full-length LcrVS228 protein, and a second isoform with measured mass of 38,152.8 ± 1.5 Da, which corresponds to the LcrVS228 protein lacking the initiator methionine residue. Data are means ± SEM (n = 9). (B) A representative molecular mass spectrum of Y. pestis LcrVS228 reveals a single predominant isoform with a measured mass of 38,594.4 ± 2.3 Da, which is 314.2 Da heavier than the calculated mass for full-length LcrVS228. Data are means ± SEM (n = 6). (C) LcrVS228 was purified from Y. pestis supernatants and subjected to Edman sequencing; the preponderant N-terminal amino acid released for each cycle (and its picomole abundance) is listed. Download FIG S1, TIF file, 5.1 MB (5.2MB, tif) .
Copyright © 2017 Mitchell et al.
This content is distributed under the terms of the Creative Commons Attribution 4.0 International license.
Summary of mass spectrometry analysis of tryptic peptides from Y. pestis LcrVS228 and E. coli rLcrVS228. Download TABLE S1, DOCX file, 0.1 MB (19.2KB, docx) .
Copyright © 2017 Mitchell et al.
This content is distributed under the terms of the Creative Commons Attribution 4.0 International license.
Tandem mass spectrometry of the 1,985.79-Da LcrVS228 peptide. Download TABLE S2, DOCX file, 0.1 MB (19.1KB, docx) .
Copyright © 2017 Mitchell et al.
This content is distributed under the terms of the Creative Commons Attribution 4.0 International license.
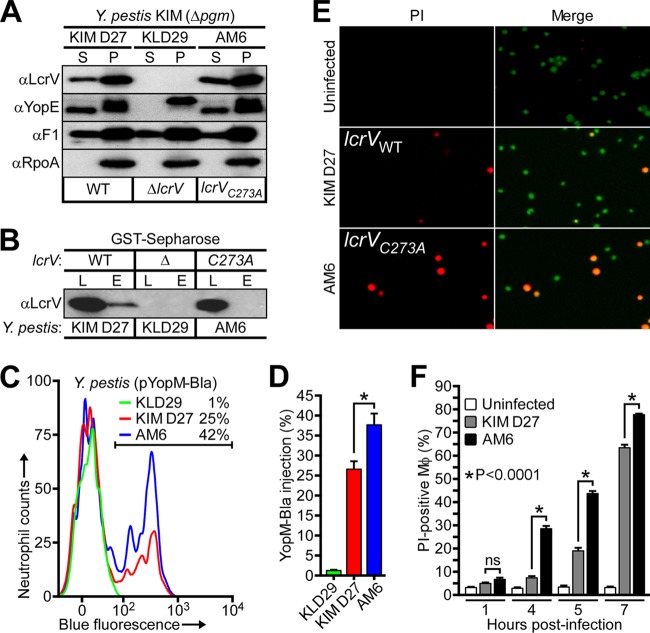
lcrVC273A accelerates Y. pestis killing of macrophages and increases type III injection of effectors into neutrophils.
Unlike wild-type (WT) Y. pestis (KIM D27), the ΔlcrV mutant (KLD29) did not secrete YopE via the type III pathway (Fig. 2A). The lcrVC273A mutation did not impact type III secretion of YopE or LcrV in either low-calcium-induced broth cultures or during Yersinia infection of HeLa tissue cell cultures (Fig. 2A; see Fig. S2A and B in the supplemental material). We wondered whether Y. pestis KIM D27 Δpgm, a nonpigmented plague strain (14) and parent of the Y. pestis KLD29 ΔlcrV variant (13), secretes glutathionylated LcrV. Because the glutathione-specific antibody, due to its low affinity (15), failed to detect LcrV in Y. pestis extracts, we used glutathione S-transferase (GST)-Sepharose as bait for enrichment of glutathionylated LcrV. Culture supernatants of Y. pestis KIM D27 and AM6 lcrVC273A were subjected to GST-Sepharose affinity chromatography, and the eluate was analyzed with LcrV-specific antibody to reveal that wild-type LcrV, but not LcrVC273A, was selectively retained (Fig. 2B). Thus, Y. pestis KIM D27 LcrV is glutathionylated similarly to LcrVS228.
FIG 2 .
The lcrVC273A mutation abolishes LcrV glutathionylation and accelerates Y. pestis-mediated macrophage death. (A) Y. pestis KIM D27 lcrV, KLD29 ΔlcrV, and AM6 lcrVC273A were induced for type III secretion by growth at 37°C in M9-Casamino Acids (M9-Ca) minimal medium lacking exogenous calcium ions. Proteins in the supernatant (S) and bacterial pellet (P) were separated by centrifugation and identified by immunoblotting with rabbit antibodies specific for type III secretion substrates (LcrV and YopE), the secreted F1 pilus subunit (F1), and, as a fractionation control, cytoplasmic RNA polymerase subunit A (RpoA). (B) LcrV secreted by the indicated Y. pestis strains was assayed for glutathionylation by subjecting the culture supernatant to GST-Sepharose affinity chromatography. The load (L) and eluate (E) fractions were analyzed by immunoblotting with anti-LcrV. (C and D) Type III effector (YopM-Bla)-mediated cleavage of CCF2-AM-stained human polymorphonuclear leukocytes infected with Y. pestis KIM D27(pYopM-Bla), KLD29(pYopM-Bla), or AM6(pYopM-Bla) was analyzed via flow cytometry for blue fluorescence (YopM-Bla cleavage of CCF2-AM). (C) Representative histograms show the blue fluorescence traces of Y. pestis-infected neutrophils; the percentage of YopM-Bla-injected neutrophils (blue cells) is indicated above the gating scheme that was used to measure blue fluorescence above background. (D) Percentage of quantification of YopM-Bla-injected human neutrophils. Data are means ± standard errors of the means (SEM) (n = 3). *, P < 0.05, by two-tailed unpaired Student’s t test. (E and F) The kinetics of host cell death were examined by infecting murine J774.A1 macrophages with Y. pestis KIM D27 or AM6 and enumerating propidium iodide (PI)-positive cells. (E) Macrophages, either left uninfected or infected with Y. pestis KIM D27 or AM6, were stained with membrane-permeant (Hoechst [blue]) and membrane-impermeant (PI [red]) dyes and analyzed by fluorescence microscopy to determine Y. pestis-mediated macrophage death (PI positive, red, and Hoechst positive, magenta). (F) The kinetics of cell death were examined by quantifying PI-positive macrophages at timed intervals following Y. pestis infection. Data are means ± SEM (n = 3). *, P < 0.0001, and ns, not significant, by two-tailed unpaired Student’s t test.
The codon substitution Cys273Ala, which precludes LcrV glutathionylation, does not affect Y. pestis type III secretion of Yop effectors. (A) Densitometric quantification of LcrV and YopE secreted by Y. pestis KIM D27 (Δpgm lcrV), KLD29 (Δpgm ΔlcrV), and AM6 (Δpgm lcrVC273A) following growth at 37°C in M9-Ca minimal medium in the absence of exogenous calcium ions. The immunoreactive signal of each secreted protein (S) was normalized to its total abundance in the medium and pellet (S + P); the ratio of secreted protein to total protein, (S)/(S + P) is presented as a percent average. ND, no immunoreactive signal detected. (B) Compared to uninfected HeLa cells, infection by Y. pestis KIM D27 or AM6 causes actin cable rearrangements and cytotoxicity (cell rounding) as detected by differential interference contrast (DIC) or fluorescence microscopy of rhodamine-phalloidin-stained cells. (C and D) Y. pestis CO92 pgm+ lcrV, LQ1 pgm+ ΔlcrV, and TD1 pgm+ lcrVC273A were induced for type III secretion by growth at 37°C in M9-Ca minimal medium with chelated calcium ions; secreted proteins (S) were separated from intact bacteria (P) by centrifugation. (C) Representative immunoblot analysis was performed by probing fractions with antibodies specific for type III secretion substrates (LcrV and YopE), the secreted F1 pilus subunit (F1), and a cytoplasmic fractionation control (RpoA). (D) The percentage of secretion of LcrV and YopE was determined by densitometry. ND, no immunoreactive signal detected. (E) LcrV secreted by the indicated Y. pestis strains was assayed for glutathionylation by subjecting the culture supernatant to GST-Sepharose affinity chromatography. The load (L) and eluate (E) fractions were analyzed by immunoblotting with anti-LcrV. All data are means ± SEM (n = 3). ns, not significant by two-tailed unpaired Student’s t test. Download FIG S2, TIF file, 22.3 MB (22.8MB, tif) .
Copyright © 2017 Mitchell et al.
This content is distributed under the terms of the Creative Commons Attribution 4.0 International license.
We investigated the impact of LcrV glutathionylation on Y. pestis infection of host immune cells. Following infection of human neutrophils, Y. pestis effector injection was measured by the conversion of the CCF2-AM fluorophore (green) to its YopM-Bla-cleaved chromophore (blue) (8), which occurred to a greater extent with Y. pestis AM6 relative to Y. pestis KIM D27 (Fig. 2C and D). During infection of murine J774.A1 macrophages, Y. pestis effector secretion triggers apoptotic cell death as well as a low level of pyroptotic cell death, and overall cytotoxicity can be quantified by enumerating propidium iodide (PI)-positive cells (16). Y. pestis AM6-mediated killing of J774.A1 macrophages occurred with significantly increased kinetics compared to Y. pestis KIM D27 (Fig. 2E and F). Prior work has demonstrated that, during in vivo pathogenesis as well as ex vivo infection of splenocytes, Y. pestis selectively targets neutrophils, macrophages, and dendritic cells for injection of Yops in order to evade and eliminate the innate immune responses of its mammalian host (8, 17). For this reason, our observation that glutathionylated LcrV impedes Y. pestis type III injection of Yop effectors and the killing of innate immune cells suggests that this modification could play a role in mediating Y. pestis target cell preference during bacterial pathogenesis.
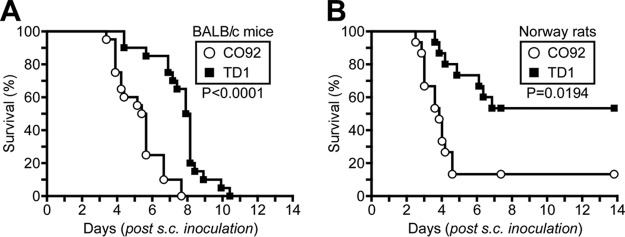
Glutathionylated LcrV is associated with enhanced virulence in rodent models of bubonic plague.
To examine whether the glutathionylation of LcrV impacts bubonic plague pathogenesis, we introduced the lcrVC273A mutation into Y. pestis CO92 pgm+ lcrV, a pigmented plague strain isolated from a fatal case of human plague in Colorado (18), resulting in the generation of Y. pestis TD1 pgm+ lcrVC273A. Genome sequencing confirmed that apart from the Cys273Ala codon substitution in lcrV, Y. pestis CO92 and TD1 were genetically identical. Y. pestis CO92 and TD1 catalyzed type III secretion of LcrV and YopE at similar rates (Fig. S2C and D). GST-Sepharose affinity chromatography detected the glutathionylation of LcrV secreted by Y. pestis CO92 but not by the lcrVC273A variant Y. pestis TD1 (Fig. S2E).
Nonenzootic mammalian hosts are highly susceptible to Y. pestis infection, a disease process that can be modeled by subcutaneous challenge of laboratory mice (cohorts of 6- to 8-week-old female BALB/c mice [n = 20]). Whereas the ΔlcrV mutant is avirulent in this model, Y. pestis CO92 causes lethal bubonic plague at a 50% lethal dose (LD50) of 1 to 5 bacteria (19). When analyzed in BALB/c mice by subcutaneous inoculation of 20 CFU Y. pestis CO92 or TD1, all mice succumbed to lethal plague disease by 11 days postchallenge (Fig. 3A). Nevertheless, mice infected by Y. pestis TD1 were slow to exhibit the characteristic features of plague disease (ruffled fur and hunched posture), and the median time to death of Y. pestis TD1-infected mice was delayed by 2.5 days relative to that of mice infected with Y. pestis CO92 (Fig. 3A). Animals were euthanized after exhibiting the symptoms of terminal plague disease: laterally recumbent and lethargic with rapid respiration. We examined Y. pestis colonization and dissemination in moribund BALB/c mice that were euthanized between 4 and 7 days postinfection. At the terminal stage of disease, the bacterial loads in the regional lymph node and spleen were similar for all Y. pestis-infected mice (see Fig. S3A in the supplemental material).
FIG 3 .
Glutathionylation of LcrV enhances bubonic plague pathogenesis. (A) Survival of cohorts of BALB/c mice (n = 20) infected via subcutaneous (s.c.) inoculation with 20 CFU of Y. pestis CO92 lcrV or Y. pestis TD1 lcrVC273A. WT versus lcrVC273A, P < 0.0001. (B) Survival of cohorts of Brown Norway rats (n = 15) infected via subcutaneous inoculation with 500 CFU of Y. pestis CO92 or TD1. WT versus lcrVC273A, P = 0.0194. Statistical analysis was performed using the Gehan-Breslow-Wilcoxon test. Data are representative of two independent experiments.
Kinetics of disease progression and host adaptive immune responses in bubonic plague-infected rodents. (A) BALB/c mice or (B to F) Brown Norway rats were infected by subcutaneous injection into the left inguinal fold with 20 CFU or 500 CFU, respectively, of Y. pestis CO92 pgm+ lcrV or Y. pestis TD1 pgm+ lcrVC273A. (A) Bacterial load in the regional lymph node and spleen of moribund BALB/c mice (n = 5) that were euthanized between 4 and 7 days postchallenge after exhibiting the symptoms of terminal illness. (B) Cohorts of Brown Norway rats (n = 5) were euthanized 72 h postchallenge to analyze the kinetics of bacterial replication in the regional lymph node as well as the kinetics of bacterial dissemination to the spleen. (C) Moribund rats (n = 5) that were euthanized between 4 and 7 days postchallenge were analyzed for disease progression by assessing the bacterial burden in the regional lymph node and spleen. (D to F) Bubonic plague-infected Brown Norway rats that survived for 14 days postchallenge were euthanized and necropsied. (D) Bacterial loads in the regional lymph node and spleen. (Note that since only two rats survived Y. pestis CO92 infection, necropsies were performed on two survivors—selected at random—of Y. pestis TD1 infection.) For rats surviving Y. pestis infection, serum IgG antibody titers for (E) LcrV or (F) capsular fraction F1 were quantified by ELISA. In panels A to D, the dotted lines represent the limit of detection, and red lines indicate geometric means. Statistical analysis was performed using the Mann-Whitney U test. In panels E and F, red lines indicate arithmetic means. Statistical analysis was performed using the two-tailed unpaired Student’s t test. All data are representative of two independent experiments. Download FIG S3, TIF file, 27.9 MB (28.5MB, tif) .
Copyright © 2017 Mitchell et al.
This content is distributed under the terms of the Creative Commons Attribution 4.0 International license.
Bubonic plague pathogenesis was also examined in Brown Norway rats (Rattus norvegicus), an enzootic species that is moderately resistant to challenge with Y. pestis CO92, which causes bubonic disease in rats at an LD50 of 1,000 to 5,000 CFU (20). Cohorts of 6-week-old female Rattus norvegicus animals (n = 15) were infected by subcutaneous injection into the left inguinal fold with 500 CFU Y. pestis CO92 or TD1. Whereas only 13% (2/15) of the rats survived bubonic plague infection with Y. pestis CO92, 53% (8/15) of infected rats survived the Y. pestis TD1 challenge (Fig. 3B). Bubonic plague-infected rats (n = 5) were also euthanized at 3 days postchallenge to monitor disease progression. Compared to Y. pestis CO92-infected rats, rats infected with Y. pestis TD1 displayed a reduction in the kinetics of replication in the regional lymph node (4.4 × 107 CFU CO92 versus 1.5 × 105 CFU TD1; P = 0.24) as well as in the kinetics of dissemination to the spleen (3.2 × 108 CFU CO92 versus 1.4 × 106 CFU TD1; P = 0.75); due to the small cohort size of rats surviving Y. pestis CO92 challenge, the observed differences were not statistically significant (Fig. S3B).
Rats euthanized between 4 and 7 days postchallenge were analyzed for disease progression. At the terminal stage of bubonic plague disease, Y. pestis CO92 and TD1 had replicated to similar levels in the regional lymph node as well as the spleen (Fig. S3C). Rats that survived bubonic plague infection for 14 days were euthanized and necropsied. All survivors of Y. pestis CO92 and TD1 challenge lacked detectable levels of plague bacteria in their spleens, nor was there a statistically significant difference in the number of viable plague bacteria in the regional lymph nodes of surviving animals (1.2 × 107 CFU CO92 versus 1.0 × 102 CFU TD1; P = 0.67) (Fig. S3D). Moreover, no difference in antibody titers against LcrV or capsular fraction 1 (F1), the predominant plague antigen, was detectable in serum from Y. pestis CO92- and TD1-infected animals (Fig. S3E and F). Together these data indicate that a single amino acid substitution (Cys273Ala) associated with loss of LcrV glutathionylation increases the survival of bubonic plague-infected rats.
Serine substitution at LcrV residue 273.
The plague pathogen evolved in the rodent population of China (21), where isolates are still scattered over multiple phylogenetic branches (22, 23). The pCD1-encoded type III secretion machine and its lcrV gene are conserved among all members of this clade, albeit that a polymorphism substituting LcrV Cys273Ser is found in some isolates of the Y. pestis biovar microtus, which does not cause plague in humans (24), and in the Y. pestis biovar pestoides Angola isolate (25) (see Fig. S4A in the supplemental material). A previous study reported that the lcrVC273S polymorphism impacts the oligomerization of LcrV and represents one out of four highly variable regions of LcrV that are unique to nonepidemic strains of Y. pestis (26). Since the lcrVC273A mutation was associated with attenuated virulence in animal models of bubonic plague, we asked whether the lcrVC273S mutation causes a similar phenotype when introduced into modern plague strains. The codon substitution Cys273Ser was introduced into the lcrV alleles of Y. pestis KIM D27 and Y. pestis CO92 to generate Y. pestis AM15 Δpgm lcrVC273S and Y. pestis DE1 pgm+ lcrVC273S, respectively. Y. pestis KIM D27 lcrV and AM15 lcrVC273S catalyzed type III secretion of YopE and LcrV into the extracellular medium at similar rates (Fig. S4B and C). LcrV secreted by Y. pestis AM15 was not retained during GST-Sepharose affinity chromatography, suggesting that Ser273 was not modified with glutathione (Fig. S4D). To validate this conjecture, LcrVS228 C273S was affinity purified from the culture supernatant of Y. pestis KLD29 ΔlcrV(pAM199) (Fig. S4E). When analyzed by matrix-assisted laser desorption ionization–time of flight mass spectrometry (MALDI-TOF MS) along with recombinant rLcrVS228 C273S purified from E. coli DH5α(pAM199) lysates, we observed m/z 38,261.34 for LcrVS228 C273S and m/z 38,286.09 for rLcrVS228 C273S (Fig. S4E; see Table S4 in the supplemental material). These measurements approximate the calculated mass for unmodified LcrVS228 C273S (38,264.16 Da), suggesting that LcrVS228 C273S is not posttranslationally modified with glutathione (Table S4). Following infection of human neutrophils, Y. pestis AM15(pYopM-Bla), compared to Y. pestis KIM D27(pYopM-Bla), caused a small but statistically insignificant increase in the conversion of CCF2-AM fluorophore to the YopM-Bla-cleaved chromophore (blue) (Fig. S4F and G). Y. pestis CO92 lcrV and Y. pestis DE1 lcrVC273S exported type III effectors into the extracellular milieu at similar levels (Fig. S4H and I). When analyzed in a mouse model of bubonic plague following subcutaneous inoculation of 20 CFU, all Y. pestis CO92- or DE1-infected animals succumbed to lethal plague disease. Similar to mice infected with Y. pestis TD1 lcrVC273A, Y. pestis DE1 lcrVC273S infection caused a delay in time to death (Fig. S4J). Taken together, these data suggest that the codon 273 polymorphism (lcrVC273S) observed in Y. pestis biovar pestoides and microtus isolates (26) prevents LcrV glutathionylation and affects bubonic plague pathogenesis.
The codon substitution Cys273Ser abolishes Y. pestis posttranslational modification of LcrV and attenuates virulence in a mouse model of bubonic plague. (A) Y. pestis isolates and nucleotide sequences at codons 272 to 273 (nucleotides 814 to 819 of Y. pestis CO92 lcrV) that impact codon 273 (Cys or Ser). (B and C) Following growth at 37°C in M9-Ca minimal medium lacking calcium ions, cultures of Y. pestis KIM D27 Δpgm lcrV or AM15 Δpgm lcrVC273S were fractionated and analyzed for type III secretion. (B) Representative immunoblot analysis was performed by probing supernatant (S) and pellet (P) fractions with the indicated rabbit antibodies. (C) Percentages of secretion of YopE and LcrV were determined by densitometric quantification of immunoreactive signals. (D) Y. pestis culture supernatants were subjected to GST-Sepharose affinity chromatography. The load (L) and eluate (E) fractions were immunoblotted with LcrV-specific antisera to assay for the secretion of glutathionylated LcrV. (E) Y. pestis KLD29 ΔlcrV and E. coli DH5α strains expressing LcrVS228 C273S (pAM199) were propagated in LB broth at 37°C. LcrV was affinity purified from Y. pestis culture supernatants (LcrVS228 C273S) or E. coli lysates (rLcrVS228 C273S), visualized by Coomassie-stained SDS-PAGE, and analyzed by MALDI-TOF MS. The experimentally observed m/z of each LcrVS228 C273S preparation is indicated. (F and G) Following infection with Y. pestis KIM D27(pYopM-Bla), KLD29(pYopM-Bla), or AM15(pYopM-Bla), human neutrophils were stained with CCF2-AM and analyzed by flow cytometry for blue fluorescence indicative of type III effector (YopM-Bla)-mediated cleavage of CCF2-AM. (F) Representative histograms show the blue fluorescence traces of Y. pestis-infected neutrophils; the percentage of YopM-Bla-injected neutrophils (blue cells) is indicated above the gating scheme that was used to measure blue fluorescence above background. (G) Percentage of quantification of YopM-Bla-injected human neutrophils. (H and I) Y. pestis CO92 pgm+ lcrV and DE1 pgm+ lcrVC273S were evaluated for type III secretion following growth at 37°C in M9-Ca minimal medium in the absence of exogenous calcium ions. (H) Representative immunoblot analysis of supernatant (S) and pellet (P) fractions. (I) Percentages of secretion of LcrV and YopE were determined by densitometry. (J) Survival of cohorts of BALB/c mice (n = 15) infected by subcutaneous injection into the left inguinal fold with 20 CFU of Y. pestis CO92 or DE1. The figure presents pooled data that were gathered from two independent experiments. For WT versus lcrVC273S, P = 0.0351 by Gehan-Breslow-Wilcoxon test. In panels C, G, and I, data are means ± SEM (n = 3). ns, not significant by two-tailed unpaired Student’s t test. Download FIG S4, TIF file, 25.8 MB (26.4MB, tif) .
Copyright © 2017 Mitchell et al.
This content is distributed under the terms of the Creative Commons Attribution 4.0 International license.
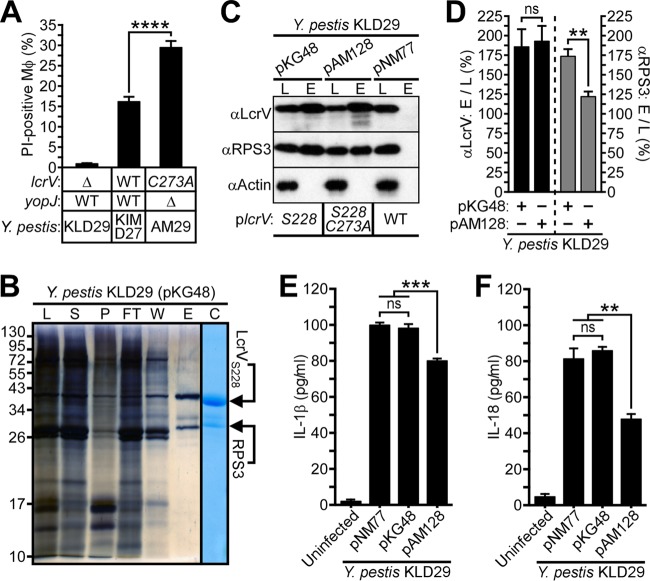
Decreased LcrV-RPS3 association is correlated with increased macrophage apoptosis and diminished cytokine release.
Earlier work demonstrated that YopJ, a type III effector injected into host immune cells, functions as an acetyltransferase that inhibits NF-κB and mitogen-activated protein kinase (MAPK) signaling, triggers caspase-1 activation and interleukin-1β (IL-1β) and IL-18 secretion, and also promotes target cell death in Y. pestis-infected macrophages (27, 28). Furthermore, yopJ has been shown to be dispensable for bubonic plague pathogenesis in Y. pestis-infected Brown Norway rats (29). Since loss of LcrV glutathionylation attenuated plague pathogenesis, we asked whether yopJ was required for or contributed to increased cytotoxicity in vitro by generating an in-frame yopJ deletion strain by allelic exchange with Y. pestis AM6. Significantly, the lcrVC273A-mediated increase in macrophage cell death during Y. pestis infection did not require yopJ, as Y. pestis AM29 lcrVC273A ΔyopJ also promoted increased macrophage cytotoxicity compared with Y. pestis KIM D27 (Fig. 4A; see Fig. S5A in the supplemental material).
FIG 4 .
LcrV binds to macrophage RPS3 and modulates host inflammatory responses. (A) Y. pestis-mediated death of J774.A1 macrophages was assessed 3 h postinfection by propidium iodide staining. (B) Y. pestis KLD29 lcrVS228(pKG48)-infected J774.A1 macrophages were subjected to Strep-Tactin affinity chromatography. The crude lysate (L), lysate supernatant (S), lysate pellet (P), flowthrough (FT), wash (W), and eluate (E) fractions were collected and analyzed by silver- and Coomassie-stained SDS-PAGE; bottom-up proteomics was used to identify the indicated protein bands as LcrVS228 and macrophage ribosomal protein S3 (RPS3). (C and D) Immunoblotting of lysate (L) and eluate (E) fractions generated during Strep-Tactin affinity chromatography reveals variable association between LcrV variants and RPS3 in J774.A1 macrophages infected with Y. pestis KLD29 ΔlcrV expressing wild-type lcrV (pNM77), lcrVS228 (pKG48), or lcrVS228 C273A (pAM128). (C) Representative immunoblot analysis of LcrV and RPS3 purified from Y. pestis-infected macrophages; actin levels were used as a loading control. (D) Densitometric quantification of the interaction between LcrVS228 and RPS3. Immunoreactive signals of Strep-Tactin-purified LcrV and RPS3 were normalized to the corresponding actin band; the ratio of eluate to lysate (E to L) is presented as a percent average. (E and F) Supernatants from J774.A1 macrophages, either left uninfected or infected with the indicated Y. pestis strains, were assayed by ELISA for (E) IL-1β or (F) IL-18. All data are means ± SEM (n = 3). **, P < 0.01; ***, P < 0.001; ****, P < 0.0001; ns, not significant.
yopJ is dispensable for lcrVC273A-mediated killing of Y. pestis-infected macrophages, and type III secretion is not impacted by loss of glutathione synethase (gshB). (A) An in-frame deletion of yopJ was introduced by allelic exchange with wild-type Y. pestis KIM D27 and its lcrVC273A variant, Y. pestis AM6, to generate Y. pestis AM27 lcrV ΔyopJ and Y. pestis AM29 lcrVC273A ΔyopJ, respectively. Murine J774.A1 macrophages were infected for 3 h with the indicated Y. pestis strains, and macrophage cell death was quantified by enumeratng propidium iodide (PI)-positive cells. (B) Partial HPLC chromatograms include a reaction blank that was used to identify peaks originating from the derivatization reaction in the absence of sample-derived thiols, a standard mixture containing 10 pmol of Cys, GSH, and γ-EC that was used to assign peak positions for the corresponding thiol-mBBr adducts on the basis of retention time, and sample runs for TMH medium and LB broth. (C and D) Densitometric quantification of LcrVS228 and YopE secreted by Y. pestis KLD29 ΔlcrV(pKG48) and AM43 ΔlcrV ΔgshB(pKG48) following growth in the presence (+Ca2+) or absence (−Ca2+) of calcium ions at 37°C in (C) LB broth or (D) TMH medium. The immunoreactive signal of each secreted protein (S) was normalized to its total abundance in the medium and pellet (S + P); the ratio of secreted protein to total protein, (S)/(S + P), is presented as a percent average. All data are means ± SEM (n = 3). ****, P < 0.0001, and ns, not significant, by two-tailed unpaired Student’s t test. Download FIG S5, TIF file, 30.9 MB (7.9MB, tif) .
Copyright © 2017 Mitchell et al.
This content is distributed under the terms of the Creative Commons Attribution 4.0 International license.
To investigate the molecular mechanism for LcrV-mediated killing of immune cells, we purified LcrVS228 via affinity chromatography from Y. pestis-infected J774.A1 macrophages and used mass spectrometry to identify proteins separated by Coomassie-stained SDS-PAGE (Fig. 4B; see Table S3 in the supplemental material). Infection of macrophages with Y. pestis KLD29 expressing LcrVS228 (pKG48), but not with Y. pestis KLD29 expressing wild-type LcrV (pNM77), led to purification of LcrVS228 and ribosomal protein S3 (RPS3), a component of the eukaryotic 40S ribosomal subunit and a regulator of DNA repair, apoptosis, and innate immune responses (30) (Fig. 4B and C; Table S3). Strikingly, analysis of J774.A1 macrophages infected with Y. pestis KLD29 expressing LcrVS228 C273A (pAM128) revealed that copurification of RPS3 with LcrVS228 C273A was diminished (Fig. 4C and D). Earlier work has shown that pathogenic E. coli effectors, injected into immune cells by type III secretion machines, target RPS3 to inhibit host immune defenses by modulating RPS3/NF-κB-mediated signaling and proinflammatory responses (30–32). We wondered whether the differential association between RPS3 and LcrV variants that was observed for Y. pestis-infected macrophages influences host inflammatory responses. The impact of LcrV glutathionylation on host inflammatory responses in Y. pestis-infected J774.A1 macrophages undergoing apoptotic or pyroptotic cell death was assessed by quantifying the caspase 1/11-induced cytokines IL-1β and IL-18 (33). Compared to Y. pestis KLD29 expressing wild-type LcrV (pNM77) or LcrVS228 (pKG48), Y. pestis KLD29 expressing LcrVS228 C273A (pAM128) caused a significant increase in nonpyroptotic cell death of J774.A1 macrophages, as suggested by reduced levels of IL-1β and IL-18 cytokine release (Fig. 4E and F). Thus, the association of LcrV with RPS3 may be involved in regulating macrophage cell death during Y. pestis infection and, reciprocally, perturbation of the RPS3 association with LcrV in Y. pestis-infected macrophages may be responsible for the decrease in disease severity as well as the increase in apoptotic cell death observed for the lcrVC273A variants (Fig. 2F, 3A and B, and 4D).
Peptide mass fingerprinting by LC-MS/MS identifies macrophage RPS3 as a ligand of translocated LcrV. Download TABLE S3, DOCX file, 0.1 MB (16.8KB, docx) .
Copyright © 2017 Mitchell et al.
This content is distributed under the terms of the Creative Commons Attribution 4.0 International license.
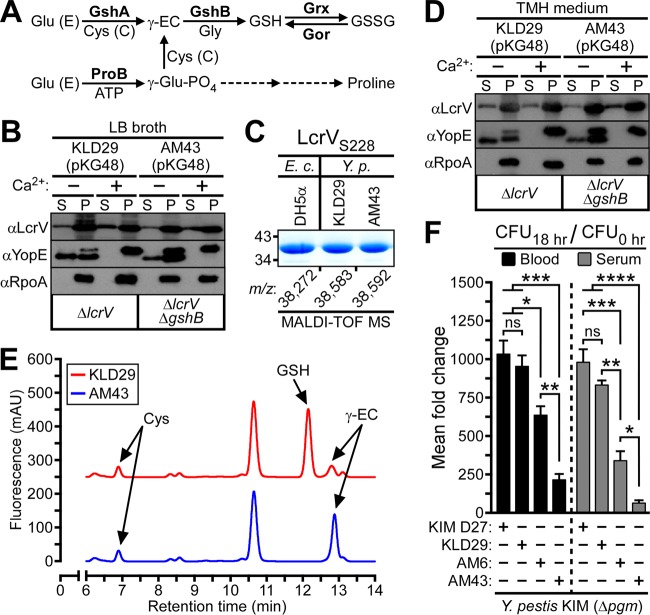
LcrV is modified via disulfide formation with extracellular glutathione.
In E. coli, a Gram-negative enterobacterium and relative of Y. pestis, the tripeptide glutathione (γ-glutamyl-cysteinyl-glycine [GSH]) can be synthesized through two pathways. The de novo GSH biosynthetic pathway is a two-step process catalyzed by the ATP-dependent enzymes γ-glutamylcysteine synthetase (GshA) and glutathione synthetase (GshB), whereby glutamate (Glu [E]) and cysteine (Cys [C]) are first ligated by GshA to form γ-glutamylcysteine (γ-EC), which is then conjugated to glycine by GshB to generate GSH (34, 35) (Fig. 5A). An alternate pathway for GSH synthesis was characterized in a ΔgshA mutant strain of E. coli and involves the first enzyme of the proline biosynthetic pathway, γ-glutamyl kinase (ProB), catalyzing the conversion of glutamate to γ-glutamyl phosphate, which in a condensation reaction with cysteine, generates γ-glutamylcysteine that is subsequently ligated to glycine by GshB to form GSH (36) (Fig. 5A). Glutathione is oxidized at its sulfhydryl to generate glutathione disulfide (GSSG), which, in turn, is reduced by the NADPH-dependent enzyme glutathione reductase (Gor) in order to maintain a high GSH/GSSG ratio in the bacterial cytoplasm (37) (Fig. 5A).
FIG 5 .
Extracellular glutathione modifies secreted LcrV and promotes Y. pestis survival in blood. (A) Pathways of glutathione biosynthesis in E. coli. Glu (E), glutamic acid; Cys (C), cysteine; GshA, γ-glutamylcysteine synthetase; GshB, glutathione synthetase; ProB, γ-glutamyl kinase; γ-EC, γ-glutamylcysteine; GSH, glutathione; GSSG, glutathione disulfide; Gor, glutathione reductase; Grx, glutaredoxin; γ-glutamyl-PO4, γ-glutamyl phosphate. (B) Y. pestis KLD29 ΔlcrV lcrVS228(pKG48) and AM43 ΔlcrV ΔgshB lcrVS228(pKG48) were grown at 37°C in LB broth, in either the presence or absence of calcium ions (Ca2+), and assayed for type III secretion by immunoblotting; proteins secreted into the supernatant (S) were separated from intact bacteria (P) by centrifugation. (C) Y. pestis and E. coli strains expressing LcrVS228 (pKG48) were propagated in LB broth. LcrV was purified from Y. pestis supernatants (LcrVS228) or E. coli extracts (rLcrVS228), visualized by Coomassie-stained SDS-PAGE, and analyzed by MALDI-TOF MS to reveal the m/z of each LcrVS228 purification sample. (D) Y. pestis strains were analyzed for calcium-regulated type III secretion in TMH medium. (E) Partial HPLC chromatograms of LMW thiol-mBBr derivatives extracted from Y. pestis cultures grown to the stationary phase in TMH medium. Peaks corresponding to Cys, GSH, and γ-EC were assigned on the basis of retention time by comparison to a chromatogram of thiol standards. (F) Approximately 105 CFU of Y. pestis KIM D27 lcrV, KLD29 ΔlcrV, AM6 lcrVC273A, or AM43 ΔlcrV ΔgshB was inoculated into 4 ml of defibrinated sheep blood or heat-inactivated sheep serum. Culture aliquots were removed before and after 18 h of growth at 37°C and plated on LB agar to enumerate bacterial load. Y. pestis growth was calculated as the mean fold increase in bacteria at the time of inoculation (CFU0 h) to bacteria recovered after the 37°C incubation (CFU18 h). Data are means ± SEM (n = 3). *, P < 0.05, **, P < 0.01, ***, P < 0.001, and ****, P < 0.0001, and ns, not significant, by one-way ANOVA with Tukey’s multiple-comparison posttest.
We asked whether LcrV glutathionylation occurs in the Y. pestis cytoplasm via thiol-disulfide exchange with GSSG or a mixed disulfide prior to its secretion and capping of the type III needle complex. As GshB is required for both the de novo and compensatory pathways of GSH synthesis, we generated an in-frame ΔgshB deletion strain by allelic exchange with Y. pestis KLD29. We hypothesized that ΔgshB mutant Y. pestis would be unable to synthesize glutathione and thereby preclude cytoplasmic, but not extracellular, glutathionylation of LcrV. When analyzed for type III secretion in Luria-Bertani (LB) broth, a rich medium that contains glutathione (Fig. S5B), Y. pestis KLD29 ΔlcrV(pKG48) and Y. pestis AM43 ΔlcrV ΔgshB(pKG48) exhibited calcium-regulated secretion of LcrVS228 and YopE (Fig. 5B; Fig. S5C). To assess glutathionylation of LcrV secreted by Y. pestis during growth in LB broth, LcrVS228 was affinity purified from Y. pestis KLD29(pKG48) and Y. pestis AM43(pKG48) and analyzed by MALDI-TOF MS to reveal m/z 38,583.10 and 38,592.16, respectively, which approximate the calculated mass for glutathionylated LcrVS228 (38,585.54 Da) (Fig. 5C; Table S4). Compared to the m/z of rLcrVS228 purified from E. coli DH5α(pKG48) grown in LB broth (38,271.66), these data suggest that LcrVS228 secreted by ΔgshB mutant Y. pestis is glutathionylated. Confirming this result, DTT treatment collapsed the measured masses of Y. pestis LcrVS228 to match the mass of rLcrVS228, which was unaffected by DTT treatment (Table S4). These data establish that LcrVS228 secreted by ΔgshB mutant Y. pestis during growth in LB broth is modified with glutathione.
MALDI-TOF MS analysis of LcrVS228 and LcrVS228 C273S purified from Y. pestis supernatants or E. coli extracts. Download TABLE S4, DOCX file, 0.1 MB (16.7KB, docx) .
Copyright © 2017 Mitchell et al.
This content is distributed under the terms of the Creative Commons Attribution 4.0 International license.
Following growth at 37°C in thoroughly modified Higuchi (TMH) medium, a chemically defined minimal medium that lacks glutathione (Fig. S5B), Y. pestis KLD29(pKG48) and Y. pestis AM43(pKG48) exhibited calcium-regulated export of LcrVS228 and YopE at similar rates (Fig. 5D; Fig. S5D). To investigate whether the ΔgshB mutation was sufficient to abolish bacterial glutathione synthesis, Y. pestis KLD29 and AM43 were propagated to stationary phase in TMH medium, and nonprotein thiols were acid extracted, reduced by treatment with tris(2-carboxyethyl)phosphine (TCEP), derivatized with the thiol-specific reagent monobromobimane (mBBr), and analyzed by high-performance liquid chromatography (HPLC) for the total abundance of cysteine, glutathione, and γ-glutamylcysteine in cell extracts. Compared to Y. pestis KLD29, the HPLC chromatogram of Y. pestis AM43 revealed an undetectable level of glutathione alongside a significant accumulation of its biosynthetic precursor, γ-glutamylcysteine (Fig. 5E). We infer from these data two conclusions. First, the glutathionylation of LcrV occurs after the protein is exported from the Y. pestis cytoplasm to cap the type III needle complex, and second, the molecular mechanism underpinning LcrV glutathionylation is thiol-disulfide exchange with oxidized glutathione in the extracellular milieu.
Glutathione promotes Y. pestis growth in mammalian blood and heat-inactivated serum.
The survival of Y. pestis in the blood of its mammalian host—as occurs during its initial trafficking from the site of fleabite inoculation to the regional lymph node and, more significantly, during its systemic hematogenous dissemination to colonize distal host tissues—is essential for bubonic plague pathogenesis (38). Recent studies of pathogenic bacteria identified mutations that, either by abolishing de novo glutathione synthesis or abrogating bacterial import of host-derived glutathione, result in attenuated virulence in animal models of infection and/or impaired survival in vertebrate blood (2). Glutathione has also been shown to play a significant role in bacterial pathogenesis by functioning as a thiol redox buffer that enables blood-borne pathogens to rapidly acclimate to the high osmolality and oxidative stresses inherent to animal blood (6). For these reasons, we investigated whether the lcrVC273A and ΔgshB mutations impact Y. pestis survival in defibrinated sheep blood by enumerating the mean fold change in viable CFU following 18 h of growth at 37°C. Unlike Y. pestis KIM D27 lcrV (1,034-fold increase in CFU), Y. pestis KLD29 ΔlcrV (954-fold increase), or Y. pestis AM6 lcrVC273A (636-fold increase), the CFU of Y. pestis AM43 ΔlcrV ΔgshB increased only 216-fold (Fig. 5F). Animal blood contains immune cells and factors facilitating complement-mediated cell lysis. To determine whether these antimicrobial properties of blood account for the diminished replication of ΔgshB mutants, Y. pestis survival was assayed in heat-inactivated sheep serum. Compared to the increase in viable CFU observed for Y. pestis KIM D27 (980-fold), Y. pestis KLD29 (832-fold), and Y. pestis AM6 (342-fold) following 18 h of growth at 37°C, growth in heat-inactivated sheep serum was diminished for Y. pestis AM43 (64-fold increase in CFU) (Fig. 5F). This result suggests that neither immune cells nor the complement system of defibrinated sheep blood is responsible for the observed growth defects of lcrVC273A or ΔgshB variant Y. pestis strains. As ΔgshB mutant Y. pestis exhibited a pronounced growth defect in both blood and heat-inactivated serum, we presume that the ΔgshB mutation may also attenuate the pathogenesis of Y. pestis in animal models of bubonic plague.
Although Y. pestis LcrV has been the subject of intensive study for decades, a complete understanding of its multifaceted contributions to plague pathogenesis continues to evolve. Here we demonstrate that LcrV is modified by host-derived glutathione following its export to the tip of the type III secretion machine. LcrV glutathionylation moderates the rate of Y. pestis type III effector injection into immune cells and enhances Y. pestis virulence in mouse and rat models of bubonic plague. We arrived at these conclusions when comparing the phenotypes of wild-type (Cys273) and lcrV mutant (Ala273) strains, where the amino acid side chains of LcrV residue 273 both display hydrophobic properties (methylene-sulfhydryl in cysteine and methyl in alanine); however, alanine, in contrast to cysteine, cannot be glutathionylated. On the other hand, the lcrV Ser273 mutant, in which the methylene-hydroxyl side chain at residue 273 exerts a polar character, displayed weaker phenotypes in both Y. pestis type III injection and plague virulence assays. We presume that the side chain of LcrV residue 273 occupies a critical position that may directly affect the type III injection of Y. pestis effectors. LcrV glutathionylation promotes also the association of LcrV with host RPS3 and suppresses the apoptotic killing of Y. pestis-infected macrophages. We think it is likely that the abundance of glutathione and the strong oxidizing environment in mammalian blood promote Cys273 glutathionylation. It is, however, not clear, whether LcrV glutathionylation is impacted during Y. pestis type III injection of effectors into immune cells, as the disulfide of LcrV glutathione may be exposed to the reducing environment of the host cell cytoplasm. LcrV glutathionylation promotes necroptotic cell death and IL-1β and IL-18 secretion, triggering inflammatory responses to plague infection that presumably enable Y. pestis to rapidly kill large numbers of immune cells via the type III mechanism or to disseminate with immune cells through host tissues. These activities of glutathionylated LcrV are correlated with its association with RPS3, a protein that resides in the cytoplasm of host cells. We presume that LcrV may gain access to RPS3 via the Y. pestis type III mechanism; however, the molecular details for these events are not known. In the absence of LcV glutathionylation, Y. pestis injects larger amounts of effectors into immune cells, an alteration that is associated with increased apoptotic cell death and diminished secretion of IL-1β and IL-18. This reduction in host inflammatory responses may delay Y. pestis type III-mediated killing of immune cells and the distribution of plague bacteria in host tissues, thereby attenuating Y. pestis virulence in animal models of plague pathogenesis. Intriguingly, the site of LcrV glutathionylation is located in a domain that is also known to modulate host immune responses by stimulating IL-10 release (39). To the best of our knowledge, LcrV glutathionylation represents the first report of a bacterial secreted virulence factor that is modified by glutathione. We wondered whether other virulence factors, whether secreted by Y. pestis or other bacterial pathogens, may likewise be modified by host-derived glutathione and contribute to the pathogenesis of infectious diseases. The lcrV genes of two related pathogens, Yersinia pseudotuberculosis and Yersinia enterocolitica, also carry a cysteine codon at position 273. In contrast, the genes for needle cap proteins in the type III pathways of many other bacterial pathogens are not endowed with cysteine codons. Thus, glutathionylation of the type III secretion needle cap protein may be unique to Yersinia spp. and not a universal attribute of pathogenic bacteria.
MATERIALS AND METHODS
Ethical conduct, biosafety, and biosecurity.
Experiments with blood from human volunteers were performed with protocols that had been reviewed, approved, and supervised by the University of Chicago’s Institutional Review Board (IRB). Animal research was performed in accordance with institutional guidelines following experimental protocol review, approval, and supervision by the Institutional Animal Care and Use Committee at The University of Chicago. Experiments with Y. pestis were performed in biosafety level 3 (BSL-3)/animal BSL3 (ABSL3) containment. The University of Chicago Select Agent Program is approved and routinely inspected by both Institutional Biosafety Committee and Centers for Disease Control and Prevention (CDC) officials. The manuscript was analyzed for dual-use research of concern (DURC): i.e., the description of mutations that may increase the virulence of natural isolates of Y. pestis or affect their ability to cause fulminant plague or epizootic outbreaks in rats or other host species. The analysis was reviewed by The University of Chicago Institutional Biosafety Committee DURC Task Force (DTF) and by the funding agency, the National Institute of Allergy and Infectious Diseases, which agreed with the investigators’ assessment that the findings presented in the manuscript do not present DURC.
Bacterial strains and plasmids.
The strains, plasmids, and primers used in this study are listed in Table S5 in the supplemental material (8, 13, 16, 18, 19, 40–43). Overnight cultures of Y. pestis were propagated at 26°C in heart infusion broth (HIB), M9-Casamino Acids (M9-Ca) minimal medium, or thoroughly modified Higuchi’s (TMH) medium. E. coli strains were propagated at 37°C in Luria-Bertani (LB) broth. When necessary, the growth medium was supplemented with ampicillin (100 µg/ml), kanamycin (50 µg/ml), or chloramphenicol (20 µg/ml) for plasmid maintenance. The lcrVC273A mutant strains (AM6 and TD1), the lcrVC273S mutant strains (AM15 and DE1), and the in-frame deletions in yopJ and gshB were generated via allelic exchange in Y. pestis KIM D27 and Y. pestis CO92, as previously described (16). For the construction of plasmids pAM128 (lcrVS228 C273A) and pAM199 (lcrVS228 C273S), the QuikChange Lightning site-directed mutagenesis kit was used to introduce the Cys273 codon substitution into the lcrVS228 allele carried by pKG48. For genome sequencing, DNA was extracted from Y. pestis strains CO92, TD1 lcrVC273A, and DE1 lcrVC273S using the Wizard Genomic DNA purification kit (Promega). The Next Generation Sequencing Core at Argonne National Laboratory used extracted DNA to generate TruSeq libraries (average insert size, 400 to 500 bp) that were sequenced on an Illumina MISeq system (250 by 250 bp, paired-end reads). The FASTQ formatted files of raw genomic sequencing data were analyzed with Geneious R9.0 to assemble and compare genomic sequences for single nucleotide polymorphism (SNP), indel, and structural variations. Compared with Y. pestis CO92, Y. pestis TD1 and Y. pestis DE1 carried the lcrVC273A and lcrVC273S mutations, respectively, without additional mutations affecting the coding sequence of proteins.
Bacterial strains, plasmids, and primers used in this study. Download TABLE S5, DOCX file, 0.1 MB (102.7KB, docx) .
Copyright © 2017 Mitchell et al.
This content is distributed under the terms of the Creative Commons Attribution 4.0 International license.
LcrV purification.
For purification of LcrVS228, Y. pestis KLD29(pKG48) overnight cultures were diluted 1:20 into 4 liters HIB, grown for 2 h at 26°C, supplemented with 5 mM CaCl2 and 1 mM isopropyl-β-d-thiogalactopyranoside (IPTG), and propagated at 37°C for 3 h. Bacteria were sedimented at 8,500 × g for 7 min. Supernatant was filtered through a 0.22-µm-pore membrane (Millipore). Proteins were precipitated with 60% ammonium sulfate and overnight incubation at 4°C. Protein precipitate was sedimented at 12,500 × g for 15 min, suspended in 16 ml of column buffer (150 mM NaCl, 50 mM Tris-HCl [pH 7.0]), dialyzed, and subjected to affinity chromatography using 2 ml of preequilibrated 50% (vol/vol) Strep-Tactin–Sepharose (IBA BioTAGnology). Bound proteins were eluted in four 1-ml fractions with 2.5 mM desthiobiotin in column buffer. Recombinant LcrVS228 (rLcrVS228) was purified from cell extracts of E. coli DH5α as previously described (13). For anti-GSH (ViroGen) immunoblots, LcrVS228 was separated by native PAGE. For Edman degradation, purified LcrVS228 was separated by SDS-PAGE, electrotransferred to polyvinylidene difluoride (PVDF) membrane, stained with Coomassie blue, excised, and subjected to Edman degradation on an ABI Procise 494 sequencer.
For GST-Sepharose purification, overnight Y. pestis cultures were diluted 1:20 into 60 ml of M9-Ca minimal medium, incubated at 26°C for 2 h, and then incubated at 37°C for 3 h to induce type III secretion. Bacteria were sedimented by centrifugation at 7,500 × g for 10 min, and 50 ml of supernatant was filtered (0.22-µm-pore membrane). Protein in the filtrate was concentrated in an Amicon Ultra-15 centrifugal device (molecular weight cutoff [MWCO], 10,000) by serial centrifugations at 3,000 × g for 10 min and then washed twice with 14 ml of GST-tag column buffer (140 mM NaCl, 40 mM phosphate buffer [pH 7.3]). After the second wash, concentrated sample was transferred to an Eppendorf tube containing 100 μl of preequilibrated 50% (vol/vol) GST-Sepharose (Pierce); the final reaction volume was brought to 1 ml by the addition of GST-tag column buffer. Following overnight incubation at 4°C on a rotating shaker, the sample was centrifuged at 5,000 × g for 5 min. The supernatant was discarded, and GST-Sepharose was washed with 1 ml of GST-tag column buffer. After four washes, GST-Sepharose was suspended in 60 μl of 2× reducing SDS-PAGE sample buffer to elute bound proteins. Samples were boiled at 100°C for 5 min, centrifuged at 15,000 × g for 5 min, and analyzed by SDS-PAGE and immunoblotting with LcrV-specific antisera.
To purify LcrVS228 from infected macrophages, J774.A1 cells were propagated to confluence in 225-cm2 tissue culture flasks with 40 ml Dulbecco’s modified Eagle’s medium (DMEM) supplemented with 10% fetal bovine serum and 1% GlutaMAX. Prior to infection, the growth media were exchanged with DMEM supplemented with 1 mM IPTG. Overnight Y. pestis plcrVS228 cultures were diluted 1:20 into 20 ml of HIB and grown at 26°C for 2 h. After 1 mM IPTG supplementation, cultures were propagated at 37°C for 1 h. Bacteria were added at a multiplicity of infection (MOI) of 10 to J774.A1 macrophages. After 3 h of infection at 37°C with 5% CO2, tissue culture media were decanted and retained for cytokine analysis; macrophages were suspended in 20 ml of column buffer (150 mM NaCl, 50 mM Tris-HCl [pH 7.0]). Macrophage samples were freeze-thawed twice at −80°C, lysed in a French press at 15,000 lb/in3, and centrifuged at 30,000 × g for 30 min. The supernatant was subjected to affinity chromatography using 2 ml of preequilibrated 50% (vol/vol) Strep-Tactin–Sepharose. Columns were washed twice with 15 ml of column buffer, and bound proteins were eluted in four 0.5-ml fractions with 5 mM desthiobiotin in column buffer. Eluate was analyzed by silver- and Coomassie-stained SDS-PAGE. Mass spectrometry of trypsin-digested peptides was used to identify proteins. Samples were also analyzed by immunoblotting with antibodies specific for LcrV, RPS3 (Abcam, Inc.), and actin (Sigma); where indicated, the intensities of immunoreactive signals were quantified by densitometry using ImageJ (version v1.49t). Using commercially available enzyme-linked immunosorbent assay (ELISA) kits (eBioscience), the concentrations of IL-1β and IL-18 in the tissue culture media overlying Y. pestis-infected J774.A1 macrophages were determined according to the manufacturer’s protocols.
Mass spectrometry.
Combined liquid chromatography-electrospray ionization mass spectrometry with fraction collection (LC-ESI-MS+) was used to analyze protein samples. Sample volumes—typically 400 to 1,000 μl, each containing 0.4 to 0.6 mg protein/ml in 50 mM Tris-HCl (pH 7.0)–150 mM NaCl buffer—were dried in a vacuum concentrator and redissolved in water (250 to 1,000 μl), and aliquots (typically 250 μl) were loaded onto a polymeric reverse-phase column (Agilent PLRP-S; 300-Å pore size, 5-μm particle size, 2.1 by 150 mm), equilibrated in solvent A (water-formic acid, 100/0.1 [vol/vol]), and eluted (100 μl/min) with a linearly increasing concentration of solvent B (acetonitrile-isopropanol-formic acid, 50/50/0.1 [vol/vol/vol]: min/% B, 0/5, 5/5, 45/90, 50/5, and 60/5). The column effluent was passed through a stream splitter, with a proportion (approximately 50%) directed to a fraction collector (1 min/fraction) and the remainder to an Ionspray source connected to a triple-quadrupole mass spectrometer (ABI Sciex API III+) scanning in the positive-ion MS mode from m/z 500 to 1,850 (step size, 0.3 Da; dwell, 1 ms; 4.82 s/scan; orifice, 90 V). Multiple injections of the same samples were collected into the same fraction collector tubes. For disulfide reduction, protein samples were treated with 6 M guanidine-HCl containing 300 mM dithiothreitol (DTT) for 60 min at room temperature prior to injection onto the liquid chromatograph. Data were collected using software supplied by the instrument’s manufacturer (Tune 2.5-FPU) and were interrogated using MacSpec (version 3.3) for molecular mass calculations from multiply charged ion clusters and BioMultiView (version 1.3.1) for display of the deconvoluted spectra. Protein and peptide molecular weight calculations from known amino acid sequences were made with ExPASy at http://www.expasy.org/proteomics using Compute Pi/MW. For trypsin digestion, proteins of interest were pooled in preweighed glass test tubes and taken to dryness in a vacuum concentrator. An estimation of the protein content of each dried sample was made from the increased mass of the tube after drying. Dried samples were dissolved in 50 mM ammonium bicarbonate, and aliquots (4.34 nmol) were treated with sequencing-grade trypsin (Promega [50 pmol]) in a total volume of 150 μl of 50 mM ammonium bicarbonate at 37°C for 15 h. Aliquots (2 to 10 µl) were injected onto a Phenomenex Kinetex C18 column (100-Å pore size, 1.7-µm particle size, 150 by 2.1 mm), equilibrated in solvent A, and eluted (100 μl/min) with a linearly increasing concentration of solvent B (min/% B, 0/3, 2.5/3, 62.5/80, 65/3, and 80/3). The column effluent was directed to an Agilent Jet Stream source connected to a hybrid quadrupole time-of-flight mass spectrometer (Agilent 6550 iFunnel QTOF) scanning in the positive-ion data-dependent mode (m/z 200 to 2,500 for MS and 100 to 2,000 for tandem MS [MS/MS]; 4 spectra/s; MS/MS on multiply charged precursors of intensity >/1,000 counts excluded after one cycle; fragmentor, 380 V; collision energy automatically adjusted by instrument manufacturer-supplied software). Data were interrogated using MassHunter software. To reduce disulfide bonds, trypsin-digested samples were treated with 143 mM DTT in 50 mM ammonium bicarbonate at 37°C for 60 min. For the prediction of peptide fragmentation patterns (displays of b and y ions) from a known amino acid sequence, the MS-Product subroutine at Protein Prospector was used (http://prospector.ucsf.edu).
For MALDI-TOF MS analysis, purified LcrVS228 was concentrated in HPLC-grade H2O. Samples, either treated with DTT or left untreated, were spotted undiluted with sinapinic acid onto a MALDI plate and subjected to matrix-assisted laser desorption ionization–time of flight mass spectrometry (MALDI-TOF MS) using an Autoflex Speed Bruker MALDI instrument in linear mode (10- to 60-kDa range), with myoglobin as a calibration standard (2,000 shots/s at 95% intensity). Integrated data processing software (Bruker) was used to determine the molecular weight of each sample.
Type III secretion assays.
Assays for Y. pestis type III secretion of Yops into the culture medium or injection into HeLa cells, as well as measurements for F1 assembly, were performed as previously described (16, 19). For type III secretion assays, the intensities of immunoreactive signals were quantified by densitometry and analyzed with ImageJ. For murine J774.A1 macrophage infection experiments, 105 cells were seeded on the day prior to infection in 24-well tissue culture dishes in DMEM supplemented with 10% fetal bovine serum (FBS) and 1% GlutaMAX. Prior to infection, growth media were exchanged for DMEM. Overnight Y. pestis cultures were diluted 1:20 into 4 ml of HIB, propagated at 26°C for 2 h and then at 37°C for 1 h, added at an MOI of 5 to the J774.A1 cells, and incubated at 37°C with 5% CO2. Macrophages were washed once with phosphate-buffered saline (PBS) and stained with 2 µg/ml propidium iodide (Sigma) and 15 µg/ml Hoechst 33342 (Life Technologies, Inc.) for 10 min at room temperature, washed twice in PBS, fixed with 3.7% formaldehyde for 10 min, washed once with PBS, and then visualized by fluorescence microscopy using an Olympus IX81 inverted microscope. Infections were performed in triplicate, and the total numbers of live and dead macrophages were enumerated for three randomly selected fields of view.
To measure Y. pestis type III injection into primary neutrophils, Na2EDTA-anticoagulated venous blood from healthy human volunteers was layered 1:1 (vol/vol) onto PolymorphPrep and centrifuged at 500 × g for 35 min at 20°C. Neutrophils were removed, mixed 1:1 (vol/vol) with 0.5 × Hanks’ balanced saline solution (HBSS), and centrifuged at 350 × g for 10 min. Sedimented neutrophils were suspended in 10 ml HBSS, centrifuged at 350 × g for 10 min, and suspended in 2 ml of red blood cell lysis buffer (Roche). Samples were centrifuged at 250 × g for 5 min, and neutrophils were washed in 10 ml HBSS and suspended in 2 ml RPMI 1640 (Cellgro 10-040-CV) supplemented with 2% human serum albumin. Neutrophil viability (>95%) and purity (>97%) were determined by Trypan blue exclusion and Wright/Giemsa staining, respectively, with at least 400 cells counted per assay. Overnight Y. pestis cultures were diluted 1:40 into fresh HIB supplemented with 20 µg/ml chloramphenicol, incubated for 1.5 h at 26°C to reach the mid-exponential phase, and then incubated for 1.5 h at 37°C. Human neutrophils were suspended in Eppendorf tubes at a density of 5.5 × 105 cells in 500 µl of growth medium (RPMI 1640 supplemented with 2% human serum albumin [HSA]). Neutrophils were infected for 3 h (37°C, 5% CO2) at an MOI of 10 with Y. pestis strains expressing either YopM-Bla (pMM83) or, as a negative control, GST-Bla (pMM91) in a final volume of 600 µl growth medium. At the conclusion of the infection, polymorphonuclear leukocytes (PMNs) were sedimented by centrifugation at 1,500 × g for 3 min and suspended in 100 µl of growth medium supplemented with 50 µg/ml kanamycin to abrogate Y. pestis growth and type III injection. Neutrophils were stained with 1× CFF2-AM (Invitrogen) for 1 h at room temperature in the dark. Cells were collected by centrifugation at 1,500 × g for 3 min, washed once with 500 µl HBSS, and suspended in 500 µl of HBSS Flow (1× HBSS, 0.5 mM EDTA, 25 mM HEPES, 2% bovine serum albumin [BSA] [pH 7.4]). To discriminate between live and dead cells, propidium iodide (PI) was added to each sample at a final concentration of 0.5 µg/ml immediately prior to fluorescence-activated cell sorter (FACS) analysis. A BD FACSCanto flow cytometer was used to analyze at least 10,000 cells per sample, and data were analyzed using FlowJo (v10.0.7) and GraphPad Prism 6. Samples were first gated with the forward and side scatter for the population of singlet PMNs and subsequently gated for live cells by negative PI selection. PI-negative cells were then analyzed for blue fluorescence indicative of Y. pestis type III injection of YopM-Bla. Uninfected neutrophils were used to determine the background level of blue fluorescence.
Animal experiments.
BALB/c mice (n = 20) and Brown Norway rats (n = 20) were purchased from Charles River Laboratories, Inc. (6- to 8-week old females), and infected by subcutaneous injection with 100 µl PBS with Y. pestis strain CO92, TD1, or DE1 at a dose of 20 CFU (mice) or 500 CFU (rats), as previously described (44). At 72 h postchallenge in rats, or when animals (mice and rats) were deemed moribund (laterally recumbent and lethargic with rapid respiration), the animals were euthanized by compressed CO2 inhalation. At day 14 postinfection, Brown Norway rats that survived the initial challenge were euthanized as detailed above. Cardiac puncture was performed to obtain sera for analysis of IgG antibody titers. Draining lymph nodes and spleens were removed during necropsy and analyzed for bacterial load by CFU enumeration. Antibody titers were determined by ELISA as previously described (39).
HPLC analysis of thiol-mBBr derivatives.
Y. pestis strains were propagated overnight at 26°C in TMH medium, washed once, subcultured into 4 ml of fresh TMH medium at an initial optical density at 600 nm (OD600) of 0.5, and then grown for 5 h at 26°C to reach stationary phase. After transfer of 1 ml of stationary-phase culture to a preweighed Eppendorf tube, Y. pestis cells (~200 mg) were sedimented by centrifugation at 7,500 × g for 5 min and washed once with 1 ml of 1× PBS. For acid extraction of nonprotein thiols, washed bacterial cells were suspended in 1 ml of extraction buffer (6.3 mM DTPA [diethylenetriaminepentaacetic acid], 0.1% [vol/vol] trifluoroacetic acid [TFA]) and subjected to three rounds of freeze-thawing. Cellular debris was sedimented by centrifugation at 15,000 × g for 10 min. The supernatant was stored at −80°C, and the pellet was vacuum-dried at 30°C. The dry weight of the cell pellet was used to normalize the abundance of low-molecular-weight (LMW) thiols present in the corresponding supernatant fraction. A similar approach was used to analyze LMW thiol abundance in Y. pestis growth media (LB broth and TMH medium). Specifically, 1 ml of extraction buffer was added to an Eppendorf tube containing 250 µl of growth medium, and the sample was subjected to three freeze-thaw cycles as described above. After the sample was centrifuged at 15,000 × g for 10 min to pellet any insoluble material, the supernatant fraction was immediately collected, transferred to another Eppendorf tube, and stored at −80°C. For monobromobimane (mBBr) derivatization, 615 μl of HEPPS {3-[4-(2-hydroxyethyl)piperazinyl]propanesulfonic acid} buffer (200 mM HEPPS, 6.3 mM DTPA [pH 8.2]) was mixed with 25 μl of 20 mM TCEP, a nonthiol disulfide reductant. To this mixture, 250 μl of a thiol standard mixture or sample extract was added, followed by the addition of 10 μl of 0.5 mM N-acetyl cysteine, which served as an internal control. After preincubation of this reaction mixture in a heat block at 45°C for 10 min, derivatization was carried out by adding 10 μl of 50 mM mBBR and incubating the samples in the dark in a heat block at 45°C for 30 min. The reaction was terminated by the addition of 100 μl of 1 M methanesulfonic acid, samples were passed through 0.45-μm-pore nylon syringe filters (Pall-Gelman Labs) and stored at −20°C. HPLC analysis of thiol-mBBr derivatives was performed over a 250- by 4.6-mm Thermo Scientific Hypersil Gold column with a 5-μm particle-size guard column (Thermo Scientific). The column temperature was maintained at 40°C, and the injection volume was 10 μl. Separation of LMW thiol-mBBr adducts was achieved by using a linear gradient in which the mobile phase was supplemented with 0.1% TFA. The gradient was derived from buffer A (water, 10% acetonitrile, 0.1% TFA) and buffer B (acetonitrile, 0.1% TFA), with a continuous flow rate of 1 ml per min and the following parameters: 0 to 5 min, 0% buffer B; 5 to 16.2 min, linear gradient from 0 to 10.6% buffer B; 16.2 to 29.8 min, linear gradient from 10.6 to 21.1% buffer B; 29.9 to 39.9 min, 100% buffer B; 40 to 45 min, 0% buffer B. The elution profile was monitored by fluorescence, using an excitation wavelength of 394 nm and an emission wavelength of 490 nm.
Y. pestis survival in vertebrate blood and serum.
Y. pestis strains were propagated overnight in 4 ml LB broth at 26°C. After 0.5 ml of Y. pestis overnight culture was centrifuged at 7,500 × g for 5 min, sedimented bacteria were washed with 1 ml of 1× PBS and suspended in 1 ml of 1× PBS. After dilution of the bacterial suspension at 1:20 in 1× PBS, its OD600 was measured in order to calculate the volume required to inoculate 105 CFU of the bacterial suspension into 4 ml of sheep blood or serum (Hemostat Laboratories). Cultures were incubated for 18 h at 26 or 37°C. To enumerate the fold change in viable Y. pestis cells over 18 h of growth, CFU counts were determined both pre- and postincubation by serially diluting sheep blood or sheep serum cultures and plating on LB agar.
Statistics.
Statistical analysis was performed using Prism 6 (GraphPad Software, Inc.). For in vitro experiments, the two-tailed unpaired Student’s t test was used to compare differences between two groups, and one-way analysis of variance (ANOVA) with Tukey’s posttest was used to compare differences between more than two groups. For in vivo experiments, differences between two groups were analyzed using either the Mann-Whitney U test (CFU) or the two-tailed unpaired Student’s t test (serum IgG titers). Survival analysis of Y. pestis-infected animals was performed using the Gehan-Breslow-Wilcoxon test. A P value of <0.05 was determined to be statistically significant.
ACKNOWLEDGMENTS
We thank Owen Demke for experimental assistance and members of our laboratories for critical comments and discussion.
This project has been supported by funds from the National Institute of Allergy and Infectious Diseases, National Institutes of Health, Department of Health and Human Services, under awards U19 AI107792, RO1AI042797, and S10RR023718.
Footnotes
Citation Mitchell A, Tam C, Elli D, Charlton T, Osei-Owusu P, Fazlollahi F, Faull KF, Schneewind O. 2017. Glutathionylation of Yersinia pestis LcrV and its effects on plague pathogenesis. mBio 8:e00646-17. https://doi.org/10.1128/mBio.00646-17.
REFERENCES
- 1.Masip L, Veeravalli K, Georgiou G. 2006. The many faces of glutathione in bacteria. Antioxid Redox Signal 8:753–762. doi: 10.1089/ars.2006.8.753. [DOI] [PubMed] [Google Scholar]
- 2.Loi VV, Rossius M, Antelmann H. 2015. Redox regulation by reversible protein S-thiolation in bacteria. Front Microbiol 6:187. doi: 10.3389/fmicb.2015.00187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dalle-Donne I, Rossi R, Colombo G, Giustarini D, Milzani A. 2009. Protein S-glutathionylation: a regulatory device from bacteria to humans. Trends Biochem Sci 34:85–96. doi: 10.1016/j.tibs.2008.11.002. [DOI] [PubMed] [Google Scholar]
- 4.Reniere ML, Whiteley AT, Hamilton KL, John SM, Lauer P, Brennan RG, Portnoy DA. 2015. Glutathione activates virulence gene expression of an intracellular pathogen. Nature 517:170–173. doi: 10.1038/nature14029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Potter AJ, Trappetti C, Paton JC. 2012. Streptococcus pneumoniae uses glutathione to defend against oxidative stress and metal ion toxicity. J Bacteriol 194:6248–6254. doi: 10.1128/JB.01393-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Song M, Husain M, Jones-Carson J, Liu L, Henard CA, Vázquez-Torres A. 2013. Low-molecular-weight thiol-dependent antioxidant and antinitrosative defenses in Salmonella pathogenesis. Mol Microbiol 87:609–622. doi: 10.1111/mmi.12119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Slack P. 1989. The black death past and present. 2. Some historical problems. Trans R Soc Trop Med Hyg 83:461–463. doi: 10.1016/0035-9203(89)90247-2. [DOI] [PubMed] [Google Scholar]
- 8.Marketon MM, DePaolo RW, DeBord KL, Jabri B, Schneewind O. 2005. Plague bacteria target immune cells during infection. Science 309:1739–1741. doi: 10.1126/science.1114580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mueller CA, Broz P, Müller SA, Ringler P, Erne-Brand F, Sorg I, Kuhn M, Engel A, Cornelis GR. 2005. The V-antigen of Yersinia forms a distinct structure at the tip of injectisome needles. Science 310:674–676. doi: 10.1126/science.1118476. [DOI] [PubMed] [Google Scholar]
- 10.Burrows TW. 1956. An antigen determining virulence in Pasteurella pestis. Nature 177:426–427. doi: 10.1038/177426b0. [DOI] [PubMed] [Google Scholar]
- 11.Perry RD, Harmon PA, Bowmer WS, Straley SC. 1986. A low-Ca2+ response operon encodes the V antigen of Yersinia pestis. Infect Immun 54:428–434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lee VT, Tam C, Schneewind O. 2000. LcrV, a substrate for Yersinia enterocolitica type III secretion, is required for toxin targeting into the cytosol of HeLa cells. J Biol Chem 275:36869–36875. doi: 10.1074/jbc.M002467200. [DOI] [PubMed] [Google Scholar]
- 13.Ligtenberg KG, Miller NC, Mitchell A, Plano GV, Schneewind O. 2013. LcrV mutants that abolish Yersinia type III injectisome function. J Bacteriol 195:777–787. doi: 10.1128/JB.02021-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Brubaker RR. 1969. Mutation rate to nonpigmentation in Pasteurella pestis. J Bacteriol 98:1404–1406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gao XH, Bedhomme M, Veyel D, Zaffagnini M, Lemaire SD. 2009. Methods for analysis of protein glutathionylation and their application to photosynthetic organisms. Mol Plant 2:218–235. doi: 10.1093/mp/ssn072. [DOI] [PubMed] [Google Scholar]
- 16.Miller NC, Quenee LE, Elli D, Ciletti NA, Schneewind O. 2012. Polymorphisms in the lcrV gene of Yersinia enterocolitica and their effect on plague protective immunity. Infect Immun 80:1572–1582. doi: 10.1128/IAI.05637-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pechous RD, Sivaraman V, Price PA, Stasulli NM, Goldman WE. 2013. Early host cell targets of Yersinia pestis during primary pneumonic plague. PLoS Pathog 9:e1003679. doi: 10.1371/journal.ppat.1003679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Doll JM, Zeitz PS, Ettestad P, Bucholtz AL, Davis T, Gage K. 1994. Cat-transmitted fatal pneumonic plague in a person who traveled from Colorado to Arizona. Am J Trop Med Hyg 51:109–114. [DOI] [PubMed] [Google Scholar]
- 19.Quenee LE, Cornelius CA, Ciletti NA, Elli D, Schneewind O. 2008. Yersinia pestis caf1 variants and the limits of plague vaccine protection. Infect Immun 76:2025–2036. doi: 10.1128/IAI.00105-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chen TH, Meyer KF. 1974. Susceptibility and antibody response of Rattus species to experimental plague. J Infect Dis 129:S62–S71. doi: 10.1093/infdis/129.Supplement_1.S62. [DOI] [PubMed] [Google Scholar]
- 21.Achtman M, Zurth K, Morelli G, Torrea G, Guiyoule A, Carniel E. 1999. Yersinia pestis, the cause of plague, is a recently emerged clone of Yersinia pseudotuberculosis. Proc Natl Acad Sci U S A 96:14043–14048. doi: 10.1073/pnas.96.24.14043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bos KI, Stevens P, Nieselt K, Poinar HN, Dewitte SN, Krause J. 2012. Yersinia pestis: new evidence for an old infection. PLoS One 7:e49803. doi: 10.1371/journal.pone.0049803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Morelli G, Song Y, Mazzoni CJ, Eppinger M, Roumagnac P, Wagner DM, Feldkamp M, Kusecek B, Vogler AJ, Li Y, Cui Y, Thomson NR, Jombart T, Leblois R, Lichtner P, Rahalison L, Petersen JM, Balloux F, Keim P, Wirth T, Ravel J, Yang R, Carniel E, Achtman M. 2010. Yersinia pestis genome sequencing identifies patterns of global phylogenetic diversity. Nat Genet 42:1140–1143. doi: 10.1038/ng.705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhou D, Tong Z, Song Y, Han Y, Pei D, Pang X, Zhai J, Li M, Cui B, Qi Z, Jin L, Dai R, Du Z, Wang J, Guo Z, Wang J, Huang P, Yang R. 2004. Genetics of metabolic variations between Yersinia pestis biovars and the proposal of a new biovar, microtus. J Bacteriol 186:5147–5152. doi: 10.1128/JB.186.15.5147-5152.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chain PS, Hu P, Malfatti SA, Radnedge L, Larimer F, Vergez LM, Worsham P, Chu MC, Andersen GL. 2006. Complete genome sequence of Yersinia pestis strains Antiqua and Nepal516: evidence of gene reduction in an emerging pathogen. J Bacteriol 188:4453–4463. doi: 10.1128/JB.00124-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Anisimov AP, Dentovskaya SV, Panfertsev EA, Svetoch TE, Kopylov PK, Segelke BW, Zemla A, Telepnev MV, Motin VL. 2010. Amino acid and structural variability of Yersinia pestis LcrV protein. Infect Genet Evol 10:137–145. doi: 10.1016/j.meegid.2009.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mukherjee S, Keitany G, Li Y, Wang Y, Ball HL, Goldsmith EJ, Orth K. 2006. Yersinia YopJ acetylates and inhibits kinase activation by blocking phosphorylation. Science 312:1211–1214. doi: 10.1126/science.1126867. [DOI] [PubMed] [Google Scholar]
- 28.Zheng Y, Lilo S, Brodsky IE, Zhang Y, Medzhitov R, Marcu KB, Bliska JB. 2011. A Yersinia effector with enhanced inhibitory activity on the NF-κB pathway activates the NLRP3/ASC/caspase-1 inflammasome in macrophages. PLoS Pathog 7:e1002026. doi: 10.1371/journal.ppat.1002026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lemaître N, Sebbane F, Long D, Hinnebusch BJ. 2006. Yersinia pestis YopJ suppresses tumor necrosis factor alpha induction and contributes to apoptosis of immune cells in the lymph node but is not required for virulence in a rat model of bubonic plague. Infect Immun 74:5126–5131. doi: 10.1128/IAI.00219-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gao X, Hardwidge PR. 2011. Ribosomal protein S3: a multifunctional target of attaching/effacing bacterial pathogens. Front Microbiol 2:137. doi: 10.3389/fmicb.2011.00137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hodgson A, Wier EM, Fu K, Sun X, Yu H, Zheng W, Sham HP, Johnson K, Bailey S, Vallance BA, Wan F. 2015. Metalloprotease NleC suppresses host NF-kappaB/inflammatory responses by cleaving p65 and interfering with the p65/RPS3 interaction. PLoS Pathog 11:e1004705. doi: 10.1371/journal.ppat.1004705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wan F, Weaver A, Gao X, Bern M, Hardwidge PR, Lenardo MJ. 2011. IKKbeta phosphorylation regulates RPS3 nuclear translocation and NF-kappaB function during infection with Escherichia coli strain O157:H7. Nat Immunol 12:335–343. doi: 10.1038/ni.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.LaRock CN, Cookson BT. 2012. The Yersinia virulence effector YopM binds caspase-1 to arrest inflammasome assembly and processing. Cell Host Microbe 12:799–805. doi: 10.1016/j.chom.2012.10.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hopkins FG. 1921. On an autoxidisable constituent of the cell. Biochem J 15:286–305. doi: 10.1042/bj0150286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Quastel JH, Stewart CP, Tunnicliffe HE. 1923. On glutathione. IV. Constitution. Biochem J 17:586–592. doi: 10.1042/bj0170586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Veeravalli K, Boyd D, Iverson BL, Beckwith J, Georgiou G. 2011. Laboratory evolution of glutathione biosynthesis reveals natural compensatory pathways. Nat Chem Biol 7:101–105. doi: 10.1038/nchembio.499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rall TW, Lehninger AL. 1952. Glutathione reductase of animal tissues. J Biol Chem 194:119–130. [PubMed] [Google Scholar]
- 38.Sebbane F, Gardner D, Long D, Gowen BB, Hinnebusch BJ. 2005. Kinetics of disease progression and host response in a rat model of bubonic plague. Am J Pathol 166:1427–1439. doi: 10.1016/S0002-9440(10)62360-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Overheim KA, Depaolo RW, Debord KL, Morrin EM, Anderson DM, Green NM, Brubaker RR, Jabri B, Schneewind O. 2005. LcrV plague vaccine with altered immunomodulatory properties. Infect Immun 73:5152–5159. doi: 10.1128/IAI.73.8.5152-5159.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hanahan D. 1983. Studies on transformation of Escherichia coli with plasmids. J Mol Biol 166:557–580. doi: 10.1016/S0022-2836(83)80284-8. [DOI] [PubMed] [Google Scholar]
- 41.de Lorenzo V, Eltis L, Kessler B, Timmis KN. 1993. Analysis of Pseudomonas gene products using lacIq/Ptrp-lac plasmids and transposons that confer conditional phenotypes. Gene 123:17–24. doi: 10.1016/0378-1119(93)90533-9. [DOI] [PubMed] [Google Scholar]
- 42.Cheng LW, Anderson DM, Schneewind O. 1997. Two independent type III secretion mechanisms for YopE in Yersinia enterocolitica. Mol Microbiol 24:757–765. doi: 10.1046/j.1365-2958.1997.3831750.x. [DOI] [PubMed] [Google Scholar]
- 43.Donnenberg MS, Kaper JB. 1991. Construction of an eae deletion mutant of enteropathogenic Escherichia coli by using a positive-selection suicide vector. Infect Immun 59:4310–4317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Quenee LE, Ciletti NA, Elli D, Hermanas TM, Schneewind O. 2011. Prevention of pneumonic plague in mice, rats, guinea pigs and non-human primates with clinical grade rV10, rV10-2 or F1-V vaccines. Vaccine 29:6572–6583. doi: 10.1016/j.vaccine.2011.06.119. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Mass determination and Edman sequencing of LcrVS228. (A and B) Molecular mass spectra of (A) rLcrVS228 purified from cell extracts of E. coli DH5α(pKG48) or (B) LcrVS228 purified from culture supernatants of Y. pestis KLD29 ΔlcrV(pKG48) were reconstructed from the multiply charged ions recorded during combined liquid chromatography-electrospray ionization mass spectrometry (LC-ESI-MS). (A) The representative molecular mass spectrum of E. coli rLcrVS228 reveals a predominate isoform with a measured mass of 38,284.9 ± 1.4 Da, which corresponds to the full-length LcrVS228 protein, and a second isoform with measured mass of 38,152.8 ± 1.5 Da, which corresponds to the LcrVS228 protein lacking the initiator methionine residue. Data are means ± SEM (n = 9). (B) A representative molecular mass spectrum of Y. pestis LcrVS228 reveals a single predominant isoform with a measured mass of 38,594.4 ± 2.3 Da, which is 314.2 Da heavier than the calculated mass for full-length LcrVS228. Data are means ± SEM (n = 6). (C) LcrVS228 was purified from Y. pestis supernatants and subjected to Edman sequencing; the preponderant N-terminal amino acid released for each cycle (and its picomole abundance) is listed. Download FIG S1, TIF file, 5.1 MB (5.2MB, tif) .
Copyright © 2017 Mitchell et al.
This content is distributed under the terms of the Creative Commons Attribution 4.0 International license.
Summary of mass spectrometry analysis of tryptic peptides from Y. pestis LcrVS228 and E. coli rLcrVS228. Download TABLE S1, DOCX file, 0.1 MB (19.2KB, docx) .
Copyright © 2017 Mitchell et al.
This content is distributed under the terms of the Creative Commons Attribution 4.0 International license.
Tandem mass spectrometry of the 1,985.79-Da LcrVS228 peptide. Download TABLE S2, DOCX file, 0.1 MB (19.1KB, docx) .
Copyright © 2017 Mitchell et al.
This content is distributed under the terms of the Creative Commons Attribution 4.0 International license.
The codon substitution Cys273Ala, which precludes LcrV glutathionylation, does not affect Y. pestis type III secretion of Yop effectors. (A) Densitometric quantification of LcrV and YopE secreted by Y. pestis KIM D27 (Δpgm lcrV), KLD29 (Δpgm ΔlcrV), and AM6 (Δpgm lcrVC273A) following growth at 37°C in M9-Ca minimal medium in the absence of exogenous calcium ions. The immunoreactive signal of each secreted protein (S) was normalized to its total abundance in the medium and pellet (S + P); the ratio of secreted protein to total protein, (S)/(S + P) is presented as a percent average. ND, no immunoreactive signal detected. (B) Compared to uninfected HeLa cells, infection by Y. pestis KIM D27 or AM6 causes actin cable rearrangements and cytotoxicity (cell rounding) as detected by differential interference contrast (DIC) or fluorescence microscopy of rhodamine-phalloidin-stained cells. (C and D) Y. pestis CO92 pgm+ lcrV, LQ1 pgm+ ΔlcrV, and TD1 pgm+ lcrVC273A were induced for type III secretion by growth at 37°C in M9-Ca minimal medium with chelated calcium ions; secreted proteins (S) were separated from intact bacteria (P) by centrifugation. (C) Representative immunoblot analysis was performed by probing fractions with antibodies specific for type III secretion substrates (LcrV and YopE), the secreted F1 pilus subunit (F1), and a cytoplasmic fractionation control (RpoA). (D) The percentage of secretion of LcrV and YopE was determined by densitometry. ND, no immunoreactive signal detected. (E) LcrV secreted by the indicated Y. pestis strains was assayed for glutathionylation by subjecting the culture supernatant to GST-Sepharose affinity chromatography. The load (L) and eluate (E) fractions were analyzed by immunoblotting with anti-LcrV. All data are means ± SEM (n = 3). ns, not significant by two-tailed unpaired Student’s t test. Download FIG S2, TIF file, 22.3 MB (22.8MB, tif) .
Copyright © 2017 Mitchell et al.
This content is distributed under the terms of the Creative Commons Attribution 4.0 International license.
Kinetics of disease progression and host adaptive immune responses in bubonic plague-infected rodents. (A) BALB/c mice or (B to F) Brown Norway rats were infected by subcutaneous injection into the left inguinal fold with 20 CFU or 500 CFU, respectively, of Y. pestis CO92 pgm+ lcrV or Y. pestis TD1 pgm+ lcrVC273A. (A) Bacterial load in the regional lymph node and spleen of moribund BALB/c mice (n = 5) that were euthanized between 4 and 7 days postchallenge after exhibiting the symptoms of terminal illness. (B) Cohorts of Brown Norway rats (n = 5) were euthanized 72 h postchallenge to analyze the kinetics of bacterial replication in the regional lymph node as well as the kinetics of bacterial dissemination to the spleen. (C) Moribund rats (n = 5) that were euthanized between 4 and 7 days postchallenge were analyzed for disease progression by assessing the bacterial burden in the regional lymph node and spleen. (D to F) Bubonic plague-infected Brown Norway rats that survived for 14 days postchallenge were euthanized and necropsied. (D) Bacterial loads in the regional lymph node and spleen. (Note that since only two rats survived Y. pestis CO92 infection, necropsies were performed on two survivors—selected at random—of Y. pestis TD1 infection.) For rats surviving Y. pestis infection, serum IgG antibody titers for (E) LcrV or (F) capsular fraction F1 were quantified by ELISA. In panels A to D, the dotted lines represent the limit of detection, and red lines indicate geometric means. Statistical analysis was performed using the Mann-Whitney U test. In panels E and F, red lines indicate arithmetic means. Statistical analysis was performed using the two-tailed unpaired Student’s t test. All data are representative of two independent experiments. Download FIG S3, TIF file, 27.9 MB (28.5MB, tif) .
Copyright © 2017 Mitchell et al.
This content is distributed under the terms of the Creative Commons Attribution 4.0 International license.
The codon substitution Cys273Ser abolishes Y. pestis posttranslational modification of LcrV and attenuates virulence in a mouse model of bubonic plague. (A) Y. pestis isolates and nucleotide sequences at codons 272 to 273 (nucleotides 814 to 819 of Y. pestis CO92 lcrV) that impact codon 273 (Cys or Ser). (B and C) Following growth at 37°C in M9-Ca minimal medium lacking calcium ions, cultures of Y. pestis KIM D27 Δpgm lcrV or AM15 Δpgm lcrVC273S were fractionated and analyzed for type III secretion. (B) Representative immunoblot analysis was performed by probing supernatant (S) and pellet (P) fractions with the indicated rabbit antibodies. (C) Percentages of secretion of YopE and LcrV were determined by densitometric quantification of immunoreactive signals. (D) Y. pestis culture supernatants were subjected to GST-Sepharose affinity chromatography. The load (L) and eluate (E) fractions were immunoblotted with LcrV-specific antisera to assay for the secretion of glutathionylated LcrV. (E) Y. pestis KLD29 ΔlcrV and E. coli DH5α strains expressing LcrVS228 C273S (pAM199) were propagated in LB broth at 37°C. LcrV was affinity purified from Y. pestis culture supernatants (LcrVS228 C273S) or E. coli lysates (rLcrVS228 C273S), visualized by Coomassie-stained SDS-PAGE, and analyzed by MALDI-TOF MS. The experimentally observed m/z of each LcrVS228 C273S preparation is indicated. (F and G) Following infection with Y. pestis KIM D27(pYopM-Bla), KLD29(pYopM-Bla), or AM15(pYopM-Bla), human neutrophils were stained with CCF2-AM and analyzed by flow cytometry for blue fluorescence indicative of type III effector (YopM-Bla)-mediated cleavage of CCF2-AM. (F) Representative histograms show the blue fluorescence traces of Y. pestis-infected neutrophils; the percentage of YopM-Bla-injected neutrophils (blue cells) is indicated above the gating scheme that was used to measure blue fluorescence above background. (G) Percentage of quantification of YopM-Bla-injected human neutrophils. (H and I) Y. pestis CO92 pgm+ lcrV and DE1 pgm+ lcrVC273S were evaluated for type III secretion following growth at 37°C in M9-Ca minimal medium in the absence of exogenous calcium ions. (H) Representative immunoblot analysis of supernatant (S) and pellet (P) fractions. (I) Percentages of secretion of LcrV and YopE were determined by densitometry. (J) Survival of cohorts of BALB/c mice (n = 15) infected by subcutaneous injection into the left inguinal fold with 20 CFU of Y. pestis CO92 or DE1. The figure presents pooled data that were gathered from two independent experiments. For WT versus lcrVC273S, P = 0.0351 by Gehan-Breslow-Wilcoxon test. In panels C, G, and I, data are means ± SEM (n = 3). ns, not significant by two-tailed unpaired Student’s t test. Download FIG S4, TIF file, 25.8 MB (26.4MB, tif) .
Copyright © 2017 Mitchell et al.
This content is distributed under the terms of the Creative Commons Attribution 4.0 International license.
yopJ is dispensable for lcrVC273A-mediated killing of Y. pestis-infected macrophages, and type III secretion is not impacted by loss of glutathione synethase (gshB). (A) An in-frame deletion of yopJ was introduced by allelic exchange with wild-type Y. pestis KIM D27 and its lcrVC273A variant, Y. pestis AM6, to generate Y. pestis AM27 lcrV ΔyopJ and Y. pestis AM29 lcrVC273A ΔyopJ, respectively. Murine J774.A1 macrophages were infected for 3 h with the indicated Y. pestis strains, and macrophage cell death was quantified by enumeratng propidium iodide (PI)-positive cells. (B) Partial HPLC chromatograms include a reaction blank that was used to identify peaks originating from the derivatization reaction in the absence of sample-derived thiols, a standard mixture containing 10 pmol of Cys, GSH, and γ-EC that was used to assign peak positions for the corresponding thiol-mBBr adducts on the basis of retention time, and sample runs for TMH medium and LB broth. (C and D) Densitometric quantification of LcrVS228 and YopE secreted by Y. pestis KLD29 ΔlcrV(pKG48) and AM43 ΔlcrV ΔgshB(pKG48) following growth in the presence (+Ca2+) or absence (−Ca2+) of calcium ions at 37°C in (C) LB broth or (D) TMH medium. The immunoreactive signal of each secreted protein (S) was normalized to its total abundance in the medium and pellet (S + P); the ratio of secreted protein to total protein, (S)/(S + P), is presented as a percent average. All data are means ± SEM (n = 3). ****, P < 0.0001, and ns, not significant, by two-tailed unpaired Student’s t test. Download FIG S5, TIF file, 30.9 MB (7.9MB, tif) .
Copyright © 2017 Mitchell et al.
This content is distributed under the terms of the Creative Commons Attribution 4.0 International license.
Peptide mass fingerprinting by LC-MS/MS identifies macrophage RPS3 as a ligand of translocated LcrV. Download TABLE S3, DOCX file, 0.1 MB (16.8KB, docx) .
Copyright © 2017 Mitchell et al.
This content is distributed under the terms of the Creative Commons Attribution 4.0 International license.
MALDI-TOF MS analysis of LcrVS228 and LcrVS228 C273S purified from Y. pestis supernatants or E. coli extracts. Download TABLE S4, DOCX file, 0.1 MB (16.7KB, docx) .
Copyright © 2017 Mitchell et al.
This content is distributed under the terms of the Creative Commons Attribution 4.0 International license.
Bacterial strains, plasmids, and primers used in this study. Download TABLE S5, DOCX file, 0.1 MB (102.7KB, docx) .
Copyright © 2017 Mitchell et al.
This content is distributed under the terms of the Creative Commons Attribution 4.0 International license.