Abstract
Context:
Stress is defined as an alteration of an organism's balance in response to a demand perceived from the environment. Diverse methods exist to evaluate physiological response. A noninvasive method is salivary measurement of cortisol and alpha-amylase. A growing body of evidence suggests that the regular practice of Yoga would be an effective treatment for stress.
Aims:
To determine the Kundalini Yoga (KY) effect, immediate and after 3 months of regular practice, on the perception of psychological stress and the salivary levels of cortisol and alpha-amylase activity.
Settings and Design:
To determine the psychological perceived stress, levels of cortisol and alpha-amylase activity in saliva, and compare between the participants to KY classes performed for 3 months and a group that does not practice any type of yoga.
Subjects and Methods:
The total sample consisted of 26 people between 18 and 45-year-old; 13 taking part in KY classes given at the Faculty of Dentistry, University of Chile and 13 controls. Salivary samples were collected, enzyme-linked immunosorbent assay was performed to quantify cortisol and kinetic reaction test was made to determine alpha-amylase activity. Perceived Stress Scale was applied at the beginning and at the end of the intervention.
Statistical Analysis Used:
Statistical analysis was applied using Stata v11.1 software. Shapiro–Wilk test was used to determine data distribution. The paired analysis was fulfilled by t-test or Wilcoxon signed-rank test. T-test or Mann–Whitney's test was applied to compare longitudinal data. A statistical significance was considered when P < 0.05.
Results:
KY practice had an immediate effect on salivary cortisol. The activity of alpha-amylase did not show significant changes. A significant decrease of perceived stress in the study group was found.
Conclusions:
KY practice shows an immediate effect on salivary cortisol levels and on perceived stress after 3 months of practice.
Keywords: Alpha-amylase, cortisol, Kundalini Yoga, saliva, stress, yoga
Introduction
Stress is defined as an alteration of an organism's homeostasis in response to a real or perceived demand from the environment. The stressors can be biological, environmental, social, emotional, or psychological, unleashing a response to restore the balance.[1,2,3]
The physiological response to stress is formed by two principal branches: autonomic nervous system (ANS) and the hypothalamic-pituitary-adrenal axis (HPA).[3] The sympathetic nervous system part of ANS responds immediately by adrenergic hormones. The HPA axis allows a late and supported over time response by secreting glucocorticoids as cortisol.[4]
Cortisol and adrenergic hormones have been defined as reliable indicators of the activity of the physiological systems of stress. Nevertheless, stress is a many-sided phenomenon that needs a multidimensional approach.[5,6,7]
Saliva has received great attention as a fluid that allows to the quantification of the presence of diverse markers such as immunoglobulin, cortisol,[2,8,9] and alpha-amylase[3,10,11,12,13] among others, in a noninvasive way.
To approach stress in an integrated way, its subjective component is also relevant. Every person reacts differently to stressors, resulting in different perceptions of stress. The characteristics of this response have an important relationship with individual, social, and cultural aspects, giving a particular aspect to the experience perceived by each individual.[14]
In 1983, Cohen et al.[15] developed the Perceived Stress Scale (PSS) to measure the degree, in which the persons evaluate the stressful situations in their daily life. The scale includes questions destined to evaluate the perception of stress during the last month.[16]
Nowadays, diverse forms of treatment for stress exist. Thousand-year-old technologies as yoga are gaining increasing attention as a holistic system that involves the physical body, the mind, and breathing to achieve balance.[2,17,18]
In this context, our investigation was carried out to determine if Kundalini Yoga (KY) regular practice could modify the perception of psychological stress and the salivary levels of cortisol and activity of alpha-amylase in beginners' practitioners of this discipline, in comparison to a control group.
Subjects and Methods
Kundalini Yoga
Kundalini comes from the word “kundal”; coiled energy; the creative potential of an individual. “Kundalini” literally means “the curl of the lock of hair of the beloved.” This poetic metaphor alludes to the flow of energy and consciousness that exists within each of us and enables us to merge with the universal self.
KY is a Raaj Yoga that creates vitality in the body, balance in the mind, and openness to the spirit and is the yoga of awareness, the science of potential exploration of the self within the self; its focus is on self-awareness and delivering an experience of your highest consciousness.
The primary objective is to awaken the full potential of human awareness in each individual, that is, recognize our awareness, refine that awareness, and expand that awareness to our unlimited self. Clear any inner duality, create the power to deeply listen, cultivate inner stillness, and prosper and deliver excellence in all that we do.
The focus of KY as taught by Yogi Bhajan is on one's personal experience and awareness through the practice of kriya and meditation including mantra chanting. We awaken the kundalini to be able to call upon the full potential of the nervous and glandular systems and to balance the subtle system of chakras and meridians within the body. “Kriya” is an orchestrated pattern of movements, sound, pranayam, mudras, concentration, and meditation that automatically guide the energies of the body and the mind to a specific result or change of consciousness. They can be simple short sequences or they may involve vigorous, even strenuous exercises, which challenge and strengthen the nervous and endocrine systems and test the will of the practitioner beyond the limitations of their ego.
In any KY class, anywhere in the world, you can expect it to include six major components: (1) Tuning-in with the Adi Mantra, (2) pranayam or warmup, (3) kriya, (4) relaxation, (5) meditation, and (6) close with the blessing song, “May the Long Time Sun Shine Upon You.” The typical class is 60–90 min: 5–10 min warmup, 30–45 min kriya, 5–15 min layout, 11–31 min of meditation. It is different than all the yogas in one way it is a science of a householder, it is not the science of a hermit.
Subjects
Previous approval from the Ethics Committee of the Faculty of Dentistry was obtained for our prospective controlled clinical study. Participants were volunteers from the north campus of University of Chile who attended KY regular classes at the Faculty of Dentistry for at least 3 months. The control group was recruited by public notices in the same campus to obtain a similar group. To protect the identity of the participants and to avoid biases, they were codified by correlative numbers. The studied group was initially 26 individuals. Nevertheless, the final size was reduced to 13 individuals for the following reasons: irregular attendance, participation to < 50% of the classes, and/or salivary samples lower than 1 ml. The initial size of the control group was 20 individuals that diminished to 13 because the salivary samples were lower than 1 ml of saliva or for lack of final sample. The final size of the sample was 13 individuals in each group (n = 13); 11 women and 2 men, average age 25.1 ± 3.9 in the study group and 10 women and 3 men, average age 23.9 ± 2.1 in the control group. Criteria used for selection were healthy individuals between 18 and 45-year-old. The study group had to be composed by beginners in KY practice, defining beginners as those who practice continually < 1 year and attend at least 50% of the total of 30 lessons. Control group did not practice any type of yoga. For both groups, a general anamnesis and clinical oral examination were made, excluding the individuals suffering from disorders of anxiety and/or stress diagnosed or under treatment of corticoids and individuals who presented infectious diseases such as caries, periodontal diseases, and mucositis. All participants signed an informed assent approved by the Ethics Committee of the Faculty of Dentistry. KY lessons were carried out twice a week between 12:30 and 14:00 h for 3 months by a teacher certified by the Kundalini Research Institute; classes were given as Yogi Bhajan teachings.[19]
Sampling
The samples from both groups were obtained in the same days and schedules. Participants were asked not to consume alcohol 12 h before, to brush their teeth 2 h before, and not to consume liquids and/or food within this period to avoid the pollution and/or alteration of the sample. They rinsed their mouth with drinkable water 10 min before collecting the sample. One milliliter of not stimulated saliva was collected using the Salivette device (Sarstedt, Germany).[20] For the study group, 4 samples were collected, at the beginning and at the end of the first and the last class to determine immediate and longitudinal effect. In the control group, two samples were collected at the beginning of the study and after 3 months.
Methods
Samples were processed immediately in the Periodontal Laboratory of the Faculty of Dentistry. The obtained samples were centrifuged at 1000 rpm for 3 min at 4°C and free ethylenediaminetetraacetic acid protease inhibitor cocktail was added and kept at −80°C. Determination of cortisol levels and alpha-amylase activity in the obtained samples was carried out in duplicate using commercial kits according to the indications of the manufacturer (Cortisol Salivary Immunoassay kit [ELISA/EIA], Salimetrics and Alpha-Amylase Salivary Assay Kit, Salimetric). Multimodal reader Synergy™ HTX was used for both tests.
The PSS Spanish version of 14 articles was applied. The total score of the PSS was obtained by inverting the score of the articles 4, 5, 6, 7, 9, 10, and 13 (in the following order 0 = 4, 1 = 3, 2 = 2, 3 = 1, and 4 = 0) and dividing equally this way 14 articles. The direct obtained score indicates that a major score corresponds to a higher level of perceived stress, being 4 the major level of stress and 0 the absence of stress.[15,16] Every psychological test was analyzed by an experienced psychologist (R.C.).
Statistical analysis was performed using GraphPad Prosm V 7 © 2017 GraphPad Software, Inc. Shapiro–Wilk test was used to determine data distribution. The analysis of pre- and post-intervention was fulfilled by t-test or Wilcoxon signed-rank test depending on the data distribution. T-test or Mann–Whitney's test were performed to compare the basal and longitudinal data between the study and control groups. A statistical significance was considered when P < 0.05 [Flow chart 1].
Flow Chart 1.
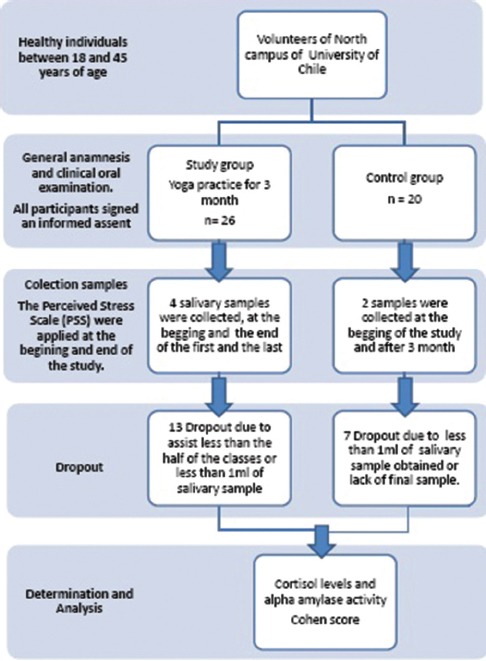
Study design
Results
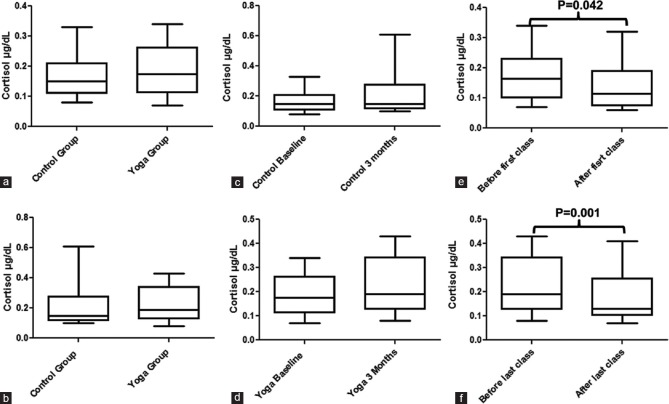
The basal value of salivary cortisol was 0.17 ± 0.08 μg/dL for the control group and 0.19 ± 0.08 μg/dL for the study group [Figure 1a]. The concentration post intervention was 0.23 ± 0.17 μg/dL in the control group and 0.24 ± 0.12 μg/dL for the study group [Figure 1b]. In both cases, we did not find statistically significant differences in the basal and postintervention values (P = 0.56 and 0.53 respectively) [Table 1].
Figure 1.
Effect of Kundalini Yoga practice for 3 months in salivary levels of cortisol. (a) Baseline levels of cortisol, (b) postintervention levels of cortisol, (c) longitudinal effect in control group, (d) longitudinal effect in yoga group, (e) baseline immediate effect (f) postintervention immediate effect
Table 1.
Summary table of results
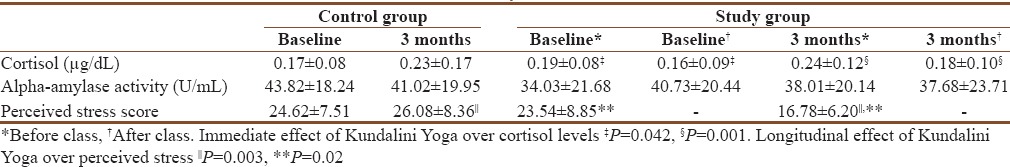
On the other hand, after 3 months of KY practice, there were no statistically significant differences in salivary cortisol levels with a P = 0.53 for the control group and 0.09 for the study group [Figure 1c and d respectively].
The immediate effect of KY was determined by cortisol levels before and after the first and the last class in the study group. At the beginning of the study, the values were 0.19 ± 0.08 μg/dL versus 0.16 ± 0.09 μg μg/dL and at the end of the study 0.24 ± 0.12 μg/dL versus 0.18 ± 0.10 μg/dL. In both cases, we observed a decrease of cortisol. The difference was statistically significant with a P = 0.042 and 0.001, respectively [Figure 1e and f, respectively].
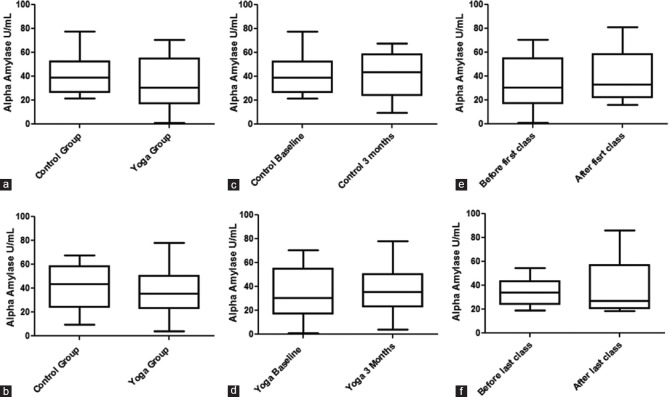
Alpha-amylase activity in the study group at the beginning was 34.03 ± 21.68 U/mL and after 3 months of yoga practice 38.01 ± 20.14 U/mL while in the control group, the values were 43.82 ± 18.24 U/mL versus 41.02 ± 19.95 U/mL. The groups did not present significant differences in their basal and postintervention values (P = 0.25 and P = 0.72, respectively) [Figure 2a and b, respectively].
Figure 2.
Effect of Kundalini Yoga practice for 3 months in salivary alpha amylase activity. (a) Baseline alpha amylase activity, (b) postintervention alpha amylase activity, (c) longitudinal effect in control group, (d) longitudinal effect in yoga group, (e) baseline immediate effect (f) postintervention immediate effect
Three months after the first salivary sample, we did not find significant differences in alpha-amylase activity in the study group (P = 0.37) and neither in the control group (P = 0.67) [Figure 2c and d, respectively].
The immediate effect was determined according to the activity before and after the first and last class. The values of the first class were basal 34.03 ± 21.68 U/mL and final 40.73 ± 20.44, while those of the last session were basal 38.01 ± 20.14 U/mL and final 37.68 ± 23.71U/mL. In both cases, before and after the first and last class, we did not observe an immediate effect of yoga practice on the activity of salivary alpha-amylase (P = 0.26 and P = 0.85, respectively) [Figure 2e and f respectively].
On the other hand, the analysis of perceived stress score obtained with t-test for independent samples demonstrated that the groups did not present differences in the basal measurement (P = 0.74), but there was a statistical significance after the intervention (P = 0.003) [Figure 3].
Figure 3.
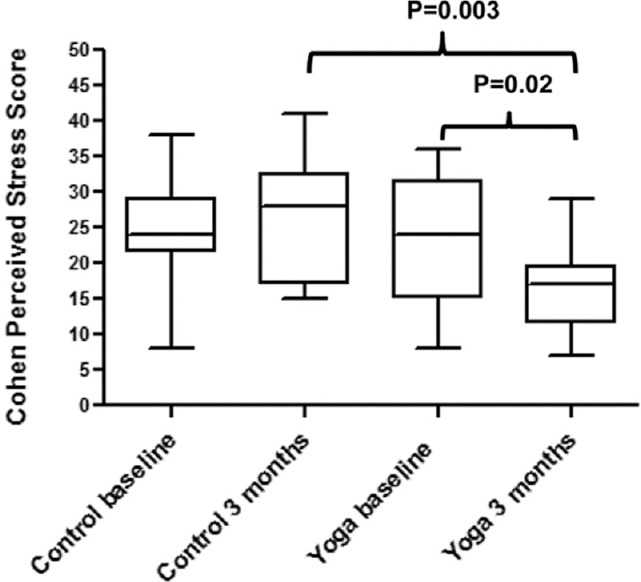
Effect of Kundalini Yoga practice for 3 months in perceived stress
Student's t-test for paired samples determined that level of stress perceived in the control group had a scanty variation between the first measurement (24.62 ± 7.51) and the second one (26.08 ± 8.36) with a P = 0.47 while the experimental group had a marked decrease of perceived stress after intervention (23.54 ± 8.85 vs. 16.78 ± 6.20). This was statistically significant with a P = 0.02. Therefore, the intervention had an important diminishing effect on perceived stress [Figure 3].
Discussion
This study evaluated the longitudinal and immediate effect of the KY in the salivary levels of cortisol and activity of alpha-amylase and its effect on perceived stress.
The salivary alpha-amylase levels are widely considered a marker of psychological stress and reflect the activity of sympathetic adrenal medullary system. On Duchemin's[21] study, mindfulness-based intervention levels of salivary α-amylase were significantly decreased between the 1st and 2nd assessments in the intervention group with no changes in the control group as well as on Sieverdes et al.[22] study were a small-to-moderate effect size was seen in the Hatha yoga group favoring a reduction of α-amylase, while α-amylase increased in the prehypertensive attention control group who attended to music or art class. Alpha-amylase activity did not show statistically significant differences between the group that practiced Hatha Yoga and the control group[22] as well as our study where no significant variations were found in any of the measurements.
Methodological weaknesses as sample size, eating behavior, quantity of yoga classes, and the duration of intervention could be improved in the future studies. It is important to consider that even though they were asked not to consume alcohol 12 h before, to brush their teeth 2 h before, and not to consume liquids and/or food within this period to avoid the pollution and/or alteration of the sample we cannot be sure of it, which could explain the large variation in the values of alpha-amylase, especially if they ate or drank before sampling.
For immediate changes on the salivary activity of alpha-amylase, we did not find significant differences as well as in a study carried out in 2011 with a test of social stress (trier social stress test). A possible explanation could be that changes in salivary markers such as the alpha-amylase might appear 2, 6, or 24 h later after the intervention.[23]
Psychological stress activates autonomic system, increasing the activity of alpha-amylase.[6,24] Chatterton described significant correlations between alpha-amylase, adrenaline, and noradrenaline after exercise. Furthermore, the activity of this enzyme in saliva is affected by physical exercise, having a direct relationship with the exercise intensity.[11,20,25] As for the psychological component, marked alterations in alpha-amylase levels were detected after applying stressors such as skydiving, academic tests, or stressful videos by different research groups[11,26,27] that could be an explanation for our results because our study finished in period of academic exams.
Unlike the previous evidence that shows a decrease in cortisol levels, longitudinally and immediately with the practice of yoga,[28] we did not find a statistical difference in the longitudinal measurement in the study group. This may be due to uncontrolled factors which could influence directly on the levels of cortisol, such as the use of oral contraceptives, physical exercise, and smoking.[29,30]
A study performed in 2004 found significant differences in salivary cortisol levels when comparing the immediate effect of African dance and Hatha yoga, describing a decrease of cortisol in the yoga group in comparison to the dance group. However, both disciplines showed lower values of perceived stress compared with the control group.[31]
Immediate effect of KY on salivary cortisol levels shows a statistically significant decrease in the first and in the last class as in Juster's study.[23] Although literature says that cortisol helps support stress as physiological response before constant stress stimulus contributing principally to the late response, there is an evidence that indicates that the peak of cortisol would be between 20 and 30 min after the stimulus, increasing immediately when homeostasis is altered.[29]
Although PSS is not validated in a Chilean population, it offers a brief and simple application, available in our native language and its shows internal consistency in the desirable range in different contexts and languages such as Spanish, English, and Japanese.[14,16,32,33]
Perceived stress diminished longitudinally in the study group as it has been observed in other investigations with KY practice.[34] Furthermore, in accordance to the available literature, perceived stress diminished in the control groups when complementary tools for the treatment of stress were applied.[35]
However, there is a discrepancy in our results. While perceived stress diminished longitudinally, salivary cortisol levels did not change significantly, probably due to the factors previously mentioned, especially that the study ended in period of academic exams. Evidence shows that subjects undergoing examinations increase their perceptions of stress;[36,37] therefore, the above-mentioned factors would apparently not affect the perception of stress.
In literature, there are described factors that might modify the concentrations of cortisol and activity of alpha-amylase in saliva, such as the age, sex, use of oral contraceptives, menstrual cycle,[30,38] cycles of dream, and consumption of caffeine[39] and nicotine.[40] These factors were not controlled or used as criteria of exclusion because our sample size was very limited. Due to the fact that the evidence is ambiguous with respect to the influence of age and gender in the salivary concentrations of stress markers,[41] the effects of oral contraceptives on cortisol levels[42,43] and the increase in cortisol secretion due to nicotine consumption,[40] it is suggested to approach these factors in the future studies.
Although different styles of yoga exist, there are different ways to achieve the same end, where variations might exist since they have different approaches.[44] Recent studies support the positive effect of yoga in the treatment of stress[45] though even more studies with a stricter exclusion criteria and longer periods of intervention are necessary.
Conclusions
This study presents an approximation where immediate and longitudinal perceived stress declined, which leads us to think that KY might be a useful tool in the complementary treatment of pathologies directly related to high levels of stress, such as cardiovascular diseases,[46] hypertension,[47,48] immune system disorders,[49] bruxism and periodontal disease,[50,51,52] insomnia, depression,[46,53] and also in diabetes[54,55] and chronic diseases in general.
Financial support and sponsorship
The study was supported by Project FIOUCH 13-012, Faculty of Dentistry, University of Chile.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Seyle H, editor. Stress without Distress. 1st ed. Philadelphia: Lippincott; 1974. [Google Scholar]
- 2.Ali N, Pruessner JC. The salivary alpha amylase over cortisol ratio as a marker to assess dysregulations of the stress systems. Physiol Behav. 2012;106:65–72. doi: 10.1016/j.physbeh.2011.10.003. [DOI] [PubMed] [Google Scholar]
- 3.Laurent HK, Powers SI, Granger DA. Refining the multisystem view of the stress response: Coordination among cortisol, alpha-amylase, and subjective stress in response to relationship conflict. Physiol Behav. 2013;119:52–60. doi: 10.1016/j.physbeh.2013.05.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chrousos GP, Kino T, Charmandari E. Evaluation of the hypothalamic-pituitary-adrenal axis function in childhood and adolescence. Neuroimmunomodulation. 2009;16:272–83. doi: 10.1159/000216185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Miller GE, Chen E, Zhou ES. If it goes up, must it come down? Chronic stress and the hypothalamic-pituitary-adrenocortical axis in humans. Psychol Bull. 2007;133:25–45. doi: 10.1037/0033-2909.133.1.25. [DOI] [PubMed] [Google Scholar]
- 6.Nater UM, La Marca R, Florin L, Moses A, Langhans W, Koller MM, et al. Stress-induced changes in human salivary alpha-amylase activity – Associations with adrenergic activity. Psychoneuroendocrinology. 2006;31:49–58. doi: 10.1016/j.psyneuen.2005.05.010. [DOI] [PubMed] [Google Scholar]
- 7.Charmandari E, Tsigos C, Chrousos G. Endocrinology of the stress response. Annu Rev Physiol. 2005;67:259–84. doi: 10.1146/annurev.physiol.67.040403.120816. [DOI] [PubMed] [Google Scholar]
- 8.Hellhammer DH, Wüst S, Kudielka BM. Salivary cortisol as a biomarker in stress research. Psychoneuroendocrinology. 2009;34:163–71. doi: 10.1016/j.psyneuen.2008.10.026. [DOI] [PubMed] [Google Scholar]
- 9.Maidana P, Bruno OD, Mesch V. A critical analysis of cortisol measurements: An update. Medicina (B Aires) 2013;73:579–84. [PubMed] [Google Scholar]
- 10.Al-Tarawneh SK, Border MB, Dibble CF, Bencharit S. Defining salivary biomarkers using mass spectrometry-based proteomics: A systematic review. OMICS. 2011;15:353–61. doi: 10.1089/omi.2010.0134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chatterton RT, Jr, Vogelsong KM, Lu YC, Ellman AB, Hudgens GA. Salivary alpha-amylase as a measure of endogenous adrenergic activity. Clin Physiol. 1996;16:433–48. doi: 10.1111/j.1475-097x.1996.tb00731.x. [DOI] [PubMed] [Google Scholar]
- 12.Chatterton RT, Jr, Vogelsong KM, Lu YC, Hudgens GA. Hormonal responses to psychological stress in men preparing for skydiving. J Clin Endocrinol Metab. 1997;82:2503–9. doi: 10.1210/jcem.82.8.4133. [DOI] [PubMed] [Google Scholar]
- 13.Skosnik PD, Chatterton RT, Jr, Swisher T, Park S. Modulation of attentional inhibition by norepinephrine and cortisol after psychological stress. Int J Psychophysiol. 2000;36:59–68. doi: 10.1016/s0167-8760(99)00100-2. [DOI] [PubMed] [Google Scholar]
- 14.Campo-Arias A, Bustos-Leiton GJ, Romero-Chaparro A. Internal consistency and dimensionality of perceived stress scale (PSS-10 and PSS-14) in a sample of university students from Bogotá, Colombia, Aquichán. 2009;9:271–80. [Google Scholar]
- 15.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385–96. [PubMed] [Google Scholar]
- 16.Remor E. Psychometric properties of a European Spanish version of the Perceived Stress Scale (PSS) Span J Psychol. 2006;9:86–93. doi: 10.1017/s1138741600006004. [DOI] [PubMed] [Google Scholar]
- 17.Sharma M. Yoga as an alternative and complementary approach for stress management: A systematic review. J Evid Based Complementary Altern Med. 2014;19:59–67. doi: 10.1177/2156587213503344. [DOI] [PubMed] [Google Scholar]
- 18.Wang F, Lee EK, Wu T, Benson H, Fricchione G, Wang W, et al. The effects of tai chi on depression, anxiety, and psychological well-being: A systematic review and meta-analysis. Int J Behav Med. 2014;21:605–17. doi: 10.1007/s12529-013-9351-9. [DOI] [PubMed] [Google Scholar]
- 19.Kundalini Research Institute (KRI) Santa Cruz. Second Edition. USA: 2006. Khalsa HS (Yogi Bhajan). The Acuarian Teacher (spanish version) [Google Scholar]
- 20.Rohleder N, Nater UM, Wolf JM, Ehlert U, Kirschbaum C. Psychosocial stress-induced activation of salivary alpha-amylase: An indicator of sympathetic activity? Ann N Y Acad Sci. 2004;1032:258–63. doi: 10.1196/annals.1314.033. [DOI] [PubMed] [Google Scholar]
- 21.Duchemin AM, Steinberg BA, Marks DR, Vanover K, Klatt M. A small randomized pilot study of a workplace mindfulness-based intervention for surgical intensive care unit personnel: Effects on salivary a-amylase levels. J Occup Environ Med. 2015;57:393–9. doi: 10.1097/JOM.0000000000000371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sieverdes JC, Mueller M, Gregoski MJ, Brunner-Jackson B, McQuade L, Matthews C, et al. Effects of hatha yoga on blood pressure, salivary a-amylase, and cortisol function among normotensive and prehypertensive youth. J Altern Complement Med. 2014;20:241–50. doi: 10.1089/acm.2013.0139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Juster RP, Sindi S, Marin MF, Perna A, Hashemi A, Pruessner JC, et al. A clinical allostatic load index is associated with burnout symptoms and hypocortisolemic profiles in healthy workers. Psychoneuroendocrinology. 2011;36:797–805. doi: 10.1016/j.psyneuen.2010.11.001. [DOI] [PubMed] [Google Scholar]
- 24.Nater UM, Rohleder N, Gaab J, Berger S, Jud A, Kirschbaum C, et al. Human salivary alpha-amylase reactivity in a psychosocial stress paradigm. Int J Psychophysiol. 2005;55:333–42. doi: 10.1016/j.ijpsycho.2004.09.009. [DOI] [PubMed] [Google Scholar]
- 25.Koibuchi E, Suzuki Y. Exercise upregulates salivary amylase in humans (Review) Exp Ther Med. 2014;7:773–7. doi: 10.3892/etm.2014.1497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bosch JA, Brand HS, Ligtenberg TJ, Bermond B, Hoogstraten J, Nieuw Amerongen AV. Psychological stress as a determinant of protein levels and salivary-induced aggregation of Streptococcus gordonii in human whole saliva. Psychosom Med. 1996;58:374–82. doi: 10.1097/00006842-199607000-00010. [DOI] [PubMed] [Google Scholar]
- 27.Takai N, Yamaguchi M, Aragaki T, Eto K, Uchihashi K, Nishikawa Y. Effect of psychological stress on the salivary cortisol and amylase levels in healthy young adults. Arch Oral Biol. 2004;49:963–8. doi: 10.1016/j.archoralbio.2004.06.007. [DOI] [PubMed] [Google Scholar]
- 28.Rocha KK, Ribeiro AM, Rocha KC, Sousa MB, Albuquerque FS, Ribeiro S, et al. Improvement in physiological and psychological parameters after 6 months of yoga practice. Conscious Cogn. 2012;21:843–50. doi: 10.1016/j.concog.2012.01.014. [DOI] [PubMed] [Google Scholar]
- 29.Kirschbaum C, Hellhammer DH, editors. Encyclopedia of Stress. 1st ed. San Diego: Academic Press; 2000. [Google Scholar]
- 30.Kozlov AI, Kozlova MA. Cortisol as a marker of stress. Fiziol Cheloveka. 2014;40:123–36. [PubMed] [Google Scholar]
- 31.West J, Otte C, Geher K, Johnson J, Mohr DC. Effects of Hatha yoga and African dance on perceived stress, affect, and salivary cortisol. Ann Behav Med. 2004;28:114–8. doi: 10.1207/s15324796abm2802_6. [DOI] [PubMed] [Google Scholar]
- 32.González-Ramírez MT, Rodríguez-Ayán MN, Hernández RL. The perceived stress scale (PSS): Normative data and factor structure for a large-scale sample in Mexico. Span J Psychol. 2013;16:E47. doi: 10.1017/sjp.2013.35. [DOI] [PubMed] [Google Scholar]
- 33.Mimura C, Griffiths P. A Japanese version of the perceived stress scale: Cross-cultural translation and equivalence assessment. BMC Psychiatry. 2008;8:85. doi: 10.1186/1471-244X-8-85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Granath J, Ingvarsson S, von Thiele U, Lundberg U. Stress management: A randomized study of cognitive behavioural therapy and yoga. Cogn Behav Ther. 2006;35:3–10. doi: 10.1080/16506070500401292. [DOI] [PubMed] [Google Scholar]
- 35.Michalsen A, Grossman P, Acil A, Langhorst J, Lüdtke R, Esch T, et al. Rapid stress reduction and anxiolysis among distressed women as a consequence of a three-month intensive yoga program. Med Sci Monit. 2005;11:CR555–61. [PubMed] [Google Scholar]
- 36.Merz CJ, Wolf OT. Examination of cortisol and state anxiety at an academic setting with and without oral presentation. Stress. 2015;18:138–42. doi: 10.3109/10253890.2014.989206. [DOI] [PubMed] [Google Scholar]
- 37.Pau A, Rowland ML, Naidoo S, AbdulKadir R, Makrynika E, Moraru R, et al. Emotional intelligence and perceived stress in dental undergraduates: A multinational survey. J Dent Educ. 2007;71:197–204. [PubMed] [Google Scholar]
- 38.Chrousos GP, Torpy DJ, Gold PW. Interactions between the hypothalamic-pituitary-adrenal axis and the female reproductive system: Clinical implications. Ann Intern Med. 1998;129:229–40. doi: 10.7326/0003-4819-129-3-199808010-00012. [DOI] [PubMed] [Google Scholar]
- 39.Klein LC, Whetzel CA, Bennett JM, Ritter FE, Nater UM, Schoelles M. Caffeine administration does not alter salivary a-amylase activity in young male daily caffeine consumers. BMC Res Notes. 2014;7:30. doi: 10.1186/1756-0500-7-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wong JA, Pickworth WB, Waters AJ, al'Absi M, Leventhal AM. Cortisol levels decrease after acute tobacco abstinence in regular smokers. Hum Psychopharmacol. 2014;29:152–62. doi: 10.1002/hup.2382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Duval F, Gonzalez F, Rabia H. Stress Neurobiology. Rev Chil Neuropsiquiat. 2010;48:307–18. [Google Scholar]
- 42.González-Cabrera J, Fernández-Prada M, Iribar-Ibabe C, Peinado JM. Acute and chronic stress increase salivary cortisol: A study in the real-life setting of a national examination undertaken by medical graduates. Stress. 2014;17:149–56. doi: 10.3109/10253890.2013.876405. [DOI] [PubMed] [Google Scholar]
- 43.Kirschbaum C, Kudielka BM, Gaab J, Schommer NC, Hellhammer DH. Impact of gender, menstrual cycle phase, and oral contraceptives on the activity of the hypothalamus-pituitary-adrenal axis. Psychosom Med. 1999;61:154–62. doi: 10.1097/00006842-199903000-00006. [DOI] [PubMed] [Google Scholar]
- 44.Cramer H, Lauche R, Langhorst J, Dobos G. Is one yoga style better than another? A systematic review of associations of yoga style and conclusions in randomized yoga trials. Complement Ther Med. 2016;25:178–87. doi: 10.1016/j.ctim.2016.02.015. [DOI] [PubMed] [Google Scholar]
- 45.Büssing A, Michalsen A, Khalsa SB, Telles S, Sherman KJ. Effects of yoga on mental and physical health: A short summary of reviews. Evid Based Complement Alternat Med. 2012;2012:165410. doi: 10.1155/2012/165410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Cramer H, Lauche R, Langhorst J, Dobos G. Yoga for depression: A systematic review and meta-analysis. Depress Anxiety. 2013;30:1068–83. doi: 10.1002/da.22166. [DOI] [PubMed] [Google Scholar]
- 47.Cramer H, Lauche R, Haller H, Steckhan N, Michalsen A, Dobos G. Effects of yoga on cardiovascular disease risk factors: A systematic review and meta-analysis. Int J Cardiol. 2014;173:170–83. doi: 10.1016/j.ijcard.2014.02.017. [DOI] [PubMed] [Google Scholar]
- 48.Murugesan R, Govindarajulu N, Bera TK. Effect of selected yogic practices on the management of hypertension. Indian J Physiol Pharmacol. 2000;44:207–10. [PubMed] [Google Scholar]
- 49.Qu S, Olafsrud SM, Meza-Zepeda LA, Saatcioglu F. Rapid gene expression changes in peripheral blood lymphocytes upon practice of a comprehensive yoga program. PLoS One. 2013;8:e61910. doi: 10.1371/journal.pone.0061910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Barbieri PG, Mateos RL, Bascones M. Role of stress in the etiopathogenesis of periodontal disease. Av Periodoncia Implantol Oral. 2003;15:77–86. [Google Scholar]
- 51.Katuri KK, Dasari AB, Kurapati S, Vinnakota NR, Bollepalli AC, Dhulipalla R. Association of yoga practice and serum cortisol levels in chronic periodontitis patients with stress-related anxiety and depression. J Int Soc Prev Community Dent. 2016;6:7–14. doi: 10.4103/2231-0762.175404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Lu H, Xu M, Wang F, Liu S, Gu J, Lin S. Chronic stress enhances progression of periodontitis via a1-adrenergic signaling: A potential target for periodontal disease therapy. Exp Mol Med. 2014;46:e118. doi: 10.1038/emm.2014.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Bershadsky S, Trumpfheller L, Kimble HB, Pipaloff D, Yim IS. The effect of prenatal Hatha yoga on affect, cortisol and depressive symptoms. Complement Ther Clin Pract. 2014;20:106–13. doi: 10.1016/j.ctcp.2014.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Innes KE, Bourguignon C, Taylor AG. Risk indices associated with the insulin resistance syndrome, cardiovascular disease, and possible protection with yoga: A systematic review. J Am Board Fam Pract. 2005;18:491–519. doi: 10.3122/jabfm.18.6.491. [DOI] [PubMed] [Google Scholar]
- 55.Innes KE, Vincent HK. The influence of yoga-based programs on risk profiles in adults with type 2 diabetes mellitus: A systematic review. Evid Based Complement Alternat Med. 2007;4:469–86. doi: 10.1093/ecam/nel103. [DOI] [PMC free article] [PubMed] [Google Scholar]