Abstract
Objectives: To determine the marginal microleakage of Class II restorations made with different composite base materials and the static load-bearing capacity of direct composite onlay restorations.
Methods: Class II cavities were prepared in 40 extracted molars. They were divided into five groups (n = 8/group) depending on composite base material used (everX Posterior, SDR, Tetric EvoFlow). After Class II restorations were completed, specimens were sectioned mid-sagitally. For each group, sectioned restorations were immersed in dye. Specimens were viewed under a stereo-microscope and the percentage of cavity leakage was calculated. Ten groups of onlay restorations were fabricated (n = 8/group); groups were made with composite base materials (everX Posterior, SDR, Tetric EvoFlow, Gradia Direct LoFlo) and covered by 1 mm layer of conventional (Tetric N-Ceram) or bulk fill (Tetric EvoCeram Bulk Fill) composites. Groups made only from conventional, bulk fill and short fiber composites were used as control. Specimens were statically loaded until fracture. Data were analyzed using ANOVA (p = 0.05).
Results: Microleakage of restorations made of plain conventional composite or short fiber composite base material showed statistically (p < 0.05) lower values compared to other groups. ANOVA revealed that onlay restorations made from short fiber-reinforced composite (FRC) as base or plain restoration had statistically significant higher load-bearing capacity (1593 N) (p < 0.05) than other restorations.
Conclusion: Restorations combining base of short FRC and surface layer of conventional composite displayed promising performance related to microleakage and load-bearing capacity.
Keywords: Short fiber-reinforced composite, microleakage, only restoration
Introduction
Together with a development of adhesive techniques and the increase in aesthetic demand, particulate filler composite (PFC) resin has become the material of choice for posterior tooth restoration.[1] With the improvements in the mechanical properties of PFCs, their use has been widened not only to the posterior intra-coronal area, but also to extra-coronal restorations.[2] However, further significant improvements are needed in order to extend the use of PFC to high stress-bearing applications such as direct posterior restorations involving cusps.[3,4] In terms of indirect restorations, inlays/onlays are being used from past many years. They were introduced in the hope of overcoming problems associated with the lower degree of conversion related to direct posterior PFCs being replaced by conventional incremental techniques. It was hoped that the use of the indirect technique would improve the load-bearing capacity of the composite by raising the degree of conversion obtained by laboratory post-curing of the restoration. It is reported that extra-oral polymerizations of the composite followed by cementation appear to improve the marginal fit and minimize contraction stress.[5] The mechanical properties of the composites were also improved by post-cure heat treatment, although such improvements were modest and sometimes not statistically significant.[6,7] The relatively high brittleness and low load-bearing capacity of current PFCs still hinder their use in large stress-bearing restorations.[8–10] It therefore follows that there is a considerable need for improved mechanical properties, especially load-bearing capacity and wear resistance, whilst still retaining esthetic properties.
Polymerization shrinkage is another critical limitation of the light-cured dental composites. The shrinkage of current composite resin ranged from 2 to 3% after curing.[11] Such shrinkage induces contraction stress at interface between composite resin and cavity walls, leading to gap-formation and secondary caries. This is a major problem in current restorative dentistry. Different measurement techniques were used to follow and to understand this phenomenon, including the mercury dilatometric technique, the bonded-disc technique, strain-gage methods, shrinkage stress tests and laser interferometry. However, the comparison between these device set-ups and clinical situations is difficult. From this viewpoint, microleakage studies are useful as in vitro indicators of the polymerization shrinkage and marginal adaptation.
Clinically, it is widely recommended nowadays to use a layer of composite base material to reduce the polymerization stress and to develop better mechanical properties.[12,13] The latter is accomplished by decreasing tensile stress concentrations at the restoration interface and reducing the cuspal strain.[12] The significant advantage of this bilayered restoration is its ability to mimic the natural behavior of enamel and dentine.[14]
A new type of short fiber-reinforced composite (FRC) (everX Posterior) was launched recently, whose properties are similar to those of composite base or dentine-replacing materials. It consists of a combination of a resin matrix, short E-glass fibers and inorganic particulate fillers. Short glass fibers are oriented while packing the composite resin into the cavity. The resin matrix contains cross-linked bis-GMA, TEGDMA and linear PMMA forming a polymer matrix called semi-interpenetrating polymer network (semi-IPN), which provides good bonding property and increases the toughness of composite.[15,16] The short fiber composite resin has also proved to control the polymerization shrinkage stress by fiber orientation and, thus, marginal microleakage was reduced compared with conventional PFC resins.[17] To the authors’ knowledge, this short FRC is the only available composite resin which structurally mimics the dentine.
It can be hypothesized that, by using short fiber composite base under PFC, the static load-bearing capacity and microleakage of the material combination could be improved. Thus, the aim of this study is to investigate the effect of short FRC base on load-bearing capacity and microleakage of posterior bilayered composite restorations.
Materials and methods
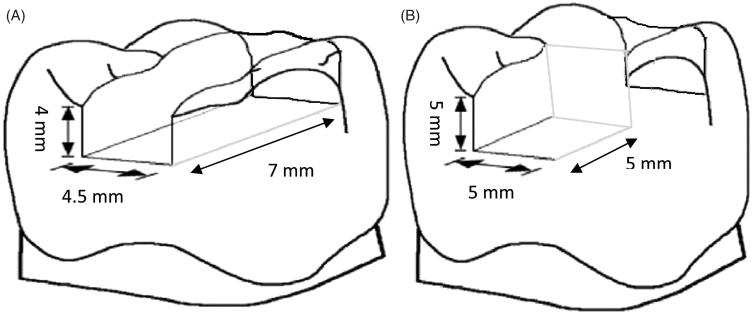
The materials used in the study are listed in Table 1. Forty extracted, sound and caries-free human molar teeth of similar occlusal size (±1 mm) were selected. Upon collection, adhering soft tissues and blood were removed under running water and the teeth were stored in water for a period not exceeding 2 months. The protocol for using these teeth for this research purpose was approved by the research and ethics committee of the Libyan International Medical University. Class II cavities were prepared on the mesial or distal surface. These preparations were accomplished with parallel diamond burs and carbide burs at high speed and under water cooling. The cavities had a 4.5 mm buccal–lingual width, a 7 mm mesio-distal length and 4 mm depth (Figure 1). The margins were located 1–1.5 mm above the cement–enamel junction (CEJ). Following cavity preparation, the tooth surfaces were prepared for bonding with a one-step adhesive system (G-aenial bond, GC Corp., Tokyo, Japan) according to the manufacturer instructions. The teeth were wrapped with circumferential metal matrix and matrix retainers, and the cavity preparations were tightly sealed with a metal matrix. Teeth were distributed into five groups (n = 8).
Table 1. The composite resins investigated and their composition.
| Brand | Manufacturer | Type | Composition |
|---|---|---|---|
| Tetric N-Ceram | IvoclarVivadent AG, Schaan, Liechtenstein | Nano-hybrid | Barium glass 63.5 wt%, prepolymer 17 wt% UDMA, bis-GMA, bis-EMA |
| Tetric Flow | IvoclarVivadent AG, Liechtenstein | Flowable | UDMA, bis-GMA, Bariumglass 63 wt% |
| Gradia LoFlo | GC Corp., Tokyo, Japan | Flowable | UDMA, TEGDMA, Strontium glass 69 wt%, 50 vol% |
| Tetric EvoCeram Bulk Fill | IvoclarVivadent AG, Liechtenstein | Bulk-fill | Barium glass filler 80 wt%, 60 vol% Dimethacrylate co-monomers |
| SDR | Dentsply, York, PA | Bulk-fill | TEGDMA, EBADMA, 68 wt%, 44 vol%, Barium borosilicateglass |
| Alert | Jeneric/Pentron, Wallingford, CT | Condensable | Filler (conventional and micro glass fiber) 84 wt%, 62 vol% |
| everX Posteior | GC Corp, Tokyo, Japan | Short fibre composite | bis-GMA, PMMA, TEGDMA, Shot E-glass fiber filler, Barium glass 74.2 wt%, 53.6 vol% |
PMMA, polymethylmethacrylate; MMA, methylmethacrylate; bis-GMA, bisphenol-A-glycidyldimethacrylate; TEGDMA, triethylene glycol dimethacrylate; UDMA, urethane dimethacrylate; EBADMA, EthoxylatedBisphenol A dimethacrylate; bis-EMA, Ethoxylatedbisphenol-A-dimethacrylate; wt%, weight percentage; vol%, volume percentage.
Figure 1.
Schematic representation of Class II (A) and onlay (B) preparation measurements in mm.
Group A: teeth were incrementally (2 mm) restored with conventional PFC (Tetric N-Ceram); Group B: everX Posterior was used as base and covered with 1 mm layer of PFC. Group C: cavities were restored with SDR base and covered with 1 mm thick layer of PFC. Group D: conventional flowable composite (Tetric EvoFlow) was used as base and covered with 1 mm layer of PFC. Group E: teeth were restored with only bulk fill composite (Tetric EvoCeram Bulk Fill). Restoration of each group was polymerized with hand-light curing unit (Elipar™ FreeLight 2, LED curing light, 3 M ESPE, Seefeld, Germany) for 40 s for each increment (wavelength: 380 and 520 nm with maximal intensity at 470 nm, light irradiance 1000 mW/cm2). After removal of the metal matrix, the restorations were completed with fine diamond burs and polished with abrasive discs. The experimental teeth were stored at room temperature for 2 months. After storage, the root apex was sealed carefully with acrylic resin. A self-curing denture base material was poured into a plastic ring to provide a firm embedding matrix for the tooth specimen. Once the embedding polymer is set, teeth were placed in water to prevent dentine desiccation. All teeth were coated with nail varnish, except for 1 mm beyond the margin of the restorations.
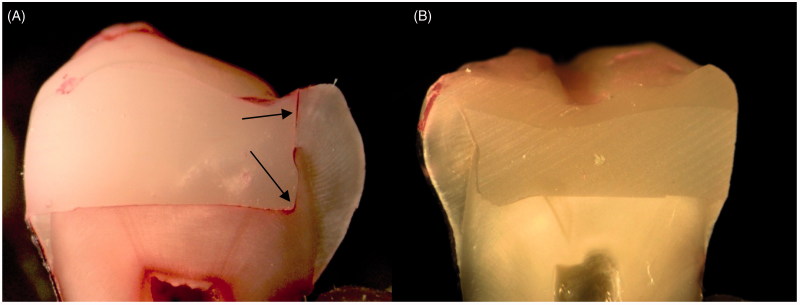
The teeth were sectioned mid-sagitally in the mesio-distal plane (two sections per tooth) using a ceramic cutting disc operating at a speed of 100 rpm (Struers, Glasgow, Scotland) under water cooling. In each group, half of the sectioned restorations were soaked in 0.5% basic Fuchsin dye for 24 h and other half for only 30 min at room temperature. The sectioned teeth were removed from the dye, rinsed in running tap water and brushed gently for 1 min. The dye penetration along restoration margins of each section was evaluated independently using a stereo-microscope (Heerbrugg M3Z, Heerbrugg, Switzerland) at a magnification of 6.5× and the extent of dye penetration was recorded in mm as a percentage of the total margin length (Figure 2).
Figure 2.
Picture of sectioned specimen showing (A) microleakage at restoration margin and (B) no microleakage.
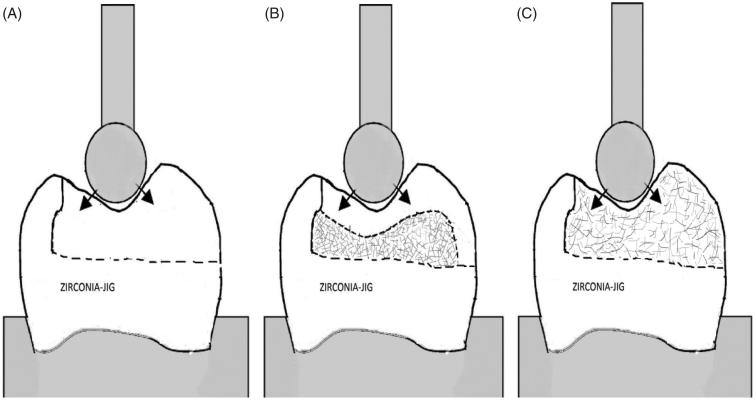
Onlay preparation with one cusp coverage of upper 1st molar was prepared on the zirconia model; preparation was made with 5 mm of axial and occlusal reduction (Figure 1). A transparent template matrix of an ideally contoured upper 1st molar crown was used to aid standardized onlay restoration construction. Onlays were constructed using three different approaches (10 groups) in order to simulate clinical techniques with seven different composite resins (Figure 3).
Approach A: groups (control) made only from PFC (Tetric N-Ceram, Alert) or bulk fill (Tetric EvoCeram) composite resin.
Approach B: groups made with composite base materials (everX Posterior, SDR, Tetric Flow, Gradia Direct Flo) as substructure and covered by 1 mm surface layer of PFC (Tetric N-Ceram) or bulk fill (Tetric EvoCeram Bulk Fill) composite resin.
Approach C: group made from short FRC (everX Posterior).
Figure 3.
Schematic representation of onlay-shaped test specimens and the compressive load test setup. (A) Group made from plain composite resin; (B) group made of different composite base materials and 1 mm surface layer of composite resin; (C) group made only from short FRC resin.
The onlay restorations of each group (n = 10) were polymerized with hand-light curing unit (Elipar™ FreeLight 2, LED curing light, 3M ESPE, Seefeld, Germany) for 40 s for increment (wavelength: 380 and 520 nm with maximal intensity at 470 nm, light irradiance 1000 mW/cm2). Luting cement (Rely-X Unicem2, 3M ESPE, Seefeld, Germany) was used and the restorations were tightly bonded to the model. Subsequently after cementation, the zirconium model with the onlay restoration was fixed to the metal base of testing device before statically loaded (spherical Ø 5 mm) (Figure 3). The static compressive fracture test was performed using a universal testing machine (model LRX, Lloyd Instruments Ltd., Fareham, UK) at a speed of 1 mm/min, and data were recorded using PC software (Nexygen Lloyd Instruments Ltd., Fareham, UK). The loading event was registered until restoration was fractured. Failure patterns of each loaded restorations were visually analyzed.
Data were statistically analyzed by one-way ANOVA followed by Tukey’s test at the p < 0.05 significance level with SPSS version 20 (Statistical Package for Social Science, SPSS Inc, Chicago, IL).
Results
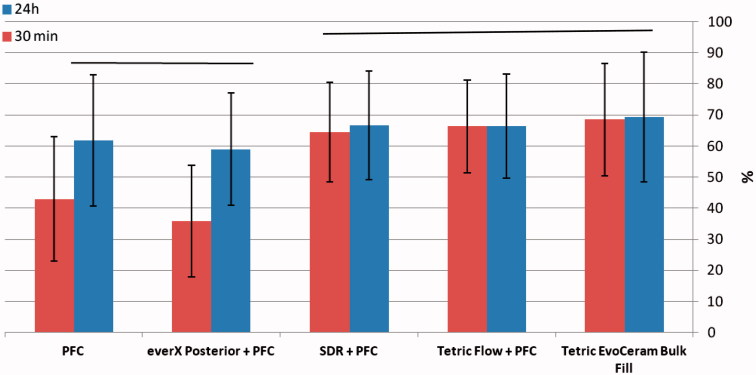
The mean values and standard deviations of microleakage percentage at composite–tooth interface of the five groups are presented in Figure 4. Data showed that restorations made from short FRC base material (everX Posterior) with PFC (Group B) had a significantly lower microleakage percentage than other groups (p < 0.05) except for Group A, the difference was not statistically significant (p < 0.05). In Groups A and B, microleakage percentage after 30 min of staining was significantly lower (p < 0.05) than 24 h staining time, and no difference was found in the other groups (Figure 4).
Figure 4.
Mean percentage of microleakage observed in different groups from total margin length after 30 min and 24 h staining time. Vertical lines represent standard deviation. PFC refers to Tetric N-Ceram composite resin. Horizontal lines above the columns indicate groups that do not differ statistically from each other.
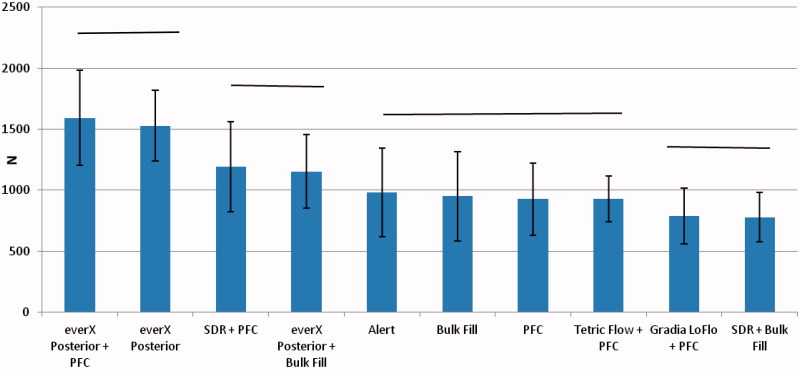
The mean load-bearing capacities of the onlay restorations with standard deviations (SD) are given in Figure 5. ANOVA revealed that onlay restorations made from short FRC base (everX Posterior) with the surface layer of PFC (Tetric N-Ceram) (Approach B) and restorations made only from everX Posterior (Approach C) had significantly higher load-bearing capacity (p < 0.05) than other groups (1593, 1528 N). Onlays made of SDR as base with a surface layer of PFC gave force values of 1193 N, which was statistically higher than the control group (Approach A) (p < 0.05). On the other hand, group made of SDR as base with a surface layer of bulk fill (Tetric EvoCeram) gave force values of 779 N, which was statistically (p < 0.05) the lowest values among all the tested groups. No statistically significant difference was found in the load-bearing capacity between groups made of plain PFC (Tetric N-Ceram and Alert) or bulk fill (Tetric EvoCeram) composite resin (Approach A). Using conventional flowable composite resin (Tetric Flow, Gradia Direct Flo) as base materials did not show any reinforcing effect (Figure 5). Visual inspection revealed two types of fracture patterns according to the material used: (a) chipping restoration fracture was found in most of the restorations made from either plain or base FRC resins and (b) catastrophic splitting of loaded cusps in all other restorations.
Figure 5.
Mean values of compressive load-bearing capacity of onlay restorations. N refers to Newton; PFC refers to Tetric N-Ceram composite resin; Bulk Fill refers to Tetric EvoCeram Bulk Fill composite resin. Vertical lines represent standard deviations. Horizontal lines above the columns indicate groups that do not differ statistically from each other.
Discussion
In our laboratory study, we examined the microleakage of Class II composite restorations and fracture resistance of composite specimens simulating posterior onlay restorations. After years of follow-up of posterior composite restorations, the clinical studies show that fracture of the restoration and recurrent caries are the most common reasons for failure.[18,19] Problems such as poor marginal adaptation, microleakage and recurrent carries depend on the magnitude of the shrinkage and the accompanying stress generated by the polymerization reaction of the resin composite. The polymerization shrinkage depends on many factors such as filler load, type of filler particles and monomer system.
Attempts have been made to reduce the polymerization shrinkage and shrinkage stress of resin composite, and one of these efforts is the placement technique.[12,13] It is known that placement technique is an important factor in the modification of shrinkage stresses, and the magnitude of the stress is mediated by the stiffness of the composite and its stress-relieving capacity. The incremental technique has been largely recommended because it is expected to reduce the shrinkage stress by decreasing the C-factor. A previous study showed that cuspal deflection in Class II cavities was reduced after using composite base materials compared to bulk placement of composite resin.[12] On the other hand, short FRC (everX Posterior) is the unique material of this work containing randomly oriented short glass fiber fillers. This composite was previously reported to exhibit high fracture toughness as well as low polymerization shrinkage.[15–17] Thus, we hypothesized that using short FRC base could reduce the marginal microleakage and reinforce the posterior composite restorations.
Data of this study showed that Class II restorations made from short FRC base with surface layer of PFC had a significantly lower microleakage percentage than other groups (p < 0.05) made of different composite base materials (Figure 4). This in agreement with previous studies which reported low polymerization shrinkage of short FRC compared to PFC.[15,17] Stresses generated during polymerization shrinkage of composites have potential to cause an adhesive failure or microcracking of restorative material and/or at interface with tooth structure. Tezvergil et al. showed that fiber orientation is an important factor influencing the shrinkage-strain and that the shrinkage-strain along the fiber direction is low.[20] Accordingly, short fiber fillers (randomly oriented) might absorb some of the polymerization shrinkage stresses and increase the stress-relieving capacity of the matrix, and this could decrease the marginal microleakage and improve the adaptation of the material.
The high-volumetric shrinkage produced by flowable composite materials (SDR, Tetric Flow and Tetric EvoCeram Bulk Fill) used in this study leads to elevated shrinkage stress values and reduces the marginal integrity. Considering bulk fill placement technique, it has been demonstrated that SDR has better internal adaptation than conventional composites in high C-factor cavities.[21] Another study showed similar levels of microleakage of bulk fill (SDR, Tetric EvoCeram Bulk Fill) and conventional PFC.[12] However, this characteristic did not produce better results for these materials in the present study.
Interestingly, depth of cure and light irradiance at 4 mm increment thickness of everX Posterior was similar to the highest translucent bulk fill composite resin.[22,23] Although the contribution of microleakage to restoration failure remains controversial,[24] microleakage studies are still the most popular test method employed to obtain a preliminary idea about the quality of a new material or combination of materials. Many studies using identical laboratory techniques on the same material are often contradictory, probably due to different manipulation and handling of the materials. Dye penetration technique being simple, common and comparable method was utilized for microleakage evaluation in the present study. Some authors have suggested using staining time of 30 min rather than 24 h to reduce the overestimation of leakage at tooth–restoration interfaces.[25,26] For this reason, we used both and found some differences, but not with all groups (Figure 4).
This in accordance with Scotti et al., who showed that 30 min staining time was suitable for marking marginal microleakage of posterior composite restorations.[26]
Our loading data showed substantial improvements in load-bearing capacity when combinations of materials were used (Figure 5). The function of short fiber composite base is based on supporting the surface PFC layer and working as crack stopper layer. Reinforcing effect of the fiber fillers is based not only on stress transfer from polymer matrix to fibers, but also behavior of individual fiber as a crack stopper. In the posterior region, forces range from 8 to 880 N during normal mastication, but greater loads have been described in bruxism, and teeth in this region may be exposed to extremely high forces when accidentally biting on a hard object or in trauma.[27] Such extreme forces might lead to cracking and/or fracture of the enamel, but crack propagation continues toward the dentine where it is completely absorbed.
From this point of view, short FRC base mimics the supportive function of dentine during loading and acts as dentine replacing material. To receive support from the short fiber composite substructure for the surface particulate composite, the structural rigidity of the short fiber composite substructure should be higher than that of the surface particulate composite resin. In this study, the FRC contains short E-glass fiber fillers with length ranging from 0.6 to 1.5 mm (main 0.8 mm), resulting in random orientation of the short fibers within the composite restorations. Random fiber orientation and lowered cross-linking density of the polymer matrix by the semi-IPN structure likely had a significant role in mechanical properties. According to Krenchel, short random orientated in 3D fiber provides strengthening factor of 0.2, whereas in 2D orientation gives 0.38, and unidirectional fibers gives factor of 1.[16]
Previous study by authors demonstrated that fiber orientation likely has a significant role in the load-bearing capacity of composite onlay restorations reinforced by two types of FRCs as base materials.[3] Continuous bidirectional FRC gave a stiffer structure, and thus the ability to slow or arrest crack propagation was higher than the random-oriented FRC, which led to delamination of surface PFC from the underlying FRC.[3] In contrast, the less stiff structure of short random FRC allowed the crack to propagate through the FRC structure to make a compound-like fracture without any delamination.
On the other hand, if the function of the short fiber composite base is based on the mechanism of a crack stopper, the distance from the surface of the stress initiation point to the fibers is of importance. Therefore, the volume fraction or thickness of short fiber composite could contribute to the crack propagation and load-bearing capacity. Previous study by authors showed that, when short random FRC was used as substructure for PFC, the load-bearing capacity of the materials combination increased linearly as the thickness layer of FRC increased.[3,28] From this point of view, in this study, short fiber composite base was covered with only 1 mm layer thickness of PFC resin.
Stress applied to the teeth and dental restorations is generally low and repetitive rather than being isolated and impactive in nature. However, because of a linear relationship between fatigue and static loading, the compressive static test also gives valuable information concerning load-bearing capacity.[29] The fracture resistance values determined by various investigators were recorded under different measurement criteria. These criteria were either initial cracking that was interpreted as crack development or a reduction in the load by an absolute or relative amount.[30] For this study, the maximum force on the final fracture was determined. Fracture patterns were analyzed visually and two types of fracture patterns were found, where each fracture type occurred according to the type of material. Because of the brittleness of composite resin, the catastrophic splitting of cusps was found in all specimens made from PFC only. In contrast, short fiber composite allowed the crack to propagate through the surface PFC and short fiber composite resin to make a compound-like fracture without any delamination. Our finding is in accordance with a new study by Fráter et al., who demonstrated that short FRC base improves the fracture resistance and the failure mode (restorable) of posterior composite restorations.[31]
Methodologically, limitations like sample size and aging process, such as alternate thermal stress, mechanical stress, wear and water storage, should be taken into consideration. Despite the importance of laboratory studies to answer some questions in a short time, the real performance of restorations can only be determined by long-term clinical trials.
Conclusions
Based on the microleakage and compressive loading tests, base of short FRC resin and surface layer of conventional composite resin is the best combination.
Acknowledgements
Testing materials were provided by the manufacturing companies, which is greatly appreciated. This study is part of the activity of BioCity Turku Biomaterials Research Program (www.biomaterials.utu.fi).
Declaration of interest
Author Pekka K. Vallittu consults Stick Tech Ltd – Member of GC Group in RD. Other authors declare no conflicts of interest.
References
- 1. Park J, Chang J, Ferracane J, Lee IB. How should composite be layered to reduce shrinkage stress: incremental or bulk filling? Dent Mater. 2008;24:1501–1505 [DOI] [PubMed] [Google Scholar]
- 2. Fennis WM, Kuijs RH, Roeters FJ, Creugers NH, Kreulen CM. Randomized control trial of composite cuspal restorations: five-year results. J Dent Res. 2014;93:36–41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Garoushi S, Lassila LVJ, Vallittu PK. Fiber-reinforced composite substructure: load bearing capacity of an onlay restoration. Acta Odontol Scand. 2006;64:281–285 [DOI] [PubMed] [Google Scholar]
- 4. Xu HH, Quinn JB, Smith DT, Giuseppetti AA, Eichmiller FC. Effect of different whiskers on the reinforcement of dental resin composites. Dent Mater. 2003;19:359–367 [DOI] [PubMed] [Google Scholar]
- 5. Wendt SL, Leinfelder KF. The clinical evaluation of heat-treated composite resin inlays. J Am Dent Assoc. 1990;120:177–181 [DOI] [PubMed] [Google Scholar]
- 6. Loza-Herrero MA, Rueggeberg FA, Caughman WF, Schuster GS, Lefebvre CA, Gardner FM. Effect of heating delay on conversion and strength of a post-cured resin composite. J Dent Res. 1998;77:426–431 [DOI] [PubMed] [Google Scholar]
- 7. Hejazi AAE, Watts DC. Creep and visco-elastic recovery of cured and secondary-cured composites and resin-modified glass ionomers. Dent Mater. 1999;15:138–143 [DOI] [PubMed] [Google Scholar]
- 8. Zandinejad AA, Atai M, Pahlevan A. The effect of ceramic and porous fillers on the mechanical properties of experimental dental composites. Dent Mater. 2006;22:382–387 [DOI] [PubMed] [Google Scholar]
- 9. Wilder AD Jr Bayne SC, Heymann HO. Long-term clinical performance of direct posterior composites. Trans Acad Dent Mater. 1996;9:151–169 [Google Scholar]
- 10. Xu HH. Dental composite resins containing silica-fusedceramic single-crystalline whiskers with various filler levels. J Dent Res. 1999;78:1304–1311 [DOI] [PubMed] [Google Scholar]
- 11. Chen MH, Chen CR, Hsu SH, Sun SP, Su WF. Low shrinkage light curable nanocomposite for dental restorative material. Dent Mater. 2006;22:138–145 [DOI] [PubMed] [Google Scholar]
- 12. Moorthy A, Hogg CH, Dowling AH, Grufferty BF, Benetti AR, Fleming GJ. Cuspal deflection and microleakage in premolar teeth restored with bulk-fill flowable resin-based composite base materials. J Dent. 2012;40:500–505 [DOI] [PubMed] [Google Scholar]
- 13. Campos EA, Ardu S, Lefever D, Jassé FF, Bortolotto T, Krejci I. Marginal adaptation of Class II cavities restored with bulk-fill composites. J Dent. 2014;42:575–581 [DOI] [PubMed] [Google Scholar]
- 14. Magne P, Knezevic A. Thickness of CAD–CAM composite resin overlays influences fatigue resistance of endodontically treated premolars. Dent Mater. 2009;25:1264–1268 [DOI] [PubMed] [Google Scholar]
- 15. Garoushi S, Säilynoja E, Vallittu PK, Lassila L. Physical properties and depth of cure of a new short fiber reinforced composite. Dent Mater. 2013;29:835–841 [DOI] [PubMed] [Google Scholar]
- 16. Garoushi S, Vallittu PK, Lassila LVJ. Short glass fiber reinforced restorative composite resin with semi-interpenetrating polymer network matrix. Dent Mater. 2007;23:1356–1362 [DOI] [PubMed] [Google Scholar]
- 17. Garoushi S, Vallittu PK, Watts DC, Lassila LVJ. Polymerization shrinkage of experimental short glass fiber reinforced composite with semi-inter penetrating polymer network matrix. Dent Mater. 2008;24:211–215 [DOI] [PubMed] [Google Scholar]
- 18. Pallesen U, Qvist V. Composite resin fillings and inlays: an 11-year evaluation. Clin Oral Invest. 2003;7:71–79 [DOI] [PubMed] [Google Scholar]
- 19. Wassell RW, Walls AWG, McCabe JF. Direct composite inlays versus conventional composite restorations: 5-year follow-up. J Dent. 2000;28:375–382 [DOI] [PubMed] [Google Scholar]
- 20. Tezvergil A, Lassila LV, Vallittu PK. The effect of fiber orientation on the polymerization shrinkage strain of fiber-reinforced composites. Dent Mater. 2006;22:610–616 [DOI] [PubMed] [Google Scholar]
- 21. Van Ende A, De Munck J, Van Landuyt KL, Poitevin A, Peumans M, Van Meerbeek B. Bulk-filling of high C-factor posterior cavities: effect on adhesion to cavity-bottom dentin. Dental Mater. 2013;29:269–277 [DOI] [PubMed] [Google Scholar]
- 22. Garoushi S, Vallittu P, Lassila L. Depth of cure and surface microhardness of experimental short fiber-reinforced composite. Acta Odontol Scand. 2008;66:38–42 [DOI] [PubMed] [Google Scholar]
- 23. Goracci C, Cadenaro M, Fontanive L, Giangrosso G, Juloski J, Vichi A, Ferrari M. Polymerization efficiency and flexural strength of low-stress restorative composites. Dent Mater. 2014;30:688–694 [DOI] [PubMed] [Google Scholar]
- 24. Heintze SD. Systematic reviews: I. The correlation between laboratory tests on marginal quality and bond strength. II. The correlation between marginal quality and clinical outcome. J Adhes Dent. 2007;9:77–106 [PubMed] [Google Scholar]
- 25. Ernst CP, Galler P, Willershausen B, Haller B. Marginal integrity of class V restorations: SEM versus dye penetration. Dent Mater. 2008;24:319–327 [DOI] [PubMed] [Google Scholar]
- 26. Scotti N, Comba A, Gambino A, Paolino DS, Alovisi M, Pasqualini D, Berutti E. Microleakage at enamel and dentin margins with a bulk fills flowable resin. Eur J Dent. 2014;8:1–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Magne P, Knezevic A. Simulated fatigue resistance of composite resin versus porcelain CAD/CAM overlay restorations on endodontically treated molars. Quintessence Int. 2009;40:125–133 [PubMed] [Google Scholar]
- 28. Garoushi S, Lassila LVJ, Tezvergil A, Vallittu PK. Load bearing capacity of fiber-reinforced and particulate filler composite resin combination. J Dent. 2006;34:179–184 [DOI] [PubMed] [Google Scholar]
- 29. Garoushi S, Lassila LV, Tezvergil A, Vallittu PK. Static and fatigue compression test for particulate filler composite resin with fiber-reinforced composite substructure. Dent Mater. 2007;23:17–23 [DOI] [PubMed] [Google Scholar]
- 30. Stipho HD. Effect of glass fiber reinforcement on some mechanical properties of autopolymerizing polymethyl methacrylate. J Prosthet Dent. 1998;79:580–584 [DOI] [PubMed] [Google Scholar]
- 31. Fráter M, Forster A, Keresztúri M, Braunitzer G, Nagy K. In vitro fracture resistance of molar teeth restored with a short fibre-reinforced composite material. J Dent. 2014;42:1143–1145 [DOI] [PubMed] [Google Scholar]