Abstract
Objective
To estimate trajectories of body mass index (BMI) and determine their association with incident frailty in later life.
Methods
Data come from the 2004 to 2012 waves of the Health and Retirement Study, a longitudinal survey of older adults. Analysis was restricted to respondents who were not frail at baseline (n = 10,827). BMI (kg/m2) was calculated from self-reported weight and height. Incident frailty was assessed using the Frailty Index. Longitudinal growth mixture modeling was used to estimate the relationship between BMI trajectories and incident frailty over a 10-year period.
Results
Four trajectory classes were identified: weight gain (n = 162 [1.4%], mean final BMI = 42 kg/m2), weight loss (n = 171 [1.7%], mean final BMI = 25.0 kg/m2), consistent obesity (n = 640 [6.8%], mean final BMI = 34.7 kg/m2), and consistent overweight (n = 9,864 [90.1%] mean final BMI = 26.0 kg/m2). Cumulative incidence of frailty was 19.9%. Relative to the consistent overweight class, the weight gain class had the highest likelihood of incident frailty (odds ratio, OR: 3.61, 95% confidence interval, CI: 2.39–5.46). The consistent obesity (OR: 2.72, 95% CI: 2.06–3.58) and weight loss (OR: 2.81, 95% CI: 1.84–4.30) classes had similarly elevated risk of frailty.
Conclusions
Weight change and obesity are associated with risk of frailty.
Introduction
Frailty is a geriatric syndrome characterized by increased vulnerability for physical decline (1). It is estimated that 1 in 10 adults aged 65 years or older, 1 in 4 aged 75 or older, and approximately half of adults aged 85 or older meet criteria for frailty (2).
Weight (and weight change) may be an important contributor to frailty risk. While some definitions of frailty specify low weight and/or weight loss as a criterion (3), other models imply that weight gain is also relevant through the inclusion of medical comorbidities associated with obesity (e.g., type 2 diabetes) in their diagnostic criteria. In addition, weakness or functional decline in the context of obesity (i.e., dynapenic obesity) (4–6) highlights the potential for a U-shaped relationship between weight and frailty. Consistent with this, a recent longitudinal study found that while frailty risk was highest among those who lost weight, individuals who were consistently overweight also had greater risk of frailty as compared with those with consistent normal weight (7). An important limitation of this study was that its sample consisted solely of non-Hispanic white (Finnish) men, and the prevalence of obesity was much lower than US estimates (9.8% vs. 26% for US men) (8).
The purpose of this study was to investigate trajectories of body mass index (BMI) in relation to frailty risk over a 10-year period. We hypothesized that trajectories characterized by weight change (either gain or loss) would be associated with greater likelihood of developing frailty relative to stable weight.
Methods
Data
Data come from five waves (2004–2012) of the Health and Retirement Study (HRS), a nationally representative cohort of approximately 20,000 US adults aged 51 and older interviewed every 2 years (9). The HRS has a steady-state design which enrolls new participants every 6 years, most recently in 2010. The analytic sample was limited to respondents who provided at least one wave of data on BMI; individuals who died or dropped out from the study during follow-up contributed to the calculation of BMI trajectories up to their point of censor. Respondents living in a nursing home and with proxies were excluded. We also excluded respondents who were frail at their baseline assessment (N = 2,139), resulting in an analytical sample of 10,827 (Supporting Information Figure 1). The mean number of interviews during the study period for this analytic cohort was 4.4 (SD = 1.2), and 749 respondents died during follow-up.
The HRS is approved by the Institutional Review Board at the University of Michigan, and all participants provided informed consent.
Exposure: BMI
BMI (kg/m2) was calculated from self-reported weight and height, which was assessed at each wave.
Outcome: Frailty
Frailty (both at baseline and follow-up) was operationalized using the Frailty Index (FI) according to the Cumulative Burdens model proposed by Rockwood et al. (10). The FI is calculated as the ratio of health problems present to the number of total possible problems considered in the study (e.g., 10 problems present/30 possible problems indicates an FI = 0.33). This study used an FI of 30 health problems, all measured by self-report, consistent with Rockwood et al.’s model (Supporting Information Table 1) (10). The cutoff criteria of FI>0.25 was used to indicate frailty status, as established in prior studies (10). Respondents with an FI>0.25 at their baseline interview were excluded from analysis.
Covariates
Demographic variables included age (in years), race (white, black, and other), gender, marital status (married, widowed, and not married), years of education, and household wealth (total assets minus total debt, in quartiles). One behavioral factor, smoking status, was also included and categorized as never, former, or current smoker. All covariates were assessed at baseline.
Statistical analysis
Growth mixture modeling (GMM) describes differences in longitudinal change in a measure (e.g., BMI) among multiple unobserved (i.e., latent) subpopulations, as well as interindividual variability in those trajectories (11). GMM allows for estimation of distinct subpopulations (i.e., classes) of growth, characterized by different patterns of change over time (12). Individual membership in a particular trajectory class can then serve as a predictor of outcomes (e.g., frailty) within the GMM framework (12).
We built GMMs describing longitudinal trajectories in BMI according to a stepwise procedure (11). First, we used model fit statistics to compare three one-class (i.e., no heterogeneity in the BMI trajectory) models assuming different forms of overall growth: no growth, linear growth, and quadratic growth. At this step, model fit statistics indicated that the linear growth model provided the best and most parsimonious fit to the data. Next, we determined the number of subclasses best explaining the variation of this linear growth by comparing models with one to six growth classes. Growth parameter (i.e., intercept and slope) means and variances were estimated freely across all growth classes. Selection of the appropriate number of classes was guided by both model fit and interpretability. The sample size-adjusted Bayesian Information Criterion and the Adjusted Lo-Mendell-Rubin likelihood ratio test were used to compare the nested models of one through six classes; smaller values of these statistics indicate better model fit. Third, we obtained parameter estimates from the selected GMM model of BMI trajectories. Finally, we regressed frailty status in 2012 on the BMI trajectories to estimate the relative odds of developing frailty; the most common BMI trajectory class was selected as the reference group.
Analyses were weighted according to HRS respondent-level sampling weights. We used full information maximum likelihood estimation as implemented in MPlus software (Version 7), and all P values refer to two-tailed tests.
Results
Mean age of the sample at baseline was 65 years, approximately 55% were women, and 84% were non-Hispanic white (Table 1). Model fit statistics for the series of GMMs evaluated are shown in Supporting Information Table 2. Using a balance of model fit indices, interpretability, and explanatory power, we selected the four-class model of BMI trajectories: Class 1 (n = 162, 1.4% of the sample) was characterized by weight gain, Class 2 (n = 171, 1.7%) was characterized by weight loss, Class 3 (n = 9,864, 90.1%) was consistent overweight, and Class 4 (n = 640, 6.8%) was consistent obesity. Spaghetti plots were visually inspected to validate the trajectory classes. We note that these class names are simply useful heuristics for describing the average trajectory for each group.
TABLE 1.
Descriptive characteristics in the overall sample and by BMI trajectory class
| Overall | Class 1, weight gain | Class 2, weight loss | Class 3, consistent overweight | Class 4, consistent obesity | |
|---|---|---|---|---|---|
| N | 10,827 | 162 | 171 | 9,854 | 640 |
| Female | 54.65 | 68.52 | 73.10 | 52.65 | 77.03 |
| Age (mean, SD) | 65.14 (9.70) | 61.27 (8.2) | 64.28 (9.97) | 65.44 (9.75) | 61.83 (8.10) |
| Race/ethnicity | |||||
| Non-Hispanic white | 83.79 | 67.28 | 77.19 | 84.84 | 73.59 |
| Black | 13.34 | 27.78 | 19.88 | 12.28 | 24.22 |
| Hispanic/other | 2.87 | 4.94 | 2.92 | 2.88 | 2.19 |
| Education (mean, SD) | 12.94 (3.04) | 11.51 (3.79) | 11.62 (3.52) | 13.01 (3.02) | 12.63 (2.93) |
| Marital status | |||||
| Currently married/partnered | 70.13 | 59.26 | 60.23 | 71.02 | 61.88 |
| Separated/divorced/never married | 14.79 | 20.37 | 17.55 | 14.19 | 21.88 |
| Widowed | 15.08 | 20.37 | 22.22 | 14.80 | 16.25 |
| Household wealth | |||||
| Quartile 1 (lowest) | 25.12 | 47.53 | 50.88 | 23.10 | 43.75 |
| Quartile 2 | 24.91 | 24.69 | 25.73 | 24.68 | 28.28 |
| Quartile 3 | 24.97 | 20.99 | 12.28 | 25.89 | 15.31 |
| Quartile 4 | 24.99 | 6.79 | 11.11 | 26.33 | 12.66 |
Values are means (SD) or percents.
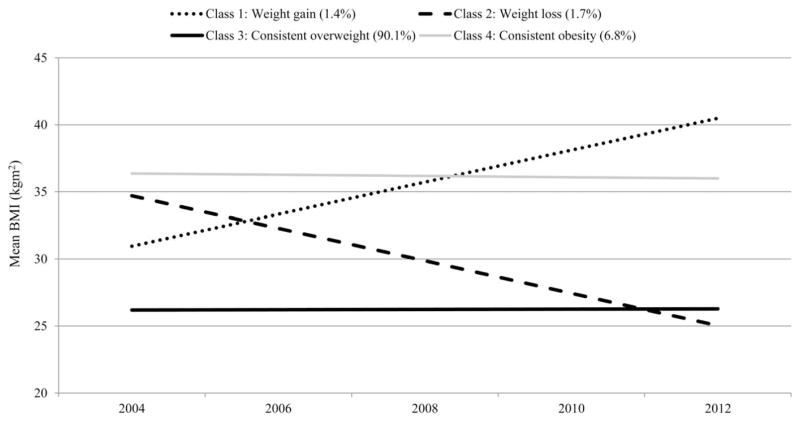
Figure 1 shows the probability of class membership, conditional on demographic characteristics, and mean BMI of the four trajectories over time. The mean BMI of the weight gain class was approximately 30 kg/m2 at baseline and 42 kg/m2 at follow-up. The consistent obesity and weight loss classes had similar BMI at baseline (36.4 kg/m2 and 34.7 kg/m2, respectively) but differed substantially at follow-up (36.0 kg/m2 and 25.0 kg/m2, respectively). The consistent overweight class had a stable BMI of approximately 26 kg/m2. The predictors of these BMI trajectories are summarized in Table 2. Regardless of class membership, predictors of lower initial BMI (intercept) were female gender, more education, older age, greater wealth, and current smoking. Being married and black race were associated with higher initial BMI. Older age, male gender, and black race were negatively associated with rate of BMI change.
Figure 1.
Estimated mean BMI over time for the four-class model of growth trajectories. Percentages represent the class prevalence. Values are estimated from conditional LGMM, accounting for covariates. N = 10,872.
TABLE 2.
Predictors of BMI trajectory class membership
| Odds ratio | P | |
|---|---|---|
| BMI trajectory: Weight gain | ||
| Age | 0.96 | 0.003 |
| Education | 0.90 | 0.002 |
| Female gender | 1.82 | 0.006 |
| Race (ref. Non-Hispanic white) | ||
| Black | 1.56 | 0.378 |
| Other race | 1.15 | 0.769 |
| Marital status (ref. currently married) | ||
| Divorced/separated/never married | 1.00 | 0.997 |
| Widow | 1.43 | 0.435 |
| Wealth | 0.71 | 0.003 |
| Smoking status (ref. Never) | ||
| Former | 1.31 | 0.214 |
| Current | 1.91 | 0.083 |
| BMI trajectory: Weight loss | ||
| Age | 0.98 | 0.251 |
| Education | 0.93 | 0.008 |
| Female gender | 2.39 | <0.001 |
| Race (ref. Non-Hispanic white) | ||
| Black | 1.08 | 0.778 |
| Other race | 0.76 | 0.603 |
| Marital status (ref. currently married) | ||
| Divorced/separated/never married | 1.16 | 0.572 |
| Widowed | 1.30 | 0.423 |
| Wealth | 0.60 | <0.001 |
| Smoking status (ref. Never) | ||
| Former | 1.25 | 0.285 |
| Current | 1.02 | 0.939 |
| BMI trajectory: Consistent obesity | ||
| Age (years) | 0.96 | <0.001 |
| Education (years) | 0.99 | 0.69 |
| Female gender | 2.58 | 0 |
| Race (ref. Non-Hispanic white) | ||
| Black | 1.28 | 0.214 |
| Other race | 0.54 | 0.105 |
| Marital status (ref. currently married) | ||
| Divorced/separated/never married | 0.91 | 0.588 |
| Widowed | 0.98 | 0.948 |
| Household wealth | 0.69 | 0 |
| Smoking status (ref. Never) | ||
| Former | 1.15 | 0.247 |
| Current | 0.62 | 0.044 |
Finally, we examined the relationship between these BMI trajectories and likelihood of frailty at follow-up, accounting for demographic characteristics and smoking status. The 10-year cumulative incidence of frailty was 2,156 (19.9%). Relative to the consistent overweight class, the weight gain class had the highest relative likelihood of incident frailty (Nfrail = 72; odds ratio, OR: 3.61, 95% confidence interval, CI: 2.39–5.46). The consistent obesity (Nfrail = 248; OR: 2.72, 95% CI: 2.06–3.58) and weight loss (Nfrail = 56; OR: 2.81, 95% CI: 1.84–4.30) classes also had elevated risk of frailty relative to the consistent overweight class (Supporting Information Table 3).
Discussion
The primary finding from this study is that weight change trajectories in later life are associated with frailty risk for older adults. Specifically, weight gain and weight loss are associated with elevated risk of frailty relative to a trajectory of stable weight in the overweight range. These results add context to prior work on the measurement of frailty which had indicated that the weight loss/low weight criterion is generally a poor discriminator of identifying who is frail (13–15). Together with this study, this suggests that other symptoms, particularly weakness—a defining characteristic of dynapenic obesity—may be more relevant to the mechanisms underlying physical decline (16).
Results should be interpreted in light of study limitations. BMI was measured using self-report weight and height, which underestimates true BMI (17); this suggests that our findings regarding weight gain and risk of frailty are conservative. By excluding individuals in nursing homes and with proxies we may have underestimated the incidence of frailty. Finally, frailty was only assessed at the end of follow-up. This study also has a number of strengths: our data are derived from a large population-based sample, which enhances the generalizability of the findings, and we excluded prevalent cases of frailty at baseline to reduce the risk of reverse causation.
Our findings have potential clinical implications because BMI is routinely collected at healthcare visits and thus is a readily available way to monitor risk of frailty. The Meaningful Use Core Measures in Electronic Medical Records requires that providers record and chart changes in BMI for patients of all ages (18), and Medicare recently started covering behavioral weight loss counseling for patients who have obesity (19). In addition, since in this study weight loss was not associated with substantially lower risk of frailty among participants who had obesity at baseline, this suggests that wellness approaches other than, or in addition to, weight loss (e.g., strength training), may be needed in order to prevent the functional declines seen with obesity (20).
Overall, these findings call into question the notion that frailty is a condition primarily applicable to older adults who have underweight.
Supplementary Material
Acknowledgments
Funding agencies: AR is supported by an award from the Microbiology, Infectious Diseases and Public Health Epidemiology (MIDPH) Summer Research Fellowship Program at Virginia Commonwealth University. ML is supported by T32-MH073553. MP was supported by Duke University Building Interdisciplinary Research Careers in Women’s Health (K12-HD043446). BM is supported by K01-MH093642, 2P60-MD002249-06, and 1-16-ICTS-082.
Footnotes
Disclosure: The authors declared no conflicts of interest.
Author contributions: AR: conception of study, drafting of manuscript. ML: conception of study, data analysis and interpretation of data, drafting and revision of manuscript. MP: conception of study, interpretation of data, drafting and revision of manuscript. BM: conception of study, interpretation of data, drafting and revision of manuscript.
Additional Supporting Information may be found in the online version of this article.
References
- 1.Woods NF, LaCroix AZ, Gray SL, et al. Frailty: emergence and consequences in women aged 65 and older in the Women’s Health Initiative Observational Study. J Am Geriatr Soc. 2005;53:1321–1330. doi: 10.1111/j.1532-5415.2005.53405.x. [DOI] [PubMed] [Google Scholar]
- 2.Cigolle CT, Ofstedal MB, Tian Z, Blaum CS. Comparing models of frailty: the Health and Retirement Study. J Am Geriatr Soc. 2009;57:830–839. doi: 10.1111/j.1532-5415.2009.02225.x. [DOI] [PubMed] [Google Scholar]
- 3.Fried LP, Tangen CM, Walston J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56:M146. doi: 10.1093/gerona/56.3.m146. [DOI] [PubMed] [Google Scholar]
- 4.Blaum CS, Xue QL, Michelon E, Semba RD, Fried LP. The association between obesity and the frailty syndrome in older women: the Women’s Health and Aging Studies. J Am Geriatr Soc. 2005;53:927–934. doi: 10.1111/j.1532-5415.2005.53300.x. [DOI] [PubMed] [Google Scholar]
- 5.Bowen ME. The relationship between body weight, frailty, and the disablement process. J Gerontol B Psychol Sci Soc Sci. 2012;67:618–626. doi: 10.1093/geronb/gbs067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Strandberg TE, Sirola J, Pitkala KH, Tilvis RS, Strandberg AY, Stenholm S. Association of midlife obesity and cardiovascular risk with old age frailty: a 26-year follow-up of initially healthy men. Int J Obes (Lond) 2012;36:1153–1157. doi: 10.1038/ijo.2012.83. [DOI] [PubMed] [Google Scholar]
- 7.Strandberg TE, Stenholm S, Strandberg AY, Salomaa VV, Pitkala KH, Tilvis RS. The “obesity paradox,” frailty, disability, and mortality in older men: a prospective, longitudinal cohort study. Am J Epidemiol. 2013;178:1452–1460. doi: 10.1093/aje/kwt157. [DOI] [PubMed] [Google Scholar]
- 8.May AL, Freedman D, Sherry B, Blanck HM Centers for Disease Control and Prevention. Obesity - United States, 1999–2010. MMWR Surveill Summ. 2013;62:120–128. [PubMed] [Google Scholar]
- 9.Heeringa SG, Connor J. HRS/AHEAD Documentation Report. Institute for Social Research, University of Michigan; Ann Arbor, MI: 1995. Technical Description of the Health and Retirement Study Sample Design. [Google Scholar]
- 10.Rockwood K, Song X, MacKnight C, et al. A global clinical measure of fitness and frailty in elderly people. CMAJ. 2005;173:489–495. doi: 10.1503/cmaj.050051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ram N, Grimm KJ. Growth mixture modeling: a method for identifying differences in longitudinal change among unobserved groups. Int J Behav Dev. 2009;33:565–576. doi: 10.1177/0165025409343765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Muthen B. Latent variable analysis: Growth mixture modeling and related techniques for longitudinal data. In: Kaplan D, editor. Handbook of Quantitative Methodology for the Social Sciences. Sage; Thousand Oaks, CA: 2004. pp. 345–368. [Google Scholar]
- 13.Lohman M, Dumenci L, Mezuk B. Sex differences in the construct overlap of frailty and depression: evidence from the Health and Retirement Study. J Am Geriatr Soc. 2014;62:500–505. doi: 10.1111/jgs.12689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bandeen-Roche K, Xue QL, Ferrucci L, et al. Phenotype of frailty: characterization in the women’s health and aging studies. J Gerontol A Biol Sci Med Sci. 2006;61:262–266. doi: 10.1093/gerona/61.3.262. [DOI] [PubMed] [Google Scholar]
- 15.Mezuk B, Lohman M, Dumenci L, Lapane KL. Are depression and frailty overlapping syndromes in mid- and late-life? A latent variable analysis. Am J Geriatr Psychiatry. 2013;21:560–569. doi: 10.1016/j.jagp.2012.12.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Xue QL, Bandeen-Roche K, Varadhan R, Zhou J, Fried LP. Initial manifestations of frailty criteria and the development of frailty phenotype in the Women’s Health and Aging Study II. J Gerontol A Biol Sci Med Sci. 2008;63:984–990. doi: 10.1093/gerona/63.9.984. [DOI] [PubMed] [Google Scholar]
- 17.Stommel M, Schoenborn CA. Accuracy and usefulness of BMI measures based on self-reported weight and height: findings from the NHANES & NHIS 2001–2006. BMC Public Health. 2009;9:421. doi: 10.1186/1471-2458-9-421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Center for Medicare and Medicaid Services. Eligible Professional Meaningful Use Table of Contents: Core and Menu Set Objectives. Stage 1 (2013 Definition) US Department of Health and Human Services; Baltimore, MD: Available from: https://www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/downloads/EP-MU-TOC.pdf. [Google Scholar]
- 19.Center for Medicare and Medicaid Services. Obesity Screening & Counseling. US Department of Health and Human Services; Baltimore, MD: Available from: http://www.medicare.gov/coverage/obesity-screening-and-counseling.html. [Google Scholar]
- 20.Villareal DT, Apovian CM, Kushner RF, et al. Obesity in older adults: technical review and position statement of the American Society for Nutrition and NAASO, The Obesity Society. Obes Res. 2005;13:1849–1863. doi: 10.1038/oby.2005.228. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.