Abstract
Respiratory sinus arrhythmia (RSA) is accepted as a peripheral marker of cardiac-linked parasympathetic regulation. According to polyvagal theory, the RSA is also considered as the index of emotion regulation. The neurovisceral integration model posits that parasympathetic modulation of the heart marked by RSA is related to complex nervous regulation associated with emotional and cognitive processing. From this perspective, high resting RSA amplitude associated with a greater withdrawal during stressors and subsequent recovery could represent a flexible and adaptive physiological response system to a challenge. Conversely, low resting RSA accompanied by an inadequate reactivity to stress might reflect maladaptive regulatory mechanisms. The RSA reactivity is different with various types of stressors: while the RSA decreases to cognitive tasks indicating a vagal withdrawal, the RSA magnitude increases to emotional challenge indicating an effective cognitive processing of emotional stimuli. The RSA reactivity to stress could have important implications for several mental disorders, e.g. depressive or anxiety disorder. It seems that the study of the RSA, as a non-invasive index of ‘brain-heart’ communication, could provide important information on the pathway linked to mental and physical health.
Keywords: Cognition, emotion, heart rate variability, respiratory sinus arrhythmia, stress
Introduction
Breathing oscillations influence the firing activity of the sinoatrial node defined as respiratory sinus arrhythmia (RSA). RSA is a consequence of various central as well as peripheral effects from medullary cardiorespiratory centre and reflex responses from pulmonary/cardiovascular receptors resulting in heart rate oscillations in accordance with respiratory cycle. However, RSA is mainly affected by cardiac-linked vagal efferent modulation from the nucleus ambiguus, which is influenced by several central projections (e.g. amygdala, hypothalamus)1,2. Despite the fact that sympathetic activity can contribute to RSA by a specific pattern, it is elevated in the inspiratory period with maximum at the end of inspiration3. The question that RSA is confined to parasympathetic regulation of the heart has been discussed by many researchers4,5,6. Muscarine receptors inhibition by parasympatholytic agent atropine results in diminished RSA magnitude7,8. However, understanding of RSA is limited by peripheral factors including alterations of muscarinic receptors functioning (e.g. density of distribution, sensitivity)9,10. Hence, the peripheral mechanisms involved in cardiac vagal regulation remain unclear10.
RSA as an index of cardiac vagal modulation has been used in the study of emotion and self-regulatory capacity and reactivity11,12. This issue is still discussed in the context of neurophysiological mechanisms influencing RSA, such as breathing, and from the perspective of relation between RSA and stress reactivity, important for the understanding of stress-related disorders13,14. The aim of the present review was to highlight the nature of RSA and discuss implications in psychophysiological research with regard to emotional regulation and stress reactivity.
Respiratory sinus arrhythmia (RSA) in the context of neurovisceral integration model
Thayer and Lane15,16 reported the significance of cardiac vagal regulation indexed by RSA in the context of neurovisceral integration model. Afferent-efferent vagal central functional consolidation is regulated through the central autonomic network (CAN)17. Morphological central CAN areas include forebrain regions (prefrontal and cingulate cortices; amygdala, hypothalamus), middle and posterior brain regions (nucleus tractus solitarii, nucleus ambiguus). The sympathovagal interaction from the CAN results in multiple instantaneous heart rate variations, i.e. the heart rate variability (HRV)15.
With regard to the heart, the momentary HRV is determined mainly by parasympathetic regulation based on fast metabolism of acetylcholine (sympathetic nerve effect occurs with latency). Thus, the HRV linear analysis provides information about breathing-related effects on the high-frequency band of the HRV (HF-HRV: 0.15-0.4 Hz) while low-frequency band (LF-HRV: 0.04-0.15 Hz) is influenced by contribution of sympathetic modulation mediated by baroreceptor activity. The respiratory-linked HRV indexed by HF-HRV is associated with several central regions such as prefrontal or cingulate cortex12,18,19. Thus, the objective neuroimaging methods underpin the assumption that RSA indexed by the HF-HRV reflects the ‘brain-heart’ bidirectional communication6,15.
The CAN-mediated HRV is characterized as a non-linear dynamical system with numerous mutual interactions and complexity14,15,20. In contrast, various pathological states are characterized by lower complexity as a non-linear characteristic of heart rate regulation resulting in deficient cardiac responses to many conditions21,22,23. Thus, the linear HRV analysis does not provide adequate information about complex cardiac dynamics. Therefore, novel non-linear methods assessing the qualitative features [e.g. heart rate complexity by symbolic dynamics, heart rate asymmetry (HRA)] have been applied in HRV analysis24.
Specifically, HRA represents the non-linear feature of the heart control associated with breathing cycle characterized by unequal duration of inhalation and exhalation25,26. Karmakar et al27 concluded that pharmacological parasympatholytic agent atropine or parasympathomimetic scopolamine influences asymmetric patterns, i.e. atropine reduces and scopolamine increases HRA. These studies confirm the link between vagal activity and HRA indices. In addition to breathing, the physiological mechanisms underlying the heart rate accelerations or decelerations can be modulated by other complex factors, such as baroreflex, chemoreflexes, hormones and others26.
The faster HRV oscillations expressing cardiac-linked modulation result in faster variations of consecutive heart beats, i.e. patterns with two similar variations (2LV%). The symbolic dynamics index 2LV% indicates the rate of occurrence of these patterns28,29. The 2LV% declines in response to different stressors (e.g. orthostasis or mental tasks); therefore, this index could be predominantly influenced by cardiac vagal regulatory effects28,30,31. Moreover, if these non-linear symbolic dynamics and HRA indices reflect predominantly cardiovagal activity, it should be correlated with the linear index HF-HRV determined by dominant vagal regulatory inputs. Our previous study revealed no significant relations between HF-HRV, 2LV% and HRA indices31. Therefore, these indices might offer different data about non-linear dynamics in heart rate vagal regulation that is independent on the RSA magnitude quantified by HF-HRV. This assumption, however, should be elucidated by further research.
The effect of breathing pattern: Importantly, the RSA is determined by breathing parameters such as respiratory rate or tidal volume, i.e. RSA magnitude is decreased in higher breathing rate and greater with increased tidal volume. Thus, tachypnoea reduces RSA, and bradypnoea with maximal volumes results in pronounced RSA magnitude14,32. The changes in parameters characterizing breathing patterns could influence cardiorespiratory conjunction33. In this context, slow breathing can affect the low-frequency band34. These alterations in breathing pattern characterize resting conditions as well as cognitive or emotional activity. Emotional activation was shown to be related to different respiratory activities characterized by augmented tidal volume associated with lower breathing rate resulting in high RSA magnitude, e.g. during meditation35. Thus, these psychological states associated with altered breathing pattern might affect RSA size32. Denver et al36 based on literature review reported that RSA magnitude was not related to breathing parameters. Several studies found no effect of breathing measures on the RSA37,38. Therefore, this field is still a matter of extensive discussion36.
Controlled breathing eliminates this controversial aspect; however, this pattern may not represent normal physiological cardiorespiratory interaction. Controlled breathing is associated with voluntary component involving cortical control of respiratory muscle activity accompanied by sympathetic excitation39. In cognitive task, the cardiorespiratory coupling may be affected by the motor cortical activation and sympathetic excitation40. The effects of voluntary and spontaneous breathing on HRV spectral analysis were reported to be similar in another study41.
The RSA variations represent differences in phasic pattern of vagal influences on heart rate32. Grossman and Taylor32 have referred to significant caveats: (i) breathing indices may affect the relation between RSA and parasympathetic heart rate regulation; (ii) RSA recording is influenced by physical activity resulting in individual cardiac-vagal modulation; and (iii) RSA amplitude is influenced by sympathetic modulation. Taken together, these issues should be considered in the correct interpretation of the RSA as a marker of parasympathetic regulation of the heart rate in psychophysiological research.
From pathophysiological perspective, the attenuated RSA reflecting autonomic dysregulation is considered a risk factor for later cardiovascular adverse outcomes42. Samuels43 referred to the stress aetiology related to cardiovascular diseases suggesting complex interaction between altered cortical/neural centres regulating cardiac autonomic activity (e.g. frontal lobe, anterior cingulate gyrus, insula, hypothalamus, limbic cortex, mesencephalic reticular formation and others) and peripheral factors (catecholamine toxicity, stress hormones and others) leading to heart injury.
Despite the fact that reduced RSA is a frequent finding in somatic diseases such as obesity or hypertension44,45, the past research was focused on the RSA as a potential psychophysiological marker indicating organism's flexibility and adaptability with emotions.
Respiratory sinus arrhythmia (RSA) in the context of emotional regulation
In the polyvagal theory6,46, the nucleus ambiguus plays an important role in the emotional and social behaviour. Specifically, efferent pathways from the nucleus ambiguus modulate the larynx as an organ important for expression of emotions46. In addition, the nucleus ambiguus is connected with cranial nerves involved in the emotional expression and vocalization23,46. Several studies showed the RSA link to affective regulation in people16,47,48,49,50. The RSA could be considered as an index of emotional regulation. However, it is important to note that cognitive control is important for emotions, termed as emotion regulation51. According to the neurovisceral theory, Thayer and Lane15 described the connection between mental and somatic functioning. Higher resting HRV (greater RSA amplitude) represents better cognitive control of emotions necessary for appropriate processing of negative effect. On the contrary, reduced RSA at rest can indicate maladaptive cognitive reflection to emotional conditions51,52. From this context, a prefrontal hypoactivity leading to subcortical excitation can result in the perseverative cognition (e.g. worry, rumination)51. Therefore, the deficiency in cognitive-emotional circuitry represented by cortical as well as subcortical areas could be connected with several mental disorders22,53.
The vagal reactivity is important, i.e. ‘vagal brake’ is withdrawn in response to a challenge, and parasympathetic inhibition in response to stress could reflect more flexible individual's adaptability to stress46,54. Taken together, the RSA magnitude (indexed by HF-HRV) at rest and during stress could provide important information related to physiological and behavioural flexibility of the organism including emotional regulation54,55,56,57,58. It is important to note that this assumption is not uniform, particularly in somatic and mental disorders. In somatic diseases, the resting HF-HRV may be substantially influenced by the effect of comorbidities, such as diabetes, hypertension and others. Specifically, lower HF-HRV was found in patients suffering from diabetes compared to non-diabetics, with significant inverse relationship between HF-HRV and fasting insulin and glycaemia59,60. Our previous studies revealed lower HF-HRV in diabetic, hypertensive and obese patients compared to controls44,45,61. The lower baseline cardiac vagal control indicates a lower functional reserve autonomic capacity to regulate stress response62. Therefore, the significance of resting HF-HRV in the presence of comorbid diseases is questionable.
In mental disorders, the robust vagal withdrawal to stress can be a non-specific index of emotional lability63. Our previous study demonstrated a reduced baseline RSA magnitude associated with higher RSA reactivity in the attention deficit hyperactivity disorder (ADHD) group compared to controls53. Thus, it remains unclear if these results are associated with the ADHD symptoms or these findings indicate clinically asymptomatic cardiac autonomic dysregulation to posture stress in ADHD patients53. The findings concerning the RSA reactivity in response to different stressors are controversial; and this area requires further research.
Developmental aspect: The development of the neural structures involved in the cardiac vagal control is important for social skills, behavioural state, adaptability and flexibility. Vagal myelinization is important for the newborns and the infants prosocial behaviour64. Further, the early childhood is a vulnerable age period for the emotion regulation65; and the RSA differences may indicate developmental differences66. In biopsychosocial developmental model, impulsive children with family and emotional support are socialized through de-escalation of arousal, positive reinforcement, and are protected from delinquency behaviour through appropriate emotional regulation mediated by vagus nerve. In contrast, risk children without family and emotional support are prone to later problems in behavioural and emotional domain due to ineffective vagal regulation of effects11. With regard to psychopathology, baseline RSA was similar between ADHD and controls at the age of 4-6 years67; however, vagal deficiency was observed in middle childhood and adolescence such as a period characterized by parasympathetic nervous system ‘online’11,68.
The puberty represents a specific period because of central nervous system developmental changes including prefrontal cortex16,69. McRae et al70 reported the brain regions of cognitive reappraisal for emotion regulation in various age periods ranged from 10 to 22 years. These authors observed linear age-related increases in the prefrontal cortex activity accompanied by better cognitive functioning important for emotional skills70. Further, older adults (55-65 yr) showed diminished prefrontal cortical activation associated with lower cognitive reappraisal of emotions in older adults71.
The physiological maturation of neurocardiac regulatory mechanisms should also be considered. For example, the maximal increase of cardiac vagal activity indexed by HF-HRV was found between 9 and 14 yr in the group of 5400 children72. Another study found HRV increase during the first decade reflecting a gradual development of the parasympathetic nervous system73. Our study revealed increase in RSA magnitude (indexed by HF-HRV and deep breathing test) indicating augmentation of cardiovagal activity in the group of 206 boys and girls aged 15-19 years. A systematic review summarized that HRV values are typically higher in younger adult participants with emphasis on the necessity of HRV standard values for individual age periods74. Processes responsible for age-related influences could involve maturation of central brain regions, changes in neurotransmitters, growth of the heart, receptor's level (sensitivity and density) and other unknown mechanisms75,76. It seems that the developmental process is important for RSA understanding in the emotional and cognitive regulation at the different age periods.
Respiratory sinus arrhythmia (RSA) in response to the acute cognitive/emotional stress
Porges56 suggested that stress could be specified by abnormal autonomic functioning characterized by decreased vagal modulation; thus, the RSA quantification might be used for assessment of stress response. RSA responses to different stressful stimuli showed large variability. Previous studies confirmed a parasympathetic decrease marked by RSA to cognitive stress31,77. However, other authors concluded that the two cognitive tasks had dissimilar effects on RSA reactivity78. While the continuous working memory task requiring high cognitive control had a substantial inhibitory effect on the parameters characterizing RSA, the perceptual attention task involving low cognitive control had a limited inhibitory effect on the RSA measures78. The intensity of cognitive control thus seems to be an important determinant of differential effects of cognitive tasks on RSA78. The literature shows large inconsistencies in the RSA responses to emotional tasks. In certain studies, specific emotional states produced an increase in RSA relative to a resting baseline, while others found RSA reduction or no RSA alterations in response to similar states47,79. For clinical implications, the RSA reactivity to stress could have important implications for specific conditions associated with affective regulation12.
Therefore, we aimed to show that RSA response could be different from cognitive and emotional stress. Ten healthy non-obese cases between 22 and 23 yr were examined in the special psychophysiological laboratory. The electrocardiography signal was recorded during the protocol: rest – mental arithmetic test (cognitive test) – rest – negative emotional stress (video clip with dental intervention) – rest (recovery phase). The duration of each period was six minutes suitable for short-term HRV analysis80. However, the participants were not instructed about the precise order of individual stressors to minimalize a potential impact of cognitive processing before the examination. The results displayed a distinct response pattern of the RSA indexed by HRV time parameter [root mean squared successive difference of RR intervals (rMSSD)] to different stressors: decreased vagal activity (significantly lower rMSSD) in response to cognitive test (arithmetic test), and increased RSA magnitude (significantly higher rMSSD) to negative emotional task. In addition, the HRV parameter returned to baseline values after the stress was over (unpublished results, Table). These results were in accordance with the studies which found a cardiac-linked parasympathetic decrease indexed by reduced RSA magnitude to cognitive stress indicating physiological adaptive response system31,57,81,82.
Table.
Effect of mental arithmetic test and negative emotion stress on the heart rate variability parameter rMSSD
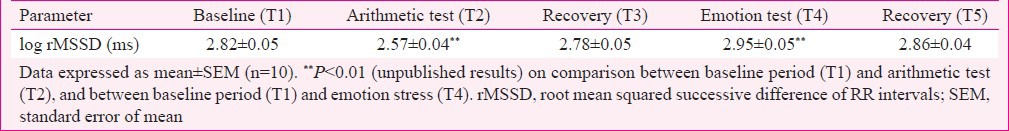
Our findings revealed an increase in RSA magnitude during emotional negative task in healthy students (unpublished data). We speculated that cognitive inhibitory strategies could be involved in the RSA increase to emotional stress: if RSA augmentation is associated with self-regulation, then cognitive reappraisal of negative emotional task should lead to RSA increase mediated through higher inhibition of the subcortical sympathoexcitatory circuits by prefrontal cortex83. Furthermore, different neurobiological and neurophysiological neural structures are involved in this distinct RSA response evoked by different stressors. In particular, dorsal subdivision of cingulate cortex is stimulated in cognitive regulation, and the ventral subdivision of anterior cingulate cortex plays a significant role in emotional regulation84. It seems that these findings can contribute to the understanding of RSA reactivity in emotional stress.
The stress reactivity is also influenced by age. Kudielka et al85 found reduced heart rate reactions in older people (60-76 yr) compared to younger adults (19-32 yr) and children (9-15 yr). Despite the fact that resting RSA could show two-year stability, the RSA reactivity is characterized by steady responses only in adult people86. In addition, while active cognitive stressors are accompanied by sympathetic control of the heart rate associated with a vagal withdrawal, the passive emotional stress is associated with increases in parasympathetic system due to potential immobilization effect6. The evaluation of such effects requires further systematic investigation.
Conclusion
Cardiac vagal function indexed by RSA may reflect activity of complex neural system responsible for adequate cognitive-affective regulation. High resting RSA amplitude associated with a greater withdrawal during stressors and subsequent recovery could represent a flexible physiological response system. It seems that RSA stress-linked reactivity depends on the type of stressors: while the RSA decreases to cognitive tasks indicating a vagal withdrawal, the RSA magnitude increases to emotional stimulus indicating a proper cortical-subcortical functioning, i.e. effective cognitive processing of emotional stimuli.
Acknowledgment
This work was supported by National Research Grant VEGA 1/0087/14, APVV-15-0075 and the project ‘Biomedical Center Martin’ (ITMS code: 26220220187); the project is co-financed from EU sources.
Footnotes
Conflicts of Interest: None.
References
- 1.Berntson GG, Bigger JT, Jr, Eckberg DL, Grossman P, Kaufmann PG, Malik M, et al. Heart rate variability: origins, methods, and interpretive caveats. Psychophysiology. 1997;34:623–48. doi: 10.1111/j.1469-8986.1997.tb02140.x. [DOI] [PubMed] [Google Scholar]
- 2.Yasuma F, Hayano J. Respiratory sinus arrhythmia: why does the heartbeat synchronize with respiratory rhythm? Chest. 2004;125:683–90. doi: 10.1378/chest.125.2.683. [DOI] [PubMed] [Google Scholar]
- 3.Costa-Silva JH, Zoccal DB, Machado BH. Glutamatergic antagonism in the NTS decreases post-inspiratory drive and changes phrenic and sympathetic coupling during chemoreflex activation. J Neurophysiol. 2010;103:2095–106. doi: 10.1152/jn.00802.2009. [DOI] [PubMed] [Google Scholar]
- 4.Cohen MA, Taylor JA. Short-term cardiovascular oscillations in man: measuring and modelling the physiologies. J Physiol. 2002;542(Pt 3):669–83. doi: 10.1113/jphysiol.2002.017483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ursino M, Magosso E. Role of short-term cardiovascular regulation in heart period variability: a modeling study. Am J Physiol Heart Circ Physiol. 2003;284:H1479–93. doi: 10.1152/ajpheart.00850.2002. [DOI] [PubMed] [Google Scholar]
- 6.Porges SW. The polyvagal theory: new insights into adaptive reactions of the autonomic nervous system. Cleve Clin J Med. 2009;76(Suppl 2):S86–90. doi: 10.3949/ccjm.76.s2.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Taylor EW, Jordan D, Coote JH. Central control of the cardiovascular and respiratory systems and their interactions in vertebrates. Physiol Rev. 1999;79:855–916. doi: 10.1152/physrev.1999.79.3.855. [DOI] [PubMed] [Google Scholar]
- 8.Berntson GG, Cacioppo JT, Grossman P. Whither vagal tone. Biol Psychol. 2007;74:295–300. doi: 10.1016/j.biopsycho.2006.08.006. [DOI] [PubMed] [Google Scholar]
- 9.Myslivecek J, Rícný J, Palkovits M, Kvetnanský R. The effects of short-term immobilization stress on muscarinic receptors, beta-adrenoceptors, and adenylyl cyclase in different heart regions. Ann N Y Acad Sci. 2004;1018:315–22. doi: 10.1196/annals.1296.038. [DOI] [PubMed] [Google Scholar]
- 10.Ritz T. Studying noninvasive indices of vagal control: the need for respiratory control and the problem of target specificity. Biol Psychol. 2009;80:158–68. doi: 10.1016/j.biopsycho.2008.08.003. [DOI] [PubMed] [Google Scholar]
- 11.Beauchaine TP, Gatzke-Kopp L, Mead HK. Polyvagal theory and developmental psychopathology: emotion dysregulation and conduct problems from preschool to adolescence. Biol Psychol. 2007;74:174–84. doi: 10.1016/j.biopsycho.2005.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Thayer JF, Ahs F, Fredrikson M, Sollers JJ, 3rd, Wager TD. A meta-analysis of heart rate variability and neuroimaging studies: implications for heart rate variability as a marker of stress and health. Neurosci Biobehav Rev. 2012;36:747–56. doi: 10.1016/j.neubiorev.2011.11.009. [DOI] [PubMed] [Google Scholar]
- 13.Fortunato CK, Gatzke-Kopp LM, Ram N. Associations between respiratory sinus arrhythmia reactivity and internalizing and externalizing symptoms are emotion specific. Cogn Affect Behav Neurosci. 2013;13:238–51. doi: 10.3758/s13415-012-0136-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Quintana DS, Heathers JA. Considerations in the assessment of heart rate variability in biobehavioral research. Front Psychol. 2014;5:805. doi: 10.3389/fpsyg.2014.00805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Thayer JF, Lane RD. A model of neurovisceral integration in emotion regulation and dysregulation. J Affect Disord. 2000;61:201–16. doi: 10.1016/s0165-0327(00)00338-4. [DOI] [PubMed] [Google Scholar]
- 16.Thayer JF, Lane RD. Claude bernard and the heart-brain connection: further elaboration of a model of neurovisceral integration. Neurosci Biobehav Rev. 2009;33:81–8. doi: 10.1016/j.neubiorev.2008.08.004. [DOI] [PubMed] [Google Scholar]
- 17.Benarroch EE. The central autonomic network: functional organization, dysfunction, and perspective. Mayo Clin Proc. 1993;68:988–1001. doi: 10.1016/s0025-6196(12)62272-1. [DOI] [PubMed] [Google Scholar]
- 18.Napadow V, Dhond R, Conti G, Makris N, Brown EN, Barbieri R. Brain correlates of autonomic modulation: combining heart rate variability with fMRI. Neuroimage. 2008;42:169–77. doi: 10.1016/j.neuroimage.2008.04.238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lane RD, McRae K, Reiman EM, Chen K, Ahern GL, Thayer JF. Neural correlates of heart rate variability during emotion. Neuroimage. 2009;44:213–22. doi: 10.1016/j.neuroimage.2008.07.056. [DOI] [PubMed] [Google Scholar]
- 20.Friedman BH. An autonomic flexibility-neurovisceral integration model of anxiety and cardiac vagal tone. Biol Psychol. 2007;74:185–99. doi: 10.1016/j.biopsycho.2005.08.009. [DOI] [PubMed] [Google Scholar]
- 21.Baumert M, Baier V, Haueisen J, Wessel N, Meyerfeldt U, Schirdewan A, et al. Forecasting of life threatening arrhythmias using the compression entropy of heart rate. Methods Inf Med. 2004;43:202–6. [PubMed] [Google Scholar]
- 22.Tonhajzerova I, Ondrejka I, Javorka K, Turianikova Z, Farsky I, Javorka M. Cardiac autonomic regulation is impaired in girls with major depression. Prog Neuropsychopharmacol Biol Psychiatry. 2010;34:613–8. doi: 10.1016/j.pnpbp.2010.02.023. [DOI] [PubMed] [Google Scholar]
- 23.Tonhajzerova I, Ondrejka I, Turianikova Z, Javorka K, Calkovska A, Javorka M. Heart rate variability: an index of the brain-heart interaction. In: Yamada T, editor. Tachycardia. Rijeka: InTech; 2012. pp. 185–202. [Google Scholar]
- 24.Voss A, Schulz S, Schroeder R, Baumert M, Caminal P. Methods derived from nonlinear dynamics for analysing heart rate variability. Philos Trans A Math Phys Eng Sci. 2009;367:277–96. doi: 10.1098/rsta.2008.0232. [DOI] [PubMed] [Google Scholar]
- 25.Porta A, Casali KR, Casali AG, Gnecchi-Ruscone T, Tobaldini E, Montano N, et al. Temporal asymmetries of short-term heart period variability are linked to autonomic regulation. Am J Physiol Regul Integr Comp Physiol. 2008;295:R550–7. doi: 10.1152/ajpregu.00129.2008. [DOI] [PubMed] [Google Scholar]
- 26.Piskorski J, Guzik P. Asymmetric properties of long-term and total heart rate variability. Med Biol Eng Comput. 2011;49:1289–97. doi: 10.1007/s11517-011-0834-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Karmakar C, Khandoker A, Palaniswami M. Investigating the changes in heart rate asymmetry (HRA) with perturbation of parasympathetic nervous system. Australas Phys Eng Sci Med. 2012;35:465–74. doi: 10.1007/s13246-012-0173-x. [DOI] [PubMed] [Google Scholar]
- 28.Porta A, Gnecchi-Ruscone T, Tobaldini E, Guzzetti S, Furlan R, Malliani A, et al. Symbolic analysis of short-term heart period variability during graded head-up tilt. Comput Cardiol. 2006;33:109–12. [Google Scholar]
- 29.Porta A, Faes L, Masé M, D’Addio G, Pinna GD, Maestri R, et al. An integrated approach based on uniform quantization for the evaluation of complexity of short-term heart period variability: application to 24 h holter recordings in healthy and heart failure humans. Chaos. 2007;17:015117. doi: 10.1063/1.2404630. [DOI] [PubMed] [Google Scholar]
- 30.Porta A, Guzzetti S, Montano N, Furlan R, Pagani M, Malliani A, et al. Entropy, entropy rate, and pattern classification as tools to typify complexity in short heart period variability series. IEEE Trans Biomed Eng. 2001;48:1282–91. doi: 10.1109/10.959324. [DOI] [PubMed] [Google Scholar]
- 31.Visnovcova Z, Mestanik M, Javorka M, Mokra D, Gala M, Jurko A, et al. Complexity and time asymmetry of heart rate variability are altered in acute mental stress. Physiol Meas. 2014;35:1319–34. doi: 10.1088/0967-3334/35/7/1319. [DOI] [PubMed] [Google Scholar]
- 32.Grossman P, Taylor EW. Toward understanding respiratory sinus arrhythmia: relations to cardiac vagal tone, evolution and biobehavioral functions. Biol Psychol. 2007;74:263–85. doi: 10.1016/j.biopsycho.2005.11.014. [DOI] [PubMed] [Google Scholar]
- 33.Porges SW. A phylogenetic journey through the vague and ambiguous Xth cranial nerve: a commentary on contemporary heart rate variability research. Biol Psychol. 2007;74:301–7. doi: 10.1016/j.biopsycho.2006.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wang YP, Kuo TB, Lai CT, Chu JW, Yang CC. Effects of respiratory time ratio on heart rate variability and spontaneous baroreflex sensitivity. J Appl Physiol (1985) 2013;115:1648–55. doi: 10.1152/japplphysiol.00163.2013. [DOI] [PubMed] [Google Scholar]
- 35.Krygier JR, Heathers JA, Shahrestani S, Abbott M, Gross JJ, Kemp AH. Mindfulness meditation, well-being, and heart rate variability: a preliminary investigation into the impact of intensive vipassana meditation. Int J Psychophysiol. 2013;89:305–13. doi: 10.1016/j.ijpsycho.2013.06.017. [DOI] [PubMed] [Google Scholar]
- 36.Denver JW, Reed SF, Porges SW. Methodological issues in the quantification of respiratory sinus arrhythmia. Biol Psychol. 2007;74:286–94. doi: 10.1016/j.biopsycho.2005.09.00. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rottenberg J, Wilhelm FH, Gross JJ, Gotlib IH. Vagal rebound during resolution of tearful crying among depressed and nondepressed individuals. Psychophysiology. 2003;40:1–6. doi: 10.1111/1469-8986.00001. [DOI] [PubMed] [Google Scholar]
- 38.Ritz T, Thöns M, Dahme B. Increases in total respiratory resistance during forehead temperature stimulation. Biol Psychol. 2000;55:119–35. doi: 10.1016/s0301-0511(00)00075-2. [DOI] [PubMed] [Google Scholar]
- 39.Larsen PD, Tzeng YC, Sin PY, Galletly DC. Respiratory sinus arrhythmia in conscious humans during spontaneous respiration. Respir Physiol Neurobiol. 2010;174:111–8. doi: 10.1016/j.resp.2010.04.021. [DOI] [PubMed] [Google Scholar]
- 40.Zhang J, Yu X, Xie D. Effects of mental tasks on the cardiorespiratory synchronization. Respir Physiol Neurobiol. 2010;170:91–5. doi: 10.1016/j.resp.2009.11.003. [DOI] [PubMed] [Google Scholar]
- 41.Patwardhan AR, Evans JM, Bruce EN, Eckberg DL, Knapp CF. Voluntary control of breathing does not alter vagal modulation of heart rate. J Appl Physiol (1985) 1995;78:2087–94. doi: 10.1152/jappl.1995.78.6.2087. [DOI] [PubMed] [Google Scholar]
- 42.Masi CM, Hawkley LC, Rickett EM, Cacioppo JT. Respiratory sinus arrhythmia and diseases of aging: obesity, diabetes mellitus, and hypertension. Biol Psychol. 2007;74:212–23. doi: 10.1016/j.biopsycho.2006.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Samuels MA. The brain-heart connection. Circulation. 2007;116:77–84. doi: 10.1161/CIRCULATIONAHA.106.678995. [DOI] [PubMed] [Google Scholar]
- 44.Tonhajzerova I, Javorka M, Trunkvalterova Z, Chroma O, Javorkova J, Lazarova Z, et al. Cardio-respiratory interaction and autonomic dysfunction in obesity. J Physiol Pharmacol. 2008;59(Suppl 6):709–18. [PubMed] [Google Scholar]
- 45.Havlicekova Z, Tonhajzerova I, Jurko A, Jr, Jesenak M, Durdik P, Nosal S, et al. Cardiac autonomic control in adolescents with primary hypertension. Eur J Med Res. 2009;14(Suppl 4):101–3. doi: 10.1186/2047-783X-14-S4-101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Porges SW. Orienting in a defensive world: mammalian modifications of our evolutionary heritage. A polyvagal theory. Psychophysiology. 1995;32:301–18. doi: 10.1111/j.1469-8986.1995.tb01213.x. [DOI] [PubMed] [Google Scholar]
- 47.Frazier TW, Strauss ME, Steinhauer SR. Respiratory sinus arrhythmia as an index of emotional response in young adults. Psychophysiology. 2004;41:75–83. doi: 10.1046/j.1469-8986.2003.00131.x. [DOI] [PubMed] [Google Scholar]
- 48.Oveis C, Cohen AB, Gruber J, Shiota MN, Haidt J, Keltner D. Resting respiratory sinus arrhythmia is associated with tonic positive emotionality. Emotion. 2009;9:265–70. doi: 10.1037/a0015383. [DOI] [PubMed] [Google Scholar]
- 49.Kreibig SD. Autonomic nervous system activity in emotion: a review. Biol Psychol. 2010;84:394–421. doi: 10.1016/j.biopsycho.2010.03.010. [DOI] [PubMed] [Google Scholar]
- 50.Schwerdtfeger AR, Scheel SM. Self-esteem fluctuations and cardiac vagal control in everyday life. Int J Psychophysiol. 2012;83:328–35. doi: 10.1016/j.ijpsycho.2011.11.016. [DOI] [PubMed] [Google Scholar]
- 51.Park G, Thayer JF. From the heart to the mind: cardiac vagal tone modulates top-down and bottom-up visual perception and attention to emotional stimuli. Front Psychol. 2014;5:278. doi: 10.3389/fpsyg.2014.00278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Gross JJ, Thompson RA. Emotion regulation: conceptual foundations. In: Gros JJ, editor. Handbook of emotion regulation. 1st ed. New York: Guilford Press; 2011. pp. 3–24. [Google Scholar]
- 53.Tonhajzerova I, Ondrejka I, Adamik P, Hruby R, Javorka M, Trunkvalterova Z, et al. Changes in the cardiac autonomic regulation in children with attention deficit hyperactivity disorder (ADHD) Indian J Med Res. 2009;130:44–50. [PubMed] [Google Scholar]
- 54.Gentzler AL, Santucci AK, Kovacs M, Fox NA. Respiratory sinus arrhythmia reactivity predicts emotion regulation and depressive symptoms in at-risk and control children. Biol Psychol. 2009;82:156–63. doi: 10.1016/j.biopsycho.2009.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Blandon AY, Calkins SD, Keane SP, O’Brien M. Individual differences in trajectories of emotion regulation processes: the effects of maternal depressive symptomatology and children's physiological regulation. Dev Psychol. 2008;44:1110–23. doi: 10.1037/0012-1649.44.4.1110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Porges SW. Cardiac vagal tone: a physiological index of stress. Neurosci Biobehav Rev. 1995;19:225–33. doi: 10.1016/0149-7634(94)00066-a. [DOI] [PubMed] [Google Scholar]
- 57.Porges SW. The polyvagal perspective. Biol Psychol. 2007;74:116–43. doi: 10.1016/j.biopsycho.2006.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Calkins SD, Graziano PA, Keane SP. Cardiac vagal regulation differentiates among children at risk for behavior problems. Biol Psychol. 2007;74:144–53. doi: 10.1016/j.biopsycho.2006.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Liao D, Cai J, Brancati FL, Folsom A, Barnes RW, Tyroler HA, et al. Association of vagal tone with serum insulin, glucose, and diabetes mellitus - The ARIC study. Diabetes Res Clin Pract. 1995;30:211–21. doi: 10.1016/0168-8227(95)01190-0. [DOI] [PubMed] [Google Scholar]
- 60.Singh JP, Larson MG, O’Donnell CJ, Wilson PF, Tsuji H, Lloyd-Jones DM, et al. Association of hyperglycemia with reduced heart rate variability (the framingham heart study) Am J Cardiol. 2000;86:309–12. doi: 10.1016/s0002-9149(00)00920-6. [DOI] [PubMed] [Google Scholar]
- 61.Javorka M, Trunkvalterova Z, Tonhajzerova I, Javorkova J, Javorka K, Baumert M. Short-term heart rate complexity is reduced in patients with type 1 diabetes mellitus. Clin Neurophysiol. 2008;119:1071–81. doi: 10.1016/j.clinph.2007.12.017. [DOI] [PubMed] [Google Scholar]
- 62.Rash JA, Aguirre-Camacho A. Attention-deficit hyperactivity disorder and cardiac vagal control: a systematic review. Atten Defic Hyperact Disord. 2012;4:167–77. doi: 10.1007/s12402-012-0087-1. [DOI] [PubMed] [Google Scholar]
- 63.Beauchaine T. Vagal tone, development, and Gray's motivational theory: toward an integrated model of autonomic nervous system functioning in psychopathology. Dev Psychopathol. 2001;13:183–214. doi: 10.1017/s0954579401002012. [DOI] [PubMed] [Google Scholar]
- 64.Porges SW, Furman SA. The early development of the autonomic nervous system provides a neural platform for social behavior: a polyvagal perspective. Infant Child Dev. 2011;20:106–18. doi: 10.1002/icd.688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Blair C. School readiness. Integrating cognition and emotion in a neurobiological conceptualization of children's functioning at school entry. Am Psychol. 2002;57:111–27. doi: 10.1037//0003-066x.57.2.111. [DOI] [PubMed] [Google Scholar]
- 66.Beauchaine TP, Gatzke-Kopp LM. Instantiating the multiple levels of analysis perspective in a program of study on externalizing behavior. Dev Psychopathol. 2012;24:1003–18. doi: 10.1017/S0954579412000508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Crowell SE, Beauchaine TP, Gatzke-Kopp L, Sylvers P, Mead H, Chipman-Chacon J. Autonomic correlates of attention-deficit/hyperactivity disorder and oppositional defiant disorder in preschool children. J Abnorm Psychol. 2006;115:174–8. doi: 10.1037/0021-843X.115.1.174. [DOI] [PubMed] [Google Scholar]
- 68.Crowell SE, Beauchaine TP, McCauley E, Smith CJ, Stevens AL, Sylvers P. Psychological, autonomic, and serotonergic correlates of parasuicide among adolescent girls. Dev Psychopathol. 2005;17:1105–27. doi: 10.1017/s0954579405050522. [DOI] [PubMed] [Google Scholar]
- 69.Yang TT, Simmons AN, Matthews SC, Tapert SF, Bischoff-Grethe A, Frank GK, et al. Increased amygdala activation is related to heart rate during emotion processing in adolescent subjects. Neurosci Lett. 2007;428:109–14. doi: 10.1016/j.neulet.2007.09.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.McRae K, Gross JJ, Weber J, Robertson ER, Sokol-Hessner P, Ray RD, et al. The development of emotion regulation: an fMRI study of cognitive reappraisal in children, adolescents and young adults. Soc Cogn Affect Neurosci. 2012;7:11–22. doi: 10.1093/scan/nsr093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Opitz PC, Rauch LC, Terry DP, Urry HL. Prefrontal mediation of age differences in cognitive reappraisal. Neurobiol Aging. 2012;33:645–55. doi: 10.1016/j.neurobiolaging.2010.06.004. [DOI] [PubMed] [Google Scholar]
- 72.Galeev AR, Igisheva LN, Kazin EM. Heart rate variability in healthy six-to sixteen-year-old children. Hum Physiol. 2002;28:428–32. [PubMed] [Google Scholar]
- 73.Silvetti MS, Drago F, Ragonese P. Heart rate variability in healthy children and adolescents is partially related to age and gender. Int J Cardiol. 2001;81:169–74. doi: 10.1016/s0167-5273(01)00537-x. [DOI] [PubMed] [Google Scholar]
- 74.Nunan D, Sandercock GR, Brodie DA. A quantitative systematic review of normal values for short-term heart rate variability in healthy adults. Pacing Clin Electrophysiol. 2010;33:1407–17. doi: 10.1111/j.1540-8159.2010.02841.x. [DOI] [PubMed] [Google Scholar]
- 75.Tonhajzerová I, Javorka K, Petrásková M. Development of the parameters of heart rate variability in young individuals aged 15-19 years. Cesk Pediatr. 1999;54:421–4. [Google Scholar]
- 76.Tonhajzerová I, Javorka K, Javorka M, Petrásková M. Cardiovascular autonomic nervous system tests: reference values in young people (15-19 years) and influence of age and gender. Clin Physiol Funct Imaging. 2002;22:398–403. doi: 10.1046/j.1475-097x.2002.00449.x. [DOI] [PubMed] [Google Scholar]
- 77.Tonhajzerová I, Javorka K, Petrásková M. Changes of heart rate variability (HRV) during mental load. Cesk Pediatr. 2000;55:562–7. [Google Scholar]
- 78.Overbeek TJ, van Boxtel A, Westerink JH. Respiratory sinus arrhythmia responses to cognitive tasks: effects of task factors and RSA indices. Biol Psychol. 2014;99:1–14. doi: 10.1016/j.biopsycho.2014.02.006. [DOI] [PubMed] [Google Scholar]
- 79.Overbeek TJ, van Boxtel A, Westerink JH. Respiratory sinus arrhythmia responses to induced emotional states: effects of RSA indices, emotion induction method, age, and sex. Biol Psychol. 2012;91:128–41. doi: 10.1016/j.biopsycho.2012.05.011. [DOI] [PubMed] [Google Scholar]
- 80.Heart rate variability: standards of measurement, physiological interpretation and clinical use. Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Circulation. 1996;93:1043–65. [PubMed] [Google Scholar]
- 81.Niizeki K, Saitoh T. Incoherent oscillations of respiratory sinus arrhythmia during acute mental stress in humans. Am J Physiol Heart Circ Physiol. 2012;302:H359–67. doi: 10.1152/ajpheart.00746.2011. [DOI] [PubMed] [Google Scholar]
- 82.Takamoto K, Hori E, Urakawa S, Katayama M, Nagashima Y, Yada Y, et al. Thermotherapy to the facial region in and around the eyelids altered prefrontal hemodynamic responses and autonomic nervous activity during mental arithmetic. Psychophysiology. 2013;50:35–47. doi: 10.1111/j.1469-8986.2012.01488.x. [DOI] [PubMed] [Google Scholar]
- 83.Butler EA, Wilhelm FH, Gross JJ. Respiratory sinus arrhythmia, emotion, and emotion regulation during social interaction. Psychophysiology. 2006;43:612–22. doi: 10.1111/j.1469-8986.2006.00467.x. [DOI] [PubMed] [Google Scholar]
- 84.Simpson JR, Jr, Snyder AZ, Gusnard DA, Raichle ME. Emotion-induced changes in human medial prefrontal cortex: I. During cognitive task performance. Proc Natl Acad Sci U S A. 2001;98:683–7. doi: 10.1073/pnas.98.2.683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Kudielka BM, Buske-Kirschbaum A, Hellhammer DH, Kirschbaum C. Differential heart rate reactivity and recovery after psychosocial stress (TSST) in healthy children, younger adults, and elderly adults: the impact of age and gender. Int J Behav Med. 2004;11:116–21. doi: 10.1207/s15327558ijbm1102_8. [DOI] [PubMed] [Google Scholar]
- 86.El-Sheikh M. Stability of respiratory sinus arrhythmia in children and young adolescents: a longitudinal examination. Dev Psychobiol. 2005;46:66–74. doi: 10.1002/dev.20036. [DOI] [PubMed] [Google Scholar]


