ABSTRACT
Objectives
We sought to determine whether disease representation in the Cochrane Database of Systematic Reviews (CDSR) reflects disease burden, measured by the Global Burden of Disease (GBD) Study as disability-adjusted life-years (DALYs).
Materials and Methods
Two investigators performed independent assessment of ten men’s health and urologic diseases (MHUDs) in CDSR for systematic review and protocol representation, which were compared with percentage of total 2010 DALYs for the ten conditions. Data were analyzed for correlation using Spearman rank analysis.
Results
Nine of ten MHUDs were represented by at least one CDSR review. There was a poor and statistically insignificant positive correlation between CDSR representation and disease burden (rho = 0.42, p = 0.23). CDSR representation was aligned with disease burden for three conditions, greater than disease burden for one condition, and less than disease burden for six conditions.
Conclusions
These results yield high-quality estimates to inform future research prioritization for MHUDs. While prioritization processes are complex and multi-faceted, disease burden should be strongly considered. Awareness of research priority setting has the potential to minimize research disparities on a global scale.
Keywords: Men’s Health; Urologic Diseases; Neoplasms; Infertility, Male
INTRODUCTION
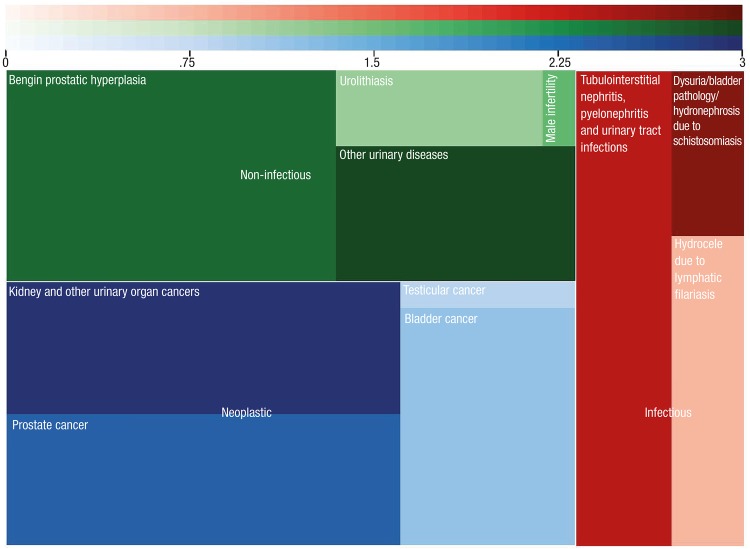
In order to achieve effective clinical research, scarce research funds must be distributed to appropriate diseases in order to maximize health benefits to the represented population. Systematic approaches to inform research prioritization include identifying and prioritizing research questions, recognizing existing research, and setting goals for primary research (1, 2). A derivative of this approach is to value major diseases, injuries, and risk factors based on their burden to society (3). Spearheaded by the Institute for Health Metrics and Evaluation (IHME), the Global Burden of Disease (GBD) 2010 Study estimates the burden of 291 diseases and injuries across 187 countries from 1990 to 2010 (4, 5). The metric of disability-adjusted life years (DALYs), in which 1 DALY is equivalent to 1 year of healthy life lost, allows for descriptive global epidemiology of a wide array of disease states. The following ten men’s health and urologic diseases (MHUDs) were studied by GBD on the basis of prevalence, common case definitions, and data availability: tubulointerstitial nephritis, pyelonephritis, and urinary tract infections; kidney and other urinary organ cancers; urolithiasis; male infertility; benign prostatic hyperplasia; prostate cancer; testicular cancer; hydrocele due to lymphatic filariasis; dysuria/bladder pathology/hydronephrosis due to schistosomiasis; and bladder cancer (Figure-1).
Figure 1. Square pie chart representing percent of total DALY for ten men’s health and urologic diseases; area of each square/rectangle represents percentage of total burden.
green = non-infectious conditions, red = infectious conditions, and blue = neoplastic conditions
Systematic reviews are the cornerstone of evidence-based medicine, yet few efforts have been made to assess whether the prioritization of systematic reviews reflect global disease burden (6). The Cochrane Database of Systematic Reviews (CDSR) produces systematic reviews and protocols (published proposals for future systematic reviews) across all medical specialties as well as health systems, public health, and child development. Cochrane systematic reviews undergo exhaustive editorial processing, are more methodologically rigorous, and are updated more frequently than non-Cochrane reviews and paper-based journals (7, 8). Prior studies have evaluated the association between broad categories of disease burden with randomized trials and Cochrane systematic reviews (9-12). This study will assess whether the CDSR representation of ten MHUDs corresponds to GBD 2010 disability estimates.
MATERIALS AND METHODS
ICD-10 code definitions for the ten MHUDs have been previously published and were used to generate search terms, which were entered into the “title, abstract, keywords” CDSR search function (5, 13). Systematic reviews and protocols were considered to determine MHUD representation in CDSR, according to abstract subject content. Online publication date, the number of studies included in each systematic review, and the particular Cochrane review group that published the review or protocol were collected.
Two authors (T.O and H.P.) collected data independently during February 2015. DALY metrics for each of the ten MHUDs, expressed as percentages of total DALY’s of all 291 conditions measured in GBD 2010, were obtained from the GBD Compare interactive time plot, available at <http://viz.healthmetricsandevaluation.org/gbd-compare/>. Spearman rank correlation analysis was performed to assess statistical dependence between CDSR representation and disease burden. Rho, a coefficient ranging from-1 (strong negative correlation) to +1 (strong positive correlation), is interpreted with a two-tailed p-value. A line-of-best-fit was also generated between CDSR representation and % of total DALYs.
As this study did not involve human subjects, institutional review board approval was not necessary.
RESULTS
Nine of the ten MHUD conditions studied in GBD 2010 were represented by at least one systematic review. A total of 116 systematic reviews and protocols published by nine Cochrane review groups represented the ten MHUDs (Supporting Tables 1 and 2 for included and excluded titles, respectively). The majority of reviews and protocols covered tubulointerstitial nephritis, pyelonephritis, and urinary tract infections (n=46). Hydrocele due to lymphatic filariasis had no representation in CDSR. Of the ten MHUDs, benign prostatic hyperplasia had the greatest global disease burden (0.2%) while male infertility had the lowest (0.007%) Table-1.
Supporting Table 1.
| Injury or Trauma | Review (R) or Protocol (P) Title | Cochrane Group | Number of Studies | Year of Online Publication |
|---|---|---|---|---|
| Tubulo-interstitial nephritis, pyelonephritis, and urinary tract infections | Antibiotics for acute pyelonephritis in children (R) | Renal Group | 27 | 2007 |
| Antibiotics for asymptomatic bacteriuria in pregnancy (R) | Pregnancy and Childbirth Group | 14 | 2007 | |
| Treatments for symptomatic urinary tract infections during pregnancy (R) | Pregnancy and Childbirth Group | 10 | 2011 | |
| Duration of treatment for asymptomatic bacteriuria during pregnancy (R) | Pregnancy and Childbirth Group | 13 | 2011 | |
| Routine blood cultures in the management of pyelonephritis in pregnancy for improving outcomes (R) | Renal Group | 0 | 2015 | |
| Procalcitonin , C-reactive protein , and erythrocyte sedimentation rate for the diagnosis of acute pyelonephritis in children (R) | Renal Group | 17 | 2015 | |
| Duration of antibacterial treatment for uncomplicated urinary tract infection in women (R) | Renal Group | 32 | 2005 | |
| Interventions for preventing recurrent urinary tract infection during pregnancy (R) | Pregnancy and Childbirth Group | 1 | 2012 | |
| Long-term antibiotics for preventing recurrent urinary tract infection in children (R) | Renal Group | 12 | 2011 | |
| Treatments for symptomatic urinary tract infections during pregnancy (R) | Pregnancy and Childbirth Group | 10 | 2011 | |
| Prophylactic antibiotics to reduce the risk of urinary tract infections after urodynamic studies (R) | Incontinence Group | 9 | 2012 | |
| Types of indwelling urethral catheters for short-term catheterization in hospitalized adults (R) | Incontinence Group | 26 | 2014 | |
| Antibiotics for treating lower urinary tract infection in children (R) | Renal Group | 16 | 2012 | |
| Methenamine hippurate for preventing urinary tract infections (R) | Renal Group | 13 | 2012 | |
| Estrogens for preventing recurrent urinary tract infection in postmenopausal women (R) | Renal Group | 9 | 2008 | |
| Short versus standard duration oral antibiotic therapy for acute urinary tract infection in children (R) | Renal Group | 10 | 2003 | |
| Urinary catheter policies for long-term bladder drainage (R) | Incontinence Group | 8 | 2012 | |
| Antimicrobial agents for treating uncomplicated urinary tract infection in women (R) | Renal Group | 21 | 2010 | |
| Modes of administration of antibiotics for symptomatic severe urinary tract infections (R) | Renal Group | 15 | 2007 | |
| Antibiotic duration for treating uncomplicated , symptomatic lower urinary tract infections in elderly women (R) | Renal Group | 15 | 2008 | |
| Antibiotic prophylaxis for short-term catheter bladder drainage in adults (R) | Incontinence Group | 6 | 2013 | |
| Cranberries for treating urinary tract infections (R) | Renal Group | 0 | 1998 | |
| Antibiotics for preventing recurrent urinary tract infection in non-pregnant women (R) | Renal Group | 19 | 2004 | |
| Cranberries for preventing urinary tract infections (R) | Renal Group | 24 | 2012 | |
| Routine neonatal circumcision for the prevention of urinary tract infections in infancy (R) | Neonatal Group | 0 | 2012 | |
| Urinary catheter policies for short-term bladder drainage in adults (R) | Incontinence Group | 17 | 2005 | |
| Intermittent catheterization for long-term bladder management (R) | Incontinence Group | 31 | 2014 | |
| Antibiotic prophylaxis for transrectal prostate biopsy (R) | Prostatic Diseases and Urologic Cancers Group | 19 | 2011 | |
| Short term urinary catheter policies following urogenital surgery in adults (R) | Incontinence Group | 39 | 2006 | |
| Washout policies in long-term indwelling urinary catheterization in adults (R) | Incontinence Group | 5 | 2010 | |
| Routine intraoperative ureteric stenting for kidney transplant recipients (R) | Renal Group | 7 | 2013 | |
| Interventions for primary vesicoureteric reflux (R) | Renal Group | 20 | 2011 | |
| Types of indwelling urinary catheters for long-term bladder drainage in adults (R) | Incontinence Group | 3 | 2012 | |
| Laser prostatectomy for benign prostatic obstruction (R) | Prostatic Diseases and Urologic Cancers Group | 20 | 2000 | |
| Quinolones for uncomplicated acute cystitis in women (R) | Renal Group | 11 | 2006 | |
| Drugs for treatment of urinary retention after surgery in adults (R) | Incontinence Group | 7 | 2010 | |
| Indwelling bladder catheterization as part of intraoperative and postoperative care for caesarean section (R) | Pregnancy and Childbirth Group | 5 | 2014 | |
| Dietary interventions for preventing complications in idiopathic hypercalciuria (R) | Renal Group | 5 | 2014 | |
| Interventions for covert bacteriuria in children (R) | Renal Group | 3 | 2012 | |
| Pharmacological interventions for preventing complications in idiopathic hypercalciuria (R) | Renal Group | 5 | 2009 | |
| Different antibiotic regimens for treating asymptomatic bacteriuria in pregnancy (R) | Pregnancy and Childbirth Group | 5 | 2010 | |
| Urinary alkalization for uncomplicated urinary tract infection (P) | Renal Group | N/A | 2013 | |
| Dimercaptosuccinic acid scan versus ultrasound in screening for vesicoureteral reflux among children with urinary tract infections (P) | Renal Group | N/A | 2013 | |
| Chinese herbal medicine for treating recurrent urinary tract infections in women (P) | Renal Group | N/A | 2013 | |
| Probiotics for preventing urinary tract infection in people with neuropathic bladder (P) | Renal Group | N/A | 2013 | |
| Probiotics for preventing urinary tract infections in adults and children (P) | Renal Group | N/A | 2010 | |
| Kidney and other urinary organ cancers | Targeted therapy for advanced renal cell carcinoma (R) | Prostatic Diseases and Urologic Cancers Group | 25 | 2008 |
| Immunotherapy for advanced renal cell cancer (R) | Prostatic Diseases and Urologic Cancers Group | 37 | 2004 | |
| Surgical management of localized renal cell carcinoma (R) | Prostatic Diseases and Urologic Cancers Group | 0 | 2010 | |
| Surgical management for upper urinary tract transitional cell carcinoma (R) | Prostatic Diseases and Urologic Cancers Group | 1 | 2011 | |
| Urolithiasis | Extracorporeal shock wave lithotripsy (ESWL ) versus percutaneous nephrolithotomy (PCNL ) or retrograde intrarenal surgery (RIRS ) for kidney stones (R) | Renal Group | 5 | 2014 |
| Dietary interventions for preventing complications in idiopathic hypercalciuria (R) | Renal Group | 5 | 2014 | |
| Extracorporeal shock wave lithotripsy (ESWL ) versus ureteroscopic management for ureteric calculi (R) | Renal Group | 7 | 2012 | |
| Pharmacological interventions for preventing complications in idiopathic hypercalciuria (R) | Renal Group | 5 | 2009 | |
| Fluids and diuretics for acute ureteric colic (R) | Renal Group | 2 | 2012 | |
| Water for preventing urinary stones (R) | Renal Group | 1 | 2012 | |
| Alpha-blockers as medical expulsive therapy for ureteral stones (R) | Renal Group | 32 | 2014 | |
| Percussion , diuresis , and inversion therapy for the passage of lower pole kidney stones following shock wave lithotripsy (R) | Renal Group | 2 | 2013 | |
| Analgesia for patients undergoing shockwave lithotripsy for urinary stones (P) | Renal Group | N/A | 2012 | |
| Interventions for treating urinary stones in children (P) | Renal Group | N/A | 2013 | |
| Male infertility | Intra-uterine insemination for male subfertility (R) | Menstrual Disorders and Subfertility Group | 8 | 2007 |
| Antioxidants for male subfertility (R) | Menstrual Disorders and Subfertility Group | 48 | 2014 | |
| Surgery or embolization for varicoceles in subfertile men (R) | Menstrual Disorders and Subfertility Group | 10 | 2012 | |
| Regular (ICSI ) versus ultra-high magnification (IMSI ) sperm selection for assisted reproduction (R) | Menstrual Disorders and Subfertility Group | 9 | 2013 | |
| Intra-uterine insemination for unexplained subfertility (R) | Menstrual Disorders and Subfertility Group | 8 | 2012 | |
| Techniques for surgical retrieval of sperm prior to intra-cytoplasmic sperm injection (ICSI ) for azoospermia (R) | Menstrual Disorders and Subfertility Group | 2 | 2008 | |
| Cervical insemination versus intra-uterine insemination of donor sperm for subfertility (R) | Menstrual Disorders and Subfertility Group | 4 | 2008 | |
| Gonadotrophins for idiopathic male factor subfertility (R) | Menstrual Disorders and Subfertility Group | 6 | 2013 | |
| Benign prostatic hyperplasia | Pygeum africanum for benign prostatic hyperplasia (R) | Prostatic Diseases and Urologic Cancers Group | 18 | 1998 |
| Finasteride for benign prostatic hyperplasia (R) | Prostatic Diseases and Urologic Cancers Group | 23 | 2010 | |
| Beta-sitosterols for benign prostatic hyperplasia (R) | Prostatic Diseases and Urologic Cancers Group | 4 | 1999 | |
| Serenoa repens for benign prostatic hyperplasia (R) | Prostatic Diseases and Urologic Cancers Group | 32 | 2012 | |
| Naftopidil for the treatment of lower urinary tract symptoms compatible with benign prostatic hyperplasia (R) | Prostatic Diseases and Urologic Cancers Group | |||
| Microwave thermotherapy for benign prostatic hyperplasia (R) | Prostatic Diseases and Urologic Cancers Group | 15 | 2012 | |
| Phosphodiesterase inhibitors for lower urinary tract symptoms consistent with benign prostatic hyperplasia (P) | Prostatic Diseases and Urologic Cancers Group | N/A | 2012 | |
| Laser prostatectomy for benign prostatic obstruction (R) | Prostatic Diseases and Urologic Cancers Group | 20 | 2000 | |
| Bipolar versus monopolar transurethral resection of the prostate for lower urinary tract symptoms secondary to benign prostatic obstruction (P) | Prostatic Diseases and Urologic Cancers Group | N/A | 2014 | |
| Prostate cancer | 5-alpha-reductase inhibitors for prostate cancer prevention (R) | Prostatic Diseases and Urologic Cancers Group | 9 | 2008 |
| Screening for prostate cancer (R) | Prostatic Diseases and Urologic Cancers Group | 5 | 2013 | |
| Lycopene for the prevention of prostate cancer (R) | Prostatic Diseases and Urologic Cancers Group | 3 | 2011 | |
| Psychosocial interventions for men with prostate cancer (R) | Prostatic Diseases and Urologic Cancers Group | 19 | 2013 | |
| Radical prostatectomy versus watchful waiting for prostate cancer (R) | Prostatic Diseases and Urologic Cancers Group | 2 | 2010 | |
| Bisphosphonates for advanced prostate cancer (R) | Prostatic Diseases and Urologic Cancers Group | 10 | 2006 | |
| Cryotherapy for localized prostate cancer (R) | Prostatic Diseases and Urologic Cancers Group | 8 | 2007 | |
| Neo- adjuvant and adjuvant hormone therapy for localized and locally advanced prostate cancer (R) | Prostatic Diseases and Urologic Cancers Group | 21 | 2006 | |
| Early versus deferred androgen suppression in the treatment of advanced prostatic cancer (R) | Prostatic Diseases and Urologic Cancers Group | 4 | 2001 | |
| Chemotherapy for hormone-refractory prostate cancer (R) | Prostatic Diseases and Urologic Cancers Group | 47 | 2006 | |
| Maximal androgen blockade for advanced prostate cancer (R) | Prostatic Diseases and Urologic Cancers Group | 20 | 1999 | |
| Adjuvant radiotherapy following radical prostatectomy for prostate cancer (R) | Prostatic Diseases and Urologic Cancers Group | 3 | 2011 | |
| Intermittent versus continuous androgen suppression for prostatic cancer (R) | Prostatic Diseases and Urologic Cancers Group | 5 | 2007 | |
| Low-dose rate brachytherapy for men with localized prostate cancer (R) | Prostatic Diseases and Urologic Cancers Group | 1 | 2011 | |
| Interventions for sexual dysfunction following treatments for cancer (R) | Pain, Palliative and Supportive Care Group | 11 | 2007 | |
| Selenium for preventing cancer (R) | Gynaecological Cancer Group | 55 | 2014 | |
| Green tea (Camellia sinensis) for the prevention of cancer (R) | Gynaecological Cancer Group | 51 | 2009 | |
| Exercise for the management of cancer-related fatigue in adults (R) | Pain, Palliative and Supportive Care Group | 56 | 2012 | |
| Laparoscopic versus open prostatectomy for the treatment of localized prostate cancer (P) | Prostatic Diseases and Urologic Cancers Group | N/A | 2012 | |
| Non-steroidal antiandrogen monotherapy compared with luteinizing hormone –releasing hormone agonists or surgical castration monotherapy for advanced prostate cancer (R) | Prostatic Diseases and Urologic Cancers Group | 11 | 2014 | |
| Conservative management for postprostatectomy urinary incontinence (R) | Incontinence Group | 50 | 2015 | |
| Surgery for stress urinary incontinence due to presumed sphincter deficiency after prostate surgery (R) | Incontinence Group | 1 | 2014 | |
| Antibiotic prophylaxis for transrectal prostate biopsy (R) | Prostatic Diseases and Urologic Cancers Group | 19 | 2011 | |
| Testicular cancer | Screening for testicular cancer (R) | Prostatic Diseases and Urologic Cancers Group | 0 | 2011 |
| Bladder cancer | Intravesical gemcitabine for non-muscle invasive bladder cancer (R) | Prostatic Diseases and Urologic Cancers Group | 6 | 2012 |
| Intravesical Bacillus Calmette-Guérin versus epirubicin for Ta and T1 bladder cancer (R) | Prostatic Diseases and Urologic Cancers Group | 5 | 2011 | |
| Gemcitabine for unresectable , locally advanced or metastatic bladder cancer (R) | Prostatic Diseases and Urologic Cancers Group | 6 | 2011 | |
| Intravesical Bacillus Calmette-Guérin in Ta and T1 bladder cancer (R) | Prostatic Diseases and Urologic Cancers Group | 6 | 2000 | |
| Neo-adjuvant chemotherapy for invasive bladder cancer (R) | Prostatic Diseases and Urologic Cancers Group | 11 | 2004 | |
| Intravesical Bacillus Calmette-Guérin versus mitomycin C for Ta and T1 bladder cancer (R) | Prostatic Diseases and Urologic Cancers Group | 7 | 2003 | |
| Surgery versus radiotherapy for muscle invasive bladder cancer (R) | Prostatic Diseases and Urologic Cancers Group | 3 | 2001 | |
| Adjuvant chemotherapy for invasive bladder cancer (individual patient data) (R) | Prostatic Diseases and Urologic Cancers Group | 6 | 2006 | |
| Green tea (Camellia sinensis) for the prevention of cancer (R) | Gyanecological Cancer Group | 51 | 2009 | |
| Perioperative nutrition for the treatment of bladder cancer by radical cystectomy (P) | Prostatic Diseases and Urologic Cancers Group | N/A | 2012 | |
| Urinary diversion and bladder reconstruction /replacement using intestinal segments for intractable incontinence or following cystectomy (R) | Incontinence Group | 5 | 2012 | |
| Hydrocele due to lymphatic filariasis | ||||
| Dysuria/bladder pathology/hydronephrosis due to schistosomiasis | Drugs for treating urinary schistosomiasis (R) | Infectious Diseases Group | 30 | 2014 |
| Therapeutic and prophylactic drug interventions for Schistosomiasis japonicum (P) | Infectious Diseases Group | N/A | 2012 | |
| Rapid screening and diagnostic tests for human schistosomiasis in endemic areas (P) | Infectious Diseases Group | N/A | 2012 | |
| Urinary diversion and bladder reconstruction/replacement using intestinal segments for intractable incontinence or following cystectomy (R) | Incontinence Group | 5 | 2012 |
Supporting Table 2:
| Condition | Review (R) or Protocol (P) |
|---|---|
| Tubulo-interstitial nephritis, pyelonephritis, and urinary tract infections | Interventions to improve professional adherence to guidelines for prevention of device-related infections (R) |
| Mechanical dilatation of the cervix at non-labour caesarean section for reducing postoperative morbidity (R) | |
| Antibiotic prophylaxis versus no prophylaxis for preventing infection after cesarean section (R) | |
| Traditional suburethral sling operations for urinary incontinence in women (R) | |
| Antibiotic prophylaxis for surgery for proximal femoral and other closed long bone fractures (R) | |
| Mupirocin ointment for preventing Staphylococcus aureus infections in nasal carriers (R) | |
| Rituximab for relapsing-remitting multiple sclerosis (R) | |
| Beta lactam antibiotic monotherapy versus beta lactam -aminoglycoside antibiotic combination therapy for sepsis (R) | |
| Habit retraining for the management of urinary incontinence in adults (R) | |
| Preoperative skin antiseptics for preventing surgical wound infections after clean surgery (R) | |
| Antibiotic prophylaxis for cirrhotic patients with upper gastrointestinal bleeding (R) | |
| Antimicrobial therapy for chronic bacterial prostatitis (R) | |
| Cyanoacrylate microbial sealants for skin preparation prior to surgery (R) | |
| Perioperative increase in global blood flow to explicit defined goals and outcomes following surgery (R) | |
| Interventions to improve antibiotic prescribing practices in ambulatory care (R) | |
| Teriflunomide for multiple sclerosis (R) | |
| Laquinimod for multiple sclerosis (R) | |
| Mitoxantrone for multiple sclerosis (R) | |
| Efficacy and safety of cesarean delivery for prevention of mother-to-child transmission of HIV-1 (R) | |
| Surgical approach to hysterectomy for benign gynecological disease (R) | |
| Interventions for preventing mastitis after childbirth (R) | |
| Laparoscopy versus laparotomy for benign ovarian tumor (R) | |
| Valproate preparations for agitation in dementia (R) | |
| Regional versus general anesthesia for caesarean section (R) | |
| Interventions for promoting the initiation of breastfeeding (R) | |
| Protocolized versus non- protocolized weaning for reducing the duration of mechanical ventilation in critically ill adult patients (R) | |
| In-hospital care pathways for stroke (R) | |
| Schedules for home visits in the early postpartum period (R) | |
| Short term benefits for laparoscopic colorectal resection (R) | |
| Diaphragm versus diaphragm with spermicides for contraception (R) | |
| Cervical cap versus diaphragm for contraception (R) | |
| Kidney and other urinary organ cancers | Early and late renal adverse effects after potentially nephrotoxic treatment for childhood cancer (R) |
| Urate oxidase for the prevention and treatment of tumor lysis syndrome in children with cancer (R) | |
| Bisphosphonates and other bone agents for breast cancer (R) | |
| Interventions for preventing non-melanoma skin cancers in high-risk groups (R) | |
| Perioperative blood transfusions and recurrence of colorectal cancer (R) | |
| Medical interventions for the prevention of platinum-induced hearing loss in children with cancer (R) | |
| Cisplatin versus carboplatin in combination with third-generation drugs for advanced non-small cell lung cancer (R) | |
| Immunosuppressive T-cell antibody induction for heart transplant recipients (R) | |
| Concomitant hydroxyurea plus radiotherapy versus radiotherapy for carcinoma of the uterine cervix (R) | |
| Amphotericin B versus fluconazole for controlling fungal infections in neutropenic cancer patients (R) | |
| HMG CoA reductase inhibitors (statins) for dialysis patients (R) | |
| Urinary diversion and bladder reconstruction /replacement using intestinal segments for intractable incontinence or following cystectomy (R) | |
| Pharmacological interventions for pruritus in adult palliative care patients (R) | |
| Homocysteine-lowering interventions for preventing cardiovascular events (R) | |
| HMG CoA reductase inhibitors (statins ) for kidney transplant recipients (R) | |
| Vitamin D supplementation for prevention of mortality in adults (R) | |
| Vitamin D and vitamin D analogues for preventing fractures in post-menopausal women and older men (R) | |
| Antibody induction therapy for lung transplant recipients (R) | |
| First-line tandem high-dose chemotherapy and autologous stem cell transplantation versus single high-dose chemotherapy and autologous stem cell transplantation in multiple myeloma , a systematic review of controlled studies (R) | |
| Antibiotic prophylaxis for preventing post solid organ transplant tuberculosis (R) | |
| Tacrolimus versus cyclosporin as primary immunosuppression for lung transplant recipients (R) | |
| Bisphosphonates in multiple myeloma: a network meta-analysis (R) | |
| Darbepoetin for the anemia of chronic kidney disease (R) | |
| Selenium for preventing cancer (R) | |
| Hyperbaric oxygenation for tumor sensitization to radiotherapy (R) | |
| Adjuvant radiotherapy following radical prostatectomy for prostate cancer (R) | |
| Exenterative surgery for recurrent gynecological malignancies (R) | |
| Laparoscopically assisted radical vaginal hysterectomy versus radical abdominal hysterectomy for the treatment of early cervical cancer (R) | |
| Laparoscopy versus laparotomy for the management of early stage endometrial cancer (R) | |
| Laparoscopic versus open total mesorectal excision for rectal cancer (R) | |
| Adjuvant radiotherapy for stage I endometrial cancer (R) | |
| Cryotherapy for localized prostate cancer (R) | |
| Spinal cord stimulation for cancer -related pain in adults (R) | |
| Chemoradiation for advanced primary vulval cancer (R) | |
| High dose rate versus low dose rate intracavity brachytherapy for locally advanced uterine cervix cancer (R) | |
| Surgical management for upper urinary tract transitional cell carcinoma (R) | |
| Cholecystectomy for patients with silent gallstones (R) | |
| Drugs for treating urinary schistosomiasis (R) | |
| Non-surgical interventions for late radiation cystitis in patients who have received radical radiotherapy to the pelvis (R) | |
| Cranberries for preventing urinary tract infections (R) | |
| Radioiodine therapy for differentiated thyroid carcinoma with thyroglobulin positive and radioactive iodine negative metastases (R) | |
| Conservative management for postprostatectomy urinary incontinence (R) | |
| Surgery for stress urinary incontinence due to presumed sphincter deficiency after prostate surgery (R) | |
| The role of alpha blockers prior to removal of urethral catheter for acute urinary retention in men (R) | |
| Urolithiasis | Pegloticase for chronic gout (R) |
| Fluids and diuretics for acute ureteric colic (R) | |
| Vitamin D supplementation for prevention of mortality in adults (R) | |
| Chinese medicinal herbs for cholelithiasis (R) | |
| Thyroid hormones for acute kidney injury (R) | |
| Vitamin D and vitamin D analogues for preventing fractures in post-menopausal women and older men (R) | |
| Male infertility | Intra-cytoplasmic sperm injection versus conventional techniques for oocyte insemination during in vitro fertilisation in couples with non-male subfertility (R) |
| Oral 5-aminosalicylic acid for induction of remission in ulcerative colitis (R) | |
| Oral 5-aminosalicylic acid for maintenance of remission in ulcerative colitis (R) | |
| Intrauterine insemination versus fallopian tube sperm perfusion for non-tubal infertility (R) | |
| Vasectomy occlusion techniques for male sterilization (R) | |
| Steroid hormones for contraception in men (R) | |
| Benign prostatic hyperplasia | Interventions for chronic abacterial prostatitis (R) |
| Prostate cancer | Interventions for improving the adoption of shared decision making by healthcare professionals (R) |
| Testicular cancer | Chemotherapy for malignant germ cell ovarian cancer in adult patients with early stage, advanced and recurrent disease (R) |
| Bladder cancer | Cholecystectomy for patients with silent gallstones (R) |
| Hyperbaric oxygenation for tumor sensitization to radiotherapy (R) | |
| Drugs for treating urinary schistosomiasis (R) | |
| High dose rate versus low dose rate intracavity brachytherapy for locally advanced uterine cervix cancer (R) | |
| Adjuvant radiotherapy for stage I endometrial cancer (R) | |
| Laparoscopy versus laparotomy for the management of early stage endometrial cancer (R) | |
| Selenium for preventing cancer (R) | |
| Radioiodine therapy for differentiated thyroid carcinoma with thyroglobulin positive and radioactive iodine negative metastases (R) | |
| Chemoradiation for advanced primary vulval cancer (R) | |
| Laparoscopic versus open total mesorectal excision for rectal cancer (R) | |
| Spinal cord stimulation for cancer-related pain in adults (R) | |
| Hydrocele due to lymphatic filariasis | Albendazole for lymphatic filariasis (R) |
| Diethylcarbamazine (DEC)-medicated salt for community-based control of lymphatic filariasis (R) | |
| Dysuria/bladder pathology/hydronephrosis due to schistosomiasis | Metrifonate for Alzheimer's disease (R) |
| Drugs for treating Schistosoma mansoni infection (R) |
Table 1. Men’s health and urologic diseases studied by GBD 2010 with corresponding ICD-10 codes, search terms, number of systematic reviews (R) and protocols (P) in CDSR, percent of total DALYs (arranged in order of decreasing % of total DALY), and number of studies included in Cochrane reviews.
| Condition | ICD-10 code | Search terms | Number of cochrane reviews (R) & protocols (P) | % total 210 dalys (out of 291 conditions) | Number of studies in cochrane review |
|---|---|---|---|---|---|
| Benign prostatic hyperplasia | N40 | “benign prostatic hyperplasia” “median bar” “prostatic hyperplasia” “adenofibromatous hypertrophy of prostrate” “hypertrophy of prostate “prostatic obstruction” | 9 (7 R, 2 P) | 0.2% | 35 |
| Prostate cancer | C61, D07.5, D40.0 | “prostate cancer” “prostatic carcinoma in situ” “prostate neoplasm” | 23 (22 R, 1 P) | 0.15% | 411 |
| Kidney and other urinary organ cancers | C64-C66, D41.0-D41.2 | “kidney cancer” “neoplasm of the ureter” “neoplasm of the kidney” “neoplasm of the renal pelvis” | 4 (4 R) | 0.15% | 63 |
| Tubulointerstitial nephritis, pyelonephritis, and urinary tract infections | N10-N12, N15.1-N15.9, N30, N34, N39.0 | “tubulointerstitial nephritis” “pyelonephritis” “urinary tract infections” “infectious interstitial nephritis” “pyelitis” “balkan nephropathy” “renal and perinephric abscess” “cystitis” “trigonitis” “urethral abscess” “urethritis” | 46 (41 R, 5 P) | 0.13% | 529 |
| Bladder cancer | C67, D09.0*, D41.4 | “bladder cancer” “bladder carcinoma” “bladder neoplasm” | 11 (10 R, 1 P) | 0.12% | 106 |
| Hydrocele due to lymphatic filariasis | B74 (except B74.3, B74.4, B74.8, B74.9) | “lymphatic filariasis” [hydrocele] | 0 | 0.064% | 0 |
| Urolithiasis | N20-N23 | “urolithiasis” “urinary stones” “nephrolithiasis” “kidney stones” “ureterolithiasis” “cystolithiasis” “bladder stones” | 10 (8 R, 2 P) | 0.045% | 59 |
| Dysuria/bladder pathology/hydronephrosis due to schistosomiasis | B65 | “schistosomiasis” [dysuria, bladder, hydronephrosis] | 4 (2 R, 2 P) | 0.034% | 35 |
| Testicular cancer | C62, D40.1 | “testicular cancer” “malignant neoplasm of testis” | 1 R | 0.013% | 0 |
| Male infertility | N46 | “azoospermia” “oligospermia” | 8 R | 0.007 | 95 |
Reviews and protocols representing the ten MHUDs were published by the following Cochrane review groups: Prostatic Diseases and Urologic Cancers Group (n=43); Renal Group (36); Incontinence Group (14); Menstrual Disorders and Subfertility Group (8); Pregnancy and Childbirth Group (7); Infectious Diseases Group (3); Pain, Palliative and Supportive Care Group (2); Gynecological Cancer Group (2); and Neonatal Group (1).
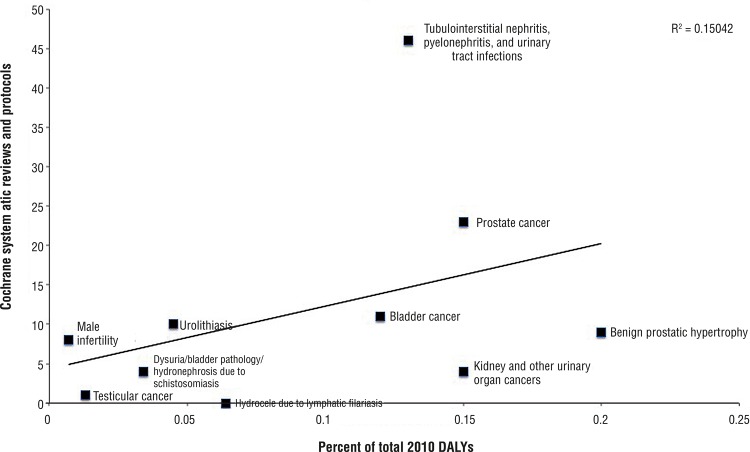
Spearman rank correlation testing between CDSR representation and DALY metrics revealed poor positive correlation that was statistically insignificant (rho=0.41, p=0.21). The majority of the MHUDs (6) were under-represented in CDSR as compared to GBD DALY (Figure-2). Most of the systematic reviews and protocols (58.6%) were published from 2011 to 2015 while 37.9% were published from 2000 to 2010; only 4 reviews were published prior to 2000. Maintaining systematic reviews up-to-date is critical to deliver consensus statements on current world literature that ultimately impact clinical decisions and patient outcomes.
Figure 2. Comparison of men’s health and urologic disease representation in the Cochrane Database of Systematic Reviews with percent of 2010 DALYs from 291 conditions studied by GBD 2010.
Representation of tubulointerstitial nephritis, pyelonephritis, and urinary tract infections exceeded GBD disease burden. This disease category also had the greatest number of cumulative studies informing its systematic reviews (529). The one systematic review representing testicular cancer, entitled “Screening for testicular cancer,” found no randomized controlled trials in the literature. Systematic reviews that find no suitable trials to address their objectives uncover areas for much-needed, high-quality research.
The World Health Organization (WHO) classifies two of the MHUDs as neglected tropical diseases: dysuria/bladder pathology/hydronephrosis due to schistosomiasis and hydrocele due to lymphatic filariasis (14). It is important to note that just as the DALY metrics reported for these two diseases include only burden due to the MHUD morbidity (dysuria, bladder pathology, hydronephrosis, hydrocele), systematic reviews were only considered representative if they included assessment of the MHUD pathology.
DISCUSSION
We acknowledge several limitations of our study. The scope of CDSR systematic reviews is subject to variability. For instance, authors may prepare one large review of multiple interventions (lumping) or several reviews of individual interventions (splitting). Therefore, treating a systematic review or protocol as one measurement unit may not be entirely accurate for every topic. While beyond the scope of this limited study, further exploration is warranted into potential underrepresentation of certain conditions.
There remains a lack of transparency in publications and databases on the quality of data and criteria involved in prioritization decisions (15). Other important factors in priority setting include availability of research funds, knowledge gap, and impact on disadvantaged populations. Research prioritization is also inherently political and dependent on financial backing, which further demonstrates the importance of a transparent process. Attention and awareness of priority setting has the potential to minimize research disparities and, ultimately, impact populations at a global scale.
ACKNOWLEDGEMENTS:
Tyler Okland and Chante Karimkhani are contributed similarly as first authors.
Luc Coffeng MD, Department of Public Health at Erasmus MC University Medical Center, Rotterdam, Nederlands.
Megan Coggeshall BA, Institute for Health Metrics and Evaluation, University of Washington, Seattle, WA.
Footnotes
FINANCIAL SUPPORT
There was no direct funding to the current study. The Global Burden of Disease study received funding from the Bill and Melinda Gates Foundation (PI: Christopher J.L. Murray). Lindsay Boyers, Mark Sawyer, and Robert Dellavalle are employees of the U.S. Department of Veterans Affairs. The U.S. Department of Veterans Affairs had no role in the design and execution of the study. Robert Dellavalle is supported by grants from the CDC and National Institutes of Health. Tyler Okland, Chante Karimkhani, Hannah Pederson, Lindsay Boyers, Mohsen Naghavi, and Mark Sawyer report no relevant disclosures. Any opinions expressed herein do not necessarily reflect the opinions of the CDC or the Department of Veterans Affairs.
REFERENCES
- 1.Fleurence RL. Setting priorities for research: a practical application of ‘payback’ and expected value of information. Health Econ. 2007;16:1345–1357. doi: 10.1002/hec.1225. [DOI] [PubMed] [Google Scholar]
- 2.Nasser M, Welch V. Prioritization of systematic reviews leads prioritization of research gaps and needs. J Clin Epidemiol. 2013;66:522–523. doi: 10.1016/j.jclinepi.2012.09.007. [DOI] [PubMed] [Google Scholar]
- 3.Shiffman J. Knowledge, moral claims and the exercise of power in global health. Int J Health Policy Manag. 2014;3:297–299. doi: 10.15171/ijhpm.2014.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Murray CJ, Ezzati M, Flaxman AD, Lim S, Lozano R, Michaud C, et al. GBD 2010: design, definitions, and metrics. Lancet. 2012;380:2063–2066. doi: 10.1016/S0140-6736(12)61899-6. [DOI] [PubMed] [Google Scholar]
- 5.Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2095–2128. doi: 10.1016/S0140-6736(12)61728-0. Erratum in: Lancet. 2013;381:628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Clarke M, Hopewell S, Chalmers I. Clinical trials should begin and end with systematic reviews of relevant evidence: 12 years and waiting. Lancet. 2010;376:20–21. doi: 10.1016/S0140-6736(10)61045-8. [DOI] [PubMed] [Google Scholar]
- 7.Jadad AR, Cook DJ, Jones A, Klassen TP, Tugwell P, Moher M, et al. Methodology and reports of systematic reviews and meta-analyses: a comparison of Cochrane reviews with articles published in paper-based journals. JAMA. 1998;280:278–280. doi: 10.1001/jama.280.3.278. [DOI] [PubMed] [Google Scholar]
- 8.Collier A, Heilig L, Schilling L, Williams H, Dellavalle RP. Cochrane Skin Group systematic reviews are more methodologically rigorous than other systematic reviews in dermatology. Br J Dermatol. 2006;155:1230–1235. doi: 10.1111/j.1365-2133.2006.07496.x. [DOI] [PubMed] [Google Scholar]
- 9.Emdin CA, Odutayo A, Hsiao AJ, Shakir M, Hopewell S, Rahimi K, et al. Association between randomised trial evidence and global burden of disease: cross sectional study (Epidemiological Study of Randomized Trials—ESORT) h117BMJ. 2015;350 doi: 10.1136/bmj.h117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yoong SL, Hall A, Williams CM, Skelton E, Oldmeadow C, Wiggers K, et al. Alignment of systematic reviews published in the Cochrane Database of Systematic Reviews and the Database of Abstracts and Reviews of Effectiveness with global burden of disease data: a bibliographic analysis. J Epidemiol Community Health. J Epidemiol Community Health. 2015 Jul;69(7):708–714. doi: 10.1136/jech-2014-205389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pederson H, Okland T, Boyers LN, Karimkhani C, Rosenfeld RM, Nasser M, et al. Identifying otolaryngology systematic review research gaps: comparing Global Burden of Disease 2010 results with Cochrane Database of Systematic Review content. JAMA Otolaryngol Head Neck Surg. 2015;141:67–72. doi: 10.1001/jamaoto.2014.2700. [DOI] [PubMed] [Google Scholar]
- 12.Karimkhani C, Trikha R, Aksut B, Jones T, Boyers LN, Schlichte M, et al. Identifying gaps for research prioritisation: Global burden of external causes of injury as reflected in the Cochrane Database of Systematic Reviews. Injury. 2016;47:1151–1157. doi: 10.1016/j.injury.2015.12.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.The Cochrane Collaboration [Accessed January 15, 2015];Search the Cochrane library. http://www.thecochranelibrary.com/view/0/index.html.
- 14.World Health Organization [Accessed March 5, 2015];Neglected tropical diseases. http://www.who.int/neglected_diseases/diseases/en/
- 15.Oxman AD, Schünemann HJ, Fretheim A. Improving the use of research evidence in guideline development: 2. Priority setting. 14Health Res Policy Syst. 2006;4 doi: 10.1186/1478-4505-4-14. [DOI] [PMC free article] [PubMed] [Google Scholar]