Abstract
Background
In multiple sclerosis (MS), treatment discontinuation leads to a higher risk of relapse, poorer quality of life and greater economic impact.
Objective
The objective of this work is to evaluate treatment discontinuation in MS, the reasons for this and the reasons for treatment resumption.
Methods
A French national Web-based survey was carried out between May and August 2011. A total of 602 MS patients answered a questionnaire on sociodemographic data, medical follow-up, disease-modifying therapies (DMTs), symptomatic treatments, care given, factors involved in treatment discontinuation and reasons for resuming treatment.
Results
Among 413 patients using DMTs, 54% have considered discontinuing their treatment, primarily because of anger (61%), side effects (61%) and fatigue (57%). Sixty-eight patients have actually discontinued their treatment because of side effects (43%), lack of observed outcomes (32%), exasperation (29%) or fatigue (29%). The reasons for symptomatic treatment discontinuation were fear of addiction (32%–46%) and lack of efficacy (28%–45%). Physiotherapy was discontinued because of fatigue (37%), stress (34%) or inefficiency (31%). According to patients, treatment discontinuation could have been prevented by psychological support, care team empathy and support from family.
Conclusion
The major factor that could prevent treatment discontinuation is psychological support. Initiating and monitoring treatment in MS leads to emotional and personality changes, requiring adaptations that may improve compliance.
Keywords: Multiple sclerosis, disease-modifying therapies, treatment discontinuation, Web survey, patient adherence
Introduction
Multiple sclerosis (MS) is the most common cause of neurological disability among young adults.1 In France, the national prevalence was estimated to be 94.7 per 100,000 patients covered by the national health insurance system in 2004 (95% confidence interval (CI): 94.3–95.1).2
Long-term MS management includes disease-modifying therapies (DMTs) to slow disease progression and treatments to relieve symptoms. Symptom management is essential and includes pharmacological and non-pharmacological measures regarding walking impairment, fatigue, spasticity, pain, sphincter problems and cognitive dysfunction.
The World Health Organization (WHO) defines adherence as “The extent to which a person’s behavior—taking medication, following a diet, and/or executing lifestyle changes—corresponds with agreed recommendations from a health care provider.”3 Studies on MS therapy in clinical practice have shown adherence rates ranging from 28% to 87%, which are similar to other chronic diseases in which the self-administration of a treatment is required, such as asthma (57%), diabetes (75%–92%), human immunodeficiency virus/acquired immunodeficiency syndrome (HIV/AIDS) (17%–67%), hypertension (49%), depression (30%–60%) and epilepsy (40%–60%).4
Patients are most likely to discontinue therapy in the first six months after treatment initiation, with rates ranging from 9% to 20%.5,6 Other studies suggest that the percentage of MS patients who do not adhere to treatment is around 40%.7,8 It has been shown that MS patients who adhere to DMTs have a lower risk of relapse9,10 and better quality of life11 than patients who do not. The poor adherence to MS treatment is also an economic burden. A retrospective study found that adherent patients were significantly less likely to have MS-related inpatient hospitalization than non-adherent patients (odds ratio (OR) = 0.63, 95% CI: 0.47–0.83).12
As outlined by the WHO, “The ability of patients to follow treatment plans in an optimal manner is frequently compromised by more than one barrier […] disease therapies and patient-related factors.3 […] Most notable are those related to the complexity of the medical regimen, duration of treatment, previous treatment failures, frequent changes in treatment, the immediacy of beneficial effects, side-effects, and the availability of medical support to deal with them.”
In France, no specific large-scale study has been conducted to evaluate the rate of discontinuation with MS treatments and other related aspects of MS care (physiotherapy, psychological support, etc.). This survey aimed to evaluate the discontinuation of various therapies among MS patients, such as DMTs, symptomatic treatments and rehabilitation, and to describe the factors affecting adherence as well as the reasons for treatment resumption.
Materials and methods
ALLIANCE is a Web-based survey conducted in France between May and August 2011. The participants were invited to take the survey through links on various French MS society websites that patients were likely to visit and by posters in hospitals or private neurology practices. MS patients were directed to visit a specific website in order to answer the survey questionnaire. The questionnaire was totally anonymous.
Questionnaire
General characteristics included location, town size, gender, year of birth, employment status, number of children, age of completing education, occupation, financial status, disease duration, time since diagnosis, walking distance, and services and health care professionals consulted, in type and frequency.
The treatment management questions covered DMT (type and duration of treatment, treatment switches, temptation to discontinue treatment and reasons for this, actual discontinuation, duration and reasons for this), symptomatic treatments (types of treatment, treatment discontinuation, duration and reasons for this) and non-pharmacological treatments (rehabilitation type, discontinuation with duration and reasons for this), the reasons for resuming treatment and the factors that could have prevented discontinuation. Treatment discontinuation taken into account concerned only those decided by the patients themselves. Participants were also asked how they had heard about the survey, and their knowledge of specific MS websites was tested.
Statistics
Open questions were first grouped by meaning and then coded. Qualitative variables were described by number of occurrences and percentages, and quantitative variables by mean and standard deviation (SD). The Chi-squared test was used for comparisons between categorical variables (gender, age under/over 42 years, disease duration, time since diagnosis, duration of DMT, self-injection for DMT and Expanded Disability Status Scale (EDSS) score).
Results
A total of 764 people visited the survey website. Of these, 162 were excluded from the survey: Forty-four did not have MS, one was under 18 years of age, 27 patients did not start the questionnaire and 90 did not complete it. There were 602 people who completed the questionnaire. More than half (56%) had been told about ALLIANCE by public or private institutions involved in MS. For the remaining participants, MS support groups, the Internet or neurologists/general practitioners had acted as middlemen.
Demographics
A total of 602 people were included; 78% of patients were women with mean age 42.9 years (SD = 10.80) and mean (SD) disease duration of 11.8 years (8.7). Most participants lived in the Paris area and northern France. Only 56% were working, with the others registered as disabled or on sick leave. The demographic characteristics of ALLIANCE participants are summarized in Table 1.
Table 1.
Demographic and clinical characteristic of MS patients.
| Characteristic | Population (n = 602) |
|---|---|
| Age | |
| mean (SD) | 42.9 years (10.8) |
| Gender | 78% women, 22% men |
| Disease duration | |
| mean (SD) | 11.8 years (8.7) |
| Time since diagnosis | |
| mean (SD) | 8.4 years (7.2) |
| EDSS score | |
| 6.0–7.0 | 22% (n = 132) |
| 4.5–5.5 | 11% (n = 66) |
| <4 | 31% (n = 187) |
| Not determined | 36% (n = 217) |
| Location | |
| Ile-de-France | 21% (n = 127) |
| Nord-Pas-de-Calais | 16% (n = 97) |
| Other regions of France | 63% (n = 378) |
| Marital status | |
| Married | 49% (n = 295) |
| In a relationship | 19% (n = 115) |
| Single | 20% (n = 120) |
| Divorced | 10% (n = 60) |
| Widowed | 1% (n = 6) |
| Number of children | |
| None | 49% (n = 295) |
| One | 23% (n = 139) |
| Two, three or more | 28% (n = 168) |
| Occupation | |
| Working | 56% (n = 337) |
| Registered disabled | 15% (n = 90) |
| On sick leave | 7% (n = 42) |
| Retired | 7% (n = 42) |
| Inactive | 5% (n = 30) |
| Financial situation | |
| Affluent | 3% (n = 18) |
| Comfortable | 53% (n = 319) |
| Experiencing financial difficulties | 35% (n = 211) |
| Poor | 5% (n = 30) |
MS: multiple sclerosis; EDSS: Expanded Disability Status Scale.
Disease management strategies
Health care providers
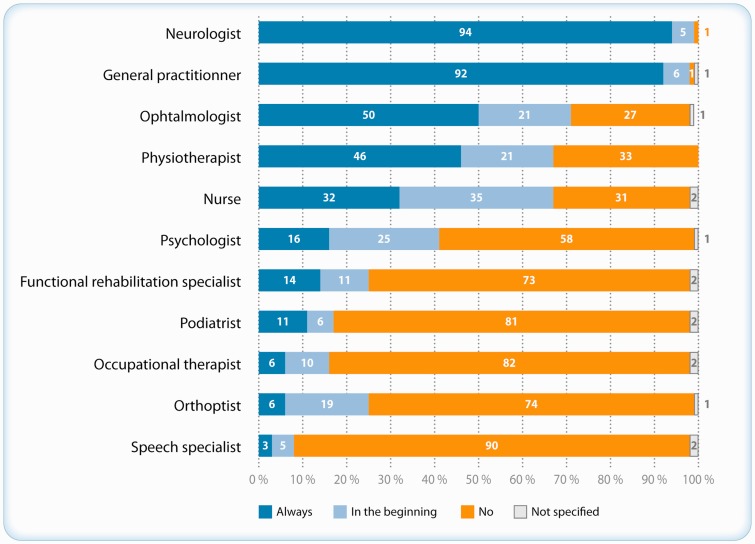
At the time of the survey, most of the 602 MS patients were still being monitored by a neurologist and general practitioner (94% and 92%, respectively); about half of the patients consulted ophthalmologists, physiotherapists and 32% nurses, whereas only a small percentage consulted psychologists (16%) or occupational therapists (6%) (Figure 1). Psychological or psychiatric support had been provided to 17% and 13% of patients respectively in the previous 12 months. Patients with long disease duration (>15 years) or higher EDSS scores were more frequently using physiotherapy or speech therapy (p = 0.001 and p < 0.001, respectively) and psychological/psychiatric support (p < 0.001). Nurses were involved mainly with patients taking DMTs (p < 0.001), especially at the outset of therapy.
Figure 1.
Health care professionals consulted since multiple sclerosis (MS) diagnosis (n = 602).
DMTs
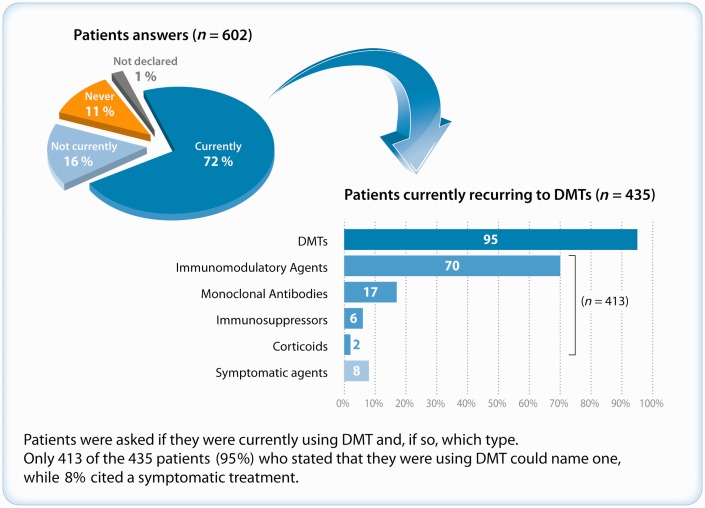
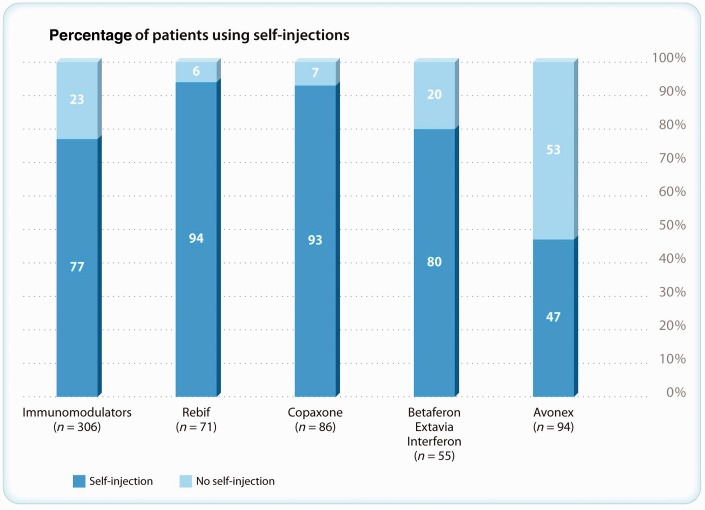
Among the 602 participants, 435 (72%) stated that they were taking DMTs at the time of the study (Figure 2) and 413 (95%) could name a DMT. A total of 306 patients were using interferon (IFN) or glatiramer acetate, with 77% using self-injections (Figure 3). Among the 413 patients who could name a DMT, 180 (44%) had changed DMT at least once.
Figure 2.
Patients using disease-modifying therapy (DMT).
Figure 3.
Patients using self-injections (n = 306).
There were 220 patients (54%) who stated that they had been tempted to discontinue their DMT, primarily because of side effects (61%), exasperation or anger (61%), fatigue (57%), wish to stop feeling sick (34%), lack of noticeable improvements (28%), constraints (28%) or needle-phobia (15%).
Sixty-eight patients (16%) actually discontinued their treatment. Of these, 67% did so for less than three months. The main reasons for DMT discontinuation are summarized in Table 2; side effects associated with DMTs and the lack of noticeable improvements were the two factors most frequently affecting the non-adherence of MS patients. Factors such as EDSS score, disease duration, and type of DMT and injection method did not appear to influence discontinuation. Patients who had had MS for 10–14 years were more inclined to take a break from treatments (p = 0.03), whereas patients treated for less than five years stated that they had never stopped their treatment (p < 0.001).
Table 2.
Reasons for disease-modifying therapy (DMT) discontinuation (n = 66).
| Reason for discontinuation | Percentage |
|---|---|
| Adverse effects (pain, flu-like symptoms, injection-site reactions, nausea, etc.) | 43% |
| Lack of noticeable improvement | 32% |
| Anger/exasperation | 29% |
| Fatigue | 29% |
| Practical issues | 18% |
| Want to stop feeling sick | 16% |
| Pregnancy/want to have children | 10% |
| Holidays/travel | 7% |
| Needle phobia | 5% |
| Inefficacy | 5% |
| Other | 21% |
| None given | 4% |
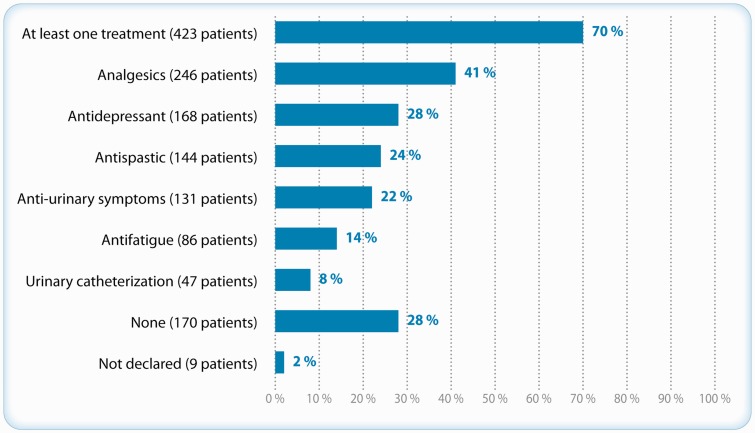
Symptomatic treatments
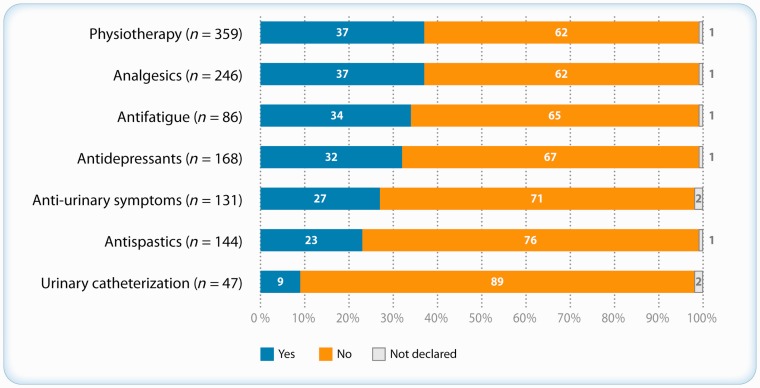
Symptomatic treatments were taken by 423 (70%) patients, primarily analgesics and antidepressants (Figure 4). Analgesics, anti-fatigue medications and antidepressants were discontinued by more than 30% of patients (Figure 5). The major reason for discontinuing treatment was lack of noticeable improvement (anti-fatigue 45%; anti-spastic 30%; urinary treatment 28%; analgesics 18%). The fear of addiction was cited by 46% of patients using antidepressants and 32% of those using analgesics, adverse effects by 24% of patients using anti-spastics and 19% of those using urinary treatment. Fatigue and exasperation were cited by 8% to 20% of patients for all types of symptomatic treatments (Table 3). Intermittent self-catheterization (ISC) was used by 47 participants, and was scarcely discontinued (9% of patients) (Figure 4 and 5).
Figure 4.
Patients using symptomatic treatments (n = 602).
Figure 5.
Symptomatic treatment and physiotherapy discontinuation.
Table 3.
Reasons for discontinuing symptomatic treatments and/or physiotherapy.
| Treatment |
||||||
|---|---|---|---|---|---|---|
| Reason for treatment | Analgesic |
Antidepressant | Antispastic | Anti- fatigue | Urinary treatments | Physiotherapy |
| discontinuation | n = 92 | n = 54 | n = 33 | n = 29 | n = 36 | n = 133 |
| Fear of addiction | 32% | 46% | 9% | 21% | 11% | – |
| Adverse events | 8% | 6% | 24% | 17% | 19% | 7% |
| Lack of noticeable improvement | 18% | 9% | 30% | 45% | 28% | 31% |
| Anger/exasperation | 16% | 20% | 12% | 10% | 17% | 22% |
| Weariness | 13% | 15% | 21% | 14% | 8% | 37% |
| Practical issues | 3% | 4% | 6% | 3% | 8% | 34% |
| Not willing to do it | – | – | – | – | – | 17% |
Display percentages do not add up to 100% because patients mentioned more than one reason.
Rehabilitation care
A total of 364 patients (60%) used rehabilitation care; 359 used physiotherapy and other kinds of rehabilitation care were rare: 8% orthoptics, 6% occupational therapy and 5% speech therapy. Physiotherapy was discontinued by 37% of patients, primarily because of fatigue (37%), constraints (34%) and lack of noticeable improvement (31%) (Table 3 and Figure 5).
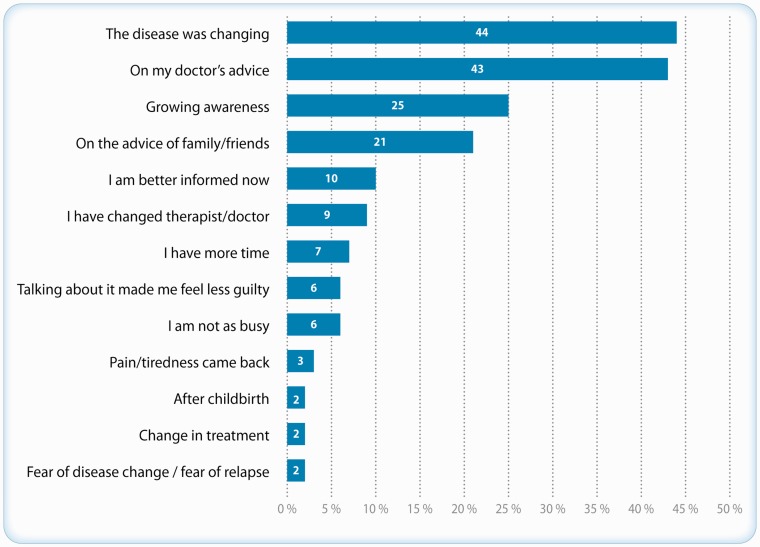
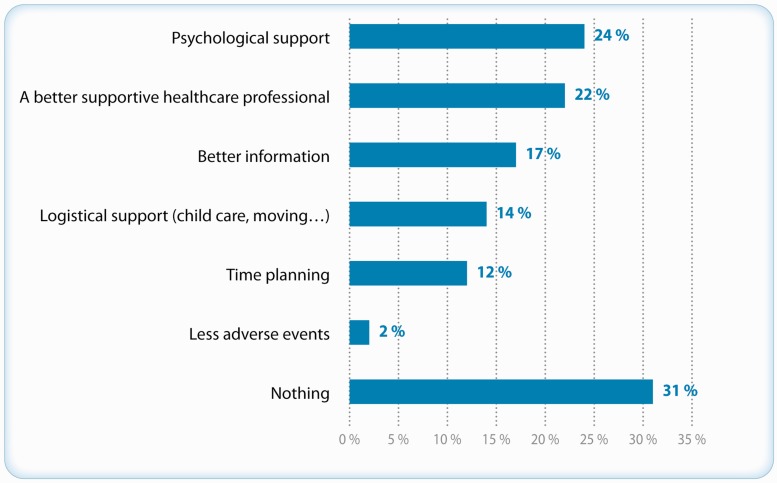
Reasons for resuming treatment
The 233 MS patients who had discontinued at least one treatment or MS care stated that they resumed it because of disease progression (44%), following medical advice (43%), after receiving new information (25%) or on the advice of friends or family (21%) (Figure 6). When patients were asked which factors might have prevented treatment discontinuation, psychological and medical support were cited by 24% and 22%, respectively, whereas better information was cited by 17%. Nevertheless, 31% of patients stated that nothing could have prevented the discontinuation (Figure 7). Finally, improving quality of life was the major aim for 40% of patients participating in the ALLIANCE survey.
Figure 6.
Reasons for resuming disease-modifying therapy (DMT)/symptomatic treatment (n = 233).
Figure 7.
Factors that may prevent treatment discontinuation (n = 233).
Discussion
This survey included 602 MS participants who completed a Web-based questionnaire. It reflects the way in which MS patients cope with the disease management burden. The limitations of the survey relate to the type of methodology used. Internet surveys do not capture the MS population as a whole, as lower educational levels or incomes can affect access to a computer-based questionnaire. In fact, the majority of ALLIANCE participants (83%) had medium to high educational levels and more than half were in comfortable financial situation. Only 90 out of 764 people (12%) failed to complete the questionnaire, which is somewhat unusual for Internet surveys; people are not as likely to complete a long Web-based questionnaire as they are when participating in a face-to-face interview. Because of self-reporting data, no information on disease activity was available enabling us to analyze treatment discontinuation. The question about treatment discontinuation within the questionnaire stated that treatment discontinuation concerned only the patient’s decision and not medical decisions. The population distribution showed an over-representation of the Paris area and north of France because patients were more numerous in these regions, which corresponds to MS distribution in France.
Up to 54% of the patients have been tempted to discontinue their DMTs, primarily because of exasperation, which is as significant as side effects, but only 16% actually did so, with side effects cited as the main reason. This percentage is consistent with the French cross-sectional study by de Seze et al. that reports a 17.8% “drug holidays” rate among DMT users.13 It is also consistent with data from various studies and previous suggestions that patient adherence to MS therapies is suboptimal.8,11,14 Adherence to treatment in MS, as in all chronic and long-term diseases, is vital. There is evidence that patients who do not adhere to their treatment are unlikely to receive its full potential benefit5 and long-term discontinuation of MS therapy entails a higher risk of severe relapse.10 Steinberg et al.9 showed that patients with high levels of exposure to IFN had lower relapse rates and used fewer health care resources than patients with low levels of exposure. The adverse events associated with DMTs are the most common reason for treatment discontinuation. For IFNs, the incidence and severity of flu-like symptoms (FLS) tend to decrease with the length and titration of the treatment,1,8 but MS patients are not always well informed about this. Injection-site reactions (ISRs) and lipoatrophy are frequently associated with subcutaneous DMTs. A correct injection technique and rotation of injection sites can help to prevent ISRs.15
Very few studies have reported the incidence of physiotherapy in MS. In a series of 1065 MS patients (73% women, 63.4 years), Finlayson et al. reported that 64% benefited from physiotherapy,16 consistent with the 60% found in ALLIANCE. At the time of this survey, 46% of the patients were receiving physiotherapy, which appears likely given the characteristics of the population: young with a mean disease duration of less than 10 years and 31% of patients with EDSS <4. In comparison, Finlayson reports only 8% of patients receiving treatment at the time of the survey.16 It is quite difficult to compare the figures with data from the literature given the different patient profiles and health systems, especially when considering the financial management of rehabilitation. However, 37% of the patients had discontinued physiotherapy, primarily because of fatigue (37%). Fatigue is very common in MS and is one of the most disabling symptoms, appearing early in the course of the disease and impairing quality of life.17 Management relies largely on energy-saving techniques but also on reconditioning.18,19 Rehabilitation is effective and should always be made available. Patients’ lack of knowledge about physical activity tends to improve but this should be accelerated by caregivers for increased awareness.20 Constraints are the second reason for discontinuing physiotherapy: Patients often have multiple appointments or regular hospitalizations with new treatments, and several physiotherapy sessions per week can increase the disease burden and interfere with their professional and private life.
Urinary intermittent self-catheterization (ISC), which is seldom assessed in MS, was used by 47 patients, with a high rate of compliance (89%) compared to 55%–61% in other published series.21,22 This high rate may reflect the immediate effect felt by patients—management of leaks, improved sleep, etc.—even though the technique is invasive. Despite involving a learning phase and patient adherence, ISC is considered simple and straightforward.22 Van Achterberg et al.23 highlighted the importance of psychological factors and emphasized the need to identify lack of knowledge of the technique, fears and feelings of shame associated with urinary catheters. Adherence to ISC requires active acceptance of the technique rather than denial and avoidance of bladder behavior issues; this would allow autonomy, resumption of normal activities and bladder control, leading to improved quality of life, dignity and self-esteem.24
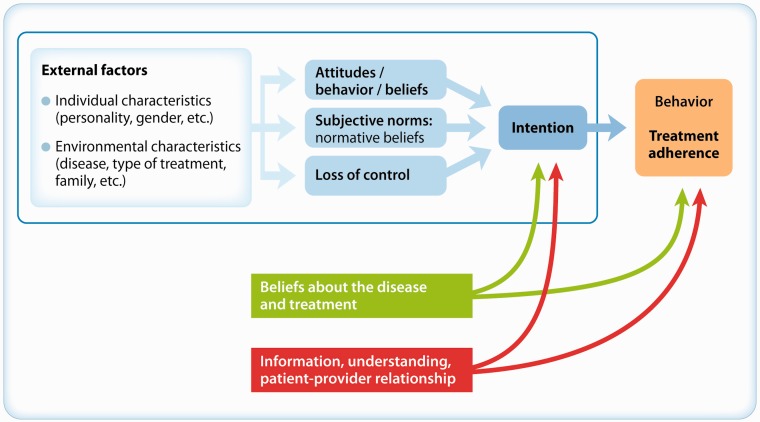
In our results, EDSS score, disease duration, type of DMT and injection method did not seem to influence non-adherence. Some others factors seem to contribute; perceived inefficacy is a major reason contributing to non-adherence. The treatment benefits may not be felt immediately and some patients tend to be overoptimistic.1,6 Prescribed MS treatments should be maintained over a long period of time to reduce the frequency of relapses, which is a difficult target to assess for patients.25 Patients may question the relevance of the therapeutic process and the threat posed by the disease. Among the factors explaining the adherence levels, Stanton26 outlined the quality of the patient-physician relationship and information, as well as patients’ beliefs (about the disease and treatment), sense of control and perception of social support. The first step that could prevent treatment discontinuation is psychological support, and this should be addressed with psychological follow-up (when requested or on a regular basis) at disease onset or exacerbation. However, ALLIANCE has shown that psychological or psychiatric support had been provided to a small proportion of patients (17% or 13%, respectively) within the 12 months prior to the study. A possible strategy to improve patient adherence would be to strengthen the therapeutic relationship, manage patient expectations (which do not always align with reality), address concerns and educate patients and their family about the disease and treatment (Figure 8). Even with the limitations and constraints of treatment, a well-informed patient will be more likely to understand the importance of treatment and adhere to it.
Figure 8.
Psychosocial factors influencing treatment adherence in multiple sclerosis.
Acknowledgement
Dr Nathalie Debbas, Medi, Axe 6 Rue Edison, 92140 CLAMART (France), helped to draft the manuscript.
Conclusions
Knowledge of MS treatments, availability of medical support to manage side effects and adherence to well-designed psychological support programs may help to increase the level of adherence to treatments.
Funding
This work was supported by Biogen Idec France, Le Capitole, 55 avenue des Champs Pierreux, 920012 Nanterre Cedex – France.
Conflict of interest.
None declared.
References
- 1.Patti F. Optimizing the benefit of multiple sclerosis therapy: The importance of treatment adherence. Patient Prefer Adherence 2010; 4: 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fromont A, Binquet C, Sauleau EA, et al. Geographic variations of multiple sclerosis in France. Brain 2010; 133: 1889–1899. [DOI] [PubMed] [Google Scholar]
- 3.World Health Org. Adherence to long-term therapies, http://www.who.int/chp/knowledge/publications/adherence_report/en/index.html (accessed 16 November 2012).
- 4.Brandes DW, Callender T, Lathi E, et al. A review of disease-modifying therapies for MS: Maximizing adherence and minimizing adverse events. Curr Med Res Opin 2009; 25: 77–92. [DOI] [PubMed] [Google Scholar]
- 5.Tremlett HL, Oger J. Interrupted therapy: Stopping and switching of the beta-interferons prescribed for MS. Neurology 2003; 61: 551–554. [DOI] [PubMed] [Google Scholar]
- 6.Mohr DC, Goodkin DE, Likosky W, et al. Therapeutic expectations of patients with multiple sclerosis upon initiating interferon beta-1b: Relationship to adherence to treatment. Mult Scler 1996; 2: 222–226. [DOI] [PubMed] [Google Scholar]
- 7.Portaccio E, Zipoli V, Siracusa G, et al. Long-term adherence to interferon beta therapy in relapsing–remitting multiple sclerosis. Eur Neurol 2008; 59: 131–135. [DOI] [PubMed] [Google Scholar]
- 8.Riñon A, Buch M, Holley D, et al. The MS Choices Survey: Findings of a study assessing physician and patient perspectives on living with and managing multiple sclerosis. Patient Prefer Adherence 2011; 5: 629–643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Steinberg SC, Faris RJ, Chang CF, et al. Impact of adherence to interferon in the treatment of multiple sclerosis: A non-experimental, retrospective, cohort study. Clin Drug Investig 2010; 30: 89–100. [DOI] [PubMed] [Google Scholar]
- 10.Al-Sabbagh A, Bennet R, Kozma C, et al. Medication gaps in disease-modifying therapy for multiple sclerosis are associated with an increased risk of relapse: Findings from a national managed care database. J Neurol 2008; 255 (Suppl 2): S79. [Google Scholar]
- 11.Treadaway K, Cutter G, Salter A, et al. Factors that influence adherence with disease-modifying therapy in MS. J Neurol 2009; 256: 568–576. [DOI] [PubMed] [Google Scholar]
- 12.Tan H, Cai Q, Agarwal S, et al. Impact of adherence to disease-modifying therapies on clinical and economic outcomes among patients with multiple sclerosis. Adv Ther 2011; 28: 51–61. [DOI] [PubMed] [Google Scholar]
- 13.de Seze J, Borgel F, Brudon F. Patient’s perception of multiple sclerosis and its treatment. Patient Prefer Adherence 2012; 6: 263–273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Halpern R, Agarwal S, Dembek C, et al. Comparison of adherence and persistence among multiple sclerosis patients treated with disease-modifying therapies: A retrospective administrative claims analysis. Patient Prefer Adherence 2011; 5: 73–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Walther EU, Hohlfeld R. Multiple sclerosis: Side effects of interferon beta therapy and their management. Neurology 1999; 53: 1622–1627. [DOI] [PubMed] [Google Scholar]
- 16.Finlayson M, Plow M, Cho C. Use of physical therapy services among middle-aged and older adults with multiple sclerosis. Phys Ther 2010; 90: 1607–1618. [DOI] [PubMed] [Google Scholar]
- 17.Krupp LB, Serafin DJ, Christodoulou C. Multiple sclerosis-associated fatigue. Expert Rev Neurother 2010; 10: 1437–1447. [DOI] [PubMed] [Google Scholar]
- 18.Andreasen AK, Stenager E, Dalgas U. The effect of exercise therapy on fatigue in multiple sclerosis. Mult Scler 2011; 17: 1041–1054. [DOI] [PubMed] [Google Scholar]
- 19.Pilutti LA, Greenlee TA, Motl RW, et al. Effects of exercise training on fatigue in multiple sclerosis: A meta-analysis. Psychosom Med 2013; 75: 575–580. [DOI] [PubMed] [Google Scholar]
- 20.Motl RW, Pilutti LA. The benefits of exercise training in multiple sclerosis. Nat Rev Neurol 2012; 8: 487–497. [DOI] [PubMed] [Google Scholar]
- 21.Luoto E, Jussilainen M, Sandell S. Intermittent self-catheterization in multiple sclerosis [article in Finnish]. Sairaanhoitaja 1993; 1: 17–20. [PubMed] [Google Scholar]
- 22.Girotti ME, MacCornick S, Perissé H, et al. Determining the variables associated to clean intermittent self-catheterization adherence rate: One-year follow-up study. Int Braz J Urol 2011; 37: 766–772. [DOI] [PubMed] [Google Scholar]
- 23.van Achterberg T, Holleman G, Cobussen-Boekhorst H, et al. Adherence to clean intermittent self-catheterization procedures: Determinants explored. J Clin Nurs 2008; 17: 394–402. [DOI] [PubMed] [Google Scholar]
- 24.Shaw C, Logan K. Psychological coping with intermittent self-catheterizations (ISC) in people with spinal injury: A qualitative study. Int J Nurs Stud 2013; 50: 1341–1350. [DOI] [PubMed] [Google Scholar]
- 25.Oliveira T, Fiore A, Fragoso Y. Adherence to glatiramer acetate treatment for multiple sclerosis: The Brazilian experience. Patient Prefer Adherence 2008; 2: 41–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Stanton AL. Determinants of adherence to medical regimens by hypertensive patients. J Behav Med 1987; 10: 377–394. [DOI] [PubMed] [Google Scholar]