Abstract
Unruptured vertebral arteries dissecting aneurysms have a benign clinical course. The most common symptoms compromise headache, neck pain, dizziness and vomiting. The optimal endovascular treatment option remains controversial. Reconstructive techniques have many advantages over deconstructive ones since the advent of flow diverters such as the Pipeline embolization device (PED). Here, we present a case successfully treated with a PED through a combination of the radial access and advancement of the Marksman catheter into the contralateral vertebral artery due to the special angio-architecture of the patient.
Keywords: Pipeline embolization device, contralateral vertebral artery, radical access
Introduction
The Pipeline embolization device (PED) is a novel flow-diverting device whose aim is the reconstruction of the parent vessel instead of intra-saccular embolization of the aneurysm per se. Its safety and efficacy in the treatment of unruptured and ruptured dissecting aneurysms have already been proven.1–3 The experience that has been accumulated by those using the PED has led to its use being extrapolated in many off-label cases, and the techniques for its deployment need to be continually reassessed in order to suit a range of situations. This case demonstrates a novel deployment option for cases of brachiocephalic artery (BRA) tortuosity and a narrow and sharped curve of the vertebrobasilar junction. The whole procedure was completed smoothly, and the patient was free from any periprocedural complication.
Clinical presentation
The patient was a 62-year-old female who presented with intermittent occipital headache and dizziness for three months. Those symptoms were aggravated 10 days before admission. A computed tomography angiogram performed at a local hospital suggested a right vertebral dissecting aneurysm.
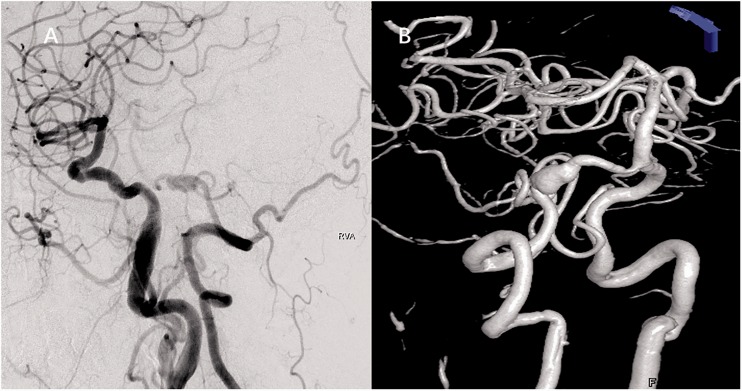
On admission, a routine digital subtraction angiography (DSA) was performed to confirm the diagnosis. However, due to the tortuosity of the BRA, the 5 F angled catheter failed to reach the orifice of the right vertebral artery (VA). The 5 F headhunter diagnostic catheter was chosen to access the right subclavian artery (RSA), but this also failed. Hence, we ultimately obtained the angiographic results by placing the tip of the diagnostic catheter in the BRA (Figure 1(a)), and the results indicated a right intradural VA dissecting aneurysm, measuring 12.3 mm × 7.2 mm (Figure 1(b)). With the patient and her relatives fearing an unfavorable outcome and due to the risks of occlusion of the parent artery, the PED was finally chosen to treat the aneurysm. Considering the difficulty navigating to the target vessel, we decided on radial artery cannulation for further deployment of the PED scheduled five days later. The treatment interval allowed the dual antiplatelet drug to take effect. In our department, for any given selective PED procedure, patients are given aspirin (100 mg) and clopidogrel (75 mg) daily for at least five days before the procedure. Allen’s test was thereafter performed to avoid ischemic event to the palm, and the result was negative.
Figure 1.
(a) Diagnostic digital subtraction angiography (DSA) revealing a right vertebral artery (VA) dissecting aneurysm. (b) Three-dimensional DSA image obtained in the following procedure depicting the aneurysm size.
The procedure was performed after inducing general anaesthesia in the patient. The right upper limb was supported by an armboard and abducted to an approximately 60° angle from the trunk. By palpitating the radial artery, puncture of the radial artery was performed approximately 2 cm cephalic to the radial styloid.
A 18 G needle was used to penetrate the double wall of the radial artery. After arterial entry was achieved, a 0.035-inch guidewire was inserted, and a 6 F artery sheath was introduced thereafter. Then a 6 F MPD guide catheter (Codman & Shurtleff, Inc., Raynham, MA) was navigated over the wire under fluoroscopy into the right subclavian artery and further placed in the VA.
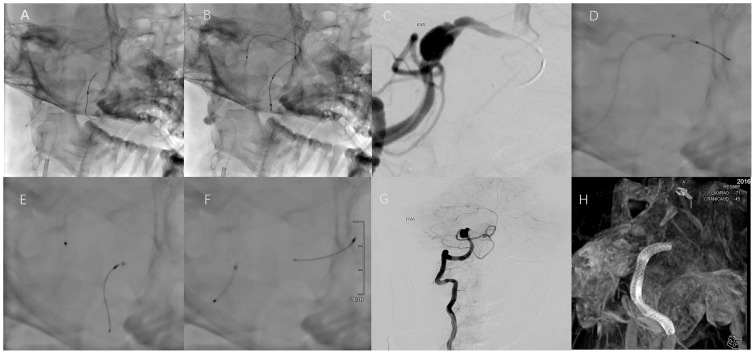
Using a coaxial system, the Marksman microcatheter (Covidien, Chicopee, MA) was navigated over a Traxcess 14 Guidewire (MicroVention, Inc., Tustin, CA) in the left VA beyond the aneurysm. At the vertebrobasilar junction, the wire and microcatheter were accidentally pushed into the contralateral VA instead of the basilar artery. Reviewing the angiogram again, the performer decided that it might be optimal to place the Marksman distally into the contralateral VA than into the basilar trunk as conventionally required. So the performer proceeded with the manoeuvre and advanced the Marksman until where the left VA enters the dural mater to provide adequate catheter support (Figure 2(a)). Then the delivery wire followed (Figure 2(b)), with a 3.25 mm × 30 mm PED (Covidien) being loaded. The distal end of the PED was opened in the contralateral VA and then retracted into its relatively horizontal part, as confirmed by DSA via the right VA (Figure 2(c)). Afterwards, the PED was deployed across the aneurysm through a process of repeating the unsheathing of the microcatheter and delivery wire stabilization/advancement. After the device was placed with full release, the microcatheter was advanced over the delivery wire to retrieve it (Figure 2(d)–(f)). A working angle angiogram indicated sufficient stasis of the angiographic agent (Figure 2(g)). Eventually, the operation was completed by performing the DynaCT angiography (Siemens, Munich, Germany) to confirm good opening of the device, as well as its apposition to the parent artery wall (Figure 2(h)).
Figure 2.
(a) and (b) The Marksman microcatheter and delivery wire were placed distally into contralateral VA. (c) and (d) Opening of the distal end of the Pipeline embolization device (PED). (e) and (f) Full release of the PED. (g) Stasis of the angiographic agent. (H) DynaCT indicates good opening of the device and apposition. This patient was discharged without any neurological deficit and was free from any complication related to radial access, including pulse discrepancy, decreased digital capillary refill or cold extremity development.
This patient was discharged without any neurological deficit and was free from any complication related to radial access, including pulse discrepancy, decreased digital capillary refill or cold extremity development.
Discussion
Conventionally accepted in the deployment of PED, the microcatheter must be advanced over the microwire past the aneurysm into the distal vasculature, that is, the M2 branch of the middle cerebral artery for aneurysms of the ICA, and P2 or P3 segments of the posterior cerebral artery for aneurysms located in the posterior circulation. Yet, in this case, the decision to advance the Marksman into the contralateral VA was made mainly due to the angio-architecture of the vertebrobasilar junction. The junction between the right VA and basilar artery is relatively narrow and sharp curved, retracting the distal-end opened PED through this curve might result in an unfavourable injury to the vessel and entailed significantly more technical effort. On the contrary, the junction between the right and left VA was apparently smoother, and the approaching part of these two arteries was located almost horizontally in a line (Figure 1(b)). In addition, navigating the Marksman into the VA instead of basilar trunk might lower the possibilities of stimulating the perforating arteries in the pons. So, during the procedure, when the microcatheter easily navigated into the contralateral VA, the surgeon decided not to redirect it into the basilar artery.
By far, we have treated 21 patients with 23 dissecting aneurysms located on posterior circulation. This is the only case where transradial access was chosen. Radial access for cerebral angiography or treatment has been proven safe and effective, especially for cases where femoral access to the right subclavian artery or right common carotid artery has either failed or would be difficult.4,5 In this case, transradial access was chosen mainly due to the tortuosity of the BRA and its inaccessibility transfemorally. But reviewing the case after the procedure, we tend to regard this access as favourable when you decide to advance the Marksman into contralateral VA instead of the distal segment of PCA, since this route results in less twisting of the guiding catheter and microcatheter than through transfemoral access. Yet, as this is the only case to be performed by placing the Marksman in the contralateral VA, we are uncertain whether this technique would be applicable in transfemoral access. However, we are reporting this technique in the hope that more options will be added to our arsenal of aneurysm treatment with PED.
Conclusion
We present a case in which the right VA was achieved via a combination of radial access and advancement of a PED into the left vertebral artery due to the specific angio-architecture of the patient. This technique may provide benefit in cases when minimal injury to the basilar artery as well as its branches is expected. Larger studies are required to validate this technique further.
Declaration of conflicting interests
The authors declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Funding
The authors received no financial support for the research, authorship and/or publication of this article.
References
- 1.Phillips TJ, Wenderoth JD, Phatouros CC, et al. Safety of the Pipeline embolization device in treatment of posterior circulation aneurysms. AJNR Am J Neuroradiol 2012; 33: 1225–1231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kuhn AL, Kan P, Massari F, et al. Endovascular reconstruction of unruptured intradural vertebral artery dissecting aneurysms with the Pipeline embolization device. J Neurointerv Surg 2016; 8: 1048–1051. [DOI] [PubMed] [Google Scholar]
- 3.Saatci I, Yavuz K, Ozer C, et al. Treatment of intracranial aneurysms using the Pipeline flow-diverter embolization device: a single-center experience with long-term follow-up results. AJNR Am J Neuroradiol 2012; 33: 1436–1446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nohara AM, Kallmes DF. Transradial cerebral angiography: technique and outcomes. AJNR Am J Neuroradiol 2003; 24: 1247–1250. [PMC free article] [PubMed] [Google Scholar]
- 5.Levy EI, Boulos AS, Fessler RD, et al. Transradial cerebral angiography: an alternative route. Neurosurgery 2002; 51: 335–340. discussion 40–42. [PubMed] [Google Scholar]