Abstract
Background and purpose
Different techniques regarding efficient utilization of thrombectomy devices have been reported. Here, we described a novel technique named ADVANCE that is based on advancing a distal access catheter over the stent retriever. In this study, we aimed to report our initial results with this novel thrombectomy technique.
Methods and results
Sixty-seven consecutive acute anterior circulation ischemic stroke patients (35 male, 32 female) between January 2015 and January 2016 who were treated by mechanical thrombectomy were included in this prospective study. Patients were classified randomly into two groups: patients treated with either the ADVANCE technique or standard technique. Patients had a mean age of 61.1 ± 12.9 years. The average NIHSS score was 15.8 ± 3.8. In the ADVANCE group, the successful revascularization (mTICI 2b–3) rate was 87.1% and the 90-day good functional outcome rate (mRS 0–2) was 74.1%. The revascularization rate in the ADVANCE group was significantly (p = 0.005) better than the standard technique group and good functional outcome at 90 days in the ADVANCE group was non-significantly better than the standard technique group (p = 0.052).
Conclusions
ADVANCE is the first comparison of this technique to standard stent retriever thrombectomy with a higher rate of revascularization with no emboli to new territory and fewer distal emboli to target territory. This safe and efficient technique needs to be validated in large patient series in new thrombectomy trials.
Keywords: Acute stroke, ADVANCE technique, interventional neurology, mechanical thrombectomy, novel technique
Introduction
With the publication of five randomized controlled trials in 2015, endovascular stroke therapy is shown to be highly effective within six hours of onset of acute ischemic stroke in patients with large artery occlusions.1–5 Better clinical outcomes were shown to correlate with effective revascularization in acute ischemic stroke.6 Despite increasing rates of revascularization with advances in device technology, additional efforts to establish new techniques to maximize the revascularization rates have been reported. In addition to the development of new devices, new techniques have been described to achieve better revascularization rates.7–10 We named this novel technique ADVANCE because the technique is based on advancing the distal access catheter (DAC) over the stent retriever. In this study, we aimed to report the effectiveness and feasibility of the ADVANCE thrombectomy technique.
Methods
This study was planned as a randomized prospective analysis of 67 consecutive acute stroke patients admitted to our neurology clinic with intracranial large arterial occlusions who received endovascular revascularization therapy (ERT) from January 2015 to January 2016, treated by either a standard (n = 31) or the ADVANCE (n = 31) thrombectomy technique. Patients were included in each group by simple randomization (toss of a coin). Patient demographic, angiographic, and clinical data were collected. This study was approved by the institutional research ethics board and the Ankara Numune Training and Research Ethics Committee. Written consent was obtained from the patients or their next of kin for participation in the study.
Patient selection
Inclusion criteria for routine clinical practice of acute stroke patients in our hospital were intracranial arterial occlusion within the anterior circulation, age limit 18–82, and baseline National Institutes of Health Stroke Scale (NIHSS) score of ≥6 at admission. Patients eligible for ERT within a time frame from symptom onset to treatment of ≤6 hours were treated with thrombectomy. All patients received intravenous (IV) tissue plasminogen activator (tPA) when eligible. Patients who had contraindication to IV tPA or presenting between 4.5 and 6 hours for anterior circulation strokes were treated with stand-alone thrombectomy.
Exclusion criteria for routine clinical practice acute stroke patients in our hospital were any intracranial hemorrhage, a cerebral infarction of a third or more of the middle cerebral artery (MCA) territory and absence of collateral circulation on computed tomography angiography (CTA) in the target territory. CTA was performed for all patients and intracranial arterial occlusion (ICA, MCA M1 or M2) was confirmed by CTA for the patients included.
Time points for groin puncture and revascularization times were recorded from time-stamped picture archiving and communication system images, and angiography nursing records.
There were five patients with vessel dissection or contrast extravasation due to microguide wire manipulation in the beginning of the procedure before advancing the DAC. In these cases, intervention was not continued and patients were transferred to intensive care unit. These patients were included for overall statistical analysis but excluded from technique-related statistical analysis as these complications occurred before advancing the DAC to the distal internal carotid artery (ICA) and were not thought to be attributed to the technique.
Imaging and clinical assessment
All angiographic images were re-evaluated by two neurointerventionalists blinded to the procedures. The degree of revascularization after treatment was defined by modified treatment in cerebral ischemia (mTICI) classification. Successful revascularization was defined as post-treatment mTICI score ≥ 2b.
Embolization in new territories (ENT) was defined as ≥1 new emboli to a territory different from the target territory and embolization of distal territories was defined as more than ≥1 new emboli in distal vessels beyond the thrombus in target territory.
Clinical assessments were performed at baseline with NIHSS score for assessing neurologic deficit and 90 days with modified Rankin Scale (mRS) for assessing global disability. A good functional outcome was defined as an mRS score of 0–2 at 90 days. Mortality was defined as death occurring within 90 days of initial presentation.
Symptomatic intracerebral hemorrhage was defined as presence of hemorrhage after treatment, with worsening of clinical examination by ≥ 4 points on NIHSS score.
A control non-enhanced CT scan was performed 24 hours after intervention or after clinical deterioration to rule out any intracranial hemorrhage. Procedural timings were taken from the angiographic records.
Endovascular procedure
The endovascular procedure was performed using femoral artery approach under local anesthesia. Heparin at a dose of 40 U/kg was administered after guiding sheath placement.
In all cases, triaxial system was used to deliver the stent retriever (Preset™, Phenox GmbH, Bochum, Germany, Solitaire FR™, ev3-Medtronic, Neurovascular, Irvine, CA, USA). A 6 Fr guiding catheter with an inner diameter of 0.087 inches (Destination™, Terumo, Tokyo, Japan) was placed distally into the ICA followed by the DAC (Navien™ Intra Cranial Support Catheter with a 0.058-inch distal inner diameter, ev3-Medtronic, Neurovascular, Irvine, CA, USA) that was advanced to the distal segments of the ICA, over a microcatheter (Rebar™ Reinforced Micro Catheter with a 0.027-inch distal inner diameter, ev3-Medtronic, Neurovascular, Irvine, CA, USA) and a 0.014-inch hydrophilic guidewire (Hi-Torque Whisper MS Guide Wire™, Abbott Vascular, Abbott Park, IL, USA).
After determining the occlusion site, a microcatheter was advanced through the thrombus distally over the microwire and superselective angiography via microcatheter was performed in order to determine the extent of the clot and to confirm that the microcatheter passed beyond the thrombus. The stent retriever was advanced and placed through the thrombus.
A DAC was used for all patients. We divided all patients randomly into two groups. In one group, we used the ADVANCE technique as described below; for the second group, we used a standard technique of pulling back the stent retriever under negative suction into the DAC, which was placed in the distal ICA.
ADVANCE technique
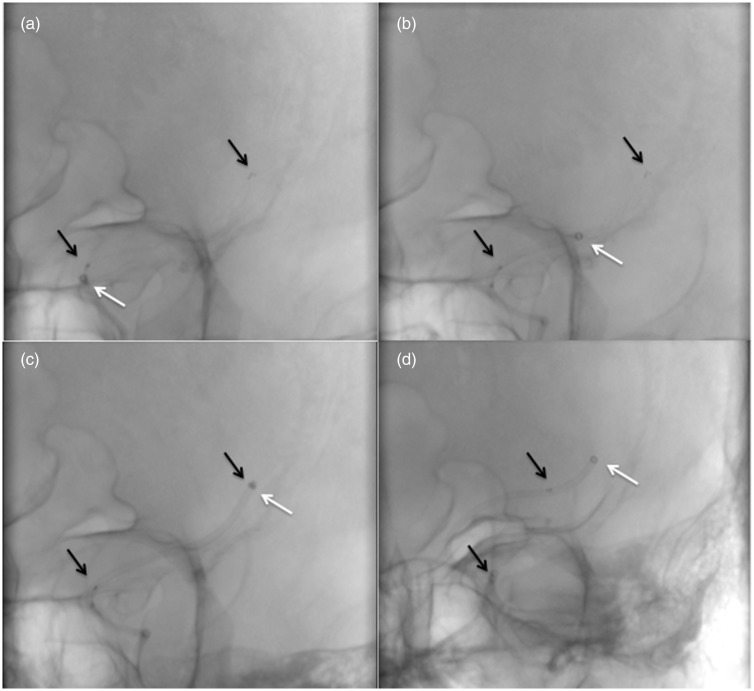
After placement of the guiding catheter in the ICA, a microguide wire and microcatheter were navigated and placed in the MCA distal to the thrombus. After ensuring that the microcatheter was placed distal to the thrombus, we waited for five minutes after stent deployment, then the DAC was advanced through the thrombus over the stent retriever (Figure 1(a) and (b) and Figure 2(a) and (b)) while creating manual negative suction with a 50 cc locked syringe. As soon as the DAC reached the distal tip of the stent retriever (Figure 1(c) and Figure 2(c)), the stent retriever was gently withdrawn (Figure 1(d) and Figure 2(d)) with continuous negative suction. When the stent retriever was totally removed, negative suction was continued through the DAC while slowly drawing back proximally. If blood flow was maintained, at least 20 ml of blood was withdrawn until no thrombus was seen in the withdrawn blood. If there was a blockade of blood flow in the DAC, then the DAC was totally removed under continuous suction. There was no technical failure in the ADVANCE group.
Figure 1.
(a)–(d) Schematic illustration of ADVANCE technique. In Figure 1(a), the distal access catheter (DAC) is advanced till the proximal marker of the stent retriever deployed in the thrombus located in the middle cerebral artery M1 segment. In Figure 1(b), the DAC is advanced over the stent retriever. In Figure 1(c), the DAC is pushed forward till the stent retriever distal marker and stent retriever together with thrombus are entrapped in the DAC. In Figure 1(d), the stent retriever is removed under negative suction without changing the position of the DAC.
Figure 2.
(a)–(d) Angiographic illustration of the ADVANCE technique. Positioning of the distal access catheter (DAC) (white arrow) and stent retriever (black arrow) is demonstrated in Figure 2(a) to 2(c). In Figure 2(d), the stent retriever is removed under negative suction without changing the position of the DAC.
Statistical analysis
The continuous variables that showed normal distribution were expressed as mean ± standard deviation and the numeric variables were expressed as median (minimum–maximum). Distribution of statistical numerical variables was analyzed by the Kolmogorov-Smirnov test. Similarity between group variances was tested using the Levene test. Differences between groups in terms of numerical variables were tested by Student t test in independent groups when parametric test assumptions were met and by Mann-Whitney U test if parametric test assumptions were not met. The relation between categorical variables was analyzed using chi square or Fisher’s exact test. Logistic regression analysis was used for mTICI revascularization and 90-day good functional outcome (mRS 0–2). All statistical analyses were performed using SPSS 22.0. A significant association was considered at a p value of <0.05.
Results
Sixty-seven acute ischemic stroke patients were treated by mechanical thrombectomy in a single stroke center including 35 male and 32 female patients with a mean age of 61.1 ± 12.9 (median 65 (26–82)) years. The average NIHSS score was 15.9 ± 3.9 with a median of 16 (6–25). The overall successful revascularization (mTICI 2b–3) rate was 76.1% and overall 90-day good functional outcome (mRS 0–2) was 64.1%. A total of 71.6% of patients (n = 48) had received IV tPA before the procedure. Demographic and clinical characteristics of all patients are summarized in Table 1. In the ADVANCE group, the revascularization rate (p = 0.005) was significantly better and number of patients with mRS 0–2 were better with a p value of 0.052. Revascularization time was shorter when compared with the standard technique group. There were no ADVANCE technique-related complications and no ENT and fewer embolization to distal territory. Other parameters are summarized in Table 2. Logistic regression analysis of factors affecting 90-day functional outcome (mRS 0–2) and mTICI revascularization 2b–3 is summarized in Table 3.
Table 1.
Clinical and demographic characteristics of all patients.
| Number of patients (n) | 67 |
| Age (mean ± SD) (min.–max.) | 61.1 ± 12.9 (26–82) |
| Sex (F/M) n (%) | 35/32 (52.2%/47.8%) |
| Comorbidity | |
| Coronary artery disease (%) | 35.8 |
| Diabetes mellitus (%) | 29.9 |
| Hyperlipidemia (%) | 14.8 |
| Hypertension (%) | 71.6 |
| Atrial fibrillation (%) | 31.3 |
| Smoking (%) | 20.9 |
| Basal NIHSS score at admission (mean ± SD) | 15.9 ± 3.9 |
F: female; M: male; NIHSS: National Institutes of Health Stroke Scale.
Table 2.
Comparison of clinical, demographic and outcome characteristics of standard and ADVANCE techniques.
| Standard technique (n = 31) | ADVANCE technique (n = 31) | p value | |
|---|---|---|---|
| Age (mean ± SD) (min.–max.) | 60.4 ± 14.6 | 59.9 ± 11.7 | 0.864 |
| Sex (F/M) (n (%)) | 16/9 (64%/36%) | 16/21 (43.2%/56.8%) | 0.179 |
| Basal NIHSS score at admission (mean ± SD) | 15.6 ± 3.7 | 16.0 ± 3.9 | 0.738 |
| Time between symptom onset and groin puncture (min) mean (min.–max.) | 180 (90–330) | 150 (90–330) | 0.424 |
| Revascularization time (min) (mean ± SD) | 64.0 ± 25.6 | 60.0 ± 25.0 | 0.543 |
| IV tPA (n (%)) | 18 (72%) | 27 (72.9%) | 0.605 |
| Rate of successful revascularization with one stent retriever attempt | 9 (29%) | 13 (41.9%) | 0.458 |
| Revascularization rate | |||
| mTICI 1–2a (n (%)) | 11 (35.4%) | 4 (12.9%) | 0.005 |
| mTICI 2b–3 (n (%)) | 20 (64.6%) | 27 (87.1%) | |
| 90-day clinical outcome | |||
| mRS 0–2 (n (%)) | 19 (61.2%) | 23 (74.1%) | 0.052 |
| mRS 3–5 (n (%)) | 7 (22.5%) | 4 (12.9%) | |
| mRS 6 (n (%)) | 5 (16.1%) | 4 (12.9%) | |
| Embolization | |||
| In new territory (n (%)) | 2 (6.4%) | 0 | 0.139 |
| In distal territory (n (%)) | 4 (12.9%) | 2 (6.4%) | |
F: female; M: male; NIHSS: National Institutes of Health Stroke Scale; IV tPA: intravenous tissue plasminogen activator; mTICI: modified treatment in cerebral ischemia; mRS: modified Rankin Scale.
Table 3.
Logistic regression analysis of factors affecting 90 day functional outcome (mRS 0–2) and mTICI revascularization 2b–3.
| Odds ratio (95% CI) | p | |
|---|---|---|
| Factors affecting 90-day functional outcome (mRS 0–2) | ||
| Time between symptom onset and groin puncture | 1.026 (0.996–1.058) | 0.093 |
| Time between symptom onset and revascularization time | 0.970 (0.944–0.998) | 0.033 |
| mTICI 2b– 3 | 12.119 (2.102–69.864) | 0.005 |
| Factors affecting mTICI revascularization 2b-3 | ||
| ADVANCE technique | 11.655 (1.737–78.181) | 0.011 |
mRS: modified Rankin Scale; mTICI: modified treatment in cerebral ischemia; CI: confidence interval.
Discussion
Efforts still aim to increase the revascularization rates with new devices and techniques in endovascular treatment of patients with acute ischemic stroke. ADVANCE is the first description of a thrombectomy technique with a very high rate of revascularization with no ENT and fewer distal emboli to target territory.
Benefits of ERT in acute ischemic stroke patients with large artery occlusion has been clearly demonstrated in recent years.1 Thrombectomy using stent retrievers has been the established device in acute ischemic stroke with large artery occlusion. Stent retrievers for acute ischemic stroke combine two mechanisms of action as follows: The deployment of the stent retriever within the clot immediately restores blood flow and then the mesh of the stent retriever embedded within the clot serves to catch and retrieve the clot.11
In recent stent-retriever trials, ERT has been shown to increase revascularization rates together with good neurological outcome.12 mTICI 2b–3 rates in these studies ranged from 58.7% to 88%. With the introduction of large-bore catheters with enhanced navigability, a technique called a direct-aspiration first-pass technique (ADAPT) has been reported.8,9 This technique is based on engaging the aspiration catheter into the clot and removing the clot by vacuum force applied with a syringe or aspiration pump. With this technique, complete revascularization was achieved in 57% of the cases. With the ADAPT for Acute Stroke Thrombectomy (FAST) study, the rate of mTICI 2b or 3 was 78% of cases where additional stent retriever use improved the revascularization rate up to 95%.7 Our study showed a similar revascularization rate of 87.1% in patients when the ADVANCE technique was used. Thus, for better rates of revascularization, stent retrievers and aspiration seems to be complementary rather than competitive.
Although revascularization still has a key role for determining good outcome, the rates of patients with mRS 0–2 in trials using stent retrievers and/or different techniques remain between 32% and 71%.1–5,13 In the ADAPT FAST study, despite a very high revascularization rate, patients with favorable clinical functional outcome remained at 40%, which is possibly due to long average time to groin puncture.7 In our opinion, differences in patient selection criteria would account for this discrepancy between these trials. In our study overall good clinical outcome was achieved in 64.1% of the patients.
Aspiration during stent retrieval was shown to decrease distal emboli rates, and manual aspiration with thrombectomy has been reported as a useful implementation in endovascular treatment of acute ischemic stroke.14
Some technical revisions during stent retriever use have been suggested in order to increase efficacy and decrease distal emboli. Use of a balloon-guiding catheter and flow blockade via balloon inflation during stent retrieval may help to decrease distal emboli.15 Analysis in The North American Solitaire Stent-Retriever Acute Stroke registry demonstrated better mTICI 3 revascularization (53.0% vs. 32.5%; p < 0.001) and higher rate of good clinical outcome (51.6% vs. 35.8%; p = 0.02) with balloon-guided catheter use (vs. guide catheter without balloon) whereas distal emboli and ENT rates were not different in both groups.16
After the use of DACs in routine clinical practice for distal intracranial vasculature, better revascularization rates with fewer distal emboli and ENT have been achieved.8–10 Once these catheters were placed in the distal ICA, they decrease the time for recurrent passes throughout all segments of the ICA while decreasing the risk of downstream detachment of the thrombus from the stent while pulling back in the arterial lumen through a shorter distance.
ADVANCE is a nonchallenging technique that requires only advancing the DAC over the stent wire and stent retriever till the distal tip of the stent retriever in addition to standard stent retriever use. In standard technique, the stent is retrieved together with the thrombus in the arterial lumen toward the DAC, which is placed usually in the distal ICA. During this maneuver, the risk of thrombus fragmentation especially in the curvatures can lead to detachment of thrombus from the stent resulting with distal emboli either to target territory or to new territory. ADVANCE combines the aspiration with stent retriever, which provides a synergistic effect. In our technique, instead of pulling back the thrombus toward the DAC, the DAC passes beyond the thrombus and the thrombus is confined in the DAC and the stent is retrieved inside the catheter under negative suction. In our opinion, it has a role to detach the attached thrombus from the arterial wall, while passing between the stent and arterial wall and local aspiration at the thrombus site possibly promotes entrapment of the thrombus in the DAC. As the flow blockage is maintained by placing the DAC distally, theoretically flow blockade together with suction reduce distal embolization especially in distal occlusions. Also, as the DAC is placed post-ICA bifurcation, it also prevents ENT (no ENT in our study vs. a 5%–9% rate of ENT in MR CLEAN,1 REVASCAT,5 SWIFT17 and TREVO18 trials). Thus, beyond its efficacy this poses an important advantage of prevention of emboli to target territory and especially to new territory. Theoretically in distal ICA occlusions, the thrombus can stay between the catheter and vessel wall when the DAC is advanced but in practice these thrombi could be easily captured and removed without any distal emboli.
In the HERMES analysis reported in the Journal of the American Medical Association, symptom onset to groin puncture was 238 minutes (interquartile range (IQR), 180–302), and symptom onset to reperfusion was 286 minutes (IQR, 215–363). This analysis showed that each one-hour delay in reperfusion was associated with a less favorable degree of disability and less functional independence. Although procedure time was similar when compared to the HERMES analysis, time from symptom onset to revascularization was shorter in the ADVANCE group. Together with high revascularization rates with the ADVANCE technique, shorter onset to revascularization times seem to influence good functional outcome rates, which were found to be better than reported in the HERMES analysis. Although additional imaging selection using perfusion imaging or collateral imaging in three of the five HERMES trials is a strategy that maximizes trial efficiency by focusing on patient groups with the greatest likelihood of benefit, in our opinion time from symptom onset to revascularization and revascularization rates are also among the major determinants of good functional outcome.19,20
Technique-related complications such as dissection or extravasation were not observed in any patients while advancing the DAC, although we already had distal occlusions such as distal M1 or M2 in the ADVANCE group. This supports the safety profile of our technique.
Limitations of our study include being a single-center experience with a relatively small number of patients with anterior circulation ischemic strokes.
Conclusion
The ADVANCE technique is a novel, efficient and safe technique that combines local aspiration and stent retriever use in patients with acute ischemic stroke due to large vessel occlusion. Although this technique was performed with ease and without complication in our study, new multicenter trials with large patient series are needed to confirm our results.
Declaration of conflicting interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
References
- 1.Berkhemer OA, Fransen PS, Beumer D, et al. MR CLEAN Investigators. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med 2015; 372: 11–20. [DOI] [PubMed] [Google Scholar]
- 2.Goyal M, Demchuk AM, Menon BK, et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med 2015; 372: 1019–1030. [DOI] [PubMed] [Google Scholar]
- 3.Campbell BC, Mitchell PJ, Kleinig TJ, et al. Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med 2015; 372: 1009–1018. [DOI] [PubMed] [Google Scholar]
- 4.Saver JS, Goyal M, Bonafe A, et al. Stent-retriever thrombectomy after intravenous t-PA vs. t-PA alone in stroke. N Engl J Med 2015; 372: 2285–2295. [DOI] [PubMed] [Google Scholar]
- 5.Jovin TG, Chamorro A, Cobo E, et al. Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med 2015; 372: 2296–2306. [DOI] [PubMed] [Google Scholar]
- 6.Rha JH, Saver JL. The impact of recanalization on ischemic stroke outcome: A meta-analysis. Stroke 2007; 38: 967–973. [DOI] [PubMed] [Google Scholar]
- 7.Turk AS, Frei D, Fiorella D, et al. ADAPT FAST study: A direct aspiration first pass technique for acute stroke thrombectomy. J Neurointervent Surg 2014; 6: 260–264. [DOI] [PubMed] [Google Scholar]
- 8.Turk AS, Spiotta A, Frei D, et al. Initial clinical experience with the ADAPT technique: A direct aspiration first pass technique for stroke thrombectomy. J Neurointerv Surg 2014; 6: 231–237. [DOI] [PubMed] [Google Scholar]
- 9.Kowoll A, Weber A, Mpotsaris A, et al. Direct aspiration first pass technique for the treatment of acute ischemic stroke: Initial experience at a European stroke center. J Neurointerv Surg 2016; 8: 230–234. [DOI] [PubMed] [Google Scholar]
- 10.Singh J, Wolfe SQ, Janjua RM, et al. Anchor technique: Use of stent retrievers as an anchor to advance thrombectomy catheters in internal carotid artery occlusions. Interv Neuroradiol 2015; 21: 707–709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wakhloo AK, Gounis MJ. Retrievable closed cell intracranial stent for foreign body and clot removal. Neurosurgery 2008; 62(5 Suppl 2): ONS390–ONS393. discussion ONS393–ONS394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hong KS, Ko SB, Lee JS, et al. Endovascular recanalization therapy in acute ischemic stroke: Updated meta-analysis of randomized controlled trials. Stroke 2015; 17: 268–281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Brinjikji W, Murad MH, Rabinstein AA, et al. Conscious sedation versus general anesthesia during endovascular acute ischemic stroke treatment: A systematic review and meta-analysis. Am J Neuroradiol 2015; 36: 525–529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jankowitz B, Aghaebrahim A, Zirra A, et al. Manual aspiration thrombectomy: Adjunctive endovascular recanalization technique in acute stroke interventions. Stroke 2012; 43: 1408–1411. [DOI] [PubMed] [Google Scholar]
- 15.Chueh JY, Kühn AL, Puri AS, et al. Reduction in distal emboli with proximal flow control during mechanical thrombectomy: A quantitative in vitro study. Stroke 2013; 44: 1396–1401. [DOI] [PubMed] [Google Scholar]
- 16.Nguyen TN, Malisch T, Castonguay AC, et al. Balloon guide catheter improves revascularization and clinical outcomes with the Solitaire device: Analysis of the North American Solitaire Acute Stroke Registry. J Neurointerv Surg 2014; 45: 141–145. [DOI] [PubMed] [Google Scholar]
- 17.Saver JL, Jahan R, Levy EI, et al. Solitaire flow restoration device versus the Merci Retriever in patients with acute ischaemic stroke (SWIFT): A randomised, parallel-group, non-inferiority trial. Lancet 2012; 380: 1241–1249. [DOI] [PubMed] [Google Scholar]
- 18.Nogueira RG, Lutsep HL, Gupta R, et al. Trevo versus Merci retrievers for thrombectomy revascularisation of large vessel occlusions in acute ischaemic stroke (TREVO 2): A randomised trial. Lancet 2012; 380: 1231–1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Saver JL, Goyal M, van der Lugt A, et al. Time to treatment with endovascular thrombectomy and outcomes from ischemic stroke: A meta-analysis. JAMA 2016; 316: 1279–1288. [DOI] [PubMed] [Google Scholar]
- 20.Goyal M, Menon BK, van Zwam WH, et al. Endovascular thrombectomy after large-vessel ischaemic stroke: A meta-analysis of individual patient data from five randomised trials. Lancet 2016; 387: 1723–1731. [DOI] [PubMed] [Google Scholar]