Abstract
Introduction:
The rate of caesarean delivery is increasing worldwide. Maternal beliefs may be influential on the mode of delivery. This study aimed to validate pregnant women's preferences for mode of delivery questionnaire among pregnant women.
Materials and Methods:
This was a cross-sectional study which was done in Ahvaz Public and Private Health Care Centers. A total of 342 low-risk pregnant women were included in a study conducted in spring 2011 in Ahvaz, Iran. After careful consideration and performing content and face validity, a 62-item measure was developed and subjects completed the questionnaire. Reliability was estimated using internal consistency and validity was assessed by performing face, content and structure and discriminate validity. Data were analyzed using explanatory factor analysis, t-test, and correlations in SPSS 16.
Results:
The findings of content and face validity showed almost perfect results for both content validity ratio = 1 and content validity index = 1. The explanatory factor analysis indicated a 7-subscale measure (Eigenvalue >1, factor loading >0.4), and discriminate validity revealed satisfying results P < 0.05 for 6 out of 7 subscales. Internal consistency as measured by the Cronbach's alpha coefficient was acceptable for subscales.
Conclusions:
In general, the findings suggest that this newly generated scale is a reliable and valid specific questionnaire for assessing pregnant women's preferences for mode of delivery. However, further studies are needed to establish stronger psychometric properties for the questionnaire.
Keywords: Mode of delivery, pregnancy, psychometric, reliability, validity
INTRODUCTION
Mode of delivery method is defined as choosing either the vaginal or caesarean section (C-section) delivery.[1] Vaginal delivery is the natural method of birth, though about 10% of normal deliveries may be complicated, caesarean section delivery is suggested to prevent either maternal or fetal morbidities and mortality.[2,3,4] However, nowadays, many C-sections are performed upon maternal request with no medical cause.
The rate of caesarean section delivery is rising worldwide. In some countries, it becomes a part of their culture.[5,6] World Health Organization (WHO) recommended that no more than 10–15% of pregnancies should be terminated by C-section.[7] Some individual and cultural factors may affect the rate of C-section.[8] The term “elective caesarean section delivery” refers to those C-section deliveries which are performed with no medical cause.[9]
It has been well documented that mortality and morbidity for C-section deliveries are greater than normal vaginal delivery. C-section delivery, also, increases the expenses up to 3 times.[10]
Protecting mothers from unnecessary medical technologies is one of the WHO strategies to promote maternal health.[11] International Confederation of midwives has announced that performing caesarean section deliveries with no medical indication is immoral.[12] Although reducing the rate of elective C-section delivery has been considered by health professionals’ authorities, this rate is increasing in some countries.[13]
In the USA, caesarean delivery rate increased from 20/7% in 1996 to 31/1% in 2006 and to 32/9% in 2009.[14] In Arab countries, also, this rate is reported to be 15%.[15] According to the results of a study this rate, in Iran, is about 50% showing Iran is far from the WHO C-section advocated rate; therefore, it seems to be crucial to conduct studies to focus on the reasons of such increases and to promote programs to reduce this health issue.[14] Considering C-section as a behavior; before any intervention to reduce the rate of C-sections deliveries, it is essential to understand the reasons for this behavior.[2] Because of the importance of the values and beliefs in directing behavior, understanding underlying elements of behavior are necessary to promote any health promotion program. As such, a valid and reliable tool is needed to extract personal values and beliefs. Taking the previous studies and researches into consideration, there is no exact measure on maternal beliefs. Only two studies which are mostly focused on the cognitive aspects of behavior are exist. Considering the fact that the nature of human behavior is very complex as many psychosocial factors are affecting it, the available tools are not provide enough reasons to extract maternal influential factors on mode of delivery.[2,16]
Therefore, designing a reliable and valid questionnaire to extract the psychological factors related to the women's preferences for mode of delivery seems to be more essential. To do so, the results of previous studies can be very helpful.[17] Fear and anxiety are one of the most frequent reasons to choose C-section women might consider themselves at risk of probable morbidities.[5,18,19,20] Many studies confirmed that negative beliefs are the main reasons for choosing any mode of delivery.[9,21]
Such beliefs, as perceived threat, as well as evaluating the benefits or risks, are the key constructs of health belief model (HBM). This model which is based on the behavioral sciences theory is an interpersonal health education model which is composed of theoretical constructs as perceived susceptibility, perceived benefit, perceived barriers, and self-efficacy.[20] In addition to these factors, some researchers believe that pain intolerance also is another effective factor on choosing the delivery mode. That is to say that this factor is inconsistent with the self-efficacy constructs in HBM.[22,23]
Based on above-mentioned results, HBM can be an appropriate model to design the materials. Since it is unlikely that one specific model can predict the behaviors appropriately, it is recommended that for having more comprehensive understanding, other components and beliefs might be taken into consideration, too. In this regard, some studies demonstrated that physicians’, midwifes’, and relatives’ ideas, as well as following the fashion are very significant factors in choosing C-section delivery.[5,15,24] This concept is consistent with the construct of normative beliefs which is found within the theory of planned behavior.
Hence, the aim of this study was to develop a questionnaire to access pregnant women's preferences for mode of delivery. It was hoped this might help to fill the gaps and perhaps contribute to the existing literature on the topic.
MATERIALS AND METHODS
This was a cross-sectional study carried out in 2011 in Ahvaz the South West of Iran Public and Private Health Care Centers. Combining the previous theory-based questionnaires, as well as studying the related text books; the researchers made a questionnaire which was piloted in a small sample of pregnant women. Internal consistency was measured (Cronbach’ alpha: 0/70). Several methods were used so as to verify the validity and the reliability of the questionnaire as: (1) Extracting items from the related texts and questionnaire and interviewing with the women. (2) Estimating the content validity based on the experts’ viewpoints. (3) Evaluating face validity based on the pregnant women's ideas. (4) Using exploratory factor analysis (EFA) to assess the construct validity. (5) Measuring discriminate validity. (6) Evaluating the reliability using Cronbach’ alpha.
In the first stage, having used the published texts, also, based on the viewpoints of the professional faculty members, the researchers designed a questionnaire consisting of 62-item questionnaire. These questions which were based on some constructs of HBM and normative beliefs of the theory of planned behavior were designed to evaluate factors affecting the mode of delivery.
In order to, qualitatively measure content validity, in the second stage, the questionnaire was given to 10 experts and their corrective ideas were applied. Then, content validity ratio (CVR) and content validity index (CVI) were calculated to assess the validity quantitatively. The results, then, were used to ensure researchers from the best selection of the items. In so doing, 10 experts including 4 health education experts, 4 midwives, and 2 health experts were asked to answer the questions arranged in three levels (necessary, useful but not necessary, and unnecessary).
Based on their answers, CVR was calculated. For each question, CVR acceptable quality limit was more than 62%.[20] The quantitative face validity was evaluated through impact score. The impact score for each item was calculated as multiplying the importance of an item with its frequency. The impact scores of >1.5 were considered suitable. In order to measure CVI, the questions were reviewed by a panel of experts and rated on simplicity, relevance, and clarity on a four-point Likert-type scale The CVI of each statement was calculated and as recommended values of ≥0.80 were considered acceptable.[20] At the end, 49 questions remained. Each item is rated on a five-point Likert scales ranging from strongly agree to strongly disagree giving a possible score of 1–5 for each item.
In the third step, to measure the construct validity and, also, to determine the factor structure of the questionnaire, at first, the questionnaires were given to 342 nonrandom pregnant women referred to Public and Private Health Care Centers. The inclusion criteria were: being aged 18–35-year-old, having the history of pregnancy without adverse outcomes, not suffering from chronic diseases during the present pregnancy and not having the history of fertility problems. Demographic characteristics of the pregnant women included recording of age, education of pregnant women and their husbands, gestational age, and family monthly income.
Statistical analysis
Data were analyzed applying descriptive and inferential tests using SPSS 15 (SPSS, Inc., Chicago, IL, USA) software. EFA was done to identify the underlying relationships between measured variables. A set of observed variables was used to identify a set of latent constructs. To determine the adequacy of the sample size, Kaiser–Meyer–Olkin test was applied. A threshold of >0.4 for corrected item-total-correlation was chosen sufficient.[25]
Discriminant validity
Discriminant validity of the instrument was assessed using known groups comparison. Known groups comparison was performed to test how well the questionnaire discriminates between pregnant women with the different intention for their mode of delivery with no medical reason (either C-section or vaginal delivery). 112 women (31/6%) chose C-section delivery, and 120 participants (33/9%) chose vaginal delivery as their definite preference. T-test, also, was used to verify the discriminated validity between these two groups.
Reliability
Internal consistency of the instrument was assessed by using Cronbach's alpha coefficient. Alpha values of ≥0.70 were thought satisfactory. However, item correlation with intended factors was assessed to calculate reliability (P < 0.05).
Ethics
The ethics committee of Ahvaz Jundishapur University of Medical Sciences approved the study. Informed consent was obtained from participants.
RESULTS
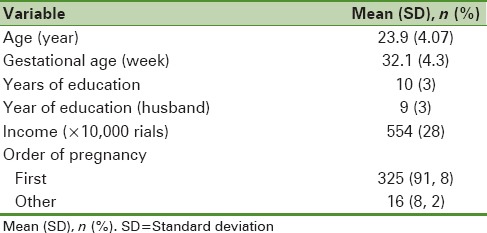
In total, 342 pregnant women completed the questionnaire. The mean age of women was 23.9 (±4.07) years, and the mean gestational age was 32.1 (±4.3) weeks. The characteristics of participants’ demographic characteristics are shown in Table 1.
Table 1.
Demographic characteristics of the study population
The results obtained from validity analysis showed good levels of the CVR (0.86), CVI (0.84), and impact score (IS = 5) for items. In the qualitative face validity, all participants acknowledged that they had no problems in reading and understanding the items. After content validity phase, 42 items were remained for the next stage of validation process.
The result of Kaiser–Meyer–Olkin measure of sampling adequacy test was 0.738, showing the adequacy of the sample size for factor analysis.
The principal component analysis with VARIMAX rotation was performed for the items resulting in a seven factor solution. Table 2 shows the rotated factor matrix of these seven factors and indicates the factor loading of each of 21 items.
Table 2.
The results of the factor analysis for exploring the key factors with rotated VARIMAX from a questionnaire, which evaluates the related factors with the mode of delivery, and internal consistency (Cronbach’ alpha) among pregnant women
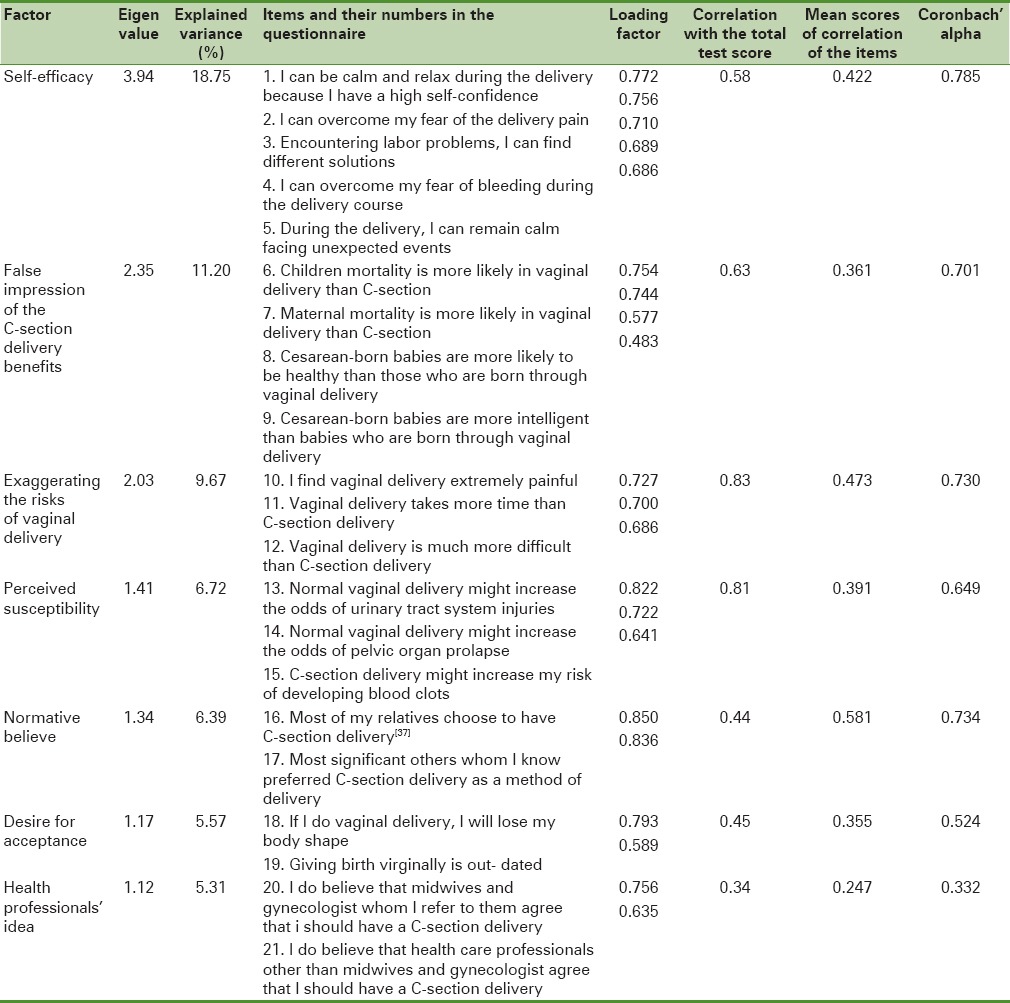
Factors were named so that they could reflect underlying measured variables. Accordingly, these seven factors were named as: (1) Self-efficacy (5 items), (2) False impression of the benefits of C-section delivery (4 items), (3) Exaggerating the risks of vaginal delivery (3 items), (4) Perceived susceptibility (3 items), (5) Normative beliefs (2 items), (6) Desire for acceptance (2 items) and (7) Health professionals’ idea (2 items). 63.619% of the total variance was explained by these seven factors.
To measure the discriminate validity, in Table 3, the scores of each factor were compared between different groups based on their intention to either vaginal or C-section. The results of the t-test indicated that these factors showed a significant difference between the pregnant women who chose C-section delivery and those whose selection was vaginal birth in self-efficacy, false impression of the benefits of C-section delivery, exaggerating the risks of vaginal delivery, perceived susceptibility, normative beliefs, desire for acceptance, and even in total score (P = 0.001).
Table 3.
Discriminate validity of the explored factors in two groups based on their intention for mode of delivery
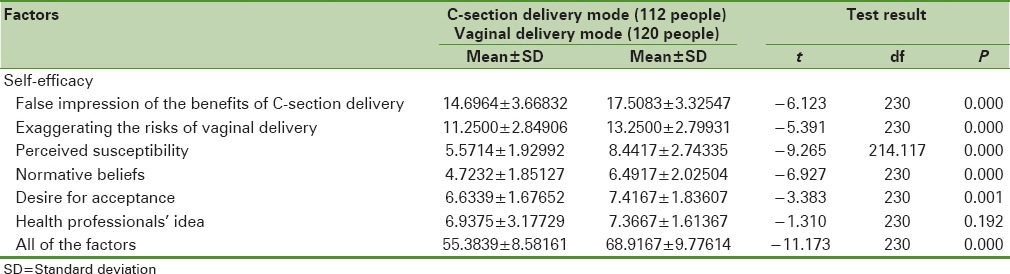
However, such difference was not found concerning the health professionals’ idea factor (P = 0.19). The mean scores of the second group in all these dimensions were higher. Generally, the mean score of the total factors in a group choosing vaginal delivery were more than those of the group that will undergo C-section delivery, 68.92 ± 9.78 and 55.38 ± 8.58, respectively [Table 3].
Cronbach’ alpha (internal consistency) for all 21 items in the questionnaire was 0.747. This number for self-efficacy, false impression of the benefits of C-section delivery, exaggerating the risks of vaginal delivery, and normative beliefs were more than 0.7, indicating that all these dimensions had high internal reliability. Other dimensions as perceived susceptibility, desire for acceptance, and health professionals’ idea showed other results (0.649, 0.534, and 0.332, respectively) [Table 2].
DISCUSSION
The aim of this study was to evaluate the overall psychometric properties of pregnant women's preferences for mode of the delivery questionnaire. Based on the findings, the developed questionnaire revealed seven factor solutions. So far no specific research has been found focusing exclusively on the behavioral beliefs related to the mode of delivery.
The first extracted subscale from factor analysis was self-efficacy. In fact, this is a key construct within many health education theories and seems to be the most fundamental behavioral constructs related with the choice of delivery method.[25,26,27,28,29,30,31,32] Self-efficacy refers to an individual's perception of his or her competence to successfully perform a specific behavior. It is driven from both Bandura's social learning theory. Self-efficacy can predict health behaviors. Given any sort of behavior, it can motivate individuals to engage in the behavior or even to change that behavior. Therefore, recognizing this construct would help to better explain individual differences in health behaviors.[22,23]
The second and the third extracted factors were false perception of the benefits of C-section delivery and exaggerating the risks of vaginal birth, respectively.[30] In spite of the fact that, in many studies, it is demonstrated that both the mother and the baby are more at risk in C-section delivery than vaginal birth, many people still perceive C-section delivery as having less risks than vaginal delivery.[9] Penna et al. in their studies showed that high socioeconomic class and awareness of delivery time were the other important reasons for women choosing C-section delivery.[7,30] Therefore, it seems that providing appropriate educational program can help pregnant women to perceive the advantages and disadvantages of vaginal delivery and C-section.
Therefore, it seems necessary that pregnant women be taught truly about the advantages and disadvantages of C-section delivery. With colleagues, Penna and Soltani and Sandall in their studies showed that social welfare and controlling the exact time of delivery and hospital release were the main reasons for women's tendency toward C-section delivery.[7,30]
Perceived susceptibility was identified as the fourth factor. It refers to one's perception of the risk or the chances of contracting a health disease or condition. Individuals who perceive that they are susceptible to a particular health problem will engage in behaviors to reduce their risk of developing a health problem. Hajian et al. found that if individuals know about the risks of C-section delivery, it is more probable that they, when having no medical indications, choose vaginal delivery.[19]
As consistent with the findings of this research, in another study by Penna and Arulkumaran, Liu et al., and Angeja et al. normative belief was found as an important factor impacting on the pregnant women's decision making of the mode of delivery.[5,30,32] The ideas of the women's spouse, family, friends, and close others are very influential. That is why such people, also, should be invited to educational classes.
The sixth factor was a desire for acceptance. Although this factor is not mentioned in any behavioral model,[23] the item of distorted body image is a variable mentioned in other studies.[33,34]
Health professionals’ idea was the last extracted factor. Although results of discriminate validity showed no significant differences between the women choosing C-section delivery and those who chose vaginal delivery, this factor was found to be influential in the studies of Turner et al. and Guittier et al.[35,36,37] In their studies, Turner et al. showed that the ideas of midwives were very effective in choosing the mode of delivery.[37] One possible explanation for nonsignificant discriminate validity for this subscale might be due to the fact that while other studies considered midwives’ idea, this study investigated all health professional's idea. Since the personnel's ideas can change the pregnant women's preferences for the mode of delivery, it is very necessary that some educational classes, focusing on the morals and social skills, be held for the health professionals too.[7]
In spite of the fact that the Cronbach’ alpha and reliability of all factors were in high levels, desire for acceptance showed a weak reliability. Moreover, the individual's perception of the health professionals was unacceptable in terms of reliability. Taking Cramines's and Zeller's ideas into consideration, the number of items are one of the important factors constructing alpha Cronbach's level, such result can be justified since these two factors had only 2 questions. They, also, believe that mean correlation of the items is another way to evaluate reliability. In their cross table, they suggested expected alpha between 0.333 and 0.572. Having only 2 items, acceptability orientation with the mean correlation of 0.355 showed a higher alpha, 0.524. According to this theory, if the number of questions become double,[4] alpha will be between 0.5 and 0.727. This number, also, will change to 0.60–0.80 if the questions become six.[38] Based on the Cromines's idea, expected alpha for the personnel's idea, having 2 items and mean correlation of 0.247, should be about 0.333. In this study, it was measured as 0.332.
If the numbers of the items change to 4 or 6, alpha levels will increase up to 0.500 or 0.600. Many experts believe that with the increase in the sample size, the alpha coefficient would increase too.[39] It is recommended, then, that in the further studies the effect of the above-mentioned factors be examined.
Limitation
Not to conduct confirmatory factor analysis is the study's limitation.
CONCLUSIONS
In general, the findings suggest that this newly generated scale is a reliable and valid specific questionnaire for assessing pregnant women's preferences for mode of delivery. However, further studies are needed to establish stronger psychometric properties for the questionnaire.
Financial support and sponsorship
Ahvaz Jundishapur University of Medical Sciences.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
The authors wish to express their deepest appreciation to those pregnant women who participated in this study. This research was a secondary analysis of data obtained from research project with the grant number of 485 which was approved by the Social Determinants of Health Research Center, Ahvaz Jundishapur University of Medical Sciences, and the official support from the university is also acknowledged.
REFERENCES
- 1.Belizán JM, Althabe F, Cafferata ML. Health consequences of the increasing caesarean section rates. Epidemiology. 2007;18:485–6. doi: 10.1097/EDE.0b013e318068646a. [DOI] [PubMed] [Google Scholar]
- 2.Mungrue K, Nixon C, David Y, Dookwah D, Durga S, Greene K, et al. Trinidadian women's knowledge, perceptions, and preferences regarding cesarean section: How do they make choices? Int J Womens Health. 2010;2:387–91. doi: 10.2147/IJWH.S12857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kushtagi P, Guruvare S. Documenting indications for cesarean deliveries. J Postgrad Med. 2008;54:52–3. doi: 10.4103/0022-3859.39195. [DOI] [PubMed] [Google Scholar]
- 4.Rozenberg P. Evaluation of cesarean rate: A necessary progress in modern obstetrics. J Gynecol Obstet Biol Reprod (Paris) 2004;33:279–89. doi: 10.1016/s0368-2315(04)96456-3. [DOI] [PubMed] [Google Scholar]
- 5.Angeja AC, Washington AE, Vargas JE, Gomez R, Rojas I, Caughey AB. Chilean women's preferences regarding mode of delivery: Which do they prefer and why? BJOG. 2006;113:1253–8. doi: 10.1111/j.1471-0528.2006.01069.x. [DOI] [PubMed] [Google Scholar]
- 6.Badakhsh MH, Seifoddin M, Khodakarami N, Gholami R, Moghimi S. Rise in cesarean section rate over a 30-year period in a public hospital in Tehran, Iran. Arch Iran Med. 2012;15:4–7. [PubMed] [Google Scholar]
- 7.Soltani H, Sandall J. Organisation of maternity care and choices of mode of birth: A worldwide view. Midwifery. 2012;28:146–9. doi: 10.1016/j.midw.2012.01.009. [DOI] [PubMed] [Google Scholar]
- 8.Althabe F, Belizán JM. Caesarean section: The paradox. Lancet. 2006;368:1472–3. doi: 10.1016/S0140-6736(06)69616-5. [DOI] [PubMed] [Google Scholar]
- 9.Cunningham F, Leveno K, Bloom S, Spong CY, Dashe J. Williams Obstetrics 24/E. 24th ed. New York, USA: McGraw Hill Professional; 2014. [Google Scholar]
- 10.Lavender T, Hofmeyr GJ, Neilson JP, Kingdon C, Gyte GM. Caesarean section for non-medical reasons at term. Cochrane Database Syst Rev. 2012;3:CD004660. doi: 10.1002/14651858.CD004660.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nouri TS. Relationship of knowledge and attitude with reasons for cesarean selection among pregnant women of Rasht health centers that were applicant for cesarean. J Guilan Univ Med Sci. 2006;15:75–84. [Google Scholar]
- 12.Devendra K, Arulkumaran S. Should doctors perform an elective caesarean section on request? Ann Acad Med Singapore. 2003;32:577–81. [PubMed] [Google Scholar]
- 13.Pezeshki Z, Pezeshk S. Educating quaternary prevention (P4) in Iran for decreasing the harms and costs of unnecessary services in clinical medicine and public health. Payesh. 2013;12:329–32. [Google Scholar]
- 14.Tita AT, Landon MB, Spong CY, Lai Y, Leveno KJ, Varner MW, et al. Timing of elective repeat cesarean delivery at term and neonatal outcomes. N Engl J Med. 2009;360:111–20. doi: 10.1056/NEJMoa0803267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jurdi R, Khawaja M. Caesarean section rates in the Arab region: A cross-national study. Health Policy Plan. 2004;19:101–10. doi: 10.1093/heapol/czh012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jacquemyn Y, Ahankour F, Martens G. Flemish obstetricians’ personal preference regarding mode of delivery and attitude towards caesarean section on demand. Eur J Obstet Gynecol Reprod Biol. 2003;111:164–6. doi: 10.1016/s0301-2115(03)00214-8. [DOI] [PubMed] [Google Scholar]
- 17.Narimani MR, Tabrizi JS, Amini A, Shaghaghi A, Asghari-Jafarabadi M, Aydilou NA. Development and psychometric properties of a new tool to assess justification and practice of patient rights (JPPR) J Clin Res Gov. 2014;3:81–91. [Google Scholar]
- 18.Bagheri A, Masoudi Alavi N, Abbaszadeh F. Iranian obstetricians’ views about the factors that influence pregnant women's choice of delivery method: A qualitative study. Women Birth. 2013;26:e45–9. doi: 10.1016/j.wombi.2012.09.004. [DOI] [PubMed] [Google Scholar]
- 19.Hajian S, Shariati M, Najmabadi KM, Yunesian M, Ajami ME. Psychological predictors of intention to deliver vaginally through the extended parallel process model: A mixed-method approach in pregnant Iranian women. Oman Med J. 2013;28:395–403. doi: 10.5001/omj.2013.115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Araban M, Tavafian SS, Motesaddi Zarandi S, Hidarnia AR, Gohari MR, Prochaska JM, et al. Introducing a new measure for assessing self-efficacy in response to air pollution hazards for pregnant women. J Environ Health Sci Eng. 2013;11:16. doi: 10.1186/2052-336X-11-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ghotbi F, Akbari Sene A, Azargashb E, Shiva F, Mohtadi M, Zadehmodares S, et al. Women's knowledge and attitude towards mode of delivery and frequency of cesarean section on mother's request in six public and private hospitals in Tehran, Iran, 2012. J Obstet Gynaecol Res. 2014;40:1257–66. doi: 10.1111/jog.12335. [DOI] [PubMed] [Google Scholar]
- 22.Bandura A. Self-efficacy: Toward a unifying theory of behavioral change. Psychol Rev. 1977;84:191–215. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- 23.Glanz K, Rimer BK, Viswanath K. Health Behavior and Health Education: Theory, Research, and Practice. 4th ed. San Francisco, CA: John Wiley & Sons; 2008. [Google Scholar]
- 24.Yazdizadeh B, Nedjat S, Mohammad K, Rashidian A, Changizi N, Majdzadeh R. Cesarean section rate in Iran, multidimensional approaches for behavioral change of providers: A qualitative study. BMC Health Serv Res. 2011;11:159. doi: 10.1186/1472-6963-11-159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Munro BH. Statistical Methods for Health Care Research. London: Lippincott Williams & Wilkins; 2005. [Google Scholar]
- 26.Khorsandi M, Asghari Jafarabadi M, Jahani F, Rafiei M. Cultural adaptation and psychometric testing of the short form of Iranian childbirth self efficacy inventory. Iran Red Crescent Med J. 2013;15:e11741. doi: 10.5812/ircmj.11741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Khorsandi M, Ghofranipour F, Faghihzadeh S, Hidarnia A, Bagheban AA, Aguilar-Vafaie ME. Iranian version of childbirth self-efficacy inventory. J Clin Nurs. 2008;17:2846–55. doi: 10.1111/j.1365-2702.2008.02385.x. [DOI] [PubMed] [Google Scholar]
- 28.Zamani F, Shahry P, Kalhori M. Factors influencing cesarean section: A theory based study. Daneshvar. 2011;19:1–10. [Google Scholar]
- 29.Lowe NK. Maternal confidence for labor: Development of the childbirth self-efficacy inventory. Res Nurs Health. 1993;16:141–9. doi: 10.1002/nur.4770160209. [DOI] [PubMed] [Google Scholar]
- 30.Penna L, Arulkumaran S. Cesarean section for non-medical reasons. Int J Gynaecol Obstet. 2003;82:399–409. doi: 10.1016/s0020-7292(03)00217-0. [DOI] [PubMed] [Google Scholar]
- 31.Ip WY, Tang CS, Goggins WB. An educational intervention to improve women's ability to cope with childbirth. J Clin Nurs. 2009;18:2125–35. doi: 10.1111/j.1365-2702.2008.02720.x. [DOI] [PubMed] [Google Scholar]
- 32.Liu NH, Mazzoni A, Zamberlin N, Colomar M, Chang OH, Arnaud L, et al. Preferences for mode of delivery in nulliparous Argentinean women: A qualitative study. Reprod Health. 2013;10:2. doi: 10.1186/1742-4755-10-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Fenwick J, Staff L, Gamble J, Creedy DK, Bayes S. Why do women request caesarean section in a normal, healthy first pregnancy? Midwifery. 2010;26:394–400. doi: 10.1016/j.midw.2008.10.011. [DOI] [PubMed] [Google Scholar]
- 34.Yilmaz SD, Bal MD, Beji NK, Uludag S. Women's preferences of method of delivery and influencing factors. Iran Red Crescent Med J. 2013;15:683–9. doi: 10.5812/ircmj.11532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Guittier MJ, Cedraschi C, Jamei N, Boulvain M, Guillemin F. Impact of mode of delivery on the birth experience in first-time mothers: A qualitative study. BMC Pregnancy Childbirth. 2014;14:254. doi: 10.1186/1471-2393-14-254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mazzoni A, Althabe F, Liu NH, Bonotti AM, Gibbons L, Sánchez AJ, et al. Women's preference for caesarean section: A systematic review and meta-analysis of observational studies. BJOG. 2011;118:391–9. doi: 10.1111/j.1471-0528.2010.02793.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Turner CE, Young JM, Solomon MJ, Ludlow J, Benness C, Phipps H. Vaginal delivery compared with elective caesarean section: The views of pregnant women and clinicians. BJOG. 2008;115:1494–502. doi: 10.1111/j.1471-0528.2008.01892.x. [DOI] [PubMed] [Google Scholar]
- 38.Corrigan JD. Development of a scale for assessment of agitation following traumatic brain injury. J Clin Exp Neuropsychol. 1989;11:261–77. doi: 10.1080/01688638908400888. [DOI] [PubMed] [Google Scholar]
- 39.Hajizadeh E, Asghari M. Statistical methods and analysis in health and biosciences a research methodological approach. Tehran: Jahade Daneshgahi Publications; 2011. [Google Scholar]


