Abstract
Background:
No previous study exists to evaluate serum phosphorus (Ph) level as a predictor of the need to mechanical ventilation (MV). This study was designed to determine the predictive ability of admission serum Ph level on MV in patients admitted in Intensive Care Unit (ICU).
Materials and Methods:
This prospective study was conducted on 100 patients (>16 years old), admitted to our ICU over 1-year. Patients were classified into two groups according to the days of the need to MV. Group A: Patients who required equal or <5 days MV, and Group B: Patients who required more than 5 days of MV. We measured total serum Ph concentrations at the times of ICU admission, connecting to the ventilator and weaning from the ventilator.
Results:
There were significant differences between serum Ph concentration on admission to ICU (Group A: 3.39 ± 0.39 mg/dl, Group B: 2.89 ± 0.31 mg/dl, P < 0.001), at the time of connecting to ventilator (Group A: 2.49 ± 0.38 mg/dl, Group B: 2.25 ± 0.26 mg/dl, P = 0.004) and weaning from ventilator (Group A: 3.42 ± 0.33 mg/dl, Group B: 2.98 ± 0.34 mg/dl, P < 0.001) between two groups. Duration of ICU stay in Group A was 6.08 ± 1.48 days and in Group B was 15.35 ± 6.45, this difference was significant (P < 0.001). We found the best cut-off point of 3.07 for serum Ph concentration to predict the longer duration of MV.
Conclusion:
According to the results of our study, hypophosphatemia may increase the need to MV. Therefore, monitoring serum Ph level is a good prognostic factor to predict the need to ventilation.
Keywords: Critically ill patient, hypophosphatemia, mechanical ventilation, phosphorus, sequential organ failure assessment score
Introduction
Mechanical ventilation (MV) is a supportive therapy for patients with acute respiratory failure.[1]
Most critically ill patients with multiple organ failures need MV to support their respiratory failure.[2] However, prolonged MV is associated with numerous life-threatening complications such as tracheal stenosis, barotraumas, pneumothorax, and sepsis.[3] Therefore in critically ill patients, elimination of predisposing illness, successful management and weaning from ventilator, are key survival factors[4,5,6,7]
Patients who have been receiving prolonged time MV may have many problems in one or more areas, which should be corrected. One of these areas may be electrolyte abnormalities such as hypokalemia, hypophosphatemia, hypomagnesemia, hyponatremia, and hypocalcemia.[1,2,3,4,5,8]
Phosphorus (Ph) is one of the most important intra and extracellular ion. The normal range of Ph is between 2.5–4 mg/dl and a large portion of it is intracellular. The extracellular part of Ph has less importance because the extracellular fluid acts as a media for movement of Ph into the cells. Maintenance of serum Ph level in normal range is vital for cellular functions.[9,10]
Significant hypophosphatemia may be occurred without low serum Ph level, thus sever and life-threatening hypophosphatemia may not be diagnosed, because it has nonspecific manifestations such as loss of consciousness, hypotension, muscular weakness, ventilator dependence and acute respiratory failure.[9]
For assessment of organ function impairment in a clinical trial and observational studies a scoring system is usually used. The sequential organ failure assessment (SOFA) score is one of the most important scoring systems, which is commonly used to assess the severity of illness and predict the outcome of critically ill patients. The scoring systems may identify high-risk groups among the critically ill patients, to whom therapeutic interventions may be directed in order to reduce morbidity and mortality.[2,8,10] The predictive value of SOFA scores as a dynamic, simple and inexpensive marker in critically ill patients who require MV, has been studied by few authors.[8]
Brunelli and Goldfarb reported that hypophosphatemia was seen in approximately 28–33% of patients admitted to an Intensive Care Unit (ICU); their study clearly explained that adequate serum Ph level is associated with successful weaning from ventilator.[11]
Doig et al. also reported that 37% of 2915 studied patients developed hypophosphatemia during their ICU stay, with 50% of cases encountered during the first 8 days of ICU admission. In these patients, the average serum Ph level was 1.63 mg/dl. This study showed the relationship between severities of hypophosphatemia with duration of ICU stay and MV, but hospital stay days and mortality rate were not significantly different.[12]
As far as the relation between hypophosphatemia and respiratory failure is obvious[9] and no studies have been done to measure the admission serum Ph level as a predictor of prolonged MV, we aimed to determine the predictive ability of admission Ph level on ventilator need, duration of MV and ICU stay in critically ill patients admitted to an ICU.
Materials and Methods
We conducted a prospective, observational study approved by our Institutional Ethics Committee for human subjects research over 1-year on adult patients (>16 years old) with multiple trauma admitted to our medical and surgical ICU and who needed MV.
The consent for enrollment was obtained by proxies (close family members) in almost all cases and Patients with burn injury, history of drug addiction and CPR in emergency room before ICU admission were excluded from our data collection.
Duration of MV was defined as the number of days patients need MV and according to similar studies.[13,14,15] Patients were classified into two groups of Group A: Patients who required equal or <5 days of MV, and Group B: Patients who required more than 5 days of MV.
Those traumatic patients who failed to maintain the PaO2 above 60 mm Hg, and didn’t have those criteria which are listed below as weaning criteria, received MV to increase lung volumes and maintain acceptable oxygenation and ventilation.
Survey was conducted on admission total serum Ph level, the variety of lab tests related to Ph, type of injury, ventilator need, duration of MV, duration of ICU stay, and general patient's demographics.
Heart rate and arrhythmias at admission and during ICU stay were recorded. Tachycardia and bradycardia were defined as heart rates more than 90 and <60 beats/min.
The SOFA score was determined, and the total serum Ph concentration was measured at the time of admission to the ICU, connection to and weaning from the ventilator.
During ICU stay, a daily formal assessment of discontinuation potential was made to determine the patient's readiness to wean. If the following criteria occurred, the weaning process could be initiated.
Weaning criteria
Lung disease is stable/resolving
Low FiO2 (<0.5), PEEP (<5–8 cm H2O) requirement and pH ≥7.25
Hemodynamic stability: No active myocardial ischemia, no clinically important hypotension (vasopressors, low dose <5 g/kg/min dopamine or dobutamine are not accepted)
Able to initiate spontaneous breaths (good neuromuscular function).
Our guidelines for indicating the feasibility of discontinuing MV included:
Vital capacity of more than 15 mL/kg,
Alveolar-arterial oxygen difference of <350 cm H2O while breathing 100% oxygen,
PaO2 of more than 60 mm Hg with FiO2 of <0.5,
Negative inspiratory pressure of more than −20 cm H2O,
Normal pHa,
Respiratory rate of <20 breaths/min, and
Dead-space ventilation/tidal volume ratio of <0.6.
Breathing at rapid rates and with low tidal volumes usually signified an inability to tolerate extubation.
Ultimately, the decision to attempt withdrawal of MV was individualized and considered not only pulmonary function but also the presence of co-existing abnormalities.
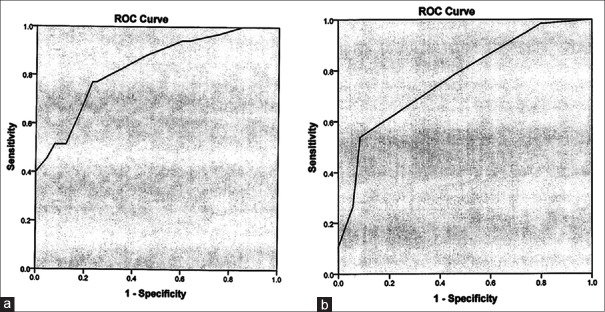
A receiver operating characteristic (ROC) curve depicts the sensitivity, specificity, positive predictive value and negative predictive value of prolonged MV for each time for both SOFA score and Ph concentration. The area under the ROC curve was evaluated. A value of 0.5 under the ROC curve indicates that the variable performs no better than chance, and a value of 1.0 indicates perfect discrimination [Figure 1]. A larger area under the ROC curve represents more reliability[16,17] and good discrimination of each time of Ph concentration and SOFA score for prolonged MV.
Figure 1.
Receiver operating characteristics curves for need to longer mechanical ventilation drawn of serum phosphorus concentration on admission (curve a). Sequential organ failure assessment score on admission (curve b)
Statistics
Data were analyzed using the statistical program SPSS 20 (Chicago, IL) for windows. All values are reported as mean ± standard error Chi-square analysis was used to determine the significance of the qualitative variables while Student's t-test was used for comparing the two groups’ quantitative variables. Statistical significance was defined as P < 0.05.
To detect a difference between two groups, at the 95% level of significance (α =0.05), with 80% power (β =0.2), 35 patients were assigned to each group.
Results
Among the critical traumatic patients requiring ventilation in ICU over a year, 100 patients were recruiting into our study. The patients were grouped according to the days of the need to MV. Thirty-six patients were in Group A (≤5 days of MV) and 64 patients were in Group B (>5 days of MV).
We studied 25 females and 75 males. The difference in gender between two groups was not significant [Table 1] (P = 0.347).
Table 1.
Demographic data, SOFA scores, serum Ph concentration and length of stay in ICU according to duration of need to MV
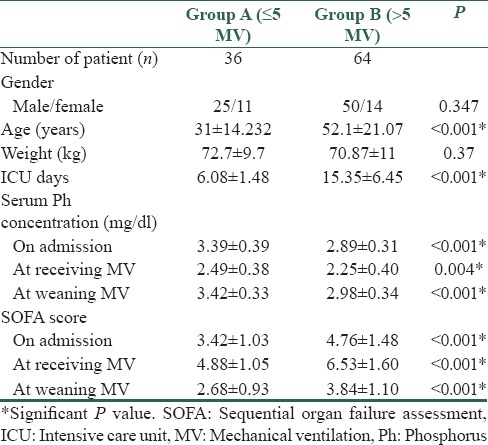
Patients’ age was ranged between 16 and 86 years old. The mean average of age in Group A was 31.2 ± 14.23 and in Group B was 52.1 ± 21.07. This difference was statically significant (P = 0.001).
There was no significant difference between weight and co-existing disease (arrhythmia, diabetes mellitus and hypertension) between two groups [Table 1] (P > 0.05).
The duration of ICU stay in Group A was 6.08 ± 1.48 days and in Group B was 15.35 ± 6.45, this difference was significant [Table 1] (P < 0.001).
There were significant difference between serum Ph concentration at the time of admission to ICU (Group A: 3.39 ± 0.39 mg/dl and Group B: 2.89 ± 0.31 mg/dl, P < 0.001), and at the time of connecting to ventilator (Group A: 2.49 ± 0.38 mg/dl and in Group B: 2.25 ± 0.26 mg/dl, P = 0.004) and weaning from ventilator (Group A: 3.42 ± 0.33 mg/dl and in Group B: 2.98 ± 0.34 mg/d) between two groups (P < 0.001).
According to our study design in separation of patients into two groups, the duration of ICU stay in Groups A and B were 6.08 ± 1.48 versus 15.35 ± 6.45 days respectively, this difference was also significant (P < 0.001) [Table 1].
In addition at the same time intervals, Group B had greater SOFA scores when compared with Group A. This difference was significant (P < 0.001) [Table 1].
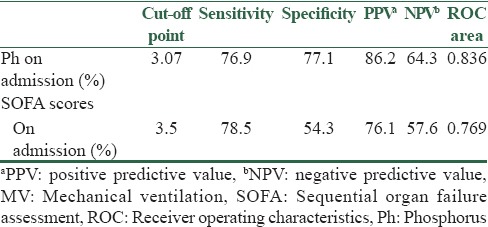
We used ROC curves of serum Ph concentration and SOFA scores to find the best cut-off point as a prediction factor for need to longer MV; the sensitivity, specificity and area of the ROC curve at the best cut-off point for longer MV are presented in Table 2.
Table 2.
Comparison of the assessment scores in need to longer MV
We also compared the groups according to the region injured:
Head (skull, face, and neck)
Torso (chest, abdomen and pelvic content)
Limbs including pelvic girdle
Head and torso
Head and limbs
Torso and limbs.
High percentage of patients in Group B had multiple organ injuries.
Discussion
The purpose of intensive care medicine is to diagnose and treat patients with life-threatening illness and to provide their health and life quality, which are important for functional results.[16]
The aim of this study was to determine the predictive ability of admission Ph level of critically ill patients, on ventilator need, duration of MV and length of stay in ICU. There are several case reports that showed a relationship between respiratory insufficiency and low serum Ph level, in the absence of underlying pulmonary disease.[18,19]
Alsumrain et al., noted that hypophosphatemia occurred in 21.2% of patients in ICU.[13]
Doig et al. showed that 50% of hypophosphatemia occurred early during ICU stay and explained that, it may be associated with re-feeding syndrome. In these patients, reducing caloric intake should be considered[12] although Grewal et al. reported that underfeeding does not appear to protect against hypophosphatemia, and other ICU interventions may predispose to hypophosphatemia.[12]
The most common clinical manifestation of hypophosphatemia is muscle (smooth, skeletal) weakness; however, rhabdomyolysis, impairing of cardiac contraction, hemolytic anemia, and respiratory failure are also other manifestation of hypophosphatemia.[15]
Respiratory failure in hypophosphatemia may be due to inadequate 2,3-diphosphoglycerate production that causes a shift in the hemoglobin dissociation curve to the left.[17] The mechanism responsible for respiratory muscle weakness in hypophosphatemia is thought to be a diminution in the supply of high-energy phosphate compounds necessary for muscle contraction. Therefore, diaphragmatic contractibility may be impaired during the hypophosphatemic state.[20]
In our study, the Ph level on admission was in normal range (3.01–3.81 in Group A and 2.58–3.1 in Group B). Patients who had the lower serum Ph concentration needed prolonger MV and stayed longer in ICU. This difference was significant.
We found the best cut-off point of 3.07 for serum Ph concentration at the time of admission to predict the need for prolonged MV in critically ill patients.
Although the value of 3.07 is in normal range but critically ill patients, usually are complicated cases with multi-organ failure, electrolyte disturbances, hypoalbuminemia. They also receive antacid and intravenous dextrose, which may result in hypophosphatemia, However, hypophosphatemia is the most neglected electrolyte deficiency in our medical practice and a number of clinical conditions, and drugs can cause hypophosphatemia. Patients who had serum Ph concentration below this value needed prolonged MV (more than 5 days).
Therefore, more précised measurement of serum Ph level may help in early diagnoses of need to prolonged MV.
In our study, we found a significant difference in age between two groups which may be due to the better amendment or correction power and more rapid recovery in younger adults than the elders.
We also found a significant relationship between SOFA scores which indicate the severity of the disease and injury on admission and the need to and duration of MV [Table 1]. Our findings were similar to the study of Honarmand et al.[21]
We found the best cut-off point of 3.5 for SOFA score at the time of admission and the scores of 5 and 3.9 at the time of receiving and weaning from MV, respectively.
Meyer reported that SOFA was not recommended for routine use in clinical decision making, whether to withhold or withdrawn intensive life support, is a difficult decision making and requires the consideration of predicted survival and projected quality of life.[18]
We also found that patients who had an injury of more than one area were talented to be receiving prolonged MV. We did not found any study assess the relation between injured organs and the need to or duration of MV specifically.
Our study presents some limitations that must be acknowledged:
First for cohesive results, we would be better monitored Ph level of patients at admission time to hospital and then hour to an hour till compensating it.
Second, as far as SOFA uses the GCS for neurological evaluation[22] and this evaluation is very difficult or almost impossible in sedated patients, it may lead to some errors in data collection.
Third, as far as our sampling was a simple nonrandomized sampling, the significant differences in sex, age and SOFA score between two groups were due to the nature and method of sampling.
Conclusion
We concluded that measurement of serum Ph in critically ill patients during ICU stay might have a predicting ability for the need to prolonged MV.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
The authors wish to sincerely thank the support of all the colleagues in intensive care unit staff of Alzahra University Hospital affiliated to Isfahan University of Medical Sciences in Isfahan, Iran. Furthermore, our special thanks to the patients, who wholeheartedly and actively assisted us to carry out this research. No conflict of interest existed. This prospective randomized observational study was approved by the Ethics Committee of our university, (Anesthesiology and Critical Care Research Center, Isfahan University of Medical Sciences, Isfahan, Iran).
References
- 1.Oud L. Transient hypoxic respiratory failure in a patient with severe hypophosphatemia. Med Sci Monit. 2009;15:CS49–53. [PubMed] [Google Scholar]
- 2.al-Ghamdi SM, Cameron EC, Sutton RA. Magnesium deficiency: Pathophysiologic and clinical overview. Am J Kidney Dis. 1994;24:737–52. doi: 10.1016/s0272-6386(12)80667-6. [DOI] [PubMed] [Google Scholar]
- 3.Boles JM, Bion J, Connors A, Herridge M, Marsh B, Melot C, et al. Weaning from mechanical ventilation. Eur Respir J. 2007;29:1033–56. doi: 10.1183/09031936.00010206. [DOI] [PubMed] [Google Scholar]
- 4.Lermitte J, Garfield M. Weaning from mechanical ventilation. Contin Educ Anaesth. 2005;5:113–117. [Google Scholar]
- 5.Boles JM, Bion J, Connors A, Herridge M, Marsh B, Melot C, et al. Weaning from mechanical ventilation. Eur Respir J. 2007;29:1033–56. doi: 10.1183/09031936.00010206. [DOI] [PubMed] [Google Scholar]
- 6.Tobin MJ. Mechanical ventilation. N Engl J Med. 1994;330:1056–61. doi: 10.1056/NEJM199404143301507. [DOI] [PubMed] [Google Scholar]
- 7.Smith RA. Principles of Mechanical Ventilation. Text Book of Critical Care. Philadelphia (PA): W.B Sanders; 1995. pp. 858–67. [Google Scholar]
- 8.Safavi M, Honarmand A. Admission hypomagnesemia impact on mortality or morbidity in critically ill patients. Middle East J Anaesthesiol. 2007;19:645–60. [PubMed] [Google Scholar]
- 9.Arend W, Drazan J, Larusso N, Armitage J, Clemmons D. Renal Diseases, Goldman's Cecils Medicine. Philadelphia: Elsevier Publication; 2008. pp. 839–40. [Google Scholar]
- 10.Amanzadeh J, Reilly RF., Jr Hypophosphatemia: An evidence-based approach to its clinical consequences and management. Nat Clin Pract Nephrol. 2006;2:136–48. doi: 10.1038/ncpneph0124. [DOI] [PubMed] [Google Scholar]
- 11.Brunelli SM, Goldfarb S. Hypophosphatemia: Clinical consequences and management. J Am Soc Nephrol. 2007;18:1999–2003. doi: 10.1681/ASN.2007020143. [DOI] [PubMed] [Google Scholar]
- 12.Doig GS, Bellomo R, Simson F, Hegarty C, Egi M, Sweetman EA, et al. Hypophosphatemia occurs early in ICU stay and associated with increased duration of mechanical ventilation and ICU and hospital stay. Am J Respir Crit Care Med: 2009;179:23–9. [Google Scholar]
- 13.Alsumrain MH, Jawad SA, Imran NB, Riar S, DeBari VA, Adelman M. Association of hypophosphatemia with failure-to-wean from mechanical ventilation. Ann Clin Lab Sci. 2010;40:144–8. [PubMed] [Google Scholar]
- 14.Grewal Y, Ong PH, Badara M, Chanda A, Balasingham SH, Diovertiprono MV, et al. Incidence and consequences of hypophosphatemia in critically ill patients. Am J Respir Crit Care Med. 2011;183 A5824. [Google Scholar]
- 15.Jaber S, Petrof BJ, Jung B, Chanques G, Berthet JP, Rabuel C, et al. Rapidly progressive diaphragmatic weakness and injury during mechanical ventilation in humans. Am J Respir Crit Care Med. 2011;183:364–71. doi: 10.1164/rccm.201004-0670OC. [DOI] [PubMed] [Google Scholar]
- 16.McNeil BJ, Hanley JA. Statistical approaches to the analysis of receiver operating characteristic (ROC) curves. Med Decis Making. 1984;4:137–50. doi: 10.1177/0272989X8400400203. [DOI] [PubMed] [Google Scholar]
- 17.Moor DJ, Rosh AJ. Hypophosphatemia. Emedicine. [Last updated on 2009 Sep 22]. Available from: http://www.emedicine.medscape.com/article/767955-overview .
- 18.Meyer AA, Messick WJ, Young P, Baker CC, Fakhry S, Muakkassa F, et al. Prospective comparison of clinical judgment and APACHE II score in predicting the outcome in critically ill surgical patients. J Trauma. 1992;32:747–53. doi: 10.1097/00005373-199206000-00013. [DOI] [PubMed] [Google Scholar]
- 19.Patel U, Sriram K. Acute respiratory failure due to refeeding syndrome and hypophosphatemia induced by hypocaloric enteral nutrition. Nutrition. 2009;25:364–7. doi: 10.1016/j.nut.2008.09.011. [DOI] [PubMed] [Google Scholar]
- 20.Dooley J, Fegley A. Laboratory monitoring of mechanical ventilation. Crit Care Clin. 2007;23:135–48. doi: 10.1016/j.ccc.2006.11.013. vii. [DOI] [PubMed] [Google Scholar]
- 21.Honarmand A, Safavi M, Moradi D. The use of infection probability score and sequential organ failure assessment scoring systems in predicting mechanical ventilation requirement and duration. Ulus Travma Acil Cerrahi Derg. 2009;15:440–7. [PubMed] [Google Scholar]
- 22.Bernard GR, Vincent JL, Laterre PF, LaRosa SP, Dhainaut JF, Lopez-Rodriguez A, et al. Quantification of organ dysfunction: Seeking standardization. Crit Care Med. 1998;26:1767–8. doi: 10.1097/00003246-199811000-00001. [DOI] [PubMed] [Google Scholar]