Abstract
Objectives:
The aim of this pilot study was to evaluate the efficacy, safety and participants’ perception of a novel technique in airway clearance therapy – specific cough technique in cystic fibrosis.
Methods:
We conducted randomised controlled individual trials (N-of-1 randomised controlled trials) in six adults. Each trial included 8 weeks of treatment with two interventions each week, one with specific cough technique and one with forced expiration technique. The efficacy was investigated by a blinded assessor measuring wet weight of sputum (g) after each session. Perceived usefulness and preference was self-reported at the end of study. Additional measurements included oxygen saturation and heart rate before and after each session and lung function (week 2).
Results:
Three of six participants produced significantly higher mean sputum weight when using specific cough technique, differences being 21%, 38% and 23%, respectively. In three of the six participants, mean sputum weight was lower after forced expiration technique than after specific cough technique in each of the eight treatment pairs. Participant-reported outcomes were completed in all participants. Specific cough technique was reported to be easier to use in daily treatments and more normalising in everyday life.
Conclusion:
Specific cough technique was well tolerated and accepted by the participants with cystic fibrosis. Specific cough technique was non-inferior to forced expiration technique in terms of sputum production, thus specific cough technique appears to represent a promising alternative for clearing sputum in airway clearance therapy.
Keywords: Airway clearance physiotherapy, forced expiration technique, N-of-1 randomised controlled trials, participants’ perception, specific cough technique, sputum production
Introduction
Lung disease in cystic fibrosis (CF) is characterised by increased mucus production and reduced mucus clearance, thus leading to a process of infection, structural changes and physiological disturbances.1,2 Effective mucus clearance is essential, in order to reduce symptoms and optimise treatment.2
Cough and forced expirations are suggested to be the most effective manoeuvres for improving mucus transport and sputum removal from central airways.3 While cough represents a basic cleaning mechanism and serves as back-up mechanism and adjunct to mucociliary clearance,4 Forced Expiration Technique (FET) is used as part of active cycle of breathing techniques5 and other airway clearance techniques (ACTs) such as positive expiratory pressure (PEP) therapy.6
The Specific Cough Technique (SCT) was developed in the late 1990s in Norway,7 aiming to make removal of bronchial secretions more efficient in individuals with CF, who tended to have less beneficial effect with other techniques. SCT comprises one gentle cough at lower lung volume to localise and collect mobilised mucus, followed by two to three coughs from higher lung volume to expectorate.
Previous evaluation and experience in clinical practice have shown that SCT easily can be learned, self-administered and used in airway clearance physiotherapy to enhance mucus clearance and effective expectoration.7
SCT may be used as part of an airway clearance strategy to mobilise and clear bronchial secretions, that is, in conjunction with saline inhalation or physical activity/exercise used as part of treatment, or with other ACTs, for example, PEP or oscillating positive expiratory pressure (OPEP).
To date, there is insufficient evidence to suggest that one ACT or approach is superior6 or non-inferior to others,8 and evaluation of the comparative effectiveness of ACTs remains to be a challenge due to differences in disease severity, pathophysiology and characteristics of subgroups.2,3,9
The aim of this pilot study was to search for possible effects of SCT compared to FET in individual participants who may be worth following up in a subsequent larger study. A secondary aim was to evaluate the feasibility of SCT in terms of participants’ perception and preference.
Methods
Study design
The pilot study was a series of N-of-1 randomised controlled trials (RCTs) undertaken at Oslo University Hospital in 2010 and 2011. The trial design uses a series of planned and repeated pairs of treatment periods, where random allocation determines the order of the treatments within each pair.10 Randomisation was performed prior to the study by an independent assessor and concealed. Coin-toss was used to determine the order of the treatments within each pair.
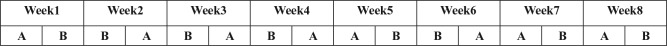
Unlike randomised controlled group trials which establish treatment efficacy by providing information about the average effect in a target population, randomised, controlled trials in single subjects provide information about the best treatment in an individual, which may be hidden by the group average.11 We used a randomised, controlled multiple crossover sequence in eight treatment periods, with two treatments in each pair, one with FET and one with SCT. Each participant underwent eight treatment periods (Figure 1) serving as their own control. The treatment pairs were performed approximately at the same time of the day on two consecutive days, separated by 24 h. The main criteria for success of the pilot study were the assessment of significant differences in sputum weight in individual participants and the complete (>90%) follow-up of participant-reported outcomes.
Figure 1.
Schematic presentation of the treatment schedule for one of the participants: 16 treatments during eight treatment periods and two interventions each week: one with SCT and one with FET and randomised sequence of the interventions.
A: forced expiration technique; B: specific cough technique.
Study subjects
Participants were recruited through the regional CF centre and consecutively included. The CF diagnosis of the participants was based upon clinical symptoms, sweat chloride levels >59 mmol/L and two CF mutations.
Inclusion criteria were as follows: CF diagnosis, age ⩾18 years, sputum production more than 5 mL in a treatment session, either isotonic or hypertonic saline inhalation as part of treatment or dornase alpha. Exclusion criteria were as follows: respiratory failure, active haemoptysis, pregnancy and acquisition with multiresistant Pseudomonas aeruginosa, Burkholderia cepacia, atypical mycobacteria or methicillin-resistant Staphylococcus aureus.
Seven participants were included in the study. In the same time period, 82 CF patients were followed at the regional CF centre, but the whole cohort was not screened for eligibility in this pilot study.
One participant withdrew halfway due to unrelated personal reasons (Figure 2). All participants were clinically stable at the time of entry, that is, required no treatment for a pulmonary exacerbation within 2 weeks. It was decided a priori to start the treatment pair over again if a participant experienced an exacerbation during one of the treatment periods and to postpone the treatment pair for 2 weeks if a participant received intravenous (i.v.) antibiotics. The Regional Ethics Committee in Oslo approved this study (2010/802). All participants provided written informed consent.
Figure 2.

Participant flow.
Intervention
The majority of the participants were familiar with FET and/or SCT prior to the study. The skill level of both techniques was secured in the beginning of the study, and each participant was trained according to recommended applications.5,7
We used a standardised protocol and the intervention was supervised by the same experienced respiratory physiotherapist. SCT and FET were evaluated using either isotonic saline or hypertonic saline during treatment12 in horizontal positions to enhance ventilation and mucociliary clearance,13 hydrate and promote mucus clearance and cough clearance.2 Each participant inhaled the same medication in each intervention.
Interventions comprised a session of approximately 60 min, with saline inhalation during treatment in side-lying horizontal positions, alternating with SCT or FET. The body side on which side-lying was first completed was selected based on previous order in individual routine treatments or participants’ preference.
The number of manoeuvres, body side, saline doses and treatment duration was defined a priori and standardised for each participant. Body side was typically changed at the halfway point of the treatment session and the procedure repeated until the predetermined time was over.
Inhalation therapy consisted of nebulised bronchodilator followed by either hypertonic saline (6%–7%) or isotonic saline. Participants were instructed to breathe calmly and slowly through the mouthpiece. Each participant completed three sets of the following breathing cycle during nebulisation: four breaths of increased tidal volume (3–4 s) and a deeper breath (5–6 s), and then, they performed either FET or SCT to aid expectoration.
The participants were using the nebuliser with the described breathing pattern as part of the treatment to mobilise and transport mucus by increasing the tidal volume, ventilation and addressing deposition of inhaled saline, alternating with either FET or SCT.
FET consisted of typically three forced expirations (mid-low lung-volume huff), combined with breathing control, followed by a huff or cough from high lung volume to clear secretions, followed by breathing control.5
SCT consisted of one single and low-sounded cough at lower lung volume following a prolonged expiration, to localise and collect mobilised mucus, followed by 2–3 coughs with modest cough-effort from higher lung volume, that is, two coughs after the first breath, followed by a modest inspiration and one single cough to expectorate, and then followed by tidal breathing.7
SCT allows adaptation and control of the expiratory starting volume, the subsequent inspiratory volume and cough-effort, thus the pressures and flows being developed. In each participant, SCT was customised in accordance with the degree of bronchial obstruction and individual breathing pattern.
The sequence of manoeuvres in each technique was repeated three times, that is, each participant expectorated three times using either FET or SCT before the saline inhalation continued. Total volume of sputum expectorated in either technique was collected in coded and pre-weighed gradated tubes (50 mL; Greiner Bio-One, Frickenhausen, Germany).
Data collection
Demographics and participant characteristics were recorded at baseline, including aerosol medication, main culture of bacteria and lung function.
Intervention pilot: efficacy
Sputum wet weight (g) was chosen as outcome measure in this pilot study since it has been suggested as appropriate in short-term studies6 and considered as a good predictor of dry weight.13 It appeared to be an easy method, often used in clinical practice to measure effectiveness.14 According to the present design, the outcome measure must be relevant both clinically and to the participants’ well-being.15 Thus, sputum wet weight was considered to be a relevant outcome measure when assessing individual efficacy.
Sputum was collected throughout each treatment and weighed wet by a blinded investigator unaware of the techniques being performed, using a Mettler-Toledo Weighing Balance (EL 202; accuracy: 0.01 g). The balance was calibrated before each measurement and sputum weight was derived from the total weight minus the pre-use tube weight.
Feasibility objectives, participants’ perception and safety
Feasibility objectives quantified prior to study initiation included eligibility, trial enrolment, follow-up and data management including self-reporting on participants’ perception. Specific outcomes included perception of usefulness.
After completion of each treatment in week 8, participants self-reported on perceived usefulness with either technique using a 5-point Likert response scale16 with seven assertions: ease of understanding instruction, ease of performance, effectiveness at clearing sputum, ease to use in daily treatment, normalising in everyday life, in terms of clearing secretions in daily treatments with a minimum of disturbance to lifestyle, degree of tiredness and breathlessness (1 = strongly agree and 5 = strongly disagree). In addition to this, after the last intervention, participants self-reported on preferred technique: 1 = I prefer FET, 2 = I prefer SCT and 3 = I have no preference. Oxygen saturation (SpO2) and heart rate (HR) were assessed to identify any differences between the techniques and as a safety issue using a Nonin 2500 Pulse Oximeter (Nonin Medical Inc, Plymouth, MN, USA).
Lung function
Lung function was measured by forced expiratory flow volumes according to the European Respiratory Society (ERS)/American Thoracic Society (ATS) guidelines using a SensorMedics Vmax 20c (SensorMedics Diagnostics, Yorba Linda, CA, USA) and performed by blinded assessor using reference values from Knudson et al.17
Power calculation: calculation of the number of treatment periods
The number of treatment periods was determined before the study based on the following calculations.10 Given that the compared treatments are equally effective in terms of sputum production, X denotes the number of weeks where SCT is more effective than FET. Given equal efficacy, X will be binomially distributed with a weekly success probability equal to 0.5, and p value can be calculated for outcomes of X. High values of X indicate that SCT is more effective that FET. Low values of X indicate that FET is more effective than SCT. With a significant level of 5% and eight treatment periods, the result ‘X = 8’ for a given participant will provide a p value of 0.008. If we use six treatment periods, the highest possible value of X is 6.
It may be shown that if the treatments are equally effective, the p value associated with the result ‘X = 6’ is 0.063. Thus, it is not possible to obtain a significant result with six treatment periods. Thus, we decided to use eight treatment periods for each participant.
We chose to include six participants in the study because we had the opportunity to conduct 16 × 6 = 96 interventions in eight treatment pairs. We considered that six participants can give us some information about this difference.
Data analysis
A one-sample binomial test was used when comparing individual sputum weight in the experiments with FET and SCT. Sputum weight was analysed by counting the number of weeks where SCT or FET produced higher weight. The level of significance was set at 5%. Data were investigated for the possibility of a carry-over effect between the techniques by calculating individual mean sputum production for each technique.
Treatment differences between FET and SCT were further assessed on group basis and compared by descriptive methods. These data include sputum weight, lung function, SpO2 and HR. Group differences between the techniques were not tested for significance due to limited number of participants. Data collected from all periods were included in the analysis. Statistical analyses were performed using SPSS 18 (SPSS Inc., Chicago, IL, USA).
Results
Demographics and baseline characteristics of the participants are listed in Table 1. The lung function parameters reflected mild-to-moderate (n = 4) and more severe (n = 2) degree of airway obstruction, range = 29%–95%. The treatment pairs were distributed over 2 months (n = 2), 3–4 months (n = 3) and 6 months (n = 1).
Table 1.
Baseline characteristics of the study participants (n = 6).
| Male/female | 4/2 |
| Age (year), median (min–max) | 35.5 (23–57) |
| BMI (kg/m2), median (min–max) | 23.0 (21–24) |
| FEV1 (% predicted), median (min–max) | 74.0 (29–95) |
| FEF50% (% predicted), median (min–max) | 49.0 (9–98) |
| FEF25%–75% (% predicted), median (min–max) | 40.5 (10–86) |
| Pseudomonas aeruginosa | 3 |
| Staphylococcus aureus | 3 |
| Bronchodilator (n) | 6 |
| Isotonic saline (n) | 2 |
| Hypertonic saline (n) | 4 |
| DNase (Pulmozyme) (n) | 4 |
| Chronic inhaled antibiotic therapy (n) | 2 |
BMI: body mass index; FEV1: forced expiratory volume in 1 s; FVC: forced vital capacity; FEF50%: forced expiratory flow at 50% of FVC; FEF25%–75%: forced expiratory flow between 25% and 75% of FVC.
Sputum production and safety
Individual sputum data are presented in Table 2. In three participants, sputum production was statistically significant in favour of SCT. Although not statistically significant, we found that SCT was the most effective technique in participant 6 in 7 of 8 weeks and in participant 5 in 6 of 8 weeks, in contrast to participant 2 where sputum production was in favour of FET in 7 of 8 weeks (Table 3).
Table 2.
Mean (range) sputum weights (g) and differences (g) for the two treatments (n = 6).
| Treatment weeks 1–8 | FET | SCT | Differencesa |
|---|---|---|---|
| Participant 1 | 42.7 (25.0–61.5) | 51.8 (30.6–73.9) | 9.0 (21%) |
| Participant 2 | 32.6 (25.8–37.6) | 28.4 (22.0–35.3) | −4.2 (13%) |
| Participant 3 | 19.1 (13.2–28.8) | 26.5 (18.9–30.1) | 7.3 (38%) |
| Participant 4 | 22.5 (18.1–25.1) | 27.7 (22.7–31.5) | 5.1 (23%) |
| Participant 5 | 15.3 (11.7–19.8) | 18.2 (14.9–21.7) | 2.9 (19%) |
| Participant 6 | 29.0 (21.7–37.5) | 33.6 (28.5–42.0) | 4.5 (16%) |
FET: forced expiration technique; SCT: specific cough technique.
Differences presented as mean (g) and percentage (%).
Table 3.
Within individual comparison of the interventions (n = 6).
| Treatment weeks 1–8 | Number of weeks where FET was the most effective | Number of weeks where SCT was the most effective | p value |
|---|---|---|---|
| Participant 1 | 8 | 0.008 | |
| Participant 2 | 7 | 1 | 0.062 |
| Participant 3 | 8 | 0.008 | |
| Participant 4 | 8 | 0.008 | |
| Participant 5 | 2 | 6 | 0.296 |
| Participant 6 | 1 | 7 | 0.062 |
FET: forced expiration technique; SCT: specific cough technique.
Group data for the measurements of sputum weight on mean change for each technique are presented in Table 4. By assessing whether the differences in sputum weight between the techniques were affected by the order in which the treatments were given, no carry-over effects were detected that can explain the differences in sputum production (data not shown).
Table 4.
Group comparison of forced expiration technique and specific cough technique on selected variables (n = 6).
| Results expressed as mean change (SD) from before and after each treatment | Forced expiration technique | Specific cough technique |
|---|---|---|
| Total sputum wet weight (g) | 26.9 (10.0) | 31.0 (11.3) |
| FEV1, % of predicteda | 2.16 (1.83) | 4.83 (3.71) |
| FVC, % of predicteda | 2.16 (2.04) | 2.33 (3.01) |
| FEF50%, % of predicteda | 5.50 (8.11) | 11.16 (10.14) |
| FEF25%–75%, % of predicteda | 1.50 (4.23) | 8.00 (7.07) |
| SpO2 (%) | −0.63 (0.87) | −0.51 (0.34) |
| HR | 4.95 (9.30) | 4.95 (9.13) |
FEV1: forced expiratory volume in 1 s; FVC: forced vital capacity; FEF50%: forced expiratory flow at 50% of FVC; FEF25%–75%: forced expiratory flow between 25% and 75% of FVC; SpO2: oxygen saturation; HR: heart rate; SD: standard deviation.
Measured as mean change before and after each treatment in pair 2.
Both treatments were well tolerated and no adverse events or unintended effects were identified, with similar SpO2 and HR levels before and after each treatment (Table 4). There was a trend (not significant) towards higher lung function values on mean change in favour of SCT (Table 4).
Feasibility, perceived usefulness and preference
An overview of the enrolment, participant flow and completion of the trial is given in Figure 2. Three participants preferred SCT, one FET and two had no preference. Perceived usefulness was similar for the two techniques (Table 5). Participants reported both techniques as effective at clearing sputum and easy to understand and perform. SCT was associated with greater ease of use in daily treatments and more normalising in everyday life (Table 5).
Table 5.
Group comparison of perceived usefulness of forced expiration technique and specific cough technique (n = 6).
| Number of participants either agreeing or strongly agreeing with the assertion for each technique | Forced expiration technique | Specific cough technique |
|---|---|---|
| Easy to understand instruction | 6 | 6 |
| Easy to perform | 5 | 6 |
| Effective at clearing sputum | 5 | 6 |
| Easy to use in daily treatment | 3 | 5 |
| Normalising in everyday life | 2 | 4 |
| Tiring to use | 3 | 2 |
| Get tired/breathless from using it | 1 | 2 |
Discussion
The SCT was found to be effective, safe and preferred in three out of six participants. Furthermore, the amount of sputum produced when using SCT was non-inferior to FET irrespectively of the order of treatments.
The evaluation of SCT and FET in conjunction with saline inhalation during treatment was not associated with adverse effects as assessed by short-term changes in oxygen saturation, HR and spirometry values. Comparable results between SCT and FET on perceived usefulness were found on several parameters.
Sputum production
The results of the presented study demonstrate that SCT is safe and non-inferior to FET, which may facilitate SCT as an alternative technique used in airway clearance physiotherapy, being of clinical value in individuals with CF.
An ultimate goal in airway clearance physiotherapy is to enhance mucus clearance and expectoration of bronchial secretions and to increase expiratory airflow velocity by cough and forced expirations by generating two-phase gas–liquid flow and shear forces which help dislodging mucus.18,19 To achieve effective expectoration, the intrathoracic pressure must be balanced to avoid dynamic airway closure20 and complications associated with vigorous coughing.19
FET was introduced to enhance clearance of secretions with less transpulmonary pressure.5,19 Thus far, FET has been compared with directed cough in short-term studies, reporting inconsistent findings.21,22 Sutton et al.21 found FET to be more effective than directed coughing alone in terms of sputum mobilisation and radioaerosol clearance in patients with copious sputum. In a study by Hasani et al.,22 FET and instructed cough were found to be equally effective in clearing secretions in patients with airway obstruction.
SCT was developed to facilitate sputum clearance by using planned and controlled cough at specific lung volumes.7 The technique is characterised by two phases as previously defined by Gursli:7 a relaxed and prolonged expiration and then one gentle and low-sounded cough at lower lung volume (initial phase), followed by inspiration, and two to three coughs from higher lung volume to expectorate (removal phase). The initial cough aims to assess whether there is mobilised mucus present and to localise mobilised mucus before expectoration. The following inspiration typically comprises a mid-sized breath relative to the subsequent modest cough-effort, as only modest increase in intrathoracic pressure is needed to generate the necessary dynamic compression to increase airflow velocity by cough.18 Mucus is cleared from central airways utilising the cleaning mechanisms of two-phase gas–liquid flow, local dynamic airway compression and increased expiratory airflow velocities, thus enhancing sputum removal.3,4,18
While SCT aims at localising mobilised mucus before expectoration, utilising the cleaning mechanism of cough by balancing lung volumes, cough-effort, pressure and flow,7 FET aims to enhance mucus transport by increasing expiratory flow in more peripheral airways before a huff or cough from high lung volume.5,9 We acknowledge that SCT may be easier to perform, which may have had an impact on the results.
It has been suggested that certain types of mucus may influence effectiveness of some ACTs23 and that sputum characteristics may play a role as to which technique is more effective.2,24 In our study, one participant removed more sputum with FET, thus indicating that FET was more effective in this participant. Given that less viscous sputum may be easily cleared by cough clearance and mucus with higher viscoelasticity by transport, sputum characteristics may explain why the sputum weight was higher when using SCT compared to FET in three participants.18
Our study found a trend towards higher lung function values on mean change from before and after each treatment (pair 2) in favour of SCT. Although not significant, this finding may possibly reflect that enhanced sputum production reduces airway obstruction. However, lung function measurements are relatively insensitive to reflect immediate changes in mucus removal,3 and group data in this study should be interpreted carefully. Furthermore, the measurements were only taken before and after the second treatment pair. Hence, there are limited numbers behind this lung function data. Nevertheless, this is an interesting finding, which should be studied further.
Feasibility and safety
Perceived usefulness was comparable between SCT and FET on several parameters. However, most participants reported SCT to be more useful in terms of ease of use in daily treatments and more normalising in everyday life.
It has been suggested that more efficient expectoration may be an important effect of treatment.3 Furthermore, that perceived lack of efficacy may influence adherence.25 Acute efficacy measured by sputum weight in our study was comparable with participants’ perception of effectiveness. Furthermore, preference for technique was associated with efficacy in four of six patients.
Subjective perception is considered valuable as it may influence adherence with treatment.8,14,25 Preference may further influence adherence with technique, and in our study, individual preference for technique was found in four participants. Two participants reported no preference, possibly reflecting the opportunity to choose technique according to individual need and treatment modality.
SCT was displayed as a safe alternative to FET in terms of sputum clearance and short-term changes in SpO2, HR and spirometry values, as no adverse events or unintended effects were identified during this study.
Strengths and limitations
A major strength of this study is the randomised, controlled multi-crossover design with individual measurements on sputum production and lung function, including assessment of participants’ perceptions and preference. A methodological strength is that no carry-over effects were detected that can explain the differences in sputum production.
Individual responses in single trials are demanding to generalise to the wider population. However, it has been suggested that results might be generalised by combining trials with the use of strict entry-criteria, similar procedures and outcome measures, and acceptable statistical tests.10
Our study demonstrates that individual RCTs can be useful in evaluating the feasibility of a novel technique. The study design seems useful in determining whether the treatment is beneficial in a particular participant and to identify responders to treatment.26 Additional benefits may be enhanced self-management, which in turn may influence adherence to maintenance treatment. The adherence to the trial design was excellent; demonstrating that the novel SCT was well tolerated and accepted as each participant underwent eight treatments with no drop outs.
This pilot study followed guidelines for N-of-1 RCTs as presented by Guyatt et al.10 However, there might be some potential limitations which could have influenced the results.10
The major limitation is the small sample size, thus making it difficult to generalise. However, we were able to find significant differences between SCT and FET in individual participants, thus indicating that the design may be valid in future larger studies.
One other limitation is the lack of blinding of the physiotherapist and participant through the intervention, thus prior beliefs, preferences and expectations may bias the results.10
Another possible limitation is related to disease stability. Previous studies have validated sputum production as a reproducible outcome measure in CF and reported sputum production to be similar within a week interval27 and on a day-to-day basis during disease stability.28 In this study, sputum production was relatively similar in each pair when the techniques were compared.
A further possible limitation relates to the use of sputum wet weight (g) as outcome due to potential overestimation and underestimation.29 Although dry weight of sputum has been considered as more accurate in reflecting sputum quantity, contradictory findings exist in the literature regarding the correlation between wet and dry weight. While some studies found no difference in the ratio of dry to wet sputum weight,21 and no significant difference in wet or dry sputum weight between treatment groups and placebo,28 other studies have found a significant difference between treatments when considering both wet and dry weight.30 Although a standardised protocol was used in this study, the lack of sufficient recoding of total coughs in the interventions, as spontaneous coughs can influence sputum production, may have affected sputum weight.
One limitation may be related to treatments being conducted by the developer of the SCT. In studies on airway clearance, supervision by an experienced physiotherapist is important. However, it may also leave the study open to bias in favour of a technique. However, in our study, treatments were based on a standardised protocol with objective outcome measures and blinding of outcome assessments, which may have helped to reduce potential variability due to the conductor.
Implications for future research
This pilot study demonstrates that the N-of-1 trial design can be useful in determining an individual treatment efficacy outcome and to identify responders to treatment. It was also managed to complete patient reported outcomes for all participants, thus the criteria for success in this pilot study were achieved.
A clinical implication of this study is that SCT compared to FET may clear sputum in a more efficient way and with less effort in individuals with CF. Further studies are required to investigate the clinical efficacy of SCT in airway clearance therapy on sputum production and clinical meaningful endpoints. Additional studies involving multiple centres to increase the number of participants are required to evaluate the effects of SCT in terms of airway clearance. Long-term studies are needed to assess potential long-term benefits and effects of the SCT on clinical endpoints, such as exacerbations and health-related quality of life, including possible key factors associated with adherence.
Conclusion
SCT was well tolerated and accepted by the participants with CF in our study. All participants completed the pilot study and no adverse effects were observed. SCT was non-inferior to FET in terms of sputum production. Thus, SCT appears to represent a promising alternative for clearing sputum in physiotherapy for airway clearance.
Acknowledgments
We thank T. Klætte, Physiotherapist, Oslo University Hospital, for providing assistance with the measurements.
The study was registered in ClinicalTrials.gov under the number NCT0 1266473.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Ethical approval: Ethical approval for this study was obtained from The Regional Ethics Committee in Oslo (#2010/802).
Funding: The author(s) received no financial support for the research, authorship and/or publication of this article.
Informed consent: Written informed consent was obtained from all subjects before the study.
References
- 1. O’Sullivan BP, Freedman SD. Cystic fibrosis. Lancet 2009; 373(9678): 1891–1904. [DOI] [PubMed] [Google Scholar]
- 2. Fahy JV, Dickey BF. Airway mucus function and dysfunction. N Engl J Med 2010; 363(23): 2233–2247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Van der Schans CP, Postma DS, Koeter GH, et al. Physiotherapy and bronchial mucus transport. Eur Respir J 1999; 13(6): 1477–1486. [DOI] [PubMed] [Google Scholar]
- 4. Foster WM. Mucus hypersecretion and mucus clearance in cough. In: Chung KF, Widdicombe JG, Boushey HA. (eds) Cough: causes, mechanisms and therapy. Malden, MA: Blackwell Publishing Ltd, 2003, pp.207–216. [Google Scholar]
- 5. Pryor JA, Prasad SA. Physiotherapy techniques. In: Pryor JA, Prasad SA. (eds) Physiotherapy for respiratory and cardiac problems. 4th ed. Edinburgh: Churchill Livingstone, 2008, pp.134–217. [Google Scholar]
- 6. Bradley JM, Moran FM, Elborn JS. Evidence for physical therapies (airway clearance and physical training) in cystic fibrosis: an overview of five Cochrane systematic reviews. Respir Med 2006; 100: 191–201. [DOI] [PubMed] [Google Scholar]
- 7. Gursli S. Respiratory physiotherapy: a dynamic process. 1st ed. Oslo: Unipub Forlag, 2005, pp.67–69. [Google Scholar]
- 8. Pryor JA, Tannenbaum E, Scott SF, et al. Beyond postural drainage and percussion: airway clearance in people with cystic fibrosis. J Cyst Fibros 2010; 9(3): 187–192. [DOI] [PubMed] [Google Scholar]
- 9. Alison JA. Clinical trials of airway clearance techniques. Chron Respir Dis 2004; 1(3): 123–124. [DOI] [PubMed] [Google Scholar]
- 10. Guyatt G, Jaeschke R, McGinn T. Therapy and validity: n of 1 randomized controlled trials. In: Guyatt G, Rennie D, Meade M, et al. (eds) Users’ guides to the medical literature: a manual for evidence-based clinical practice. Chicago, IL: American Medical Association, 2002, pp. 276–290. [Google Scholar]
- 11. Graham JE, Karmarkar AM, Ottenbacher KJ. Small sample research designs for evidence-based rehabilitation: issues and methods. Arch Phys Med Rehabil 2012; 93(8 Suppl.): S111–S116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Dentice RL, Elkins MR, Bye PT. Adults with cystic fibrosis prefer hypertonic saline before or during airway clearance techniques: a randomised crossover trial. J Physiother 2012; 58(1): 33–40. [DOI] [PubMed] [Google Scholar]
- 13. Cecins NM, Jenkins SC, Pengelley J, et al. The active cycle of breathing techniques – to tip or not to tip? Respir Med 1999; 93(9): 660–665. [DOI] [PubMed] [Google Scholar]
- 14. Flume PA, Robinson KA, O’Sullivan BP, et al. Cystic fibrosis pulmonary guidelines: airway clearance therapies. Respir Care 2009; 54(4): 522–537. [PubMed] [Google Scholar]
- 15. Guyatt G, Sackett D, Taylor DW, et al. Determining optimal therapy–randomized trials in individual patients. N Engl J Med 1986; 314(14): 889–892. [DOI] [PubMed] [Google Scholar]
- 16. Wolfle D, Likert R. Standards for appraising psychological research. Am Psychol 1949; 4(8): 320–328. [DOI] [PubMed] [Google Scholar]
- 17. Knudson RJ, Lebowitz MD, Holberg CJ, et al. Changes in the normal maximal expiratory flow-volume curve with growth and aging. Am Rev Respir Dis 1983; 127(6): 725–734. [DOI] [PubMed] [Google Scholar]
- 18. McCool FD. Global physiology and pathophysiology of cough: ACCP evidence-based clinical practice guidelines. Chest 2006; 129(1 Suppl): 48S–53S. [DOI] [PubMed] [Google Scholar]
- 19. Irwin RS, Boulet LP, Cloutier MM, et al. Managing cough as a defense mechanism and as a symptom. A consensus panel report of the American College of Chest Physicians. Chest 1998; 114(2 Suppl. Managing): 133S–181S. [DOI] [PubMed] [Google Scholar]
- 20. Zach MS. The physiology of forced expiration. Paediatr Respir Rev 2000; 1(1): 36–39. [DOI] [PubMed] [Google Scholar]
- 21. Sutton PP, Parker RA, Webber BA, et al. Assessment of the forced expiration technique, postural drainage and directed coughing in chest physiotherapy. Eur J Respir Dis 1983; 64(1): 62–68. [PubMed] [Google Scholar]
- 22. Hasani A, Pavia D, Agnew JE, et al. Regional lung clearance during cough and forced expiration technique (FET): effects of flow and viscoelasticity. Thorax 1994; 49(6): 557–561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Fink JB. Forced expiratory technique, directed cough, and autogenic drainage. Respir Care 2007; 52(9): 1210–1221. [PubMed] [Google Scholar]
- 24. Houtmeyers E, Gosselink R, Gayan-Ramirez G, et al. Regulation of mucociliary clearance in health and disease. Eur Respir J 1999; 13(5): 1177–1188. [DOI] [PubMed] [Google Scholar]
- 25. Kettler LJ, Sawyer SM, Winefield HR, et al. Determinants of adherence in adults with cystic fibrosis. Thorax 2002; (57): 459–464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Johannessen T. Controlled trials in single subjects. BMJ 1991; 303(6795): 173–174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Cantin AM, Bacon M, Berthiaume Y. Mechanical airway clearance using the frequencer electro-acoustical transducer in cystic fibrosis. Clin Invest Med 2006; 29(3): 159–165. [PubMed] [Google Scholar]
- 28. Jarad NA, Powell T, Smith E. Evaluation of a novel sputum clearance technique – hydro-acoustic therapy (HAT) in adult patients with cystic fibrosis: a feasibility study. Chron Respir Dis 2010; 7(4): 217–227. [DOI] [PubMed] [Google Scholar]
- 29. Rossman CM, Waldes R, Sampson D, et al. Effect of chest physiotherapy on the removal of mucus in patients with cystic fibrosis. Am Rev Respir Dis 1982; 131–135. [DOI] [PubMed] [Google Scholar]
- 30. Kluft J, Beker L, Castagnino M, et al. A comparison of bronchial drainage treatments in cystic fibrosis. Pediatr Pulmonol 1996; 22(4): 271–274. [DOI] [PubMed] [Google Scholar]