Abstract
Under Share-35, deceased-donor (DD) livers are offered regionally to candidates with MELD≥35 before locally to candidates with MELD<35. Using SRTR data from 6/2013–6/2015, we identified 1768 DD livers exported to regional MELD 35+ candidates who were transplanted at a median (IQR) MELD of 39 (37–40) with 30-day post-transplant survival of 96%. 1764 (99.8%) exports had an ABO-compatible candidate in the recovering OPO, representing 1219 unique reprioritized candidates who would have had priority over the regional candidate under pre Share-35 allocation. Reprioritized candidates had a median (IQR) waitlist MELD of 31 (27–34) when the liver was exported. 291 (24%) of reprioritized candidates had a comparable MELD (within 3-points of the regional recipient); 209 (72%) were eventually transplanted in 11 (3–38) days from a local (50%), regional (50%), or national (<1%) liver; 60 (21%) died; 13 (4.5%) remained waitlisted; and 9 (3.1%) were removed for other reasons. Of those eventually transplanted, MELD did not increase in 57%, increased by 1–3 points in 37%, and increased by ≥4 points in 5.7% after the export. There were 3 cases where OPOs exchanged regional exports within a 24-hour window. The majority of comparable reprioritized candidates were not disadvantaged; however 21% died after an export.
INTRODUCTION
Share-35 was implemented by the Organ Procurement and Transplantation Network (OPTN) on June 18, 2013 as a policy to broaden sharing of deceased donor (DD) livers to waitlisted liver transplant (LT) candidates who were at the highest risk of mortality determined by allocation MELD (1, 2). Under Share-35, deceased-donor livers are offered regionally to candidates with MELD ≥ 35 before being offered locally to candidates with MELD < 35, who would have previously had higher priority (3).
For candidates with MELD < 35, no differences were observed in waitlist mortality in the first 2 years of Share-35 (4), while reductions in waitlist mortality were reported for candidates with MELD ≥ 35 in the first year (5). However, every liver that was exported for a regional share may have deprived a local candidate who otherwise would have been offered that liver first. The population of local candidates who would have been offered these organs first under the pre Share-35 policy has not previously been described. These local candidates may have experienced delays before their eventual LT as a result of being reprioritized, or they may have died on the waitlist before the next liver could be offered. While no differences were observed in the quality of liver offers between pre and post Share 35 (6), it is unclear whether the liver that reprioritized candidates were eventually offered was different in quality from the exported liver that was not offered to them at all. Furthermore, it is unclear how many local candidates were shortly thereafter allocated a regionally shared liver from the same OPO that received the first export – a potentially wasteful scenario of crisscrossing livers (7).
In this retrospective study, we aimed to characterize local candidates who lost their allocation priority to regional candidates with MELD ≥ 35, to enumerate how many were comparable to the regional recipient in MELD score, to describe their eventual disposition from the waitlist, and to describe the extent of wasteful crisscrossed regional sharing that may have occurred.
METHODS
Data Sources
This study used data from the Scientific Registry of Transplant Recipients (SRTR). The SRTR data system includes data on all donor, wait-listed candidates, and transplant recipients in the US, submitted by the members of the Organ Procurement and Transplantation Network (OPTN). The Health Resources and Services Administration (HRSA), U.S. Department of Health and Human Services provides oversight to the activities of the OPTN and SRTR contractors. The interpretation and reporting of these data are the responsibility of the author(s) and in no way should be seen as an official policy of or interpretation by the SRTR or the U.S. Government.
Share-35 Recipients of Regionally Shared Livers
We identified adult LT recipient transplanted at a MELD ≥ 35 with a regionally-shared liver between June 18, 2013 and June 17, 2015 (2 years). Recovering OPOs with no active liver transplant programs were excluded, as they did not have any active liver transplant candidates. We characterized Share-35 recipients by age, gender, race, ABO compatibility with the donor, time on the waitlist when transplanted, and MELD at transplant. We reported the 30-day and 90-day post-transplant survival of the regional recipients. For each Share-35 recipient, we identified whether there was an ABO-identical or compatible local candidate on the waitlist of the recovering OPO.
Reprioritized Candidates
We defined reprioritized candidates as the top local candidate on the waitlist of the recovering OPO who would have been offered the next available DD liver first under the previous allocation system, but lost their priority under Share-35 to higher MELD candidates with MELD ≥ 35 in the region. For each liver regionally exported to a MELD ≥ 35 candidate, we identified the local candidate in the recovering OPO who was active on the waitlist on that day who had 1) the highest allocation MELD score, 2) was ABO-identical or compatible if there were no ABO-identical candidates, 3) had the longest time on the waitlist at the current or higher MELD, and 4) had the longest time on the waitlist, according to allocation priority policy established by the OPTN (3). This local candidate – with a lower MELD score than the regional recipient – we call the reprioritized candidate. Any local waitlist registrant with an equal or higher MELD than the regional recipient would have been offered the liver first, so were not considered reprioritized. We enumerated the number of unique candidates who were reprioritized, as some may have lost priority to several exports. Only the first export to the regional candidate listed for the longest time was considered for candidates who lost priority to multiple exports. Status 1a and 1b were excluded, as Share-35 did not affect the allocation priority of these candidates (3, 8). We characterized reprioritized candidates by age, gender, race, ABO compatibility with the donor, time on the waitlist when the liver was export, MELD when the liver was export and compared them to the regional recipients using Wilcox rank sum test, or χ2 test as appropriate.
Comparable Reprioritized Candidates
We defined comparable reprioritized candidates as reprioritized candidates who had an allocation MELD ≤3 points less than the allocation MELD of the regional candidate to whom the liver was exported to (i.e. the MELD of the reprioritized candidate was comparable to that of the actual regional recipient at the time the liver was exported). We examined whether there was variation between regions in the proportion of reprioritized candidates who were comparable in a multilevel logistic regression.
Waitlist Disposition of Reprioritized Candidates
After a liver was exported, the reprioritized candidate remained on the waitlist until they died or deteriorated in condition, was eventually transplanted (from a locally, regionally, or nationally allocated liver), or was removed for other reasons (e.g. transplanted at another center (multi-listed), condition improved, transferred to another center, refused transplant, etc.). Competing risk regression (9, 10) was used to describe the cumulative incidences of these waitlist outcomes for up to 12 months after the export. We reported the probability of each waitlist removal outcome at 12-months overall and for each region. We reported the median (IQR) time to eventual transplant by allocation (local, regional, or national) for those who were eventually transplanted. The change in MELD between export and eventual transplant of reprioritized candidates was examined in a multi-level linear regression to determine whether there were differences between regions (likelihood ratio test).
Regional Crisscrosses
We defined a regional crisscross to be the situation when a DD liver is exported from OPO A to OPO B, and shortly thereafter, a second DD liver is exported from OPO B to OPO A, where the OPOs are in the same region. Regional crisscrosses can occur between any pair of OPOs in a region resulting in increased CIT for both recipients and additional transport costs, compared to allocating both livers locally. We counted the number of occurrences where a reprioritized candidate was eventually transplanted with a regionally-shared liver from the OPO that the first liver was exported to – regional crisscrosses with Share 35. We reported the number of regional crisscrosses that occurred within time windows of 24, 48, and 72 hours of each other for all reprioritized candidates, and comparable reprioritized candidates, as regional crisscrosses that occur more than 72 hours apart are unlikely to be avoided.
Donor Liver Quality for Reprioritized Candidates who Received a Transplant
We calculated a modified donor risk index (DRI) (11) for exported livers by assuming that they would have been allocated locally (versus regionally) to the reprioritized candidate with a cold ischemia time (CIT) equal to the OPO local average. The modified DRI of the exported liver was compared to the observed DRI (actual CIT and local/regional allocation) of the reprioritized candidate’s eventual transplant by the Wilcox rank sum test.
Statistical Analysis
All analysis was performed using Stata 14 (College Station, Texas), except for competing risk regressions that were done in R 3.1 (the R Foundation for Statistical Computing, Vienna, Austria). For all analysis, p < 0.05 was considered statistically significant. Figures were prepared using Stata and R.
RESULTS
Share-35 Recipients of Regionally Shared Livers
Of 11,075 adult LT performed during the study period, 1768 (16.0%) were regionally shared to recipients of MELD 35 or above. These recipients had a median (IQR) allocation MELD of 39 (37–40) at transplant, were listed for a median (IQR) of 0.6 (0.2–5.0) months when transplanted, and were ABO-identical to the donor in 1573 (89%) of the transplants (Table 1). 30-day and 90-day post-transplant survival was 96% and 94%. Of these 1768 regionally shared livers, 1764 (99.8%) had an active ABO-identical or compatible local candidate in the recovering OPO. Some local candidates lost priority to several exports. The majority (74%) of reprioritized candidates lost priority to only one export, but 4.4% lost priority to 4+ exports (Table 2).
Table 1.
Characteristics of MELD 35+ Recipients and Reprioritized Candidates
| Share-35 Recipients | Reprioritized Candidates | Comparable Reprioritized Candidates | |
|---|---|---|---|
| N | 1768 | 1219 | 291 |
| Age, med (IQR) | 55 (47–61) | 58 (51–63) | 58 (50–63) |
| Female | 673 (38%) | 451 (37%) | 117 (40%) |
| MELD at Export, med (IQR) | - | 31 (27–34) | 37 (34–38) |
| MELD at Transplant, med (IQR) | 39 (37–40) | 31 (27–36) | 37 (35–39) |
| Median (IQR) months on waitlist | 0.6 (0.2–5.0) | 4.6 (0.8–13) | 4.3 (0.5–20) |
| White | 1188 (67%) | 848 (70%) | 177 (61%) |
| Black | 190 (11%) | 110 (9.0%) | 30 (10%) |
| Hispanic | 299 (17%) | 197 (16%) | 68 (23%) |
| Other | 91 (5.2%) | 64 (5.3%) | 16 (5.5%) |
| ABO-identical | 1573 (89%) | 1121 (92%) | 267 (92%) |
| ABO-compatible | 164 (9.3%) | 98 (8.0%) | 24 (8.3%) |
| ABO-incompatible | 31 (1.8%) | - | - |
MELD, Model for End-Stage Liver Disease
Table 2.
Number of Exports that Local Candidates Lost Priority to
| Number of Exports | Any MELD | Number of Reprioritized Candidates | ||
|---|---|---|---|---|
| MELD within 3-1 points | MELD within 2-1 points | MELD within 1 point | ||
| Any | 1219 (100%) | 291 (24%) | 198 (16%) | 111 (9.1%) |
| 1 | 907 (74%) | 210 | 152 | 84 |
| 2 | 193 (16%) | 49 | 29 | 15 |
| 3 | 66 (5.4%) | 21 | 12 | 9 |
| 4 | 30 (2.5%) | 7 | 3 | 1 |
| 5+ | 23 (1.9%) | 4 | 2 | 2 |
Local candidates may have lost priority to regional candidates with Share-35 in several exports.
MELD, Model for End-Stage Liver Disease
Reprioritized Candidates
There were 1219 unique reprioritized candidates among the 1764 regionally shared livers (Table 2). Reprioritized candidates had a median (IQR) waitlist MELD of 31 (IQR 27–34) at the time of the export, lower than the median MELD at transplant of 39 for regional recipients (p<0.001). They were similar in sex (p=0.4), and race (p=0.3) to the regional recipients, but were slightly older (p<0.001) and were listed longer, a median (IQR) of 4.6 (0.8–13) months at the export versus 0.6 (0.2–5.0) months at transplant for regional recipients (Table 1, p<0.001). The median MELD at export (by OPO) of reprioritized candidates ranged from 22 to 37 between 52 OPOs (Figure 1)
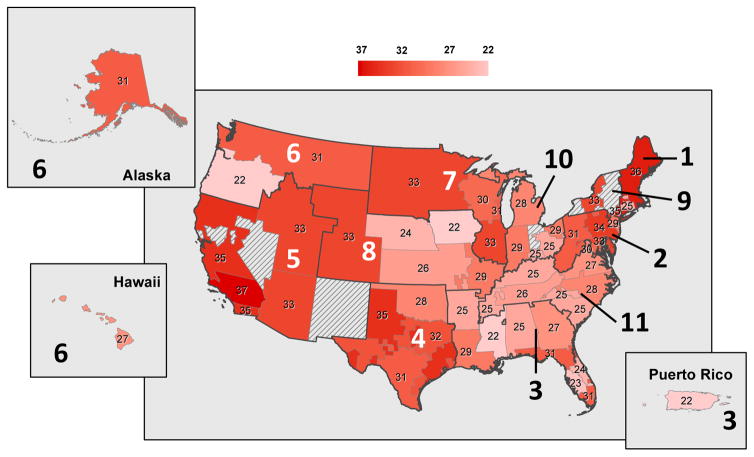
Figure 1. Median MELD of Reprioritized Candidates by OPO.
Each OPO is labeled with the median MELD of reprioritized candidates. Regions are labeled in larger text. 1219 local candidates lost allocation priority to a regional recipient with a MELD 35 or greater. Reprioritized candidates were identified by considering the waitlist in the recovering OPO on the day of a regionally shared liver that was exported to a recipient with MELD 35+. The proportion of reprioritized candidates who were comparable varied between regions (p<0.001) and was lower than the national proportion (24%) in regions 1 (7.7%), 3 (7.7%), 6 (11%), 8 (6.0%), 10 (13%), and 11 (2.6%); and higher in regions 2 (29%), 4 (28%), 5 (55%), 7 (30%), and 9 (50%).
Comparable Reprioritized Candidates
291 (24%) of reprioritized candidates had a comparable MELD (within 3 points of the regional recipient) and were listed 4.3 (0.5–20) months at the export, longer than the 0.6 (0.2–5.0) months that regional recipients were listed when transplanted (p<0.001). 198 (16%) had a MELD score within 2 points, and 111 (9.1%) had a MELD score within 1 point of the regional recipient. Comparable reprioritized candidates were similar in sex (p=0.7) to regional recipients, but were slightly older (p<0.001), and differed in race (p=0.047). The proportion of reprioritized candidates who were comparable varied between regions (p<0.001) and was lower than the overall proportion (24%) in regions 1 (7.7%), 3 (7.7%), 6 (11%), 8 (6.0%), 10 (13%), and 11 (2.6%); and higher in regions 2 (29%), 4 (28%), 5 (55%), 7 (30%), and 9 (50%).
Waitlist Disposition of Reprioritized Candidates
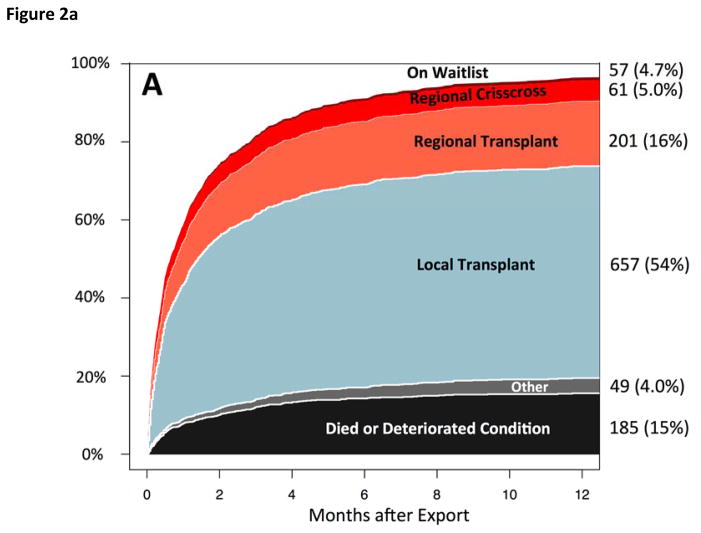
Of reprioritized candidates, 928 (76%) were eventually transplanted at 12-months after the export, 185 (15%) died or were removed for deteriorated condition, 57 (4.7%) remained waitlisted, and 49 (4.0%) were removed for other reasons (Figure 2a). Among those who were eventually transplanted, 657 (71%) received a DDLT locally in a median (IQR) of 19 (6–53) days, 262 (28%) received a DDLT regionally in 16 (5–54) days, and 9 (1%) received a nationally shared liver in a median (IQR) of 58 (25–91) days. The MELD increased between the export and the eventual transplant by a mean of 0.9 MELD points (p<0.001) and did not differ by region (p=0.3). 45% of reprioritized candidates were eventually transplanted at the same MELD they were at when the liver was exported; 26% had an increase in MELD by 1–3 points when eventually transplanted, and 15% had an increase in MELD that was 4 points or higher. 13% had a decreased MELD by median (IQR) of 3 (1–5) points when eventually transplanted. Waitlist disposition varied by region (table 3a, p=0.04), but not by ABO (table 4, p>0.9).
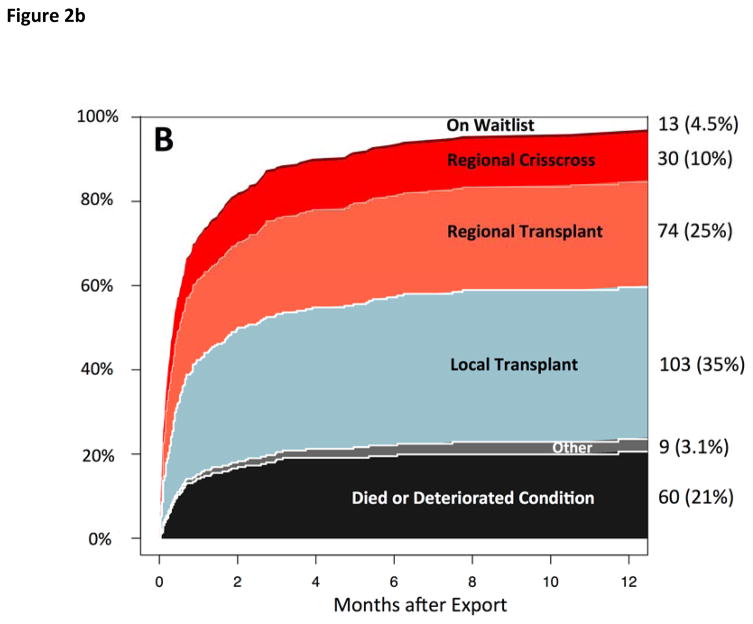
Figure 2.
Figure 2a: Waitlist Outcomes of Reprioritized Candidates
Among reprioritized candidates, 928 (76%) were eventually transplanted; 9 (0.7%) were transplanted nationally (not shown).
Figure 2b: Waitlist Outcomes of Comparable Reprioritized Candidates
Among comparable reprioritized candidates, 209 (72%) were eventually transplanted; 2 (0.7%) were transplanted nationally (not shown).
Table 3a.
Waitlist Disposition of Reprioritized Candidates by Region at 12-months
| Region | Died | Transplanted (local) | Transplanted (region/national) | On Waitlist / Other |
|---|---|---|---|---|
| 1 | 3 (23%) | 5 (38%) | 2 (15%) | 3 (23%) |
| 2 | 31 (22%) | 69 (48%) | 28 (19%) | 13 (9%) |
| 3 | 24 (10%) | 150 (61%) | 57 (23%) | 15 (6%) |
| 4 | 25 (16%) | 85 (56%) | 26 (17%) | 16 (11%) |
| 5 | 29 (13%) | 71 (33%) | 91 (42%) | 24 (11%) |
| 6 | 1 (5%) | 15 (79%) | 2 (11%) | 1 (5%) |
| 7 | 23 (17%) | 79 (59%) | 18 (13%) | 15 (11%) |
| 8 | 10 (12%) | 55 (64%) | 13 (15%) | 6 (7%) |
| 9 | 2 (10%) | 9 (45%) | 7 (35%) | 2 (10%) |
| 10 | 19 (24%) | 44 (56%) | 10 (13%) | 4 (5%) |
| 11 | 18 (15%) | 75 (64%) | 17 (15%) | 7 (6%) |
Waitlist disposition after export varied by region (p = 0.04).
Table 4.
Waitlist Disposition of Comparable Reprioritized Candidates by ABO at 12-months
| ABO | Died | Transplanted | Other Removal | On Waitlist |
|---|---|---|---|---|
| A | 78 (16%) | 370 (76%) | 15 (3%) | 26 (5%) |
| AB | 3 (13%) | 19 (79%) | 1 (4%) | 1 (4%) |
| B | 21 (14%) | 111 (77%) | 6 (4%) | 7 (5%) |
| O | 83 (15%) | 428 (76%) | 27 (5%) | 23 (4%) |
χ2 test, p>0.9
Waitlist Disposition of Comparable Reprioritized Candidates
Of comparable reprioritized candidates (MELD within 3 points of regional recipient), 209 (72%) were eventually transplanted at 12-months after the export, 60 (21%) died or were removed for deteriorating condition, 13 (4.5%) remained waitlisted, and 9 (3.1%) were removed for other reasons (Figure 2b). Comparable reprioritized candidates who were eventually transplanted received their transplant in a median (IQR) of 11 (3–38) days, sooner than non-comparable reprioritized candidates who were transplanted in a median (IQR) of 22 (7–57) days (p=0.001). Among those who were eventually transplanted, 103 (50%) received a DDLT locally in a median (IQR) of 13 (3–35) days, 104 (50%) received a DDLT regionally in 8 (3–45) days, and 2 (0.7%) received a nationally shared liver in 7–58 days. The time to eventual transplant did not differ whether it was locally or regionally allocated (p=0.3). MELD did not differ between the export and the eventual transplant of comparable reprioritized candidates (p=0.7) and did not vary by region (p=0.2). 43% of comparable reprioritized candidates were eventually transplanted at the same MELD they were at when the liver was exported; 37% had an increase in MELD by 1–3 points when eventually transplanted, and 5.7% had an increase in MELD that was 4 points or higher. 14% had a decreased MELD by median (IQR) of 4 (2–8) points when eventually transplanted.
Regional Crisscrosses
For all reprioritized candidates, there were only 3 regional crisscrosses that occurred within 24 hours of each other, 4 regional crisscrosses that occurred 24–48 hours apart, and 2 regional crisscrosses that occurred 48–72 hours apart. These regional crisscrosses occurred in regions 5 (n=3), 2 (n=2), 4 (n=1), 7 (n=1), 11 (n=1) and 3 (n=1). Of comparable reprioritized candidates, there were only 3 regional crisscrosses that occurred within 24 hours of each other, 1 regional crisscrosses that occurred 24–48 hours apart, and 2 regional crisscrosses that occurred 48–72 hours apart. These regional crisscrosses occurred in regions 5 (n=3), 2 (n=1), 4 (n=1), and 7 (n=1).
DRI of Exported Livers Compared to Eventual Transplants
Livers that were not transplanted in their recovering OPO, but were exported to another OPO for transplantation to a MELD 35+ candidate would have had a median (IQR) DRI of 1.31 (1.13–1.57) if they were transplanted locally instead. The eventual transplants (both local and regional) of reprioritized candidates had a median DRI of 1.41 (1.19–1.73), higher than the DRI the exported livers would have had (p<0.001); however, the actual DRI of exported livers was median (IQR) 1.46 (1.26–1.75) and did not differ from the DRI of 1.41 of eventual transplants (p=0.05).
DISCUSSION
Among 1768 livers that were regionally shared to MELD 35+ recipients, there were 1219 unique reprioritized candidates, 291 who were comparable to the regional recipient. These comparable reprioritized candidates were similar in sex to the regional recipient, but were slightly older, differed in race, and were on the waitlist longer. The majority of these candidates were eventually transplanted in 1–2 weeks with only a slight increase in MELD, and may have benefited themselves from regionally shared livers; however, 21% died after the export.
With the Share-35 policy, candidates with MELD ≥ 35 received more offers (6), and were transplanted at a 27% increased rate (5). Waitlist mortality decreased by 30% for candidates with MELD > 30 and by 8% for all candidates in the initial year (5). Among MELD ≥ 35 candidates who received a regionally-shared transplant, their short-term post-transplant survival was 96%. Whether this gain in survival for regional recipients came from a loss for local candidates who lost their allocation priority was unknown (7). We now showed that the majority of comparable reprioritized candidates were, in general, eventually transplanted in a short amount of time, as some also received regionally shared livers. However, 60 (21%) died on the waitlist before they could be transplanted, and there is indeed a trade-off between the risk of mortality of MELD 35+ candidates versus the risk for these MELD < 35 candidates.
While we found that reprioritized candidates were eventually transplanted with livers with slightly higher DRI than the modified DRI of exported livers, there was no difference between the observed DRI of exported livers versus the DRI of the eventual liver. In other words, the livers received by reprioritized candidates who eventually received a transplant appeared to be slightly worse quality than the livers that they would have received under pre Share-35 allocation policy, but only because the first liver would not have been exported. Increased transportation costs and cold ischemia time have been previously examined (12–14). Although regional sharing incurs additional CIT and a potential decrease in organ quality, a regionally shared liver is better than no liver to a high MELD candidate (15–17).
Similar to Halazun et al (18), we observed regional variation in the impact of Share-35. The proportion of reprioritized candidates who were comparable to the regional recipients varied between regions, with regions in the west and the northeast having the highest proportion of comparable reprioritized candidates. In regions where many of the reprioritized candidates also have high MELDs (but not > 35), it remains arguable that broader sharing can reduce waitlist mortality, especially if the region-level risk of mortality is exceedingly high for all candidates on the waitlist. Conversely, in regions where there are few comparable reprioritized candidates, broader sharing to high-MELD candidates would decrease their mortality, but not at the expense of local candidates with much lower MELD scores. That there are many areas where median MELD for reprioritized candidates is 35 or higher indicates that Share-35 cannot overcome the vast imbalances in supply and demand among the 11 regions to make transplants available to the candidates with extremely high MELDs. Redrawing optimal sharing districts may be a more promising approach to getting livers to the candidates who need them most urgently than sharing within existing regions, because the results of Share-35 demonstrate that the regions themselves have very disparate ratios of liver supply to demand.
A limitation of our study was that we did not know whether reprioritized candidates would have accepted the organ had they been offered locally first. Reprioritized candidates might have previously declined organ offers. However, most reprioritized candidates had a MELD above 30 and it is unlikely that a candidate with a high MELD would decline an offered liver that was ABO identical. Furthermore, the offers were, in general, very high quality and accepted for a regionally shared transplant.
The majority of comparable reprioritized candidates were eventually transplanted in 1–2 week after a liver was exported. Regional recipients of the exported livers had excellent short-term post-transplant survival. The extent of avoidable regional crisscrossing of livers was minimal between comparable reprioritized candidates. In general, Share-35 did not appear to disadvantage local candidates with comparably high MELD scores to regional MELD 35+ candidates; however, there was still a subset of reprioritized candidates who suffered.
Supplementary Material
Table 3b.
Waitlist Disposition of Comparable Reprioritized Candidates by Region at 12-months
| Region | Died | Transplanted (local) | Transplanted (region/national) | On Waitlist / Other |
|---|---|---|---|---|
| 1 | 0 (0%) | 1 (100%) | 0 (0%) | 0 (0%) |
| 2 | 12 (29%) | 15 (37%) | 13 (32%) | 1 (2%) |
| 3 | 4 (21%) | 7 (37%) | 8 (42%) | 0 (0%) |
| 4 | 10 (24%) | 13 (31%) | 14 (33%) | 5 (12%) |
| 5 | 16 (14%) | 36 (31%) | 56 (47%) | 10 (8%) |
| 6 | 0 (0%) | 2 (100%) | 0 (0%) | 0 (0%) |
| 7 | 11 (28%) | 18 (45%) | 7 (18%) | 4 (10%) |
| 8 | 1 (20%) | 3 (60%) | 1 (20%) | 0 (0%) |
| 9 | 1 (10%) | 5 (50%) | 3 (30%) | 1 (10%) |
| 10 | 4 (40%) | 3 (30%) | 3 (30%) | 0 (0%) |
| 11 | 1 (33%) | 0 (0%) | 1 (33%) | 1 (33%) |
Waitlist disposition after export did not vary by region (p=0.4).
Acknowledgments
Dr. Segev is supported by grant number K24DK101828 from the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK).
Abbreviations
- CIT
cold ischemia time
- DDLT
deceased donor liver transplantation
- DRI
donor risk index
- LT
liver transplant
- MELD
Model for End-Stage Liver Disease
- OPO
organ procurement organization
- OPTN
Organ Procurement and Transplantation Network
- SRTR
Scientific Registry of Transplant Recipients
Footnotes
DISCLOSURE
The authors of this manuscript have no conflicts of interest to disclose as described by the American Journal of Transplantation.
Additional Supporting Information may be found in the online version of this article.
References
- 1.Freeman RB, Wiesner RH, Edwards E, Harper A, Merion R, Wolfe R, et al. Results of the first year of the new liver allocation plan. Liver transplantation : official publication of the American Association for the Study of Liver Diseases and the International Liver Transplantation Society. 2004;10(1):7–15. doi: 10.1002/lt.20024. [DOI] [PubMed] [Google Scholar]
- 2.Kamath PS, Wiesner RH, Malinchoc M, Kremers W, Therneau TM, Kosberg CL, et al. A model to predict survival in patients with end-stage liver disease. Hepatology. 2001;33(2):464–70. doi: 10.1053/jhep.2001.22172. [DOI] [PubMed] [Google Scholar]
- 3. [Oct 13, 2015];Policy 9: allocation of livers and liver-intestines: Organ Procurement and Transplantation Network. Available from: http://optn.transplant.hrsa.gov/ContentDocuments/OPTN_Policies.pdf.
- 4.Edwards EB, Harper AM, Hirose R, Mulligan DM. The Impact of Broader Regional Sharing of Livers: 2 Year Results of “Share 35” (LT-15-441) Liver transplantation : official publication of the American Association for the Study of Liver Diseases and the International Liver Transplantation Society. 2016 doi: 10.1002/lt.24418. [DOI] [PubMed] [Google Scholar]
- 5.Massie AB, Chow EK, Wickliffe CE, Luo X, Gentry SE, Mulligan DC, et al. Early changes in liver distribution following implementation of Share 35. American journal of transplantation : official journal of the American Society of Transplantation and the American Society of Transplant Surgeons. 2015;15(3):659–67. doi: 10.1111/ajt.13099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Washburn K, Harper A, Baker T, Edwards E. Changes in liver acceptance patterns after implementation of Share 35. Liver transplantation : official publication of the American Association for the Study of Liver Diseases and the International Liver Transplantation Society. 2016;22(2):171–7. doi: 10.1002/lt.24348. [DOI] [PubMed] [Google Scholar]
- 7.Feng S, O’Grady J. Share 35: a liver in time saves lives? American journal of transplantation : official journal of the American Society of Transplantation and the American Society of Transplant Surgeons. 2015;15(3):581–2. doi: 10.1111/ajt.13102. [DOI] [PubMed] [Google Scholar]
- 8.Kremers WK, van IM, Kim WR, Freeman RB, Harper AM, Kamath PS, et al. MELD score as a predictor of pretransplant and posttransplant survival in OPTN/UNOS status 1 patients. Hepatology. 2004;39(3):764–9. doi: 10.1002/hep.20083. [DOI] [PubMed] [Google Scholar]
- 9.Fine JP, Gray RJ. A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc. 1999;94(446):496–509. [Google Scholar]
- 10.Gray RJ. R package version 2.2–7. 2014. cmprsk: Subdistribution Analysis of Competing Risks. [Google Scholar]
- 11.Feng S, Goodrich NP, Bragg-Gresham JL, Dykstra DM, Punch JD, DebRoy MA, et al. Characteristics associated with liver graft failure: the concept of a donor risk index. American journal of transplantation : official journal of the American Society of Transplantation and the American Society of Transplant Surgeons. 2006;6(4):783–90. doi: 10.1111/j.1600-6143.2006.01242.x. [DOI] [PubMed] [Google Scholar]
- 12.DuBay DA, MacLennan PA, Reed RD, Fouad M, Martin M, Meeks CB, et al. The impact of proposed changes in liver allocation policy on cold ischemia times and organ transportation costs. American journal of transplantation : official journal of the American Society of Transplantation and the American Society of Transplant Surgeons. 2015;15(2):541–6. doi: 10.1111/ajt.12981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fernandez H, Weber J, Barnes K, Wright L, Levy M. Financial Impact of Liver Sharing and Organ Procurement Organizations’ Experience With Share 35: Implications for National Broader Sharing. American journal of transplantation : official journal of the American Society of Transplantation and the American Society of Transplant Surgeons. 2016;16(1):287–91. doi: 10.1111/ajt.13436. [DOI] [PubMed] [Google Scholar]
- 14.Gentry SE, Chow EK, Dzebisashvili N, Schnitzler MA, Lentine KL, Wickliffe CE, et al. The Impact of Redistricting Proposals on Health Care Expenditures for Liver Transplant Candidates and Recipients. American journal of transplantation : official journal of the American Society of Transplantation and the American Society of Transplant Surgeons. 2016;16(2):583–93. doi: 10.1111/ajt.13569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Merion RM, Schaubel DE, Dykstra DM, Freeman RB, Port FK, Wolfe RA. The survival benefit of liver transplantation. American journal of transplantation : official journal of the American Society of Transplantation and the American Society of Transplant Surgeons. 2005;5(2):307–13. doi: 10.1111/j.1600-6143.2004.00703.x. [DOI] [PubMed] [Google Scholar]
- 16.Schaubel DE, Sima CS, Goodrich NP, Feng S, Merion RM. The survival benefit of deceased donor liver transplantation as a function of candidate disease severity and donor quality. American journal of transplantation : official journal of the American Society of Transplantation and the American Society of Transplant Surgeons. 2008;8(2):419–25. doi: 10.1111/j.1600-6143.2007.02086.x. [DOI] [PubMed] [Google Scholar]
- 17.Karp SJ, Johnson S, Evenson A, Curry MP, Manning D, Malik R, et al. Minimising cold ischaemic time is essential in cardiac death donor-associated liver transplantation. HPB : the official journal of the International Hepato Pancreato Biliary Association. 2011;13(6):411–6. doi: 10.1111/j.1477-2574.2011.00307.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Halazun KJ, Mathur AK, Rana AA, Massie AB, Mohan S, Patzer RE, et al. One Size Does Not Fit All-Regional Variation in the Impact of the Share 35 Liver Allocation Policy. American journal of transplantation : official journal of the American Society of Transplantation and the American Society of Transplant Surgeons. 2016;16(1):137–42. doi: 10.1111/ajt.13500. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.