Abstract
Background
Funding toward surgical research through the National Institutes of Health (NIH) has decreased relative to other medical specialties. This study was initiated to characterize features of academically successful, surgeon-scientists and departments of surgery. We hypothesized that there may be decreases in young investigators obtaining independent NIH awards and that successful academic departments of surgery may be depending increasingly on PhD faculty.
Methods
The NIH RePORTER database was queried for grants awarded to Departments of Surgery during fiscal years 2003 and 2013. Grant summaries were categorized by research methodology. Training of the principal investigator training and academic position were determined through the RePORTER database and publicly-available academic biographies. Institutions were ranked by number of grants funded.
Results
Between 2003 and 2013, total surgery grants awarded decreased by 19%. The number of NIH-funded, clinically-active surgeons (MDsMDs) decreased 11%, while funded PhDs increased 9%; however, clinically active junior faculty have comprised an increasing proportion of funded MDs (from 20% to 38%). Shifts in research topics include an increasing proportion of investigators engaged in outcomes research. Among institutions ranking in the top 20 for surgical research in both 2003 and 2013 (N = 15), the ratio of MDs to PhDs was 2:1 in both fiscal years. Among institutions falling out of the top 20, this ratio was less than 1:1.
Conclusions
There has been an expansion of outcomes-based surgical research. The most consistently successful institutions are those that actively cultivate MD researchers. Encouragingly, the number of young, independently-funded surgeon-scientists in America appears to be increasing.
Keywords: National Institutes of Health, Surgical research, research funding, academic surgery, mentorship
INTRODUCTION
Research by clinically active surgeons has led to some of the greatest advances in medical science, including transplantation (1), cancer therapy (2, 3), coronary and cardiac physiology (4), and countless others. Moreover, research and innovation are tied closely to professional achievement at academic centers. At the individual level, the ability to obtain funding and complete groundbreaking projects is often considered for recruitment and promotion (5, 6). At the institutional level, laying the foundation for innovation garners multi-institutional collaboration and provides competitive advantages in the clinical market share (7). For departments of surgery within the United States, the most broadly recognized measure of academic achievement is consistent funding support through the National Institutes of Health (NIH) (8).
Over the past decade, the adjusted NIH budget has decreased to its lowest point in 13 years (9, 10). Surgeon-scientist, who have had traditionally a lesser volume of NIH award applications and lesser success rate of their applications have been especially affected (11–13). A part of this trend may be attributable to increasing clinical and administrative responsibilities in an era of resident work-hour restrictions and stringent outcomes reporting (14). Consequently, many institutions are turning to dedicated PhD personnel to contribute to research endeavors (15).
Nevertheless, there remain many incentives that support the cultivation of a consistent physician-scientist workforce. The share of United States medical research support attributable from industry is increasing. These industry funders are gradually shifting away from basic science research toward late-phase clinical trials (16). In the public sector, the NIH is an especially efficient spring-board for clinical inventions. Products developed through the NIH have a high rate of attaining orphan drug status and priority review by the Food and Drug Administration (17). Tthere remains, however, a constant need to refocus the NIH toward clinically-relevant pursuits—a need filled most appropriately by practicing physicians. Thus far, no study has stratified national research contributions within surgery across clinical MDs, non-clinical MDs, and PhDs. In light of this, the purpose of this study is to characterize NIH-funded researchers within departments of surgery across the United States. By comparing recipients of NIH funding in the years 2003 and 2013, we hoped to provide insight into factors that contribute to a consistently successful academic surgery department. We hypothesized that the number of junior faculty—assistant and associate professors—obtaining independent NIH awards have decreased, and that successful academic departments of surgery are depending increasingly on PhD faculty.
METHODS
Using previously reported methods of data collection (18), the NIH RePORTER database (Research Portfolio Online Reporting Tool, available at http://report.nih.gov) was queried for all active research project grants within the United States and territories during the fiscal years of 2003 and 2013. The “Department” search field was used to identify grants allocated to departments of surgery. Because the project focused on faculty research, F- and T-awards were excluded, because these represent resident and student training grants. As the purview of surgery departments vary across institutions, only grants allocated to core surgical disciplines were retained; thus, we excluded grants awarded to divisions of neurosurgery, orthopedics, otolaryngology, ophthalmology, urology, and gynecology. Grants were included regardless of the advanced degree of the principal investigator (M.D., Ph.D., etc.). The exported data included summary descriptions of research, total costs, and investigator information. For each grant, only the principal investigator was recorded in our dataset. Total costs of grants were adjusted to 2013 equivalent dollars using an inflation adjustment factor of 1.27 (19).
The protocol used to categorize NIH grants by methodology has been reported previously (18). Briefly, research summary descriptions for all grants were reviewed by one of two study investigators (YH, BE). Each investigator reviewed grants from both datasets (2003 and 2013). Based on these descriptions, the primary methodology for each grant was classified into one of six categories: basic science, translational, clinical trial, outcomes, operative technique, and other. Projects that incorporated several methodologies were classified as translational. One hundred and fifty grants were reviewed by both reviewers to assess inter-rater agreement (0.85); all disagreements originated from the differentiation between basic science and translational research.
The academic position and advanced degree (MD vs PhD) of the principal investigator for each NIH grant was extracted from the NIH RePORTER investigator description page. When these data were not immediately available, investigator curriculum vitae or professional biographies were acquired through online search, and the academic position of the investigator at the time of funding was recorded. Among MD researchers, those who did not have an active clinical practice were designated as non-clinical MD-researchers. Faculty with both MD and PhD degrees were classified as clinically-active MDs if they were practicing clinicians, or as PhDs if they held a research position only. Departments of surgery were ranked by total number of active NIH grants in 2003 and in 2013. Proportional composition of MDs and PhDs was compared among the top 20 surgery departments and all remaining surgery departments using the Chi-squared test. Due to overlap in principal investigators between 2003 and 2013, tests of statistical significance between these two datasets were not performed.
RESULTS
We identified 1125 grants (613 from 2003 and 512 from 2013) that met inclusion criteria. Inflation-adjusted NIH funding to surgical research decreased by 19.1% from $270.4M in 2003 to $218.7M in 2013. Details regarding trends in funding across methodologic and specialty subgroups have been reported previously (18). In 2013, the majority of active surgery grants were funded through the National Cancer Institute (27%), National Heart, Lung, and Blood Institute (25%), and the National Institute of Diabetes and Digestive and Kidney Diseases (18%). Nearly half of active grants resulted from review by special emphasis panels (44%), while other top study sections included Surgery, Anesthesiology and Trauma (11%), Bioengineering, Technology and Surgical Sciences (8%), and the Subcommittee on Education through National Cancer Institute (3%). Total number of principal investigators within departments of surgery funded through the NIH decreased 4.5% (433 to 412, Table 1). The proportion of MD and PhD investigators remained relatively constant, but PhD investigators contributed to an increasing proportion of total NIH surgical research funding (34% to 47%). This increase was due to a greater decrease in funding-per-investigator among MD investigators compared to that of PhDs.
Table 1.
Research demographics and methodology
| 2003 | 2013 | |
|---|---|---|
| Funded PI | 433 | 412 |
| MD | 60.7% | 56.1% |
| PhD | 34.2% | 39.1% |
| Nonclinical MD | 5.1% | 4.9% |
|
| ||
| Total Funding Cost | ||
| MD | 61.0% | 51.0% |
| PhD | 34.2% | 47.0% |
| Nonclinical MD | 4.9% | 1.9% |
|
| ||
| Median Award Cost ($K)* | ||
| MD | 357.4 | 309.7 |
| PhD | 359.0 | 317.8 |
| Nonclinical MD | 378.7 | 319.6 |
|
| ||
| Median Funding per PI ($K)* | ||
| MD | 369.4 | 318.6 |
| PhD | 390.0 | 354.3 |
| Nonclinical MD | 442.2 | 321.7 |
|
| ||
| MD Rank | ||
| Chair | 10.2% | 5.8% |
| Chief/Director | 26.5% | 22.2% |
| Professor | 39.8% | 33.3% |
| Associate professor | 14.4% | 22.2% |
| Assistant professor | 4.5% | 16.5% |
| Unknown | 4.6% | <0.01% |
|
| ||
| MD Research Area | ||
| Basic science | 43.6% | 42.5% |
| Translational | 43.9% | 34.7% |
| Clinical trial | 3.8% | 6.7% |
| Outcomes | 4.2% | 12.0% |
| Operative | 2.7% | 0.9% |
| Other | 1.9% | 3.2% |
PI: principal investigator.
Adjusted dollar awards.
Information about academic position was not available for two investigators (1 clinically-active MD) from 2013 (0.5%) and 24 investigators (12 clinically-active MDs) from 2003 (5.6%). Among investigators with known faculty rank, the proportion of funded MD investigators who were junior faculty—associate or assistant professors—doubled from 19.8% (50/252) to 38.8% (90/232) (Table 1). Junior faculty were awarded less funding per investigator than senior faculty in both periods; however, this gap narrowed in 2013 (Table 2). Translational and basic science projects dominated during both periods for investigators at all levels of rank (Table 2). Nevertheless, outcomes research increased, comprising 4.2% of projects in 2003 and 12% in 2013.
Table 2.
Junior and Senior faculty in 2003 and 2013
| 2003
|
2013
|
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Junior | Senior | p | Junior | Senior | p | |||||
| Total Funding ($K)* | 12220.4 | 98542.0 | 21581.2 | 76559.8 | ||||||
| Median Funding ($K)* | 168.2 | 369.6 | < 0.001 | 175.0 | 332.2 | < 0.001 | ||||
| Methodology | 0.657 | 0.041 | ||||||||
| Basic/Translational | 46 | 92.0% | 177 | 87.6% | 70 | 77.8% | 104 | 73.2% | ||
| Outcomes | 1 | 2.0% | 9 | 4.5% | 14 | 15.6% | 16 | 11.3% | ||
| Other | 3 | 6.0% | 16 | 7.9% | 6 | 6.7% | 22 | 15.5% | ||
| Award | < 0.001 | < 0.001 | ||||||||
| K | 33 | 66.0% | 27 | 13.4% | 46 | 51.1% | 2 | 1.4% | ||
| R | 17 | 30.0% | 145 | 71.8% | 40 | 44.4% | 95 | 66.9% | ||
| R01 | 12 | 126 | 27 | 75 | ||||||
| R03 | 0 | 10 | 0 | 1 | ||||||
| R21 | 5 | 0 | 10 | 11 | ||||||
| U | 2 | 4.0% | 15 | 7.4% | 2 | 2.2% | 39 | 27.5% | ||
| P | 0 | 0.0% | 10 | 5.0% | 1 | 1.1% | 5 | 3.5% | ||
Junior: assistant and associate professors
Senior: professors, division chiefs, department chairs
Adjusted dollar awards.
To understand better the evolution of MD and PhD investigators within departments of surgery, we focused on those investigators funded in 2013 who were not previously funded in 2003 (Table 3). Among these newly-funded investigators, 40.5% were PhDs. More than half of all newly-funded MD investigators were junior faculty (52.6%), and most were trained in a clinical subspecialty (80.5%). Despite a trend in proportional increase of outcomes-based projects (14.3%), the majority of research performed by these newly-funded investigators remains within the areas of basic and translational sciences (74.7%). Among investigators funded in both 2013 and 2003, 97/133 (72.9%) had an R-type grant in 2013 (78.4% R01, 11.3% R21, 4% R25, 6% other). Notably, 29 (22%) of these investigators changed institutions over the study period.
Table 3.
Characteristics of 2013 NIH surgery investigators not funded in 2003
| N(%) | |
|---|---|
| New Principal Investigators | 279 |
| MD | 154 (55.2%) |
| PhD | 113 (40.5%) |
| Nonclinical MD | 12 (4.3%) |
| New MD Research Area | |
| Basic science | 63 (40.9%) |
| Translational | 52 (33.8%) |
| Clinical trial | 10 (6.5%) |
| Outcomes | 22 (14.3%) |
| Operative | 1 (0.6%) |
| Other | 6 (3.9%) |
| New MD Rank | |
| Chair | 3 (1.9%) |
| Chief/Director | 33 (21.4%) |
| Professor | 37 (24.0%) |
| Associate professor | 44 (28.6%) |
| Assistant professor | 37 (24.0%) |
| New MD Fellowship Training | |
| Clinical | 124 (80.5%) |
| Research only | 3 (1.9%) |
| None | 27 (17.5%) |
| New MD Awards | |
| Total | 186 |
| K | 47 (25.3%) |
| R | 102 (54.8%) |
| U | 34 (18.3%) |
| Other | 3 (1.6%) |
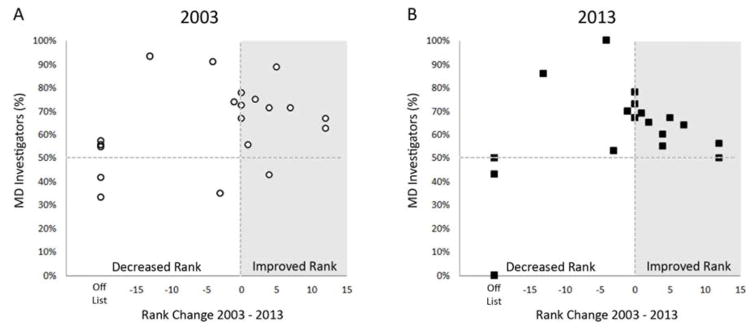
Our final aim was to characterize the patterns of personnel within surgery departments that have had durable success in research. Change in total grants awarded over time among the top 20 NIH-awarded departments of surgery in 2003 is shown in Figure 1. Out of the top 20 institutions in 2003, 15 remained in the top 20 in 2013. Among the top 20 institutions in 2013, the proportion of funded investigators who were clinically-active MDs was 59.3%. By comparison, among surgical departments outside the top 20 that received at least one grant (N = 56 during both periods), this proportion was 51.0% (p = 0.12). Further, institutions in the top 20 in 2013 were more likely to be led by an NIH-funded department chair (45% vs 7%, p < 0.01). Figure 2 shows the relationship between departmental ranking over time and the proportional composition of funded investigators in each department. For departments whose rank either stayed the same or “improved” during the study period, the proportion of investigators who were clinically-active MDs was 68% in 2003 and 64% in 2013. At the other extreme, among institutions that fell out of the top 20, this proportion was 48% in 2003 and 39% in 2013. Thus, surgical departments that experienced the most enduring success in NIH-funded research tended to be those that maintained a roughly 2-to-1 ratio of funded MDs versus PhDs. Within the top 20 institutions of 2013, 53 of 151 (35.1%) MDs were also funded in 2003. Thirteen of these investigators with sustained funding (24.5%) were newly acquired into one of these top 20 institutions over the study period.
Figure 1.
Change in total number of NIH grants (A) and proportion of NIH grants (B) between 2003 and 2013 for the 20 institutions with the most active NIH grants in 2003 (ranked high to low, A through T). Increase in grants over this period is shown as positive bars on the Y-axis; decrease in grants shown as negative bars. Total number of surgery grants among these institutions decreased from 341 to 326.
Figure 2.
Proportion of investigators with MD degrees among top 20 departments of surgery in NIH grants awarded. Among institutions with unchanged or improving rank in grants awarded (rank change > 0, shaded area), the average ratio of funded MD to PhD investigators was 68% 2003 (A) and 64% in 2013 (B).
DISCUSSION
Over the past decade, an increasing proportion of NIH-funded research conducted within departments of surgery has been contributed by PhD investigators. In terms of funding-per-investigator, PhDs outperformed MD counterparts. The highest-performing surgery departments are those that maintained a 2-to-1 ratio of MD-to-PhD investigators. Unexpectedly, but encouragingly, the contribution to MD-led research by junior clinical faculty has increased over time.
As early as the 1970’s, it was noted that basic scientists within clinical departments attained some of the greatest rates of NIH grant awards (20). PhD investigators frequently have expansive experience in study design and grant-writing and a broad, hands-on skillset in basic science. Despite these advantages, PhDs in clinical departments are less likely to be promoted and less likely to pursue a tenure track than clinicians (21). Between the 1970s and 1990s, the number of PhDs on faculty at medical schools doubled (15). By 1999, PhDs accounted for more than half of NIH-funded investigators across a number of specialties including surgery. Our data capturing the years 2003 and 2013 show that, within core surgical disciplines of the 21st century, clinical MDs comprise the majority of NIH-funded investigators. This finding could indicate that the demographic of clinically active surgeon-scientists is experiencing a rebirth. Indeed, the increasing proportion of junior MD investigators supports this explanation. An alternative reason could be that certain subspecialties not included in our dataset—such as neurosurgery, orthopedics, and ophthalmology—may have a greater proportion of PhD investigators than the classic divisions of a department of surgery.
As medical knowledge continues to expand, the real-world relevance of new discoveries requires constant refocusing. The surgeon-scientist is positioned uniquely to interpret data and pose new questions (22). Among the consistently highest-ranking surgical departments in grants awarded, a 2-to-1 ratio of MD to PhD principal investigators was evident in both 2003 and 2013. This ratio may be a target worth considering for surgery departments that desire to grow their research endeavors. Former NIH director James Wyngaarden noted in 1979 a precipitous decrease in MDs engaged in postdoctoral training supported by the NIH. The same trend was reflected in funding directed toward junior clinical faculty (23). Even as the NIH expanded in the 1980s and 1990s, the proportion of research grants awarded to MDs continued to decrease as did the number of first-time MD applicants (22). While the success rate of NIH applications by MDs during the 1970s–1990s was comparable to that for PhDs, more recent work has shown that applications from surgeons have had less success rates and funding costs than medical and PhD counterparts (12).
Surgeon-scientists face certain disadvantages compared to non-surgeon counterparts. The ratio of NIH study section members to grant submissions is less for surgery than for other specialties, thereby decreasing the rate of truee peer-review (13). This decrease may hinder the success of funding for surgeons, particularly for patient-oriented research (24). Because the salary packages for surgeons are typically reliant on operative volume, there also exists a heavier opportunity cost for time dedicated to grant writing (25). This factor is more relevant now than ever, as decreases in procedural reimbursements have lead surgeons to strive for greater clinical productivity (11), and resident work-hour restrictions have shifted more clinical responsibilities to faculty (14). Because the strongest predictor of a successful NIH proposal is previous NIH funding (26), the above factors should disproportionately hinder first-time applicants and junior surgeons. Indeed, there has been a steady decrease in first-time applicants, fellowship awards, and KO8 awards between the 1980’s and 2011 (27).
Our results indicate that today’s young surgeon-scientists are thriving in the face of these challenges. Despite a lesser average amount of funding-per-investigator than senior faculty, the total funding amount contributed by junior surgeons has nearly doubled between 2003 and 2013. Importantly, the increase in funded junior surgeons is not limited to K-awards alone. In fact, the number of junior surgeons with R-awards has nearly tripled. More than half of all MDs funded in 2013 who were not funded previously in 2003 were assistant or associate professors. Moving forward, senior surgical faculty should continue to nurture this evolution. This is exemplified by our finding that among the 20 institutions with the most NIH grants in 2013, nearly half were led by departmental chairs who were themselves funded through the NIH.
Policy changes within the NIH in 2007 have increased the success rate of applications for first-time applicants (28). Efforts must be made to bolster every phase of the research pipeline to take full advantage of this opportunity. Identification of future surgeon-scientists should begin with students and residents. Opportunities for masters or PhD degrees should be offered to aspiring scientists. One of the strongest predictors of academic productivity among faculty is the number of publications generated during residency (29, 30). With the aim of augmenting publication throughput, didactics addressing basic statistics, experimental design, epidemiology, and grantsmanship are as integral to the education of junior residents as pathophysiology. For junior faculty enrolled on research tenure tracks, courses should be offered that focus on essential research skills, such as time allocation, collaboration, grant-writing, and budget management. Because attainment of a K-award doubles effectively the likelihood for future R01 funding (31), a team of mentors should be assigned to each new investigator to proctor the process of first obtaining a K08, K23, or equivalent training award. Efforts to lobby the NIH to alter K-award requirements such that their requisite time commitments can be decreased in exchange for an extended duration of the award and a lesser annual cost. Most important, departmental policies regarding protected time and resources for research must reflect the academic mission of the institution.
This study has several limitations. Only data from the fiscal years of 2003 and 2013 were accrued. Assessing data from each year spanning this period would create a more rigorous depiction of trends; however, such a task would require the review of more than 5000 grant summaries. Accruing data only from these two fiscal years also avoids confounders from the American Recovery and Reinvestment Act, which was responsible for an aberrant influx of NIH funding in 2009. Because the roster of principal investigators from 2003 and 2013 were not mutually independent, statistical comparisons could not be made between these two years. To address this, we provided details on previously unfunded investigators in order to generate indirect insight into the directionality of change among research personnel. Further, because only the principal investigator for each grant was accounted for within our dataset (no co-principal investigators or co-investigators), our outcomes may underestimate the full breadth of research involvement among surgical faculty in the United States. This underestimate may be particularly true for junior faculty who are more likely to be involved as coinvestigators during the early stages of their research careers.
There is no doubt that PhD investigators comprise a vital component of the surgery research engine. Within core surgical disciplines, however, surgeon-scientists continue to comprise the majority of NIH-funded investigators in departments of surgery. The most consistently successful research departments maintain a stable faction of NIH-funded, clinically-active surgeons. Conversely, departments that fail to accomplish this faction of surgeon-scientists are liable to descend from the elite tier. Encouragingly, the proportion of these surgeon-scientists that are junior faculty is expanding, foretelling hopefully a durable future for surgical research. In an era of continued NIH budgetary stagnation, national and institutional policies aimed at nurturing new researchers will be valuable to preserve this momentum.
Acknowledgments
Funding: Funding support is provided by National Institutes of Health (NIH) T32 CA163177 (to YH and BE). All other authors report no conflicts of interest.
ABBREVIATIONS
- NIH
National Institutes of Health
Footnotes
Presentation: This manuscript was presented at the 2016 Academic Surgical Congress in Jacksonville, Florida on 2.3.16 as an 8-minute oral presentation. Title: “Surgical Investigators Funded through the National Institutes of Health: Then and Now.”
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Groth CG, Brent LB, Calne RY, et al. Historic landmarks in clinical transplantation: Conclusions from the consensus conference at the university of california, los angeles. World J Surg. 2000;24:834–843. doi: 10.1007/s002680010134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Whipple AO. Pancreaticoduodenectomy for islet carcinoma : A five-year follow-up. Ann Surg. 1945;121:847–852. doi: 10.1097/00000658-194506000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hill GJ., 2nd Historic milestones in cancer surgery. Semin Oncol. 1979;6:409–427. [PubMed] [Google Scholar]
- 4.SABISTON DC, Jr, BLALOCK A. Physiologic and anatomic determinants of coronary blood flow and their relationship of myocardial revascularization. Surgery. 1958;44:406–423. [PubMed] [Google Scholar]
- 5.Colaco M, Svider PF, Mauro KM, et al. Is there a relationship between national institutes of health funding and research impact on academic urology? J Urol. 2013;190:999–1003. doi: 10.1016/j.juro.2013.02.3186. [DOI] [PubMed] [Google Scholar]
- 6.Sanfey H, Gantt NL. Career development resource: Academic career in surgical education. Am J Surg. 2012;204:126–129. doi: 10.1016/j.amjsurg.2012.04.001. [DOI] [PubMed] [Google Scholar]
- 7.Souba WW, Tanabe KK, Gadd MA, et al. Attitudes and opinions toward surgical research. A survey of surgical residents and their chairpersons. Ann Surg. 1996;223:377–383. doi: 10.1097/00000658-199604000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kotchen TA, Lindquist T, Malik K, Ehrenfeld E. NIH peer review of grant applications for clinical research. JAMA. 2004;291:836–843. doi: 10.1001/jama.291.7.836. [DOI] [PubMed] [Google Scholar]
- 9.FASEB. Federal funding for biomedical and related life sciences research: FY 2015. 2014. [Google Scholar]
- 10.LaBeaud AD, McKeating H. The largest drought in american history: Funding for science is drying up. PLoS Negl Trop Dis. 2013;7:e2351. doi: 10.1371/journal.pntd.0002351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Debas HT. Impact of the health care crisis on surgery: Perspective of the dean. Arch Surg. 2001;136:158–160. doi: 10.1001/archsurg.136.2.158. [DOI] [PubMed] [Google Scholar]
- 12.Mann M, Tendulkar A, Birger N, et al. National institutes of health funding for surgical research. Ann Surg. 2008;247:217–221. doi: 10.1097/SLA.0b013e3181568e26. [DOI] [PubMed] [Google Scholar]
- 13.Rangel SJ, Efron B, Moss RL. Recent trends in national institutes of health funding of surgical research. Ann Surg. 2002;236:277–86. doi: 10.1097/00000658-200209000-00004. discussion 286–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Winslow ER, Bowman MC, Klingensmith ME. Surgeon workhours in the era of limited resident workhours. J Am Coll Surg. 2004;198:111–117. doi: 10.1016/j.jamcollsurg.2003.08.019. [DOI] [PubMed] [Google Scholar]
- 15.Fang D, Meyer RE. PhD faculty in clinical departments of U.S. medical schools, 1981–1999: Their widening presence and roles in research. Acad Med. 2003;78:167–176. doi: 10.1097/00001888-200302000-00011. [DOI] [PubMed] [Google Scholar]
- 16.Moses H, 3rd, Matheson DH, Cairns-Smith S, et al. The anatomy of medical research: US and international comparisons. JAMA. 2015;313:174–189. doi: 10.1001/jama.2014.15939. [DOI] [PubMed] [Google Scholar]
- 17.Chatterjee SK, Rohrbaugh ML. NIH inventions translate into drugs and biologics with high public health impact. Nat Biotechnol. 2014;32:52–58. doi: 10.1038/nbt.2785. [DOI] [PubMed] [Google Scholar]
- 18.Hu Y, Edwards BL, Brooks KD, et al. Recent trends in national institutes of health funding for surgery: 2003 to 2013. Am J Surg. 2015;209:1083–1089. doi: 10.1016/j.amjsurg.2015.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bureau of Labor Statistics. CPI inflation calculator. 2014;2014 [Google Scholar]
- 20.Herman SS, Singer AM. Basic scientists in clinical departments of medical schools. Clin Res. 1986;34:149–158. [PubMed] [Google Scholar]
- 21.Chinoy MR, Moskowitz J, Wilmore DW, Souba WW. Basic science faculty in surgical departments: Advantages, disadvantages and opportunities. J Surg Res. 2005;123:153–157. doi: 10.1016/j.jss.2004.09.010. [DOI] [PubMed] [Google Scholar]
- 22.Rosenberg LE. The physician-scientist: An essential--and fragile--link in the medical research chain. J Clin Invest. 1999;103:1621–1626. doi: 10.1172/JCI7304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wyngaarden JB. The clinical investigator as an endangered species. N Engl J Med. 1979;301:1254–1259. doi: 10.1056/NEJM197912063012303. [DOI] [PubMed] [Google Scholar]
- 24.Williams GH, Wara DW, Carbone P. Funding for patient-oriented research. critical strain on a fundamental linchpin. JAMA. 1997;278:227–231. [PubMed] [Google Scholar]
- 25.Kron IL. Getting funded. J Thorac Cardiovasc Surg. 2000;119:S26–8. doi: 10.1067/mtc.2000.104722. [DOI] [PubMed] [Google Scholar]
- 26.Zemlo TR, Garrison HH, Partridge NC, Ley TJ. The physician-scientist: Career issues and challenges at the year 2000. FASEB J. 2000;14:221–230. doi: 10.1096/fasebj.14.2.221. [DOI] [PubMed] [Google Scholar]
- 27.Garrison HH, Deschamps AM. NIH research funding and early career physician scientists: Continuing challenges in the 21st century. FASEB J. 2014;28:1049–1058. doi: 10.1096/fj.13-241687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.National Institutes of Health. New and early stage investigator policies. 2014;2014 [Google Scholar]
- 29.Lessin MS, Klein MD. Does research during general surgery residency correlate with academic pursuits after pediatric surgery residency? J Pediatr Surg. 1995;30:1310–1313. doi: 10.1016/0022-3468(95)90492-1. [DOI] [PubMed] [Google Scholar]
- 30.Robertson CM, Klingensmith ME, Coopersmith CM. Long-term outcomes of performing a postdoctoral research fellowship during general surgery residency. Ann Surg. 2007;245:516–523. doi: 10.1097/01.sla.0000245468.98852.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Daye D, Patel CB, Ahn J, Nguyen FT. Challenges and opportunities for reinvigorating the physician-scientist pipeline. J Clin Invest. 2015;125:883–887. doi: 10.1172/JCI80933. [DOI] [PMC free article] [PubMed] [Google Scholar]