Abstract
Objective
To determine whether minority race or ethnicity are associated with mortality and mediated by health insurance coverage among older (age ≥65 years) survivors of critical illness.
Design
A retrospective cohort study.
Setting
Two New York City academic medical centers.
Patients
A total of 1,947 consecutive white (1,107), black (361), and Hispanic (479) older adults who had their first medical-ICU admission from 2006 through 2009 and survived to hospital discharge.
Interventions
None.
Measurements and Main Results
We obtained demographic, insurance, and clinical data from electronic health records, determined each patient’s neighborhood-level socioeconomic data from 2010 US Census tract data, and determined death dates using the Social Security Death Index. Subjects had a mean (SD) age of 79 (8.6) years and median (IQR) follow-up time of 1.6 (0.4–3.0) years. Blacks and Hispanics had similar mortality rates compared to whites (adjusted-hazard ratio [HR] 0.92, 95% CI 0.76–1.11 and adjusted-HR 0.92, 95% CI 0.76–1.12, respectively). Compared to those with commercial insurance and Medicare, higher mortality rates were observed for those with Medicare only (adjusted-HR 1.43, 95% CI 1.03–1.98) and Medicaid (adjusted-HR 1.30, 95% CI 1.10–1.52). Medicaid recipients who were the oldest ICU survivors (age >82 years), survivors of mechanical ventilation, and discharged to skilled-care facilities had the highest mortality rates (p-for-interaction 0.08, 0.03, and 0.17, respectively).
Conclusions
Mortality after critical illness among older adults varies by insurance coverage, but not by race or ethnicity. Those with federal or state insurance coverage only had higher mortality rates than those with additional commercial insurance.
Keywords: Critical Illness, aged, health disparities, mortality, insurance, race
INTRODUCTION
The 1.5 million older (age ≥65 years) Americans who survive hospitalization involving intensive care each year have a high mortality rate after hospital discharge (1). Studies have identified pre-hospitalization functional impairment (2, 3), patient characteristics (4, 5), and treatment factors related to intensive care as risk factors for poor outcomes in older ICU survivors (4–6), but none have assessed whether and how race, ethnicity, and insurance coverage, factors that could predispose to health care disparities after hospital discharge, may interact to potentially affect mortality in older survivors of critical illness.
Compared to whites, blacks and Hispanics have a higher crude mortality from several common critical illnesses (e.g. acute lung injury, sepsis, sudden cardiac death (7–9)). However, after adjustment for disease severity, in-hospital mortality rates for these critical illnesses do not appear to vary by race (7, 10, 11). Whether racial and ethnic differences in mortality exist after hospitalization for critical illness remains unknown.
A systematic review of health insurance status and outcomes for patients who are critically ill showed that those without health insurance receive fewer critical care services and experience worse outcomes (12). While older Americans have basic universal health insurance coverage through the federal Medicare program, 65% have additional commercial insurance coverage from a prior or current employer or that is purchased, 15% have only Medicare coverage, and 20% who are classified as low-income individuals (living at <133% of the federal poverty level) receive additional Medicaid insurance coverage that is funded by both federal and state governments (13, 14). Access to care and outcomes for several diseases have been shown to differ by whether or not older patients have additional commercial or Medicaid insurance coverage (15–22). The associations between race/ethnicity, insurance status, and mortality after critical illness in the larger population of older ICU survivors have not been studied.
The goal of this study was to test the hypotheses that black and Hispanic older American ICU survivors would have increased mortality rates when compared to whites, and that variation in insurance coverage would mediate at least some of the association between minority status and mortality within five years after critical illness.
MATERIALS AND METHODS
Study Design and Patients
We conducted a retrospective cohort study of consecutive adults aged ≥65 years who had their first Columbia University Medical Center or Weill-Cornell Medical Center medical-ICU admission of >24 hours duration and who survived to hospital discharge between January 1, 2006 and December 31, 2009. These medical centers are located in New York City, New York, USA. A prior study describing this cohort has been published (5). We excluded patients who were discharged to hospice or other short-term acute care hospitals, who did not have a social security number, and for whom we could not obtain neighborhood level estimates of socioeconomic status (see Supplement Figure 1). We excluded those with unknown or other races in the primary analysis because our hypothesis involved only blacks, Hispanics, and whites.
Variables
The primary exposure variables were race, ethnicity, and type of health insurance coverage. Race and ethnicity were assigned based on the race/ethnicity in the demographic administrative record, an approach shown to be accurate (23). Since Hispanic ethnicity was not separately assessed from race we categorized race/ethnicity as black, Hispanic, white, other, or unknown. Insurance coverage was assessed from the payer fields in the administrative record, and categorized into commercial insurance and Medicare (i.e., commercial insurance), Medicare only (i.e., Medicare only), and Medicaid with or without Medicare (i.e., Medicaid) (see Supplement Methods for details).
The primary outcome was the mortality rate after critical illness. The date of death was determined from the social security death index, which was queried on August 16, 2011. Follow-up time was calculated as the number of days between the date of hospital discharge and the date of death for decedents. Follow-up time was right censored on January 1, 2011 for non-decedents. Accordingly, follow-up time was at most 5 years for a non-decendent discharged at the beginning of the study period. Secondary outcomes were the 1-year mortality rate (with censored observations at 365 days), and the mortality rate conditional on 1-year survival.
Covariates included all of the independent variables used in a 6-month mortality prediction model that was previously derived and validated using this cohort (5). The Supplement Methods contains a detailed description of how these variables were extracted from medical records and operationalized, and the specific variables are listed in the footnotes to Tables 2 and 3. We linked subjects’ home addresses to their corresponding 2010 US Census tract to ascertain neighborhood-level socioeconomic variables (see Supplement Methods for details).
Table 2.
Associations between race and mortality among older ICU survivors
| Race/Ethnicity | White | Black | Hispanic |
|---|---|---|---|
| Overall Mortality | |||
|
| |||
| Number of patients | 1,107 | 361 | 470 |
| Median follow-up time, years (IQR) | 1.4 (0.34–2.8) | 1.6 (0.28–3.0) | 1.8 (0.55–3.3) |
| Number of decedents | 581 | 184 | 227 |
| Person-Years | 1931 | 637 | 956 |
| Mortality rate, per 100 person-years (95% CI) | 30.1 (27.7–32.6) | 28.7 (25.0–33.4) | 23.7 (20.8–27.0) |
| Unadjusted | 1 | 0.98 (0.83–1.15) | 0.84 (0.72–0.87) |
| Model 1: HR for death (95% CI) | 1 | 1.04 (0.87–1.24) | 0.92 (0.78–1.09) |
| Model 2: HR for death (95% CI) | 1 | 1.06 (0.89–1.26) | 0.95 (0.81–1.13) |
| Model 3: HR for death (95% CI) | 1 | 0.99 (0.83–1.18) | 1.02 (0.87–1.21) |
| Model 4: HR for death (95% CI) | 1 | 0.98 (0.81–1.19) | 1.02 (0.85–1.22) |
| Model 5: HR for death (95% CI) | 1 | 0.92 (0.76–1.11) | 0.92 (0.76–1.12) |
|
| |||
| Mortality Censored at 1 Year | |||
|
| |||
| Median follow-up time, years (IQR) | 1.0 (0.34–1.0) | 1.0 (0.28–1.0) | 1.0 (0.55–1.0) |
| Number of decedents | 407 | 133 | 157 |
| Person-Years | 816 | 261 | 370 |
| Mortality rate, per 100 person-years (95% CI) | 49.8 (45.2–54.9) | 51.0 (43.0–60.4) | 42.4 (36.3–49.6) |
| Unadjusted | 1 | 1.02 (0.85–1.25) | 0.87 (0.72–1.04) |
| Model 1: HR for death (95% CI) | 1 | 1.10 (0.90–1.36) | 0.95 (0.78–1.16) |
| Model 2: HR for death (95% CI) | 1 | 1.13 (0.92–1.39) | 0.99 (0.81–1.21) |
| Model 3: HR for death (95% CI) | 1 | 1.04 (0.84–1.28) | 1.06 (0.87–1.30) |
| Model 4: HR for death (95% CI) | 1 | 1.04 (0.84–1.30) | 1.07 (0.86–1.32) |
| Model 5: HR for death (95% CI) | 1 | 0.99 (0.79–1.24) | 1.00 (0.79–1.24) |
|
| |||
| Mortality Conditioning on 1-Year Survival | |||
|
| |||
| Number of Patients | 700 | 228 | 322 |
| Median follow-up time, years (IQR) | 1.4 (0.54–2.5) | 1.5 (0.76–2.4) | 1.7 (0.82–2.9) |
| Number of decedents | 174 | 51 | 70 |
| Person-Years | 1115 | 378 | 587 |
| Mortality rate, per 100 person-years (95% CI) | 15.6 (13.5–18.1) | 13.5 (10.3–17.8) | 11.9 (9.4–15.1) |
| Unadjusted | 1 | 0.86 (0.63–1.18) | 0.78 (0.59–1.03) |
| Model 1: HR for death (95% CI) | 1 | 0.90 (0.65–1.25) | 0.86 (0.64–1.17) |
| Model 2: HR for death (95% CI) | 1 | 0.91 (0.66–1.28) | 0.87 (0.64–1.19) |
| Model 3: HR for death (95% CI) | 1 | 0.87 (0.62–1.21) | 0.93 (0.68–1.28) |
| Model 4: HR for death (95% CI) | 1 | 0.85 (0.60–1.22) | 0.92 (0.66–1.28) |
| Model 5: HR for death (95% CI) | 1 | 0.77 (0.54–1.11) | 0.78 (0.55–1.11) |
IQR: Interquartile range; HR: Hazard Ratio; 95% CI: 95% Confidence Interval
Model 1: age, gender, discharge year, strata for hospital.
Model 2: Model 1 + primary discharge diagnosis of sepsis, acute stroke, hematologic malignancy, solid malignancy, mechanical ventilation use and duration, hospital length of stay.
Model 3: Model 2 + Charlson comorbidity index score, Do-Not-Resuscitate order, additional strata for admission from or discharge to skilled-care facility.
Model 4: Model 3 + neighborhood median household income.
Model 5: Model 4 + type of insurance coverage.
Table 3.
Associations between type of insurance coverage and mortality among older ICU survivors
| Insurance | Commercial & Medicare | Medicare Only | Medicaid |
|---|---|---|---|
| Overall Mortality | |||
|
| |||
| Number of patients | 1,046 | 79 | 822 |
| Median follow-up time, years (IQR) | 1.6 (0.50–3.1) | 1.5 (0.13–2.5) | 1.5 (0.27–2.8) |
| Number of decedents | 493 | 44 | 455 |
| Person-Years | 1973 | 129 | 1423 |
| Mortality rate, per 100 person-years (95% CI) | 25.0 (22.9–27.3) | 34.0 (25.3–45.7) | 32.0 (29.2–35.0) |
| Unadjusted | 1 | 1.35 (0.99–1.84) | 1.26 (1.11–1.43) |
| Model 1: HR for death (95% CI) | 1 | 1.56 (1.13–2.15) | 1.51 (1.29–1.75) |
| Model 5: HR for death (95% CI) | 1 | 1.43 (1.03–1.98) | 1.30 (1.11–1.52) |
|
| |||
| Mortality Censored at 1 Year | |||
|
| |||
| Median follow-up time, years (IQR) | 1.0 (0.51–1.0) | 1.0 (0.13–1.0) | 1.0 (0.27–1.0) |
| Number of decedents | 344 | 35 | 318 |
| Person-Years | 809 | 53 | 586 |
| Mortality rate, per 100 person-years (95% CI) | 42.5 (38.3–47.3) | 66.4 (47.7–92.5) | 54.3 (48.6–60.6) |
| Unadjusted | 1 | 1.53 (1.09–2.18) | 1.26 (1.08–1.46) |
| Model 1: HR for death (95% CI) | 1 | 1.73 (1.21–2.50) | 1.46 (1.21–1.75) |
| Model 5: HR for death (95% CI) | 1 | 1.47 (1.02–2.12) | 1.21 (1.00–1.46) |
|
| |||
| Mortality Conditioning on 1-Year Survival | |||
|
| |||
| Number of patients | 702 | 44 | 504 |
| Median follow-up time, years (IQR) | 1.5 (0.59–2.7) | 1.5 (0.82–2.7) | 1.4 (0.67–2.6) |
| Number of decedents | 149 | 9 | 137 |
| Person-Years | 1165 | 77 | 836 |
| Mortality rate, per 100 person-years (95% CI) | 12.8 (10.9–15.1) | 11.7 (6.1–22.5) | 16.4 (13.9–19.4) |
| Unadjusted | 1 | 0.91 (0.46–1.78) | 1.28 (1.01–1.61) |
| Model 1: HR for death (95% CI) | 1 | 1.14 (0.57–2.27) | 1.63 (1.23–2.16) |
| Model 5: HR for death (95% CI) | 1 | 1.23 (0.61–2.48) | 1.53 (1.14–2.04) |
IQR: Interquartile range; HR: Hazard Ratio; 95% CI: 95% Confidence Interval
Model 2 variables: age, gender, discharge year, strata for hospital.
Model 5 variables: age, gender, race/ethnicity, discharge year, primary discharge diagnosis of sepsis, acute stroke, hematologic malignancy, or solid malignancy, mechanical ventilation use and duration, hospital length of stay, Charlson comorbidity index, Do-Not-Resuscitate order, neighborhood median household income, with strata for site of hospitalization, admission from a skilled-care facility, and discharge to a skilled-care facility.
Statistical Analyses
Baseline characteristics are expressed as mean ± standard deviation (SD) or median and interquartile range (IQR). We estimated hazard ratios for death using stratified Cox proportional Hazards with strata for center. We ultimately included additional strata for admission from a skilled-care facility and discharge to a skilled-care facility in order to satisfy the assumption of proportional hazards, which were examined by regressing Schoenfeld residuals against time.
We evaluated continuous covariates for nonlinear associations with mortality after hospital discharge using generalized additive models with Lowess smoothing functions. Only hospital length of stay had a nonlinear association with mortality, and was changed to a categorical variable to accommodate the nonlinear trend. We used only neighborhood median household income as an estimate of socioeconomic status due to multi-collinearity with other socioeconomic variables, and for other reasons described in the Supplement Methods.
We first estimated the unadjusted association between race and the rate of mortality after critical illness. We then sequentially adjusted for demographics, measures of the severity of critical illness, measures of chronic health, neighborhood median household income, and type of insurance coverage. We assessed whether an association between race/ethnicity and mortality rate differed by type of insurance coverage, and by neighborhood median annual household income by sequentially evaluating interaction terms. The presence of interaction was assessed using the likelihood ratio test, and a p-for-interaction of <0.20 was considered significant to ensure that clinically significant interactions were not overlooked.
Our primary analysis revealed that type of insurance coverage was associated with mortality after critical illness, but that race/ethnicity was not. We therefore assessed the associations between type of insurance coverage and mortality stratified on the subgroups of race, tertiles of neighborhood median income, tertiles of age, admission source, discharge location, use of mechanical ventilation, and center. We report the individual subgroup strata effect estimates and p-for-interaction for each subgroup. We performed an available case sensitivity analysis categorizing race as black, Hispanic, white, other, and unknown. Analyses were performed using Stata 14.0 (College Station, TX). A p <0.05 was considered significant. The Columbia University Medical Center and Weill Cornell Medical Center Institutional Review Boards approved the study with a waiver of informed consent.
RESULTS
Participants
The study sample for the primary analysis included 1,107 white (57%), 361 black (19%), and 479 Hispanic (25%) older ICU survivors. These 1,947 older ICU survivors had a mean (SD) age of 79 (8.6) years, median (IQR) follow-up time of 1.6 (0.4–3.0) years, and a 48% 1-year mortality. The study sample for the available case sensitivity analysis that included those with other and unknown races had 2,398 subjects (see Supplement Figure 1).
Race and Outcomes
Compared to whites, blacks and Hispanics were younger and more often female. Blacks and Hispanics had a longer duration of mechanical ventilation, and higher proportion with a hospital length of stay >7 days (Table 1). Blacks were more often discharged to skilled-care facilities (62%) compared to whites (55%) and Hispanics (46%). Seventy-five percent of whites had commercial insurance, whereas 75% of Hispanics and 60% of Blacks had Medicaid. Neighborhood median annual household income for blacks, Hispanics, and whites were $35,200, $35,200, and $81,700, respectively.
Table 1.
Patient characteristics by insurance coverage
| Characteristic | Commercial Insurance & Medicare | Medicare only | Medicaid | p-value |
|---|---|---|---|---|
| n (%) | 1046 (54) | 79 (4) | 822 (42) | |
|
| ||||
| Demographics | ||||
|
| ||||
| Age in years, mean (SD) | 78.3 (8.5) | 78.3 (8.4) | 79.0 (8.6) | 0.122 |
| Male, n (%) | 543 (52) | 40 (51) | 321 (39) | < 0.001 |
| Race, n (%) | < 0.001 | |||
| White | 828 (79) | 35 (44) | 244 (30) | |
| Black | 119 (11) | 25 (32) | 217 (27) | |
| Hispanic | 99 (9.5) | 19 (24) | 361 (44) | |
| Year Discharged, n (%) | 0.022 | |||
| 2006 | 215 (21) | 19 (24) | 195 (24) | |
| 2007 | 264 (25) | 20 (25) | 217 (26) | |
| 2008 | 256 (25) | 21 (27) | 228 (28) | |
| 2009 | 311 (30) | 19 (24) | 182 (22) | |
|
| ||||
| Measures of Acute Critical Illness Severity | ||||
|
| ||||
| Primary Diagnosis | ||||
| Sepsis, n (%) | 205 (20) | 17 (22) | 189 (23) | 0.223 |
| Acute stroke, n (%) | 16 (1.5) | 1 (1.3) | 10 (1.2) | 0.838 |
| Hematologic Malignancy, n (%) | 26 (2.5) | 1 (1.3) | 6 (0.73) | 0.013 |
| Solid Malignancy, n (%) | 61 (5.8) | 2 (2.5) | 32 (3.9) | 0.091 |
| Type and Duration of Mechanical Ventilation, n (%) | < 0.001 | |||
| None | 714 (68) | 46 (58) | 479 (58) | |
| < 96 hours | 170 (16) | 11 (14) | 139 (17) | |
| >= 96 hours | 117 (11) | 17 (22) | 128 (16) | |
| >= 96 hours + tracheostomy | 45 (4.3) | 5 (6.3) | 77 (9.3) | |
| Hospital Length of Stay, n (%) | 0.002 | |||
| 1–7 days | 285 (27) | 14 (18) | 174 (21) | |
| 8–21 days | 480 (46) | 41 (52) | 448 (55) | |
| >21 days | 281 (27) | 24 (30) | 200 (24) | |
|
| ||||
| Measures of Chronic Health Severity | ||||
|
| ||||
| Charlson Index Score, median (IQR) | 2 (1–4) | 1 (1–3) | 2 (1–4) | 0.02 |
| Do-Not-Resuscitate order during hospitalization, n (%) | 158 (15) | 21 (27) | 196 (24) | < 0.001 |
| Admission Source, n (%) | < 0.001 | |||
| Home | 971 (93) | 64 (81) | 657 (80) | |
| Skilled-care facility | 75 (7) | 15 (19) | 165 (20) | |
| Discharge location, n (%) | < 0.001 | |||
| Home | 552 (53) | 28 (35) | 320 (39) | |
| Skilled-care facility | 494 (47) | 51 (65) | 502 (61) | |
|
| ||||
| Neighborhood socioeconomic characteristics | ||||
|
| ||||
| Median household income, USD thousands, median (IQR) | 79.5 (44.7–100.6) | 45.0 (34.7–80.7) | 37.3 (27.3–74.5) | < 0.001 |
| Families below poverty line, % | 3.5 (1.1–15) | 9.2 (1.7–24) | 19 (3.1–32) | < 0.001 |
| High school graduates, %, median (IQR) | 92 (79–100) | 82 (66–92) | 72 (60–91) | < 0.001 |
| College graduates, %, median (IQR) | 56 (29–77) | 32 (20–61) | 25 (17–59) | < 0.001 |
SD: Standard Deviation; IQR: Interquartile range
Compared to whites, blacks had a similar unadjusted mortality rate (HR 0.98, 95% CI 0.83–1.15) and adjusted mortality rate after all the covariates were included in the model (Model 5 HR 0.92, 95% CI 0.76–1.11). In unadjusted analyses, Hispanics had a 16% lower mortality rate compared to whites (HR 0.84, 95% CI 0.72–0.97), but this association was attenuated after accounting for differences in age (age- and gender-controlled HR from Model 1 HR 1.04, 95% CI 0.8–1.23). The 1-year mortality rate and mortality conditional on 1-year survival did not appear to vary by race (Table 2).
Mediation by Health Insurance
Since there is no observed association between race/ethnicity and mortality in older ICU survivors, there is no evidence that health insurance coverage mediates any such association. Furthermore, the lack of association between race/ethnicity and mortality did not appear to vary by type insurance coverage (p-for-interaction = 0.88) or by neighborhood median annual household income (p-for-interaction = 0.78).
Health Insurance and Outcomes
There were 1,046 (54%) older ICU survivors with commercial insurance and Medicare, 79 (4%) with Medicare only, and 822 (42%) with Medicaid (Table 1). Compared to those with commercial insurance, Medicaid beneficiaries were more often female and black or Hispanic. Those with commercial insurance were more likely to have a primary diagnosis of a hematologic or solid malignancy, but Medicare only and Medicaid beneficiaries were more likely to have a DNR order during their hospitalization. Medicare only and Medicaid beneficiaries more often received mechanical ventilation and were more likely to be discharged to a skilled-care facility compared to those with commercial insurance. The median neighborhood median annual household income for those with commercial insurance ($79,500) was nearly twice that of Medicare only beneficiaries ($45,000) and Medicaid beneficiaries ($37,500).
Compared to those with commercial insurance, those with Medicare only and Medicaid had higher adjusted mortality rates after critical illness (Model 5 HR 1.43, 95% CI 1.03–1.98 and HR 1.30, 1.11–1.52, respectively) (Table 3, Figure 1). For those with Medicare only, the mortality rate was highest when compared to those with commercial insurance during the first year after hospital discharge (1-year mortality rate ratio, Model 5 HR 1.47, 95% CI 1.02–2.12), but not after the first year (mortality rate ratio conditional on 1-year survival, Model 5 HR 1.23, 95% CI 0.61–2.48). In contrast, for those with Medicaid, the mortality rate appeared highest when compared to those with commercial insurance after the first year following discharge (mortality rate ratio conditional on 1-year survival Model 5 HR 1.53, 95% CI 1.14–2.04), but not during the first year (1-year mortality rate ratio Model 5 HR 1.21, 95% CI 1.00–1.46).
Figure 1.
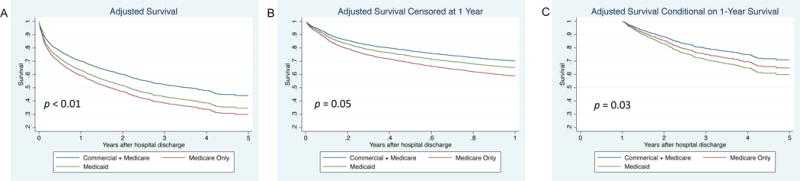
Multivariable-adjusted survival curves of categories of insurance coverage for older ICU survivors. Graphs display 5-year survival (A), survival censored at 1 year (B), and survival conditioning on 1-year survival (C). Survival estimates are derived from Cox models that include covariates of age, gender, race/ethnicity, discharge year, primary discharge diagnosis of sepsis, acute stroke, hematologic malignancy, or solid malignancy, mechanical ventilation use and duration, hospital length of stay, Charlson comorbidity index, Do-Not-Resuscitate order, and neighborhood median household income, and strata for site of hospitalization, admission from a skilled-care facility, and discharge to a skilled-care facility. P-Values are for likelihood ratio tests comparing a full model to one without the categorical variable of insurance coverage.
The associations between Medicaid coverage and mortality appeared to by modified by age and use of mechanical ventilation (p-for-interaction 0.03, 0.08), and weakly modified by discharge to a skilled-care facility (p-for-interaction 0.17) (Figure 2 and Supplement Table 2). There was a stronger association among those in the oldest tertile of subjects (age >82 years) compared to youngest tertile of subjects (age <74 years) (Model 5 HR 1.49, 95 % CI 1.16–1.92 and 1.02, 95% CI 0.73–1.44, respectively). The magnitude of the associations between Medicare only coverage, Medicaid coverage, and mortality were substantially higher among those who received mechanical ventilation (Model 5 HR 2.17, 95% CI 1.35–3.48 and 1.61, 95% CI 1.24–2.10, respectively). Compared to those with commercial insurance who were discharged to skilled-care facilities, Medicaid beneficiaries discharged to skilled-care facilities had a 34% higher mortality rate (Model 5 HR 1.34, 95% CI 1.11–1.62) (Figure 2 and Supplement Table 2). This association was strongest among those who survived at least 1 year (Model 5 HR 1.75, 95% CI 1.20–2.55) (Supplement Table 3).
Figure 2.
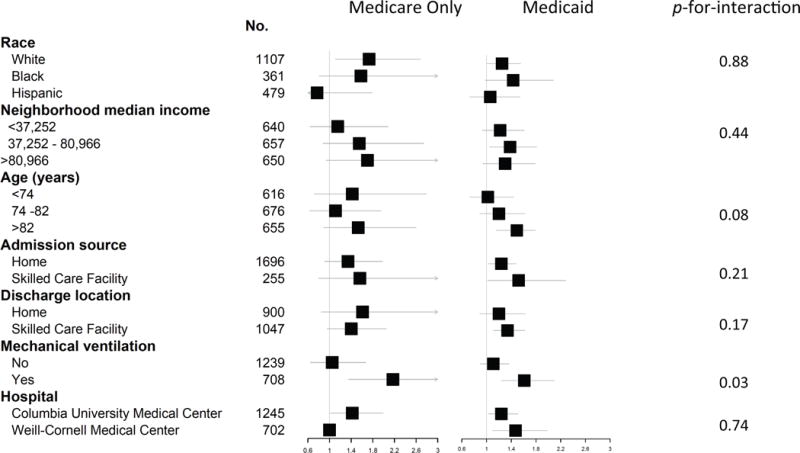
Stratified analyses across race, tertiles of neighborhood median annual income, tertiles of age, admission source, discharge location, any use of mechanical ventilation, and site of hospitalization. Hazards ratios and 95% CI are from Supplement Table 2, are derived from Cox Model 5 that is described in the footnote to Table 3, and represent 5-year adjusted mortality rate ratios.
An available case sensitivity analysis including patients who had an unknown or other race showed a similar lack of association between race/ethnicity and mortality, and similar associations between type of insurance coverage and mortality (Supplement Table 4). Neighborhood annual median household income was not associated with mortality after critical illness (Supplement Table 5).
DISCUSSION
In this racially, ethnically, and socioeconomically diverse cohort of older medical ICU survivors from two tertiary care centers in New York City, we were unable to confirm our hypothesis that black race and Hispanic ethnicity were associated with higher mortality rates after critical illness compared to whites. We instead found that, independent of race and ethnicity, those with federal or state health insurance coverage only had substantially higher mortality rates than those with additional commercial insurance. This disparity was greatest among Medicaid beneficiaries discharged to skilled-care facilities who survived at least 1 year. This is the first study to examine racial and socioeconomic disparities in long-term mortality among older ICU survivors of a broad range of critical illnesses, and the first to show an independent association between federal or state insurance coverage and an increased risk of death. Our findings have important public health implications, and suggest that a suboptimal level of care may be currently provided to older adults who lack commercial health insurance.
There are several possible reasons why we did not find racial or ethnic differences in mortality in our cohort of older ICU survivors. The quality of ICU care patients receive may not vary by race/ethnicity in way that affects post-discharge survival. A recent study found that while blacks and Hispanics present with a higher severity of critical illness, in-hospital mortality does not differ by race/ethnicity after controlling for severity of illness, resuscitation preferences, socioeconomic status, and insurance coverage (11). Similarly, we found that blacks and Hispanics may have been more acutely critically ill at presentation insofar as they used more mechanical ventilation and had a longer ICU length of stay than whites, but long-term mortality did not vary by race/ethnicity. Second, the quality of outpatient care may not vary by race/ethnicity in the elderly. The quality of care for elderly Medicare beneficiaries in managed-care plans has improved over time, and racial disparities for beneficiaries of these plans have declined substantially for several measures of quality in cancer screening, diabetes care, and prescription of cardiovascular drugs (24). While never studied specifically in older adults, the increasing use of Medicaid managed care plans for adults <65 years of age has been shown to reduce or eliminate racial/ethnic disparities in younger Medicaid beneficiaries’ access to care (25, 26).
Our finding that older ICU survivors with Medicaid or Medicare only have higher mortality rates than those with commercial insurance and Medicare may have a number of explanations. Older adults who are eligible for Medicaid are significantly poorer, less educated, and have lower levels of social support compared to those with Medicare only or Medicare and commercial insurance (27). Medicaid beneficiaries may therefore experience barriers to coordinating medical care. Compared to older Medicare beneficiaries with or without commercial insurance, older Medicaid beneficiaries also receive lower-quality outpatient care and preventative services (28, 29), and experience more adverse events at home due to unmet needs with self-care (30).
Medicaid beneficiaries are more likely to be discharged to post-acute care facilities with lower nurse-to-patient ratios (18), more deficiencies in care (19), lower quality ratings (31), and higher hospital readmission rates (32). This may be due to lower reimbursement rates for skilled-care facilities with a higher share of Medicaid patients (18, 19, 33). We found that among older ICU survivors discharged to skilled-care facilities, those with Medicaid had a 34% increased risk of death over 5-years and 75% increased risk of death among those who survived at least 1 year, compared to those with Medicare and commercial insurance. To our knowledge, our study is the first to show an independent association between Medicaid insurance coverage and mortality for older survivors of critical illness who are discharged to skilled-care facilities, and the only study to find such a large magnitude of risk of death based on insurance coverage.
Approximately 15% of Medicare Beneficiaries have no Medicaid or commercial insurance (14). Medicare D does not cover significant portions of prescription drug costs and Medicare A covers only the first 100 days of post-acute skilled care after a 3-day hospital admission (34, 35). Medicare beneficiaries without extra insurance may be unable to afford prescription drugs or skilled-facility care beyond 100 days, which may explain why the risk of death appears highest in the first year after hospitalization for this group in our study. Since only 79 subjects (4%) in our study had Medicare coverage without extra insurance, these results should be considered only preliminary and hypothesis generating.
Our study has several limitations. Socioeconomic predictors were measured at the neighborhood level, not the individual level. Since many Medicaid recipients live in poverty, some of the observed associations between Medicaid insurance and mortality may be confounded by an inability to pay for a healthy diet, adequate housing, or specialized home care, all of which may adversely affect survival. We could not determine race/ethnicity for 19% of subjects. However, a sensitivity analysis including those with other and unknown race categories yielded results similar to those from our primary analyses. We do not know how many decedents died while still receiving skilled-care or who were discharged from skilled care to home and then died. We did not assess re-hospitalizations because subjects may be readmitted to other New York City hospitals (29), and we do not have access to these data. We did not separately analyze those discharged to long-term acute care facilities (LTACs) because there were only 21 of these subjects. We attempted to control for end-of-life care preferences based on a DNR order during the hospitalization and excluded those who were discharged to hospice. However, we do not know how or whether enrollment in hospice after hospital discharge may have affected our results. Although we adjusted for covariates that reflect patient demographics, measures of the severity of critical illness, measures of chronic health, and group-level covariates, residual or unmeasured confounding may be present. Future studies of larger cohorts of older adults from different geographic regions are needed to validate our results.
CONCLUSIONS
We found no evidence that race or ethnicity influences survival time among older survivors of critical illness. In contrast, commercial health insurance may have a protective role, perhaps by increasing access to higher quality healthcare services. Our finding builds on a body of research that has demonstrated deficiencies in outpatient and skilled-facility care among older Americans with Medicaid insurance to reveal that these disparities may be associated with a substantial increased risk of death among older ICU survivors. Our findings should prompt future investigations into the factors that mediate the higher mortality rates among older ICU survivors who lack commercial health insurance coverage, ranging from measurement of the barriers to preventative and emergency care that might prevent the onset of critical illness, to the barriers to high-quality post-hospitalization outpatient care delivery, to the barriers to high-quality post-acute facility care delivery.
Supplementary Material
Acknowledgments
Financial support for the study: Funding/Support: This study was supported by UL1 TR000040, KL2 TR000081 (MRB), and K23 AG045560 (MRB), Columbia University Aging Center Faculty Research Fellowships (MRB and GSL), R25 HL096250 (NH and AJ), and K24 HL131937 (DJL).
Footnotes
Copyright form disclosure: Drs. Baldwin, Maurer, Lovasi, and Lederer received support for article research from the National Institutes of Health. Dr. Lederer received funding from Genentech/Roche, Degge group, France Foundation, XVIVO Therapeutics, and Veracyte. His institution received funding from Pulmonary Fibrosis Foundation. Dr. Lederer also received funding from Boehringer-Ingelheim, Gilead, and Pharmakea. The remaining authors have disclosed that they do not have any potential conflicts of interest.
Reprints will not be ordered
References
- 1.Wunsch H, Guerra C, Barnato AE, et al. Three-year outcomes for Medicare beneficiaries who survive intensive care. JAMA. 2010;303(9):849–856. doi: 10.1001/jama.2010.216. [DOI] [PubMed] [Google Scholar]
- 2.Ferrante LE, Pisani MA, Murphy TE, et al. Functional trajectories among older persons before and after critical illness. JAMA internal medicine. 2015;175(4):523–529. doi: 10.1001/jamainternmed.2014.7889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ferrante LE, Pisani MA, Murphy TE, et al. Factors Associated with Functional Recovery Among Older ICU Survivors. American journal of respiratory and critical care medicine. 2016 doi: 10.1164/rccm.201506-1256OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ho KM, Knuiman M, Finn J, et al. Estimating long-term survival of critically ill patients: the PREDICT model. PLoS One. 2008;3(9):e3226. doi: 10.1371/journal.pone.0003226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Baldwin MR, Narain WR, Wunsch H, et al. A prognostic model for 6-month mortality in elderly survivors of critical illness. Chest. 2013;143(4):910–919. doi: 10.1378/chest.12-1668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Barnato AE, Albert SM, Angus DC, et al. Disability among elderly survivors of mechanical ventilation. Am J Respir Crit Care Med. 2011;183(8):1037–1042. doi: 10.1164/rccm.201002-0301OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Erickson SE, Shlipak MG, Martin GS, et al. Racial and ethnic disparities in mortality from acute lung injury. Critical care medicine. 2009;37(1):1–6. doi: 10.1097/CCM.0b013e31819292ea. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Martin GS, Mannino DM, Eaton S, et al. The epidemiology of sepsis in the United States from 1979 through 2000. The New England journal of medicine. 2003;348(16):1546–1554. doi: 10.1056/NEJMoa022139. [DOI] [PubMed] [Google Scholar]
- 9.Galea S, Blaney S, Nandi A, et al. Explaining racial disparities in incidence of and survival from out-of-hospital cardiac arrest. American journal of epidemiology. 2007;166(5):534–543. doi: 10.1093/aje/kwm102. [DOI] [PubMed] [Google Scholar]
- 10.Dombrovskiy VY, Martin AA, Sunderram J, et al. Occurrence and outcomes of sepsis: influence of race. Critical care medicine. 2007;35(3):763–768. doi: 10.1097/01.CCM.0000256726.80998.BF. [DOI] [PubMed] [Google Scholar]
- 11.Erickson SE, Vasilevskis EE, Kuzniewicz MW, et al. The effect of race and ethnicity on outcomes among patients in the intensive care unit: a comprehensive study involving socioeconomic status and resuscitation preferences. Critical care medicine. 2011;39(3):429–435. doi: 10.1097/CCM.0b013e318206b3af. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fowler RA, Noyahr LA, Thornton JD, et al. An official American Thoracic Society systematic review: the association between health insurance status and access, care delivery, and outcomes for patients who are critically ill. American journal of respiratory and critical care medicine. 2010;181(9):1003–1011. doi: 10.1164/rccm.200902-0281ST. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.The Henry J. Kaiser Family Foundation. Dual Eligibles: Medicaid’s Role for Low-Income Medicare Beneficiaries. 2009 Available at: https://kaiserfamilyfoundation.files.wordpress.com/2013/01/8138-02.pdf. Accessed: September 7, 2016.
- 14.Centers for Medicare and Medicaid. Medicare Current Beneficiary Survey. 2011 Available at: https://www.cms.gov/Research-Statistics-Data-and-Systems/Research/MCBS/index.html?redirect=/MCBS. Accessed: March 24, 2016.
- 15.Hebb JH, Fitzgerald D, Fan W. Health care disparities in disadvantaged Medicare beneficiaries: a national project review. Journal of health and human services administration. 2003;26(2):153–173. [PubMed] [Google Scholar]
- 16.Parikh RR, Grossbard ML, Green BL, et al. Disparities in survival by insurance status in patients with Hodgkin lymphoma. Cancer. 2015;121(19):3515–3524. doi: 10.1002/cncr.29518. [DOI] [PubMed] [Google Scholar]
- 17.Slatore CG, Au DH, Gould MK. An official American Thoracic Society systematic review: insurance status and disparities in lung cancer practices and outcomes. American journal of respiratory and critical care medicine. 2010;182(9):1195–1205. doi: 10.1164/rccm.2009-038ST. [DOI] [PubMed] [Google Scholar]
- 18.Rahman M, Grabowski DC, Gozalo PL, et al. Are dual eligibles admitted to poorer quality skilled nursing facilities? Health Serv Res. 2014;49(3):798–817. doi: 10.1111/1475-6773.12142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Li Y, Harrington C, Temkin-Greener H, et al. Deficiencies In Care At Nursing Homes And Racial/Ethnic Disparities Across Homes Fell, 2006–11. Health Aff (Millwood) 2015;34(7):1139–1146. doi: 10.1377/hlthaff.2015.0094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mor V, Zinn J, Angelelli J, et al. Driven to tiers: socioeconomic and racial disparities in the quality of nursing home care. The Milbank quarterly. 2004;82(2):227–256. doi: 10.1111/j.0887-378X.2004.00309.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Smith DB, Feng Z, Fennell ML, et al. Separate and unequal: racial segregation and disparities in quality across U.S. nursing homes. Health Aff (Millwood) 2007;26(5):1448–1458. doi: 10.1377/hlthaff.26.5.1448. [DOI] [PubMed] [Google Scholar]
- 22.Li Y, Yin J, Cai X, et al. Association of race and sites of care with pressure ulcers in high-risk nursing home residents. JAMA. 2011;306(2):179–186. doi: 10.1001/jama.2011.942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Blustein J. The reliability of racial classifications in hospital discharge abstract data. American journal of public health. 1994;84(6):1018–1021. doi: 10.2105/ajph.84.6.1018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Trivedi AN, Zaslavsky AM, Schneider EC, et al. Trends in the quality of care and racial disparities in Medicare managed care. The New England journal of medicine. 2005;353(7):692–700. doi: 10.1056/NEJMsa051207. [DOI] [PubMed] [Google Scholar]
- 25.Cook BL. Effect of Medicaid Managed Care on racial disparities in health care access. Health Serv Res. 2007;42(1 Pt 1):124–145. doi: 10.1111/j.1475-6773.2006.00611.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Seligman HK, Chattopadhyay A, Vittinghoff E, et al. Racial and ethnic differences in receipt of primary care services between medicaid fee-for-service and managed care plans. The Journal of ambulatory care management. 2007;30(3):264–273. doi: 10.1097/01.JAC.0000278986.18428.12. [DOI] [PubMed] [Google Scholar]
- 27.Office CB. Dual-eligible beneficiaries of Medicare and Medicaid: Characteristics, health care spending, and evolving policies. Washington, DC: 2013. [Google Scholar]
- 28.Landon BE, Schneider EC, Normand SL, et al. Quality of care in Medicaid managed care and commercial health plans. Jama. 2007;298(14):1674–1681. doi: 10.1001/jama.298.14.1674. [DOI] [PubMed] [Google Scholar]
- 29.Schrag D, Xu F, Hanger M, et al. Fragmentation of care for frequently hospitalized urban residents. Med Care. 2006;44(6):560–567. doi: 10.1097/01.mlr.0000215811.68308.ae. [DOI] [PubMed] [Google Scholar]
- 30.Allen SM, Piette ER, Mor V. The adverse consequences of unmet need among older persons living in the community: dual-eligible versus Medicare-only beneficiaries. The journals of gerontology Series B, Psychological sciences and social sciences. 2014;69(Suppl 1):S51–58. doi: 10.1093/geronb/gbu124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tamara Konetzka R, Grabowski DC, Perraillon MC, et al. Nursing home 5-star rating system exacerbates disparities in quality, by payer source. Health Aff (Millwood) 2015;34(5):819–827. doi: 10.1377/hlthaff.2014.1084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Carter MW, Porell FW. Variations in hospitalization rates among nursing home residents: the role of facility and market attributes. The Gerontologist. 2003;43(2):175–191. doi: 10.1093/geront/43.2.175. [DOI] [PubMed] [Google Scholar]
- 33.Grabowski DC. A longitudinal study of Medicaid payment, private-pay price and nursing home quality. International journal of health care finance and economics. 2004;4(1):5–26. doi: 10.1023/b:ihfe.0000019258.29496.03. [DOI] [PubMed] [Google Scholar]
- 34.Flaer PJ, Younis MZ, Hussain AA, et al. Medicare Part D in 2008: rising prices and growing confusion. Journal of health care finance. 2008;34(4):89–92. [PubMed] [Google Scholar]
- 35.Centers of Medicare and Medicaid. Skilled Nursing Facility (SNF) care. 2016 Available from: https://www.medicare.gov/coverage/skilled-nursing-facility-care.html. Accessed: April 6, 2016.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


