Abstract
AIM
To compare the results of arthroscopic capsular release with intra-articular steroid injections in patients of frozen shoulder.
METHODS
Fifty-six patients with frozen shoulder were randomised to one of two treatment groups: Group 1, complete 360 degree arthroscopic capsular release and group 2, intra-articular corticosteroid injection (40 mg methyl prednisolone acetate). Both groups were put on active and passive range of motion exercises following the intervention. The outcome parameters were visual analogue scale (VAS) score for pain, range of motion and Constant score which were measured at baseline, 4, 8, 12, 16 and 20 wk after intervention.
RESULTS
All the parameters improved in both the groups. The mean VAS score improved significantly more in the group 1 as compared to group 2 at 8 wk. This greater improvement was maintained at 20 wk with P value of 0.007 at 8 wk, 0.006 at 12 wk, 0.006 at 16 wk and 0.019 at 20 wk. The Constant score showed a more significant improvement in group 1 compared to group 2 at 4 wk, which was again maintained at 20 wk with P value of 0.01 at 4, 8, 12 and 16 wk. The gain in abduction movement was statistically significantly more in arthroscopy group with P value of 0.001 at 4, 8, 12, 16 wk and 0.005 at 20 wk. The gain in external rotation was statistically significantly more in arthroscopy group with P value of 0.007 at 4 wk, 0.001 at 8, 12, and 16 wk and 0.003 at 20 wk. There was no statistically significant difference in extension and internal rotation between the two groups at any time.
CONCLUSION
Arthroscopic capsular release provides subjective and objective improvement earlier than intra-articular steroid injection.
Keywords: Adhesive capsulitis, Frozen shoulder, Capsular release, Corticosteroid, Idiopathic stiff shoulder, Intra articular injection, Steroid injection, Arthroscopic arthrolysis, Constant score
Core tip: The treatment of frozen shoulder is selected depending on the preference of the treating physician, since there are no guidelines or protocols. The physicians, physiotherapists, occupational therapists and orthopedicians who are not trained in shoulder arthroscopy often select non-surgical methods. On the other hand, shoulder arthroscopists prefer arthroscopic arthrolysis. We conducted a randomised clinical trial to compare the results of arthroscopic arthrolysis and intra-articular steroid injection in frozen shoulder. Both modalities resulted in significant improvement in pain, range of motion and Constant score. However the improvement in surgery group preceded those in injection group by 4-8 wk.
INTRODUCTION
Frozen shoulder also termed as adhesive capsulitis of shoulder, is a common cause of shoulder pain and global stiffness of the glenohumeral joint. It is estimated to affect 2%-5% of the population[1]. Frozen shoulder has been described as a self-limiting condition, lasting on average 2-3 years[2-4]. Some studies, however, have reported that 20%-50% of the sufferers continue to have pain and restricted movement beyond 3 years[5,6]. Though it is a self-limiting condition, patients find it impractical and difficult to wait for such a long period as it interferes with the activities of daily life.
A variety of treatment strategies for adhesive capsulitis have been developed to alleviate pain and enhance range of motion (ROM) of the shoulder. The commonest modalities to achieve this are physiotherapy[7] and corticosteroid injections[8] either through local injection or systemically. Other options include manipulation under general anaesthesia[9-11], scalene block, arthrographic capsular distension[12-14] and surgical intervention (arthroscopic and open arthrolysis).
Arthroscopic capsular release for the treatment of adhesive capsulitis has gained popularity for its high safety and efficacy reported in literature[15-18]. Our study aims to compare the results of arthroscopic capsular release with those of intra-articular corticosteroid injection[19-21] which seems to be the most commonly prescribed treatment for adhesive capsulitis of shoulder at present, and ascertain whether arthroscopic capsular release can provide a speedier recovery compared to the more commonly prescribed intra-articular steroid injections. Our null hypothesis was that the two modalities would provide equal outcomes.
MATERIALS AND METHODS
Patient selection
The criteria to include patients in this study were idiopathic stiffness of the shoulder with global restriction of shoulder movements for at least six months and normal findings on plain radiograph. Global restrictions would imply decrease in active and passive movements in all directions. Patients with prior history of trauma, surgery or injections to the shoulder were excluded from the study. Patients who had received any form of treatment to the affected shoulder other than physiotherapy were also excluded.
Patients
Sample size was calculated using Master 2.0 software. All the patients were explained about the study in their native language and a written consent was obtained before enrolment in the study. Sixty such patients were randomly allocated to one of the two study groups using computer tables. The patient inclusion and dropouts from the study groups is described in the consort diagram (Figure 1). In group 1, complete 360-degree arthroscopic capsular release of the affected shoulder was performed under general anaesthesia in lateral position in 28 patients. These patients underwent pre-operative magnetic resonance imaging (MRI) examination to rule out any intra-articular pathology. Arthroscopic capsular release involved excising the tissues in the rotator interval up to the coracoids process, division of the superior, middle and inferior glenohumeral ligaments and release of the anterior, posterior, superior and inferior capsule of the shoulder joint. Subacromial bursa was not viewed. In group 2, single dose of 40 mg methylprednisolone acetate along with 3 mL of 2% lignocaine was injected into the affected shoulder without image guidance through the posterior approach in 28 patients. The intervention in the both study groups was followed by active and passive range of motion exercises. Both groups of patients were given a combination of a NSAID with tramadol as analgesics for pain control.
Figure 1.
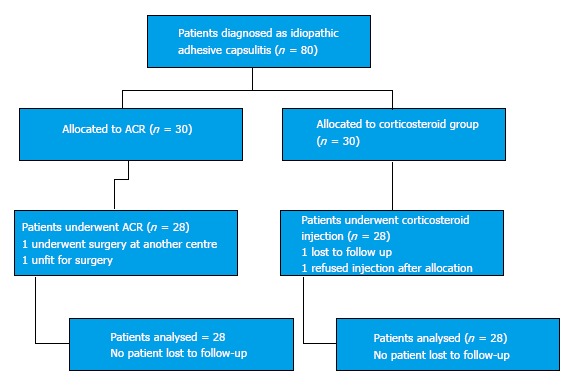
Consort diagram.
Outcome measures
The clinical outcome measures used in the study were: Visual analogue scale (VAS) score for pain (0-10), range of motion and Constant score (0-100). The parameters were initially recorded before the intervention (baseline) and then after the intervention at 4, 8, 12, 16 and 20 wk. The outcome parameters in both the study groups were compared with each other. Any complications encountered in the study were also noted.
Arthroscopic findings
Twenty-seven out of the 28 patients who underwent arthroscopic capsular release showed fibrous contracture of the rotator interval, suggesting that it is the most important pathology associated with the development of adhesive capsulitis. Synovitis was present in all the patients. Twenty-four patients had global synovitis involving the rotator interval, the joint capsule, subscapularis tendon and the rotator cuff and 4 patients had synovitis limited only to the rotator interval. Apart from the above findings, which are suggestive of adhesive capsulitis, 4 patients had partial tear of the rotator cuff on the articular side and 1 patient had a type 2 superior labrum anterior to posterior (SLAP) lesion, which were not diagnosed preoperatively. These lesions were not detected on pre-operative MRI also. The partial cuff tears were debrided and SLAP was left as such. These 4 patients were not excluded from the study because the intra-articular lesions were not symptomatic, but were incidental findings. The arthroscopic group did not experience any post-operative infection or neurovascular damage. There was one case of articular cartilage scuffing of glenoid and one case of the humeral head.
Statistical analysis
Statistical analysis was carried out using SPSS software version 20. Data was presented as number (%) or mean ± SD as appropriate. The baseline characteristics were compared using χ2 test (categorical variables) and Student’s t test (continuous variables). The outcome parameters such as VAS, range of motion and Constant score measures at baseline, 4, 8, 12, 16 and 20 wk were compared between the two groups using Student’s t test. The change in outcome parameters within each group was detected using a general linear model. P value of < 0.05 was considered statistically significant.
RESULTS
Demography
The mean age of the patients included in the study was 50.4 ± 9.0 years (capsular release group, 48.1 ± 9.6 years, and corticosteroid group, 52.6 ± 7.9 years). Out of the 56 patients in the study, 23 patients were male and 33 patients were female with 18 male patients in the capsular release group and 15 male patients in the corticosteroid group. Twenty-four patients had involvement of the dominant side and 32 patients had involvement of the non-dominant (17 patients in the capsular release group involving the non-dominant and 15 patients in the corticosteroid group involving the non-dominant side). The condition most commonly associated with adhesive capsulitis in the study was diabetes mellitus. Sixteen patients out of the 56 patients recruited in the study had diabetes mellitus. The age, sex, shoulder affected and the patients with diabetes mellitus were similarly distributed in the two groups. The average duration of symptoms was 6.3 mo (6.5-9.5 mo).
Clinical parameters
VAS score: The mean VAS score showed significant improvement at 4, 8, 12, 16 and 20 wk in both groups. The improvement in VAS was statistically significant in the capsular release group at 8, 12, 16 and 20 wk as compared to injection group (Table 1).
Table 1.
Changes in visual analogue scale scores in both groups
| Duration |
VAS score in group (mean ± SD) |
P value | |
| ACR | Corticosteroid | ||
| Baseline | 7.1 ± 1.8 | 7.1 ± 1.8 | 1 |
| 4 wk | 4.4 ± 1.6 | 5.1 ± 1.7 | 0.101 |
| 8 wk | 3.6 ± 1.7 | 4.8 ± 1.7 | 0.007 |
| 12 wk | 3.0 ± 1.6 | 4.2 ± 1.6 | 0.006 |
| 16 wk | 2.5 ± 1.8 | 3.7 ± 1.5 | 0.006 |
| 20 wk | 2.0 ± 1.7 | 3.2 ± 1.5 | 0.019 |
VAS: Visual analogue scale.
Range of motion: All the movements measured in the study, i.e., forward flexion, extension, abduction, adduction, external rotation and internal rotation, showed significant improvement in both groups during the follow-up at 4, 8, 12, 16 and 20 wk (Table 2). Forward flexion, abduction and external rotation showed a statistically significant improvement in the capsular release group as compared to that in the injection group and the improvement was maintained till the end of 20 wk.
Table 2.
Change in range motion in both groups
| Movement type | Study group |
Movement in degrees (mean ± SD) |
|||||
| Baseline | 4 wk | 8 wk | 12 wk | 16 wk | 20 wk | ||
| Forward flexion | ACR | 99.8 ± 13.4 | 133.3 ± 19.1 | 140.1 ± 18.6 | 145.5 ± 17.4 | 151.2 ± 16.4 | 152.9 ± 14.6 |
| Corticosteroid | 100.8 ± 16.7 | 118.9 ± 17.4 | 126.4 ± 16.9 | 132.5 ± 17.3 | 138.9 ± 17.6 | 143.9 ± 16.6 | |
| P value | 0.79 | 0.005 | 0.006 | 0.007 | 0.009 | 0.05 | |
| Extension | ACR | 34.1 ± 7.5 | 42.6 ± 8.1 | 45.0 ± 7.6 | 48.0 ± 6.8 | 49.8 ± 7.0 | 50.6 ± 7.2 |
| Corticosteroid | 34.4 ± 7.4 | 41.6 ± 6.3 | 43.7 ± 5.3 | 46.7 ± 6.1 | 49.2 ± 5.5 | 50.0 ± 5.4 | |
| P value | 0.86 | 0.58 | 0.48 | 0.47 | 0.53 | 0.68 | |
| Abduction | ACR | 78.3 ± 13.2 | 113.2 ± 20.4 | 121.6 ± 21.8 | 127.6 ± 21.3 | 131.9 ± 19.8 | 135.6 ± 18.5 |
| Corticosteroid | 78.0 ± 18.8 | 94.6 ± 20.2 | 100.0 ± 22.4 | 107.5 ± 21.2 | 109.2 ± 26.9 | 118.3 ± 22.0 | |
| P value | 0.93 | 0.001 | 0.001 | 0.001 | 0.001 | 0.005 | |
| Adduction | ACR | 28.0 ± 5.6 | 37.3 ± 6.1 | 39.1 ± 5.9 | 41.7 ± 5.1 | 43.9 ± 5.5 | 45.9 ± 5.0 |
| Corticosteroid | 28.7 ± 6.3 | 33.2 ± 5.4 | 35.8 ± 5.9 | 38.2 ± 6.6 | 41.2 ± 5.5 | 43.0 ± 5.8 | |
| P value | 0.65 | 0.01 | 0.04 | 0.02 | 0.07 | 0.07 | |
| Internal rotation | ACR | 28.9 ± 6.4 | 39.8 ± 8.4 | 42.5 ± 8.9 | 44.8 ± 9.1 | 48.3 ± 9.0 | 50.4 ± 7.5 |
| Corticosteroid | 32.6 ± 8.3 | 38.7 ± 6.7 | 41.0 ± 5.6 | 44.2 ± 6.1 | 46.4 ± 4.6 | 47.8 ± 5.5 | |
| P value | 0.06 | 0.6 | 0.47 | 0.79 | 0.31 | 0.16 | |
| External rotation | ACR | 39.1 ± 6.2 | 56.4 ± 11.4 | 61.4 ± 12.9 | 65.7 ± 13.2 | 69.8 ± 12.7 | 73.4 ± 14.2 |
| Corticosteroid | 42.6 ± 8.2 | 49.1 ± 7.7 | 51.4 ± 8.9 | 54.8 ± 8.2 | 59.2 ± 8.8 | 62.6 ± 9.9 | |
| P value | 0.07 | 0.007 | 0.001 | 0.001 | 0.001 | 0.003 | |
Constant score: The Constant score showed significant improvement at each follow-up in both groups. However, improvement was more significant in the surgical release group than in the injection group. No difference was found in the change of clinical parameters between the patients with and without diabetes mellitus in either groups (Table 3).
Table 3.
Changes in Constant score in both groups
| Duration |
Constant score in group (mean ± SD) |
P value | |
| ACR | Corticosteroid | ||
| Baseline | 29.5 ± 6.2 | 30.4 ± 8.3 | 0.64 |
| 4 wk | 50.3 ± 10.7 | 43.4 ± 9.5 | 0.01 |
| 8 wk | 56.0 ± 11.9 | 47.6 ± 10.3 | 0.01 |
| 12 wk | 61.0 ± 12.3 | 53.0 ± 9.9 | 0.01 |
| 16 wk | 66.5 ± 13.0 | 58.4 ± 11.2 | 0.01 |
| 20 wk | 70.2 ± 12.1 | 62.6 ± 11.6 | 0.03 |
DISCUSSION
Despite the wide variety of treatment options available and the amount of research done, the results still appear to be inconclusive about the effectiveness of different interventions for adhesive capsulitis. There is no definitive guideline as to when to change from one treatment modality to another. But it is generally acceptable to wait for 3 mo before declaring any conservative treatment ineffective. Physiotherapy and intra-articular injections of corticosteroids continue to be the commonest mode of treatment for this condition. Injections into shoulder joint is most frequently administered without any image guidance in general practice even though multiple studies have shown that even in expert hands, a large number of injections may be out of the joint. In order to replicate the general practice, no image guidance was performed during the injections in this study. Arthroscopic capsular release has shown to provide early relief of symptoms[22] and is increasingly being performed for the treatment of adhesive capsulitis of shoulder.
Baums et al[17], Smith et al[18] and Le Lievre et al[23] have demonstrated a significant early improvement in pain, range of motion and overall shoulder function following arthroscopic capsular release. In the Indian population, similar results have been shown by Sabat and Kumar[22]. Jerosch et al[24], Warner et al[25], Ogilvie-Harris et al[26] have shown the safety and effectiveness of arthroscopic capsular release for the treatment of adhesive capsulitis of shoulder. However, we could only find one study by De Carli et al[27] which compared arthroscopic capsular release with intra articular corticosteroid injections. The results of our study are in agreement with those by De Carli et al[27] in which arthroscopic capsular release resulted in an early relief of pain and increased shoulder range of motion.
Our study showed continuous improvement in all parameters in both the groups and it stared as early as 4 wk after the intervention. The scores of different parameters in the injection group at 20 wk were achieved 4-8 wk earlier in the surgery group. In contrast to the Constant score which showed significant difference between the two groups as early as 4 wk, the VAS score for pain showed significant difference between the two groups in the 8th week. The initial period of pain following surgery could be the possible reason for this slightly delayed significant improvement in VAS score in the arthroscopic group. Extension and internal rotation of the shoulder were the only two parameters where there was no significant difference between the two groups.
Our study had some notable strengths. These include a strict inclusion and exclusion criteria, random allocation of the patients to both study groups and a frequent follow-up at a 4-wk interval. The limitations of our study included the lack of a control group, a relatively small sample size, short-term follow-up of only 20 wk and lack of blinding in the study.
In conclusion, our null hypothesis was proved wrong as both the modalities of treatment give good clinical improvement both subjectively and objectively but arthroscopic capsular release can give improvement earlier as compared to intra- articular steroid injections. However, intra-articular corticosteroids injection is a much less invasive and cheaper option and continues to be an effective modality to alleviate the symptoms in patients with adhesive capsulitis of shoulder. Hence we conclude that intra-articular steroids should be more routinely recommended as the first-line therapy for treatment of idiopathic adhesive capsulitis of shoulder. Arthroscopic capsular release may be recommended as a first-line treatment to patients who do not wish to wait for the results of intra-articular steroid injections. It may also be used for the failures of conservative treatment.
COMMENTS
Background
Frozen shoulder is a common condition and many treatment options are available, but with no clear guidelines. This study compares the outcomes of the two very common methods of treatment - injection steroid (non-surgical method) and arthroscopic arthrolysis (surgical method).
Research frontiers
Researchers are trying to make an animal model mimicking frozen shoulder. Many recent studies have evaluated non-operative methods of treatment and quality of life in patients with frozen shoulder.
Innovations and breakthroughs
The study emphasizes that injection of a steroid in the shoulder without any image guidance gives significant relief in frozen shoulder. This is the situation in most of the actual clinical settings. It improves pain and range of motion, which are the main problems in frozen shoulder. It dispels the belief that image guidance is a must for the intra-articular injection. It also re-establishes the findings of De Carli et al that arthroscopic arthrolysis yields outcomes similar to steroid injection but they occur 2 wk earlier.
Application
The fact that the benefits of arthroscopic arthrolysis precede those of injection of steroid by 4 to 8 wk, may help in selection of treatment modalities depending on the patient profile. This may also be the baseline for future researches.
Peer-review
It is an interesting research.
Footnotes
Institutional review board statement: The ethics committee of All India Institute of Medical Sciences, New Delhi, approved the study.
Informed consent statement: All the patients were informed about the study before including them in the study. The informed consent was explained to them in their native language and a written consent was obtained as advised by the ethic committee of our institute. The identity of any of the patients was not disclosed.
Conflict-of-interest statement: All authors declare no conflict of interest related to this paper.
Data sharing statement: No additional data are available.
Manuscript source: Invited manuscript
Specialty type: Orthopedics
Country of origin: India
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
Peer-review started: October 15, 2016
First decision: December 15, 2016
Article in press: February 20, 2017
P- Reviewer: Cui Q, Li JM, Sewell M S- Editor: Ji FF L- Editor: A E- Editor: Lu YJ
References
- 1.Cleland J, Durall C. Physical therapy for adhesive capsulitis: systematic review. Physiotherapy. 2002;(8):450–456. [Google Scholar]
- 2.Vermeulen HM, Obermann WR, Burger BJ, Kok GJ, Rozing PM, van Den Ende CH. End-range mobilization techniques in adhesive capsulitis of the shoulder joint: A multiple-subject case report. Phys Ther. 2000;80:1204–1213. [PubMed] [Google Scholar]
- 3.Jayson MI. Frozen shoulder: adhesive capsulitis. Br Med J (Clin Res Ed) 1981;283:1005–1006. doi: 10.1136/bmj.283.6298.1005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Baslund B, Thomsen BS, Jensen EM. Frozen shoulder: current concepts. Scand J Rheumatol. 1990;19:321–325. doi: 10.3109/03009749009096786. [DOI] [PubMed] [Google Scholar]
- 5.Binder AI, Bulgen DY, Hazleman BL, Roberts S. Frozen shoulder: a long-term prospective study. Ann Rheum Dis. 1984;43:361–364. doi: 10.1136/ard.43.3.361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shaffer B, Tibone JE, Kerlan RK. Frozen shoulder. A long-term follow-up. J Bone Joint Surg Am. 1992;74:738–746. [PubMed] [Google Scholar]
- 7.Green S, Buchbinder R, Hetrick S. Physiotherapy interventions for shoulder pain. Cochrane Database Syst Rev. 2003;(2):CD004258. doi: 10.1002/14651858.CD004258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Buchbinder R, Green S, Youd JM. Corticosteroid injections for shoulder pain. Cochrane Database Syst Rev. 2003;(1):CD004016. doi: 10.1002/14651858.CD004016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Loew M, Heichel TO, Lehner B. Intraarticular lesions in primary frozen shoulder after manipulation under general anesthesia. J Shoulder Elbow Surg. 2005;14:16–21. doi: 10.1016/j.jse.2004.04.004. [DOI] [PubMed] [Google Scholar]
- 10.Dodenhoff RM, Levy O, Wilson A, Copeland SA. Manipulation under anesthesia for primary frozen shoulder: effect on early recovery and return to activity. J Shoulder Elbow Surg. 2000;9:23–26. doi: 10.1016/s1058-2746(00)90005-3. [DOI] [PubMed] [Google Scholar]
- 11.Quraishi NA, Johnston P, Bayer J, Crowe M, Chakrabarti AJ. Thawing the frozen shoulder. A randomised trial comparing manipulation under anaesthesia with hydrodilatation. J Bone Joint Surg Br. 2007;89:1197–1200. doi: 10.1302/0301-620X.89B9.18863. [DOI] [PubMed] [Google Scholar]
- 12.Andren L, Lundberg BJ. Treatment of rigid shoulders by joint distension during arthrography. Acta Orthop Scand. 1965;36:45–53. doi: 10.3109/17453676508989370. [DOI] [PubMed] [Google Scholar]
- 13.Buchbinder R, Green S, Forbes A, Hall S, Lawler G. Arthrographic joint distension with saline and steroid improves function and reduces pain in patients with painful stiff shoulder: results of a randomised, double blind, placebo controlled trial. Ann Rheum Dis. 2004;63:302–309. doi: 10.1136/ard.2002.004655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gam AN, Schydlowsky P, Rossel I, Remvig L, Jensen EM. Treatment of “frozen shoulder” with distension and glucorticoid compared with glucorticoid alone. A randomised controlled trial. Scand J Rheumatol. 1998;27:425–430. doi: 10.1080/030097498442244. [DOI] [PubMed] [Google Scholar]
- 15.Segmüller HE, Taylor DE, Hogan CS, Saies AD, Hayes MG. Arthroscopic treatment of adhesive capsulitis. J Shoulder Elbow Surg. 2004;4:403–408. doi: 10.1016/s1058-2746(05)80030-8. [DOI] [PubMed] [Google Scholar]
- 16.Klinger HM, Otte S, Baums MH, Haerer T. Early arthroscopic release in refractory shoulder stiffness. Arch Orthop Trauma Surg. 2002;122:200–203. doi: 10.1007/s00402-001-0355-6. [DOI] [PubMed] [Google Scholar]
- 17.Baums MH, Spahn G, Nozaki M, Steckel H, Schultz W, Klinger HM. Functional outcome and general health status in patients after arthroscopic release in adhesive capsulitis. Knee Surg Sports Traumatol Arthrosc. 2007;15:638–644. doi: 10.1007/s00167-006-0203-x. [DOI] [PubMed] [Google Scholar]
- 18.Smith CD, Hamer P, Bunker TD. Arthroscopic capsular release for idiopathic frozen shoulder with intra-articular injection and a controlled manipulation. Ann R Coll Surg Engl. 2014;96:55–60. doi: 10.1308/003588414X13824511650452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Arslan S, Celiker R. Comparison of the efficacy of local corticosteroid injection and physical therapy for the treatment of adhesive capsulitis. Rheumatol Int. 2001;21:20–23. doi: 10.1007/s002960100127. [DOI] [PubMed] [Google Scholar]
- 20.Carette S, Moffet H, Tardif J, Bessette L, Morin F, Frémont P, Bykerk V, Thorne C, Bell M, Bensen W, et al. Intraarticular corticosteroids, supervised physiotherapy, or a combination of the two in the treatment of adhesive capsulitis of the shoulder: a placebo-controlled trial. Arthritis Rheum. 2003;48:829–838. doi: 10.1002/art.10954. [DOI] [PubMed] [Google Scholar]
- 21.Ryans I, Montgomery A, Galway R, Kernohan WG, McKane R. A randomized controlled trial of intra-articular triamcinolone and/or physiotherapy in shoulder capsulitis. Rheumatology (Oxford) 2005;44:529–535. doi: 10.1093/rheumatology/keh535. [DOI] [PubMed] [Google Scholar]
- 22.Sabat D, Kumar V. Early arthroscopic release in stiff shoulder. Int J Shoulder Surg. 2008;2:36–40. doi: 10.4103/0973-6042.40455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Le Lievre HM, Murrell GA. Long-term outcomes after arthroscopic capsular release for idiopathic adhesive capsulitis. J Bone Joint Surg Am. 2012;94:1208–1216. doi: 10.2106/JBJS.J.00952. [DOI] [PubMed] [Google Scholar]
- 24.Jerosch J, Nasef NM, Peters O, Mansour AM. Mid-term results following arthroscopic capsular release in patients with primary and secondary adhesive shoulder capsulitis. Knee Surg Sports Traumatol Arthrosc. 2013;21:1195–1202. doi: 10.1007/s00167-012-2124-1. [DOI] [PubMed] [Google Scholar]
- 25.Warner JJ, Allen A, Marks PH, Wong P. Arthroscopic release for chronic, refractory adhesive capsulitis of the shoulder. J Bone Joint Surg Am. 1996;78:1808–1816. doi: 10.2106/00004623-199612000-00003. [DOI] [PubMed] [Google Scholar]
- 26.Ogilvie-Harris DJ, Biggs DJ, Fitsialos DP, MacKay M. The resistant frozen shoulder. Manipulation versus arthroscopic release. Clin Orthop Relat Res. 1995;(319):238–248. [PubMed] [Google Scholar]
- 27.De Carli A, Vadalà A, Perugia D, Frate L, Iorio C, Fabbri M, Ferretti A. Shoulder adhesive capsulitis: manipulation and arthroscopic arthrolysis or intra-articular steroid injections? Int Orthop. 2012;36:101–106. doi: 10.1007/s00264-011-1330-7. [DOI] [PMC free article] [PubMed] [Google Scholar]


