Abstract
Background
In the hypothesis that the increased collagen metabolism in the intestinal wall of patients affected by inflammatory bowel disease (IBD) is reflected in the systemic circulation, we aimed the study to evaluate serum level of procollagen III peptide (PIIIP) in peripheral and splanchnic circulation by a commercial radioimmunoassay of patients with different histories of disease.
Methods
Twenty-seven patients, 17 with Crohn and 10 with ulcerative colitis submitted to surgery were studied. Blood samples were obtained before surgery from a peripheral vein and during surgery from the mesenteric vein draining the affected intestinal segment. Fifteen healthy age and sex matched subjects were studied to determine normal range for peripheral PIIIP.
Results
In IBD patients peripheral PIIIP level was significantly higher if compared with controls (5.0 ± 1.9 vs 2.7 ± 0.7 μg/l; p = 0.0001); splanchnic PIIIP level was 5.5 ± 2.6 μg/l showing a positive gradient between splanchnic and peripheral concentrations of PIIIP. No significant differences between groups nor correlations with patients' age and duration of disease were found.
Conclusions
We provide evidence that the increased local collagen metabolism in active IBD is reflected also in the systemic circulation irrespective of the history of the disease, suggesting that PIIIP should be considered more appropiately as a marker of the activity phases of IBD.
Background
Crohn's disease (CD) and Ulcerative Colitis (UC) are chronic inflammatory bowel diseases (IBD) of unknown origin of adolescent and young adulthood [1] where genetic polimorphisms [2,3], abnormal inflammation pathways activation [4], and environmental influences [5] seem to concur at different levels in the pathogenesis and the progression of IBD. These pathologic conditions are characterized by focal or diffuse inflammation of the alimentary tract, mucosal damage and epithelial destruction. IBD may be associated with an inability of the intestinal mucosa to protect itself from luminal challenges and inappropriate repair following intestinal injury [6-10]. CD differs from UC by the transmural granulomatous inflammation generally leading to fibrosis, strictures and fistulas [11].
Current opinions suggest that an increased synthesis of collagen type I, III, and V may play an important role in the pathophysiological mechanism leading to intestinal fibrosis [12-15]. An increased synthesis of collagen, namely an increased of procollagen type III, is well documented in fibrotic processes involving other organs such as liver, pancreas, and lung [16-18].
However, not all authors are in agreement regarding the increased serum levels of the aminoterminal propeptide (PIIIP) of collagen in peripheral and splanchnic circulation of patients with active IBD [13,14]. Below we present the results on the serum level of PIIIP in splanchnic and peripheral circulation in patients with active IBD submitted to surgery.
Methods
Twenty-seven patients affected by active IBD, 17 with CD (age 40.2 ± 13.1, yrs from diagnosis 9.2 ± 5.5), and 10 with UC (age 50.3 ± 15.6, yrs from diagnosis 9.8 ± 7.4) submitted to surgery, were enrolled in the study in a double blind fashion. The protocol was approved by local Ethical Committee and informed consent was obtained from all participants to the study. Three patients had CD in small bowel only, two in large bowel only, 12 had ileocolonic disease. Disease activity was assessed according to the Crohn's Disease Activity Index (CDAI) [19] and the Truelove-Witts index (TWI) [20] for CD and UC, respectively. According to CDAI, 2 patients were subclassified as having a moderate form of disease while 15 patients were subclassified as having a severe form of disease. According to TWI, 3 patients were classified as having moderate form of disease, 4 a mild form, and 3 a severe form of disease.
Patients affected by CD were operated on for recurrent obstruction, whereas patients with UC were submitted to surgery because of refractory to medical therapy.
The clinical diagnosis was confirmed by histology (Fig. 1); all cases under study fulfilled the histological criteria as follows:
Figure 1.
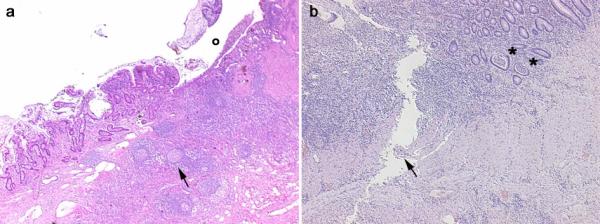
Histological images obtained from two IBD patients enrolled in the study affected by CD (panel a) and UC (panel b) with 12.0 and 10.3 μg/l splanchnic levels of PIIIP, respectively. Panel a, CD: in the transmural section is clearly evident an ulceration (o) in the mucosa and submucosa with diffuse inflammatory infiltrations, pseudo-follicle nodules (arrow), and fibrosis of the intestinal wall. Panel b, UC: the inflammatory infiltration is more evident in the mucosa and submucosa with criptic abscesses (asterisks). A serpiginous linear ulcer is evident (arrow).
- for CD: deep ulcers, marked proliferation of small lymphoid nodules involving all layers of intestinal wall sometime with sarcoid-type granulomas and serosal inflammation;
- for UC: mucosal erosions and superficial ulcerations usually limited to the upper submucosa with cryptic abscesses and glandular destruction.
The clinical profile of the studied patients is reported (Table 1). Two patients did not receive any medication, whereas other patients received two or three drugs for the treatment of IBD. Table 2 shows the treatment protocol for all the studied patients. A control group of 15 healthy age and gender matched subjects was also studied to determine normal range for peripheral PIIIP.
Table 1.
Clinical aspects of the studied patients
| Disease | N° of patients | Age | Sex | Years from diagnosis | Activity index |
| Crohn | CDAI | ||||
| 1 | 34 | F | 12 | Severe | |
| 2 | 35 | M | 8 | Moderate | |
| 3 | 38 | M | 15 | Severe | |
| 4 | 32 | F | 8 | Severe | |
| 5 | 43 | F | 14 | Severe | |
| 6 | 35 | M | 8 | Severe | |
| 7 | 58 | M | 5 | Severe | |
| 8 | 61 | F | 7 | Severe | |
| 9 | 33 | M | 8 | Severe | |
| 10 | 35 | F | 19 | Severe | |
| 11 | 21 | F | 4 | Severe | |
| 12 | 72 | F | 1 | Severe | |
| 13 | 36 | M | 15 | Moderate | |
| 14 | 42 | M | 7 | Severe | |
| 15 | 25 | F | 6 | Severe | |
| 16 | 51 | F | 18 | Severe | |
| 17 | 34 | M | 1 | Severe | |
| Ulcerative colitis | TWI | ||||
| 1 | 68 | F | 15 | Severe | |
| 2 | 70 | F | 1 | Moderate | |
| 3 | 21 | F | 3 | Mild | |
| 4 | 54 | F | 20 | Moderate | |
| 5 | 52 | M | 20 | Mild | |
| 6 | 38 | M | 4 | Moderate | |
| 7 | 64 | M | 6 | Mild | |
| 8 | 38 | F | 16 | Severe | |
| 9 | 41 | F | 3 | Severe | |
| 10 | 57 | M | 10 | Mild |
CDAI: Crohn's Disease Activity Index; TWI: truelove-Witts index.
Table 2.
Frequency distribution for therapy
| Therapy | N° of patients | Crohn | Ulcerative colitis |
| No | 2 | 1 | 1 |
| Aminosalicydic acid | 9 | 8 | 1 |
| Cortisone | 2 | 2 | 0 |
| Aminosalicydic acid + Cortisone | 14 | 6 | 8 |
| Total | 27 | 17 | 10 |
Collagen metabolism (PIIIP)
Different kinds of collagen have been identified in humans. All of them derive from longer precursor molecules (procollagens). They are synthesized intracellularly and secreted in extracellular space where they are cleaved by aminoproteases [21-23]. Among the different kinds of precursors, type III is one of the most abundant interstitial procollagens. Since its aminoterminal propeptide, PIIIP, is formed in equimolar proportions to collagen, serum measurements of this fragment can provide an index of collagen synthesis [23]. The blood samples (two, 5-ml each) for PIIIP measurements were taken from the median cubital vein (p-PIIIP) before surgery after an overnight fast, during surgery from a mesenteric vein (s-PIIIP) draining the intestinal segment chosen for resection by the surgeon. Serum levels of PIIIP were assessed by commercial radioimmunoassay (Orion Diagnostics, Finland). The intra-assay and inter-assay variation were respectively 4% and 4.3%, mean 2.6 μg/l. Normal ranges of peripheral PIIIP concentrations assessed in the control group were 2.7 ± 0.7 μg/l.
Statistical analysis
Data were analyzed using a computer statistical software (SPSS-Rel 10; SPSS Inc., Chicago, Ill). All the quantitative variables were tested for Gaussian distribution with the Kolmogorov-Smirnov test. All that followed this distribution were presented as mean ± standard deviation.
Differences at baseline in collagen parameters between IBD patients and controls were tested for significance using the analysis of variance with the Bonferroni correction. The relation between collagen parameters and the estimated duration of the disease and indices of disease were tested with regression analysis. In all cases, a p value less than 0.05 was considered significant.
Results
Peripheral PIIIP assay
At baseline, before surgery, serum p-PIIIP in IBD patients were significantly higher if compared with healthy controls (5.0 ± 1.9 vs 2.7 ± 0.7 μg/l, respectively; p = 0.0001) (fig 2a). No significant differences were found when comparing CD and UC subgroups (5.0 ± 1.6 vs 4.9 ± 2.4 μg/l, respectively; p = ns) (fig 2b).
Figure 2.
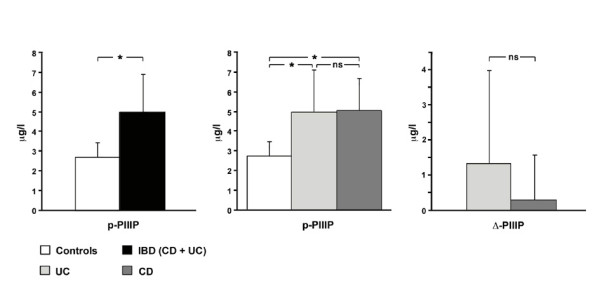
Panel a: Differences in baseline p-PIIIP values in Controls and IBD patients. Panel b: No significant differences in p-PIIIP values between CD and UC subgroups. Panel c: Differences between splancnic and periferic values of PIIIP, without significant differences in CD and UC sbgroups. p-PIIIP: periferic (median cubital vein) PIIIP; s-PIIIP: splancnic (mesenteric vein) PIIIP; Δ-PIIIP: differences between s- and p-PIIIP in IBD patients; IBD: inflammatory bowel diseases; CD: Crohn's Disease; UC: ulcerative colitis;
Splanchnic PIIIP assay
During surgery, serum s-PIIIP in IBD patients was 5.5 ± 2.6 μg/l. No significant differences were found when comparing CD and UC subgroups (5.4 ± 2.3 vs 5.7 ± 3.1 μg/l, respectively; p = ns). A positive gradient was found in IBD patients between splanchnic and peripheral serum concentrations of PIIIP (0.7 ± 1.9 μg/l). This gradient was confirmed when separately considering each disease, without significant differences between the two subgroups (CD 0.3 ± 1.3 vs UC 1.3 ± 2.6 μg/l; p = ns) (fig 2c).
Other variables and PIIIP levels
No significant correlation was found between peripheral and splanchnic levels of PIIIP and the age of the patients and the estimated duration of the disease. Regarding the activity indices, the number of patients belonging to each class was not enough to perform a statistical analysis. Notwithstanding, for the TWI in UC patients a significant difference in PIIIP levels was found between mild and severe form of the disease (Table 3). Finally, no significant differences were found in PIIIP levels between patients treated with glucocorticoids compared with patients not receiving this treatment.
Table 3.
Baseline p-PIIIP levels in UC patients
| TWI Activity Index | Mean ± SD |
| Mild | 7.05 ± 2.25 |
| Moderate | 3.9 ± 1.11 |
| Severe | 3.13 ± 1.57* |
* p = 0.02 vs mild
Discussion
CD and UC are chronic pathologies characterized by an early onset followed by sporadic episodes of acute symptoms during lifetime, debilitating the affected patients to perform their daily functions [24]. Until now controversial theories exist about the synthesis and degradation of PIIIP, its level on systemic circulation, and its deposition far for main target organ [12,13,15,25].
In the present study we have found that intestinal collagen metabolism in IBD patients was increased and that it is reflected in local and systemic circulation. Differently from some experiences [12,13], we have found that serum PIIIP levels in IBD patients was significantly higher if compared with healthy subjects. No significant differences were found in peripheral and splanchnic circulation between patients affected by UC and CD. We also found a positive gradient between serum s-PIIIP and p-PIIIP levels in IBD patients. This gradient was confirmed when considering serum s-PIIIP and p-PIIIP in UC and CD separately, even if the differences between the two subgroups were not statistically significant. In our experience no significant differences were found when considering the age of the patients, the duration of the disease, and the activity indices. This fact implies that serum PIIIP should not be considered a long-term marker of the disease, probably reflecting the short-term fluctuation in the activity phases of the remodeling processes.
When comparing the mild with the severe form of the disease, a significant difference in PIIIP levels was found only in patients affected by UC. This data will probably be confirmed when the number of patients enrolled in each disease-related activity categories is extended as presently in our series the majority of the patients were classified as severe.
The effect of glucocorticoids on collagen synthesis, collagenase, and collagen degradation has not yet fully been clarified [25]. In our study the cortisone therapy did not have influence on the PIIIP levels, but the number of patients was too small and it was not possible to speculate on this regard.
Conclusions
In conclusion we provide evidence that collagen metabolism in IBD is reflected in the systemic and local circulation, without any differences between UC and CD, irrespective of the age of the patients and the duration of the disease. Therefore, this marker may give further information on the activity phases rather than on the entire history of the disease. Further data on the possible use of PIIIP as useful marker of choice for surgical option are attended from the follow-up at 6 and 12 months, which is still on-going [26].
List of abbreviations
Inflammatory bowel diseases = IBD
Procollagen III propeptide = PIIIP
Peripheral Procollagen III propeptide = p-PIIIP
Splanchnic Procollagen III propeptide = s-PIIIP
Crohn's disease = CD
Ulcerative Colitis = UC
Crohn's Disease Activity Index = CDAI
Truelove-Witts index = TWI
Competing interests
The author(s) declare that they have no competing interests.
Authors' contributions
UC conception and design, interpretation of data, drafting the article
MDS conception and design, interpretation of data, drafting the article
ECA performed surgical operations, critical revision of the article, final approval of the version
BO patients' enrollement, blood samples collection
RP statistical analysis, interpretation of data, drafting the article
AP echocardiographic studies
GB radioimmunoassays
EO radioimmunoassays
SF histological examinations
FM interpretation of data, critical revision of the article, final approval of the version
MMC conception and design, interpretation of data, drafting the article
All Authors read and approved the final manuscript.
Pre-publication history
The pre-publication history for this paper can be accessed here:
Contributor Information
Matilde De Simone, Email: matilde.desimone@unimi.it.
Ugo Cioffi, Email: ugo.cioffi@unimi.it.
Ettore Contessini-Avesani, Email: ettore.contessini@unimi.it.
Barbara Oreggia, Email: ettore.contessini@unimi.it.
Roberta Paliotti, Email: roberta.paliotti@unimi.it.
Alberto Pierini, Email: img.lab@mailserver.unimi.it.
Gianni Bolla, Email: img.lab@mailserver.unimi.it.
Elide Oggiano, Email: img.lab@mailserver.unimi.it.
Stefano Ferrero, Email: stefano.ferrero@unimi.it.
Fabio Magrini, Email: fabio.magrini@unimi.it.
Michele M Ciulla, Email: michele.ciulla@unimi.it.
References
- Fiocchi C. Inflammatory bowel disease: etiology and pathogenesis. Gastroenterology. 1998;115:182–205. doi: 10.1016/s0016-5085(98)70381-6. [DOI] [PubMed] [Google Scholar]
- Zheng CQ, Hu GZ, Zeng ZS, Lin LJ, Gu GG. Progress in searching for susceptibility gene for inflammatory bowel disease by positional cloning. World J Gastroenterol. 2003;9:1646–1656. doi: 10.3748/wjg.v9.i8.1646. Review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tamboli CP, Cortot A, Colombel JF. What are the major arguments in favour of the genetic susceptibility for inflammatory bowel disease? Eur J Gastroenterol Hepatol. 2003;15:587–592. doi: 10.1097/00042737-200306000-00002. [DOI] [PubMed] [Google Scholar]
- Devani M, Cugno M, Vecchi M, Ferrero S, Di Berardino F, Avesani EC, de Franchis R, Colman RW. Kallikrein-kinin system activation in Crohn's disease: differences in intestinal and systemic markers. Am J Gastroenterol. 2002;97:2026–2032. doi: 10.1016/S0002-9270(02)04276-4. [DOI] [PubMed] [Google Scholar]
- Krishnan A, Korzenik JR. Inflammatory bowel disease and environmental influences. Gastroenterol Clin North Am. 2002;31:21–39. doi: 10.1016/s0889-8553(01)00003-6. [DOI] [PubMed] [Google Scholar]
- Ciulla M, Cioffi U, De Simone M, Contessini-Avesani E. TGF-beta1 and collagen methabolism in IBD patients. Med Sci Monit. 2002;8:LE55–56. [PubMed] [Google Scholar]
- Hendrickson BA, Gokhale R, Cho JH. Clinical aspects and pathophysiology of inflammatory bowel disease. Clin Microbiol Rev. 2002;15:79–94. doi: 10.1128/CMR.15.1.79-94.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chutkan RK. Inflammatory bowel disease. Prim Care. 2001;28:539–556. doi: 10.1016/s0095-4543(05)70052-x. [DOI] [PubMed] [Google Scholar]
- Harper PC, McAuliffe TL, Beeken WL. Crohn's disease in the elderly. A statistical comparison with younger patients matched for sex and duration of disease. Arch Intern Med. 1986;146:753–755. doi: 10.1001/archinte.146.4.753. [DOI] [PubMed] [Google Scholar]
- Oliva-Hemker M, Fiocchi C. Etiopathogenesis of inflammatory bowel disease: the importance of the pediatric perspective. Inflamm Bowel Dis. 2002;8:112–128. doi: 10.1097/00054725-200203000-00008. [DOI] [PubMed] [Google Scholar]
- Pucilowska JB, McNaughton KK, Mohapatra NK, Hoyt EC, Zimmermann EM, Balfour Sartor R, Kay Lund P. IGF-I and procollagen a 1 (I) are coexpressed in a subset of mesenchymal cells in active Crohn's disease. Am J Physiol Gastrointest Liver Physiol. 2000;279:G1307–1322. doi: 10.1152/ajpgi.2000.279.6.G1307. [DOI] [PubMed] [Google Scholar]
- Kjeldsen J, Schaffalitzky de Muckadell OB, Junker P. Seromarkers of collagen I and III metabolism in active Crohn's disease. Relation to disease activity and response to therapy. Gut. 1995;37:805–810. doi: 10.1136/gut.37.6.805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kjeldsen J, Rasmussen M, Schaffalitzky de Muckadell OB, Kronborg O, Junker P. Collagen metabolites in the peripheral and splanchnic circulation of patients with Crohn disease. Scand J Gastroenterol. 2001;36:1193–1197. doi: 10.1080/00365520152584833. [DOI] [PubMed] [Google Scholar]
- Silvennoinen J, Risteli L, Kartunen T, Risteli J. Increased degradation of type I collagen in patients with inflammatory bowel disease. Gut. 1996;38:223–228. doi: 10.1136/gut.38.2.223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stallmach A, Schuppan D, Riese HH, Matthes H, Riecken EO. Increased collagen type III synthesis by fibroblasts isolated from strictures of patients with Crohn's disease. Gastroenterology. 1992;102:1920–1929. doi: 10.1016/0016-5085(92)90314-o. [DOI] [PubMed] [Google Scholar]
- Hahn EG, Schuppan D. Ethanol and fibrinogenesis in the liver. In: Seitz HK, Kommerell B, editor. In Alcohol-related disease in gastroenterology. Berlin: Springer-Verlag; 1985. pp. 124–153. [Google Scholar]
- Uscanga L, Kennedy RH, Choux R, Drugmont M, Grimand JA, Sarles H. Sequential connective tissue matrix changes in experimental acute pancreatitis. An immunohistochemical and biochemical assessment in the rat. Int J Pancreatol. 1987;2:33–45. doi: 10.1007/BF02788347. [DOI] [PubMed] [Google Scholar]
- Cantin AM, Boileau R, Begin R. Increased procollagen III aminoterminal peptide related antigens and fibroblastic growth signals in the lungs of patients with idiopathic pulmonary fibrosis. Am Rev Respir Dis. 1988;137:572–578. doi: 10.1164/ajrccm/137.3.572. [DOI] [PubMed] [Google Scholar]
- Best WR, Becktel JM, Singleton JW, Kern F. Development of a Crohn's disease activity index. Gastroenterology. 1976;70:439–444. [PubMed] [Google Scholar]
- Truelove SC, Witts LJ. Cortisone in ulcerative colitis: final report of a therapeutic trial. Br Med J. 1955;4947:1041–1048. doi: 10.1136/bmj.2.4947.1041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prockop DJ, Kivirikko KI, Tuderman L, Guzman NA. The biosynthesis of collagen and its disorders. N Engl J Med. 1979;301:13–23. doi: 10.1056/NEJM197907053010104. [DOI] [PubMed] [Google Scholar]
- Querejeta R, Varo N, Lopez B, Larmanet M, Artinano E, Etayo JC, Martinez JL, Gutierrez-Stampa M, Emparanza JI, Gil MJ, Monreal I, Mindan JP, Diez J. Serum carboxi-terminal propeptide of procollagen type I is a marker of myocardial fibrosis in hypertensive heart disease. Circulation. 2000;101:1729–1735. doi: 10.1161/01.cir.101.14.1729. [DOI] [PubMed] [Google Scholar]
- Fessler JH, Fessler LI. Biosynthesis of procollagen. Annu Rev Biochem. 1978;47:129–162. doi: 10.1146/annurev.bi.47.070178.001021. [DOI] [PubMed] [Google Scholar]
- Longobardi T, Jacobs P, Bernstein CN. Work losses related to inflammatory bowel disease in the United States: Results from the National Health Interview Survey. Am J Gastroenterol. 2003;98:1064–1072. doi: 10.1111/j.1572-0241.2003.07285.x. [DOI] [PubMed] [Google Scholar]
- Babic Z, Jagic V, Petrovic Z, Bilic A, Dinko K, Kubat G, Troskot R, Vukelic M. Elevated serum values of procollagen III peptide (PIIIP) in patients with ulcerative colitis who will develop pseudopolyps. World J Gastroenterol. 2003;9:619–621. doi: 10.3748/wjg.v9.i3.619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cioffi U, Ciulla MM, De Simone M, Paliotti R, Pierini A, Magrini F, Botti F, Contessini-Avesani E. Effects of chronic inflammatory bowel diseases on left ventricular structure and function: a study protocol. BMC Public Health. 2002;2:19. doi: 10.1186/1471-2458-2-19. [DOI] [PMC free article] [PubMed] [Google Scholar]


