Abstract
Renal replacement therapy (RRT) options and practice varies in countries worldwide and is influenced by patients' choice, nephrologists' practice patterns, health system, payer practice, public policy, and socioeconomic factors. In India, hemodialysis (HD) remains the dominant RRT modality, and the practice is largely influenced by socioeconomics of the region of practice since third party payer is limited. Resource stretch to maximize outcome benefit is essential and HD session twice weekly is an improvized and cost-effective clinical practice. However, within the country, the patient characteristics, practice patterns, and outcomes of twice-weekly HD compared against patients dialyzed thrice weekly remain unclear. We did a retrospective analysis of patients who underwent twice- and thrice-weekly HD in a single center under similar settings. The patients on thrice a week dialysis were older and with a higher proportion of diabetics and were insured by private payers. Weight gain, ultrafiltration rates, blood pressures, and hemoglobin remained more favorable in the thrice-weekly patients. There was no significant difference in the hospitalization rates or mortality rates in the two groups. Patients who undergo twice-weekly HD have poorer intermediate measures of the outcome; although, morbidity and survival were not different in a small study population with short follow-up. The small sample size and the short duration of follow-up may limit the scope of findings of our study.
Keywords: Comparison twice- and thice-weekly hemodialysis, cost effective hemodialysis pattern, outcome
Introduction
Chronic kidney disease (CKD) is an emerging health problem in India, with an incidence of end-stage renal disease (ESRD) reported to be 160–232 per million population (pmp).[1] In an epidemiological study of an urban population, the projected prevalence of CKD was 785–870 pmp.[2] The care of CKD patients in India has multi-fold challenges among the constraints of economic resources, lack of the third party payer system, competing priorities for health care needs for public policy, limited trained worked force in nephrology, and significant accessibility and availability challenge in renal replacement therapy (RRT).[3] In such a background of a huge mismatch between demand for renal care and the ability to provide these services, it is estimated that only 10–20% of ESRD patients receive any form of RRT.[3,4] Delayed start of RRT-based on symptoms, the lesser frequency of dialysis, limited use of Erythropoietin, truncated laboratory monitoring are a common practice in RRT care in India to balance cost and quality.[5,6] In this context, few observational studies analysed hemodialysis (HD) outcomes in India, particularly of the variance in practice compared to set norms of the developed world.[5,6] In recent years, observational studies of twice-weekly HD (2x) in Taiwan, and China have shown a possible benefit of the slower decline of renal function and acceptable nutritional status.[7,8] However, there is a lacuna of knowledge of the unique clinical aspects of patients dialyzed twice weekly in India. We attempted to study this aspect by comparing differences between patients dialyzed twice and thrice weekly (3x) in a similar clinical setting.
Materials and Methods
This study was a retrospective observational analysis of incident and prevalent patients undergoing HD at a stand-alone dialysis facility in India. Data of patients on dialysis from June 1, 2012, to December 31, 2013, were considered for analysis. Patients who underwent fewer than five consecutive sessions or who were being dialyzed for acute kidney injury were excluded from the study. Twice weekly (2x) patients were compared against thrice weekly (3x) patients for age, sex, and cause of CKD. Duration of follow-up period, mean interval of laboratory assessment were assessed. Blood pressure at the start and end of HD were reviewed. Weight gain between dialysis sessions was noted and ultrafiltration in each session was obtained. Laboratory parameters including hemoglobin (Hb), adequacy as measured by urea reduction ratio (URR) and standard Kt/V, albumin, were collected.
Statistical analysis
Data were expressed as mean and standard deviation and proportion. To compare continuous parameters, we used independent t-test or Mann–Whitney test. For comparison of proportions, we used Pearson's Chi-square or exact test as appropriate. When distributions are counts we used exact Poisson confidence interval approach to decide the difference of significance. For regression analysis, we used Cox proportional hazard model. For multiple regression, we adopted step-wise backward (Wald) method. The probability of entry into the model was set to 0.05 and for removal was set to 0.1. Incidences were compared using mid – P exact method. Rate ratios and confidence intervals were calculated. SPSS 22 (manufactured earlier by SPSS Inc and later acquired by IBM in 2009) and STATA 12 software (manufactured by StataCorp) were used for statistical analysis. Probability <0.05 was considered statistically significant.
Results
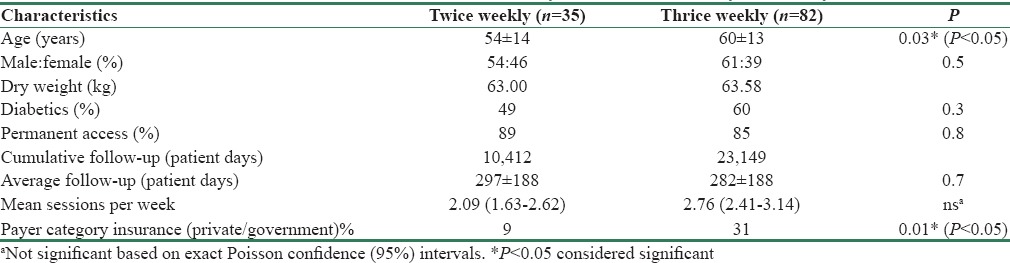
A total of 117 patients were included, of which 35 (29.91%) and 82 (70.08%) were on twice a week dialysis (2x) and thrice a week (3x) dialysis, respectively. Baseline characteristics such as age and gender distribution, etiology of CKD (diabetic and nondiabetic kidney disease) were similar in both the groups. [Table 1] The vascular access modality was similar in both groups. About 89% of twice-weekly and 85% of thrice-weekly patients had an arteriovenous fistula (AVF) whereas 11% and 15% of twice and thrice weekly patients had a temporary catheter, respectively, all being an internal jugular vein catheter.
Table 1.
Patient characteristics in twice-weekly versus thrice-weekly hemodialysis
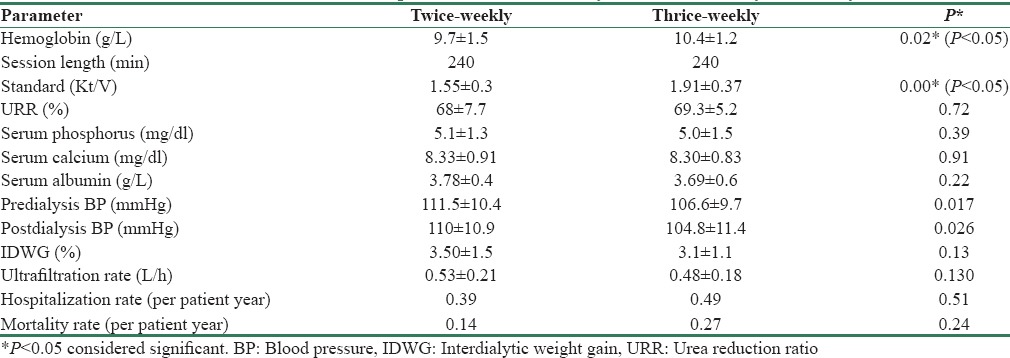
The mean interval between Hb and adequacy assessment was 1.7 and 5.4 months, respectively, for twice-weekly and 1.7 months and 3.3 months, respectively, for thrice-weekly patients. The intervals between assessment of serum phosphorus and albumin were 2.7 and 2.9 months, respectively, for 2x and 1.9 months each for 3x (not shown in table). The data presented in Table 2 are the average of all parameters during the follow-up period of the individual patient during the study.
Table 2.
Treatment outcome of patients on twice-weekly and thrice-weekly hemodialysis
Fewer number of patients in the 2x group were covered with some kind of insurance scheme compared with the 3x patients. (9% vs. 31%; P = 0.01). [Table 1]. Median duration of dialysis was about 288 days in both groups. The cumulative follow-up in patient days was 10,412 and 23,149 respectively in the 2x and 3x groups, whereas the mean follow-up in patient days was 297 ± 188 and 282 ± 188, respectively, in the two groups. The median follow-up and interquartile range were 291 and 241 days; and 341 and 358 days, respectively, in the two groups.
URR of >65% was achieved in 69.6% and 79% in twice and thrice weekly dialysis patients, respectively. Adequacy measured as standard Kt/V was defined to be adequate if it was above 1.45 for 2x and above 2.0 for 3x patients; 69.6% and 40.4% in these groups, respectively, reached their target. The mean URR was 68% ± 7.7 and 69.3% ±5.2, respectively. The mean standard Kt/V was 1.6 and 1.9, respectively, (P = 0.0001). Mean arterial pressure before and after dialysis, and access type were similar in the two groups. The mean serum albumin in the two groups were not significantly different. The mean serum phosphorus in the two groups were 5.09 ± 1.3 mg/dl and 5.01 ± 1.47 mg/dl, respectively. There was no significant difference in the inter-dialytic weight gain in the two groups. Mean ultrafiltration rate was 0.53 ± 0.21 L/h and 0.48 ± 0.18 L/h in twice weekly and thrice weekly HD, respectively.
The number of hospitalizations in the 2x and 3x groups were 14 and 46, respectively, over the study period. The hospitalization rates per patient year were 0.39 and 0.49 in the 2x and 3x groups, respectively, with rate ratio of 0.79 (0.40–1.57). The number of deaths were 4 and 17, respectively, in the two groups. Of the four deaths in the 2x group, 2 each were due to a cardiac event and 2 were sudden cardiac deaths (SCDs). Of the 17 deaths in the 3x group, 4 were cardiac events, 6 were SCDs, 4 died due to sepsis, and 3 deaths were due to other causes (liver failure, discontinuation of dialysis, and noncompliance). There were no access-related complications. The mortality rates as patient years were 0.14 and 0.27, respectively. The rate ratio was 0.52 (0.18–1.53). The number of patients who dropped out or were transferred out during the study period was 18 and 25, respectively, in the 2x and 3x groups. These also included the transit patients. Two patients in the 2x group and 3 patients in the 3x group were lost to follow-up. There were 7 patients who were transplanted in the 3x group (none in the 2x group received a transplant during the study).
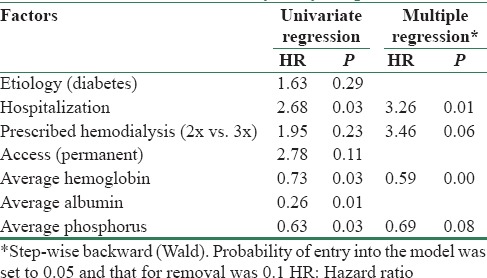
Univariate regression (Cox proportional hazard model) analysis indicated that the significant factors for mortality were hospitalization, lower Hb, serum albumin, and serum phosphorus level. [Table 3]. On multiple regression model, the significant factors for mortality identified were hospitalization and lower Hb after controlling for HD frequency and serum phosphorus level. Step-wise backward regression analysis indicated that hazard of death on hospitalization was significant (P = 0.01), and it was 3.26 times more compared to nonhospitalization after controlling the effect of HD frequency, Hb and phosphorus.
Table 3.
Factors associated with survival status of twice- and thrice-weekly dialyzed patients
Discussion
This study summarizes the salient differences in patient characteristics, intermediate measures, and outcomes in twice weekly and thrice weekly HD patients. All patients in our unit are advised to undergo dialysis three times a week as per convention. However, few chose twice a week dialysis based on affordability and insurance coverage. At times, based on clinical assessment, modification of frequency was recommended and it was implemented if the patient was willing for the same. The study was carried out retrospectively to compare outcomes in these two groups from available data. Residual renal function (RRF) could not be assessed due to the retrospective nature of the study. Subjective global assessment was not available for most of the patients for the same reason.
Mean age was similar in the two groups. Lower mean age and male predominance were traits observed in both the groups reflecting the sociocultural influence of health seeking behavior, rather than a gender difference, as reported previously.[4,5,6,9] High prevalence of AVF in our study is consistent with previously reported cohorts from India.[6,10] Diabetic patients were higher in the 3x group aligned with a high prevalence of diabetes in CKD population.[11] The follow-up period for patients in this study may appear short, but it is not insignificant given the duration of survival reported in patients on HD in India.[5,6] A small proportion of our patients had third party payers reflective of the existing practice patterns and consequential constraints in the delivery of care. There is a trend toward a higher proportion of privately insured patients in the 3x category, which reflects the choice of HD frequency is influenced by payer category.
The delivered dialysis frequency of patients in the 2x and 3x groups are marginally shifted away from the prescribed frequency due to patients in 2x patients choosing to have extra HD sessions to improve fluid management periodically and 3x patients missing occasional HD sessions. The frequency of laboratory testing is less than the standard of care in developed nations. It is indicative of the frugal practice that clinicians need to adopt in utilizing parameters of value to aid cost effective care. The mean interval for Hb, adequacy, phosphorus, and albumin indicates the average interval duration between time points of laboratory diagnostic evaluation. Since the compliance to laboratory monitoring varies in individual patients, we opted to present the data in this format. Hb seems to get the highest weight, whereas mineral bone disease, and nutritional assessment are relatively less weighted as shown by longer intervals between laboratory testing.
A study on HD in India showed that survival was better with higher dialysis dose, increased frequency of dialysis and adequate albumin level.[9] Two other studies have highlighted the practice compulsion of utilization of twice-weekly dialysis in a high proportion of patients, inadequate dosing of erythropoietin, and poor survival among insurmountable challenge in HD.[5,6] None of the previous studies have illustrated weight gain and ultrafiltration practice which may have a considerable influence on morbidity and mortality in the Indian context of 2x HD.
In an encouraging observation by Lin et al., RRF in patients undergoing twice-weekly dialysis had a slower decline than in those on thrice-weekly dialysis, and the former also had less hospitalization rates.[12] Two other studies have highlighted the same aspect on 2x HD.[13,14] In another study in Shanghai of twice weekly HD patients were significantly younger and had a shorter vintage. They had an HD session time of 4.8 h resulting in spKt/V of 1.65 and weekly Kt/V of 3.29. The values for Kt/V achieved in this study are for standard Kt/V and not single pool Kt/V. The formula used to calculate was the Daugirdas formula. As reported in the Kidney Disease Outcomes Quality Initiative (KDOQI) guidelines, the recommended target for standard Kt/V for 3x HD is 2.0 by KDOQI. There are no standard practice guidelines for 2x patients. We chose 1.45 as a target based on the largest series of 2x HD published by Dialysis Outcomes and Practice Patterns Study (DOPPS) from a patient population in China.[7] Age, body mass index, albumin, and Kt/V were markers of survival, but higher solute clearance is an influencing factor.[8] Significantly, a small subset of both incident patients and patients with dialysis vintage of 5 years had better survival on 2x HD than 3x HD.[8] Cross-sectional data from China under DOPPS found that 26% of patients in China were dialyzing twice a week. Female sex, shorter dialysis vintage, lower socioeconomic status, less health insurance coverage, and lack of diabetes and hypertension were associated with dialyzing twice a week.[7]
This study has several limitations in that it is a retrospective study. The RRF has not been analyzed. India being a very diverse and heterogeneous population, the sample is not representative as this center caters to a more affording and educated population. Larger studies targeting different groups of people across different strata of society would be helpful in knowing the differences in outcomes in the two groups. Understanding the survival predictors within the twice weekly dialysis group may help nephrologists choose such practice more appropriately. This study has limitations including the retrospective nature, small sample size, short duration of follow-up, varying frequency of laboratory monitoring intervals, lack of detailed data on hospitalizations and of clear documentation of comorbidity.
Conclusion
Twice a week hemodialysis is a feasible prescription in developing nations. Larger prospective trials comparing patients dialysed twice and thrice weekly will be needed to make this a standard practice.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Modi GK, Jha V. The incidence of end-stage renal disease in India: A population-based study. Kidney Int. 2006;70:2131–3. doi: 10.1038/sj.ki.5001958. [DOI] [PubMed] [Google Scholar]
- 2.Agarwal SK, Dash SC, Irshad M, Raju S, Singh R, Pandey RM. Prevalence of chronic renal failure in adults in Delhi, India. Nephrol Dial Transplant. 2005;20:1638–42. doi: 10.1093/ndt/gfh855. [DOI] [PubMed] [Google Scholar]
- 3.Agarwal SK, Srivastava RK. Chronic kidney disease in India: Challenges and solutions. Nephron Clin Pract. 2009;111:c197–203. doi: 10.1159/000199460. [DOI] [PubMed] [Google Scholar]
- 4.Abraham G, Moorthy AV, Aggarwal V. Chronic kidney disease: A silent epidemic in Indian subcontinent – Strategies for management. J Indian Med Assoc. 2006;104:689–91. [PubMed] [Google Scholar]
- 5.Sankarasubbaiyan S, Rajkumar A, Tangalvadi TA, Dawood US, Kaur P. Challenges and limitations of maintenance hemodialysis in urban South India. Hemodial Int. 2007;11:485–91. doi: 10.1111/j.1542-4758.2007.00219.x. [DOI] [PubMed] [Google Scholar]
- 6.Swarnalatha G, Ram R, Prasad N, Dakshinamurty KV. End-stage renal disease patients on hemodialysis: A study from a tertiary care center in a developing country. Hemodial Int. 2011;15:312–9. doi: 10.1111/j.1542-4758.2011.00546.x. [DOI] [PubMed] [Google Scholar]
- 7.Bieber B, Qian J, Anand S, Yan Y, Chen N, Wang M, et al. Two-times weekly hemodialysis in China: Frequency, associated patient and treatment characteristics and quality of life in the China dialysis outcomes and practice patterns study. Nephrol Dial Transplant. 2014;29:1770–7. doi: 10.1093/ndt/gft472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lin X, Yan Y, Ni Z, Gu L, Zhu M, Dai H, et al. Clinical outcome of twice-weekly hemodialysis patients in Shanghai. Blood Purif. 2012;33:66–72. doi: 10.1159/000334634. [DOI] [PubMed] [Google Scholar]
- 9.Chandrashekar A, Ramakrishnan S, Rangarajan D. Survival analysis of patients on maintenance hemodialysis. Indian J Nephrol. 2014;24:206–13. doi: 10.4103/0971-4065.132985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sankarasubbaiyan S, Abraham G, Soundararajan P, Chandrasekaran V, Padma G. Parathyroid hormone and biochemical profile in chronic kidney disease patients in South India. Hemodial Int. 2005;9:63–7. doi: 10.1111/j.1492-7535.2005.01119.x. [DOI] [PubMed] [Google Scholar]
- 11.Rajapurkar MM, John GT, Kirpalani AL, Abraham G, Agarwal SK, Almeida AF, et al. What do we know about chronic kidney disease in India:First report of the Indian CKD registry. BMC Nephrol. 2012;13:10. doi: 10.1186/1471-2369-13-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lin YF, Huang JW, Wu MS, Chu TS, Lin SL, Chen YM, et al. Comparison of residual renal function in patients undergoing twice-weekly versus three-times-weekly haemodialysis. Nephrology (Carlton) 2009;14:59–64. doi: 10.1111/j.1440-1797.2008.01016.x. [DOI] [PubMed] [Google Scholar]
- 13.Teruel-Briones JL, Fernández-Lucas M, Rivera-Gorrin M, Ruiz-Roso G, Díaz-Domínguez M, Rodríguez-Mendiola N, et al. Progression of residual renal function with an increase in dialysis: Haemodialysis versus peritoneal dialysis. Nefrologia. 2013;33:640–9. doi: 10.3265/Nefrologia.pre2013.May.12038. [DOI] [PubMed] [Google Scholar]
- 14.Vilar E, Wellsted D, Chandna SM, Greenwood RN, Farrington K. Residual renal function improves outcome in incremental haemodialysis despite reduced dialysis dose. Nephrol Dial Transplant. 2009;24:2502–10. doi: 10.1093/ndt/gfp071. [DOI] [PubMed] [Google Scholar]


