Abstract
Introduction:
Logbooks of self-monitoring of blood glucose (SMBG) are useful in the modulation of insulin regimens, which aid in achieving glycemic control in type 1 diabetes mellitus (T1DM). However, discrepancies in SMBG charting may impede its utility. This study aimed to assess the accuracy of log entries and its impact on long-term glycemic control.
Methods:
SMBG in logbooks was compared with readings in glucometer memory and discrepancies between the two were evaluated in 101 children with T1DM. The relationship between these discrepancies and glycated hemoglobin (HbA1c) over 44 months was assessed.
Results:
Errors in glucose charting were observed in 32.67% children. The most common observed error was omission (42.42%), followed by fabrication (27.27%), erroneous (18.18%), and others (12.12%). Age was not significantly different among children having accurate versus inaccurate SMBG logs. During follow-up of 44 months, children with accurate SMBG logs consistently had lower HbA1c as compared to children having inaccurate logs, which was statistically significant at 4, 16, 20, and 28 months' follow-up. The same was reflected in the proportion of children achieving HbA1c <7% and 7%–9%. Of the 14 children who had omissions, 9 had omission of high values only, 3 patients had omission of low values only, 1 had omission of both high and low values, and 1 had omission of normal values. Among logs with fabrication, parents were responsible in 2 of 9 incidents. In the remaining 7, it was the child himself/herself. Children with fabrication consistently had the highest HbA1c values among the different types of inaccurate blood glucose chartings, which was statistically significant at 32 and 36 months of follow-up.
Conclusions:
Reliability of SMBG logs is a significant problem among children with T1DM at our center. Children with accurate logs of SMBG readings were more likely to have better glycemic control on long-term follow-up.
Keywords: Fabrication, logbook, omission, reliability, self-monitoring of blood glucose, type-1 diabetes
INTRODUCTION
India is the diabetes capital of the world, with diabetes and prediabetes prevalence of 9% and 11%–14%, respectively.[1] Apart from type-2 diabetes mellitus (T2DM), which constitutes a bulk of this disease burden, India has also witnessed an exponential increase in the burden of T1DM, and globally it has the second largest population of children and young adults with T1DM, second only to the USA.[1,2] Self-monitoring of blood glucose (SMBG) is an invaluable method of monitoring glycemic status. Current guidelines recommend its use in all patients with T1DM, T2DM, or any other forms of diabetes (e.g., gestational diabetes) on multiple subcutaneous insulin injections (MSII).[3] A database study of almost 27,000 children and adolescents with T1DM showed that after adjustment for multiple confounders, increased daily frequency of SMBG was significantly associated with lower glycated hemoglobin (HbA1C) (0.2% per additional test per day, leveling off at five tests per day) along with added benefits of fewer acute complications.[4]
Optimal use of SMBG requires regular checking of capillary glucose using a glucometer, appropriate and timely entry in the logbook, proper review and interpretation of the data, both by the patient as well as the caregiver to optimize his treatment regimen. Use of a structured display of SMBG readings in the form of “diaries” or “logbooks” has been shown to improve glycemic control by facilitating timely treatment modulation.[5] However, interpretation of logbook entries may be complicated by the possibility of unreliable, incorrect entries, and discrepancies, which may result in less optimal titration of treatment regimens, thus hampering the glycemic control in an individual patient. Hence, the aim of this study was to assess the reliability of SMBG logs as compared to glucometer memory in children with T1DM from India and to evaluate its impact on long-term glycemic outcomes.
METHODS
The study was carried out in a dedicated clinic for T1DM patients at a tertiary care center in eastern India. This study is a retrospective analysis of the follow-up clinical and glycemic control data of children with T1DM attending this clinic. For inclusion, only those children who were visiting the clinic and were part of changing diabetes in children (CDiC) program for at least 1 year were included in this study. Children with duration of T1DM <1 year were excluded from the study, to exclude any possibility of honeymoon phase of T1DM. These children were receiving free insulin, glucometer, and strips for checking blood glucose from the CDiC program, a program running in many developing countries with the help of Novo Nordisk.
All of the consecutive 119 children <18 years age attending this clinic were considered for this study. A total of 101 willing children, who fulfilled all criteria, were recruited after obtaining informed written consent from them/caregivers. All these children were given the same glucometer and strips (Accu-Chek Active; Roche, Mumbai, Maharashtra, India). The glucometer had memory backup function. Patients also received a logbook for entering blood glucose values measured during different times of the day (fasting, 2 h postbreakfast, prelunch, 2 h postlunch, predinner, 2 h postdinner, and 2–3 a.m. blood glucose values). All children and their caregivers were given orientation classes on the use of these glucometers, SMBG logbooks, entry into these logbooks, insulin injection techniques, sick day rules, identification and management of hypoglycemia, other complications, and dietary management at the time of recruitment in the study.
Patients had to visit the clinic at least once monthly for the duration of the study. During these visits, they underwent detailed clinical examination; insulin injection sites and injection techniques were checked and correct techniques were reinforced, SMBG logbooks were evaluated, and glucometer memory logs were checked and cross-matched. Glucose measurements in the glucometer memory logs were considered as the standard. Logbook entries that differed by at least 20 mg/dl from actual values in the memory of glucometers were defined as “incorrect entries.” All discrepancies were recorded. Every attempt was made to find a cause for these discrepancies. Information was also obtained regarding the person who was checking the glucose values and entering into the logbook. Glucometers were calibrated once a year.
All children were on MSII with combinations of human insulin regular (Actrapid®, Novo Nordisk, India) and human insulin intermediate acting (Insulatard®, Novo Nordisk, India), which were provided from the clinic on a monthly basis during these visits. HbA1c levels were used for assessment of glycemic control. Blood samples of 3 ml were collected for HbA1c assessment 4 monthly during these visits for HbA1c assessment. HbA1c was measured using ion-exchange high-performance liquid chromatography method using Bio-Rad D10 HbA1c assay platform having intra- and inter-assay coefficient of variation of 0.9%–1.2%, respectively. Children with HbA1c <7%, 7%–9%, and 9% were defined to have good, intermediate, and poor glycemic control, respectively.
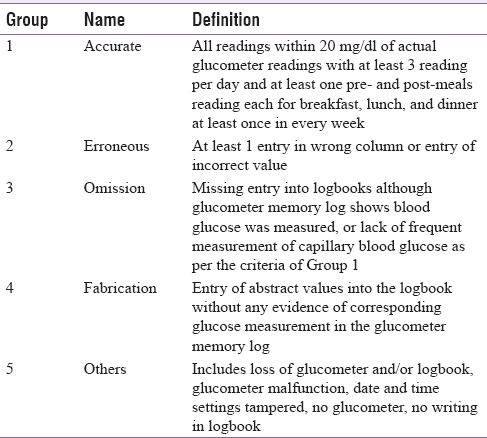
Logbook entries were defined as “accurate” (Group 1) if the entire SBMG recording in the logbook tallied with the glucometer memory logs (all readings within 20 mg/dl of actual glucometer readings with at least 3 readings per day and at least one premeals and postmeals reading each for breakfast, lunch, and dinner at least once in every week). “Incorrect entries” were classified into (a) erroneous: at least 1 entry in wrong column or entry of incorrect value (Group 2), (b) omission: Missing entry into logbooks although glucometer memory log shows blood glucose was measured, or lack of frequent measurement of capillary blood glucose as per the criteria of Group 1 (vide supra) (Group 3), (c) fabrication: Entry of abstract values into the logbook without any evidence of corresponding glucose measurement in the glucometer memory (Group 4), and (d) others: Includes loss of glucometer and/or logbook, glucometer malfunction (Group 5) [Table 1].
Table 1.
Classification of logbook glucose recordings
Statistical analysis
All continuous variables were expressed in mean and standard deviation, and comparisons between multiple groups were made through one-way ANOVA. Comparison between two groups was done through Student's unpaired t-test. Categorical variables were expressed as absolute numbers (percentage). Statistical Package for Social Sciences (SPSS®, Armonk, NY: IBM Corp) version-20 software was used for statistical analysis.
RESULTS
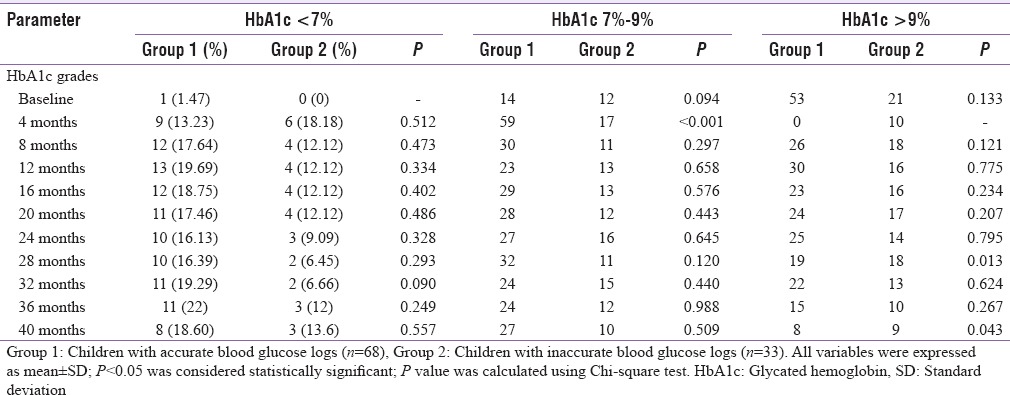
Errors in blood glucose charting in the logbooks were observed in 33 out of 101 children (32.67%) with T1DM in our study. The most common type of error observed was omission (42.42%; n = 14), followed by fabrication (27.27%; n = 9), erroneous (18.18%; n = 6), and others (12.12%; n = 4). There was no difference in the age of the children who had accurate blood glucose logs as compared to those who had incorrect blood glucose logs [Table 2]. During follow-up over a period of 44 months, children with accurate blood glucose logs consistently had lower HbA1c as compared to children who had inaccurate blood glucose logs, which was statistically significant at 4, 16, 20, and 28 months of follow-up and approached statistical significance at 44 months of follow-up [Table 3]. The same is reflected in the proportion of children achieving HbA1c <7% and 7%-9% as compared to those who continued to have HbA1c >9% during follow-up [Table 4].
Table 2.
Glycemic control of type-1 diabetes mellitus children with accurate blood glucose profile as compared to those with inaccurate blood glucose profile
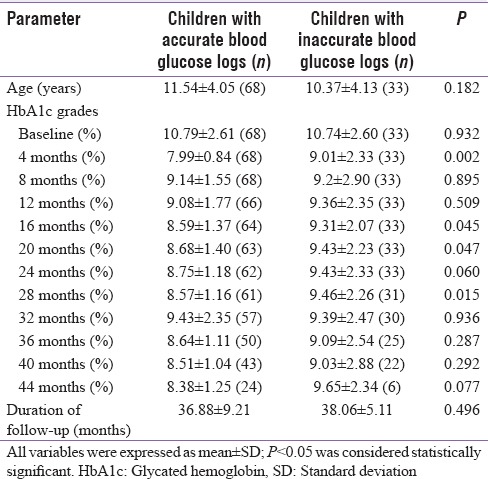
Table 3.
Glycemic control of type-1 diabetes mellitus children with different types of inaccurate blood glucose profile
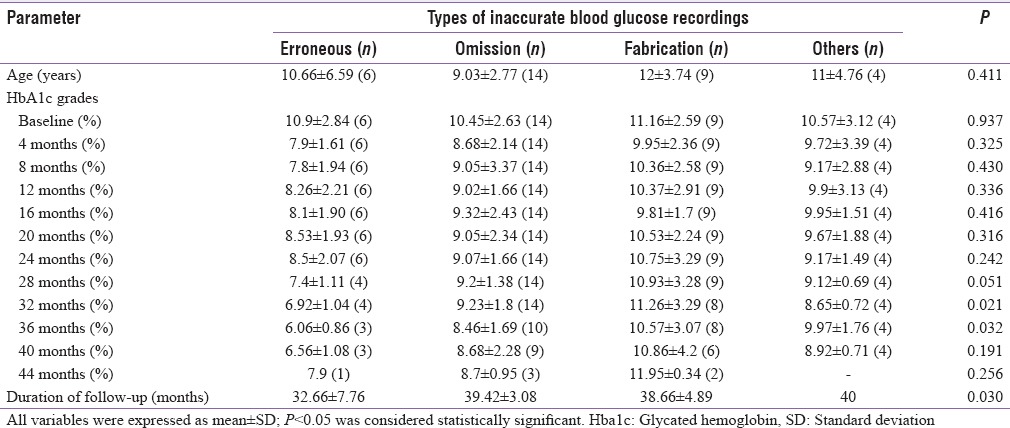
Table 4.
Profile of glycemic control of type-1 diabetes mellitus children with accurate blood glucose profile as compared to those with inaccurate blood glucose profile
On further detailed analysis of the types of inaccurate blood glucose logs, of the 14 patients who had omission of values in their logbooks, 9 had omission of high values only, 3 patients had omission of low values only, 1 had omission of both high and low values, while one patient even had omission of normal values. The three logbooks which had omissions of low values belonged to patients in the age of 4, 7, and 8 years, respectively, and were maintained by a caregiver, who was probably not informed of the hypoglycemic events. The logbooks that showed omissions of high values only belonged to children with age range from 6-12 years. Of these logbooks, 3 were maintained by parents, and the other 6 by the children themselves. In total, of the 14 cases of omission, 8 were attributed to caregivers and 6 to the children themselves.
Fabrication was the second most common type of error noted in 9 children. Parents were responsible for the fabrication in 2 of 9 instances, where the age of the child was 4 and 10 years, respectively. In the other 7 fabrication instances, it was the child responsible. All of these children were >10 years of age. Age was not significantly different among the children with different types of inaccurate blood glucose logs [Table 3]. Children with fabrication consistently had the highest HbA1c values among the different types of inaccurate blood glucose chartings, which was statistically significant at 32 and 36 months of follow-up [Table 3].
DISCUSSION
SMBG is an indispensable tool for the assessment of daily changes in blood glucose levels in all patients with diabetes. It is useful for modulating therapy, especially in patients who are on insulin. Studies have consistently shown that practicing SMBG per se leads to a significant improvement in glycemic control both in patients with T1DM and T2DM.[6,7] Studies have also demonstrated that patients who do SMBG regularly have a better sense of awareness of his disease state, feel more empowered, have lesser incidence of depression, and overall a beneficial effect on glycemic control.[8,9]
However, data on quality of SMBG done by patients are scant, especially in patients with T1DM from India. Our study highlighted that SMBG errors are common in children with T1DM at our center, observed in nearly one-third of the children. Fabrication and omission were the two most common types of SMBG errors noted in our study. One reason to explain this is that most of the children and/or parents in this study were illiterate or literate in vernacular language and had difficulty in reading Arabic numerals from the glucometers or for that matter, the column headings in the logbook. We have had instances where the code numbers displayed before test have been written down as values. The complex layout of the logbooks makes it difficult for entry if one is unable to read column headings. Poor record-keeping habits (not entering values immediately and attempting to do so at a later point in time relying on memory) are also important contributors to these errors. There is a need for designing glucometers to accommodate the needs of children in developing countries.[10]
Regarding the SMBG error of omission, it must be highlighted that a majority of the children were omitting out the higher blood glucose values only. The reason behind this behavior may be an attempt to downplay the out of range values and display a more positive, albeit false profile of glycemic state. Fear of reprimand from the family and/or treating doctor may have a role. Regarding the cause for SMBG error of omissions of only low glucose values, and this can partly be attributed to the cognitive impairment during a hypoglycemic episode and also the sense of urgency in correcting it. In our study, there were children who had not reported these episodes to the caregivers who were entering the values in the logbook. These problems highlight that as care givers, we need to be more patient and considerate with our children with T1DM, win their confidence, and get the fear/intimidation factor out of the doctor–patient relationship.
The findings of this study are in line with similar studies, which have examined the accuracy of blood glucose diaries with glucometers memory. Gonder-Frederick et al. in a study which looked at adults with T1DM found that the diaries were accurate in only 46.6% (14/30) patients.[11] Wilson and Endres also reported a fabrication rate of 40% and omission rate of 18% while studying 18 children with T1DM.[12]
Self-monitoring of glucose has been shown to be useful in improving glycemic control only when pattern analysis of the readings is done, and remedial measures are taken up.[13] The first step in recognizing patterns of dysglycemia is an orderly recording of the values and the relevant events around the reading.[14] In our study, the follow-up data of 44 months were interesting in that children with accurate blood glucose logs consistently had lower HbA1c as compared to children who had inaccurate blood glucose logs, which was statistically significant at 4, 16, 20, and 28 months of follow-up, and approached statistical significance at 44 months of follow-up [Table 2]. In addition, the proportion of children with HbA1c <7% and 7%–9% was also higher among children with accurate blood glucose logs as compared to those who had inaccurate blood glucose logs during follow-up. Thereby, it seems that to reap the benefits of SMBG in improving glycemic control, maintaining accurate and reliable logs of the reading is an important step. The reason for the HbA1c between the groups not reaching statistical significance in the other months mentioned could be attributable to the other variables that influence glycemic control such as intercurrent infections, adherence to insulin injections, dose titration, injection techniques, and eating patterns.
Innovative techniques such as the use of a detachable memory card or glucometers with USB ports from which data can be retrieved electronically by the treating doctor directly in the form of a timed chart or graph could give a better idea of any gross discrepancy between the actual and reported results. The task of manually entering values into logbooks can altogether be eliminated if such techniques are incorporated into the glucometer. In a study in which the adolescent participants were aware that their meters would be downloaded and compared to their verbal reports, this simple intervention alone halved the number of participants who misreported and reduced the total misreporting rate to 4.7% from 14%.[15]
In developing countries like India, there are some barriers unique to our situation. Since most glucometers display Arabic numerals, even patients who might be literate in the vernacular language may have trouble in reading and making sense of the readings. An option to display of values using vernacular numerals may be useful in patients with difficulty in reading Arabic numerals.
Thus, interpretation of SMBG from logbooks must be undertaken with the awareness that inaccuracy of reporting is rampant and hence using the glucometer's memory of recorded values to cross-check might be appropriate. Caregivers (doctors and nurses) should also devote time to assessing the quality of SMBG done in children during their visits to the clinic. This can further help in improving the glycemic control in children with T1DM.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Dutta D, Mukhopadhyay S. Intervening at prediabetes stage is critical to controlling the diabetes epidemic among Asian Indians. Indian J Med Res. 2016;143:401–4. doi: 10.4103/0971-5916.184281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.IDF Diabetes Atlas. 7th ed. Brussels, Belgium: International Diabetes Federation; 2015. [Last accessed 2016 Feb 12]. International Diabetes Federation. Available from: http://www.diabetesatlas.org . [Google Scholar]
- 3.American Diabetes Association. Children and adolescents. Sec. 11. In Standards of Medical Care in Diabetesd 2016. Diabetes Care. 2016;39(Suppl. 1):S86–93. [Google Scholar]
- 4.Ziegler R, Heidtmann B, Hilgard D, Hofer S, Rosenbauer J, Holl R. DPV-Wiss-Initiative. Frequency of SMBG correlates with HbA1c and acute complications in children and adolescents with type 1 diabetes. Pediatr Diabetes. 2011;12:11–7. doi: 10.1111/j.1399-5448.2010.00650.x. [DOI] [PubMed] [Google Scholar]
- 5.Polonsky WH, Jelsovsky Z, Panzera S, Parkin CG, Wagner RS. Primary care physicians identify and act upon glycemic abnormalities found in structured, episodic blood glucose monitoring data from noninsulin-treated type 2 diabetes. Diabetes Technol Ther. 2009;11:283–91. doi: 10.1089/dia.2008.0087. [DOI] [PubMed] [Google Scholar]
- 6.Zhu H, Zhu Y, Leung SW. Is self-monitoring of blood glucose effective in improving glycaemic control in type 2 diabetes without insulin treatment: A meta-analysis of randomised controlled trials. BMJ Open. 2016;6:e010524. doi: 10.1136/bmjopen-2015-010524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Murata T, Tsuzaki K, Yoshioka F, Okada H, Kishi J, Yamada K, et al. The relationship between the frequency of self-monitoring of blood glucose and glycemic control in patients with type 1 diabetes mellitus on continuous subcutaneous insulin infusion or on multiple daily injections. J Diabetes Investig. 2015;6:687–91. doi: 10.1111/jdi.12362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hortensius J, Kars MC, Wierenga WS, Kleefstra N, Bilo HJ, van der Bijl JJ. Perspectives of patients with type 1 or insulin-treated type 2 diabetes on self-monitoring of blood glucose: A qualitative study. BMC Public Health. 2012;12:167. doi: 10.1186/1471-2458-12-167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Russo GT, Scavini M, Acmet E, Bonizzoni E, Bosi E, Giorgino F, et al. The burden of structured self-monitoring of blood glucose on diabetes-specific quality of life and locus of control in patients with noninsulin-treated type 2 diabetes: The PRISMA study. Diabetes Technol Ther. 2016;18:421–8. doi: 10.1089/dia.2015.0358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Thukral A, Selvan C, Ghosh S, Chowdhury S. Glucometer for kids: What do we need? J Diabetes Sci Technol. 2013;7:1657–8. doi: 10.1177/193229681300700631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gonder-Frederick LA, Julian DM, Cox DJ, Clarke WL, Carter WR. Self-measurement of blood glucose. Accuracy of self-reported data and adherence to recommended regimen. Diabetes Care. 1988;11:579–85. doi: 10.2337/diacare.11.7.579. [DOI] [PubMed] [Google Scholar]
- 12.Wilson DP, Endres RK. Compliance with blood glucose monitoring in children with type 1 diabetes mellitus. J Pediatr. 1986;108:1022–4. doi: 10.1016/s0022-3476(86)80955-6. [DOI] [PubMed] [Google Scholar]
- 13.Riddle MC, Rosenstock J, Gerich J. Insulin Glargine Study Investigators. The treat-to-target trial: Randomized addition of glargine or human NPH insulin to oral therapy of type 2 diabetic patients. Diabetes Care. 2003;26:3080–6. doi: 10.2337/diacare.26.11.3080. [DOI] [PubMed] [Google Scholar]
- 14.Parkin CG, Davidson JA. Value of self-monitoring blood glucose pattern analysis in improving diabetes outcomes. J Diabetes Sci Technol. 2009;3:500–8. doi: 10.1177/193229680900300314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sjoeholm A, Gray A, Rayns J, Tomlinson PA, Wheeler BJ. Prior knowledge of blood glucose meter download improves the accuracy of verbal self-reported blood glucose in teenagers with type I diabetes at ski camp. Acta Diabetol. 2016;53:637–42. doi: 10.1007/s00592-016-0855-z. [DOI] [PubMed] [Google Scholar]


