Abstract
Objective:
We aimed to compare the diagnostic accuracy of 18F-Fluorocholine (FCH)-positron emission tomography/computed tomography (PET/CT) and four-dimensional (4D)- CT in detection and localization of eutopic and ectopic parathyroid adenoma (PA) in patients with hyperparathyroidism.
Materials and Methods:
Five patients with primary hyperparathyroidism underwent FCH-PET/CT after 60 min of 185 MBq of intravenous 18F-FCH administration. Images were acquired from head to mediastinum at 3 min per bed position. No intravenous contrast was used. All patients underwent 4D-CT within 2 weeks of the FCH-PET/CT, with a precontrast, post contrast arterial, and venous phase with 75 ml intravenous Iohexol 350 followed by 25 ml saline chase. Histopathology was considered as the gold standard.
Results:
Both modalities showed 100% concordance in the detection of parathyroid lesions. Both FCH-PET/CT and 4D-CT detected 7 lesions in 5 patients, with 4 patients having a single lesion, and 1 patient having three lesions. Of the 7 reported lesions, 4 were eutopic and 3 were ectopic. No additional lesions were detected by either modality in comparison to the other. All 7 specimens were resected and histopathology showed PA/hyperplasia.
Conclusion:
FCH-PET/CT and 4D-CT are equally efficacious in detection and localization of eutopic and ectopic PA. This may open up the possibility of using FCH-PET/CT in patients with negative conventional imaging who cannot undergo contrast studies.
Keywords: 18F-Fluorocholine positron emission tomography/computed tomography, four-dimensional computed tomography, parathyroid adenoma, primary hyperparathyroidism
INTRODUCTION
Hyperparathyroidism is a condition characterized by increased secretion of parathyroid hormone. It occurs mainly in two forms primary hyperparathyroidism (pHPT) and secondary hyperparathyroidism. Rarely, it can occur as a tertiary hyperparathyroidism in chronic renal failure patients. pHPT is a common endocrine disorder diagnosed mainly based on the biochemical parameters. It can present as an incidental finding, during biochemical screening of other clinical conditions or may manifest as constipation, psychiatric disturbances, fatigue, bone pain, and renal stones to a serious consequence of hypercalcemia. Parathyroid adenoma (PA) is the most common cause for pHPT comprising about 94%, out of which 90% may be solitary, and 4% may be multiple. Other causes include parathyroid hyperplasia (6%) and rarely parathyroid carcinoma (<1%).[1] Definitive treatment is surgical resection of parathyroid adenoma. Preoperative definite diagnosis and accurate localization of parathyroid gland with adenoma is of prime importance. Over a number of years, various functional and anatomical imaging modalities have evolved for preoperative localization of parathyroid adenoma. Most commonly used anatomical imaging is ultrasonography (USG). Usually, adenomas are hypoechoic and it can show cystic areas within. However, USG is associated with many limitations such as operator dependence, limited sensitivity for localization of ectopically located adenomas in the mediastinum, and difficulty in differentiating adenomas from lymph nodes and thyroid nodules.[2] Conventional modalities such as computed tomography (CT) and magnetic resonance imaging (MRI) can provide high-resolution images. The sensitivity of CT is 55.4%, and MRI is about 77% respectively for localization of parathyroid lesions.[3,4] However, it is difficult to differentiate adenomas from cervical lymph nodes, exophytic thyroid nodules, sarcoidosis, and neurofibromatosis which may lead to false positive findings. False negatives can be seen in small adenomas.
On the other hand, a major development in functional imaging was the use of 99m Tc-Sestamibi scintigraphy. It is based on the abnormal accumulation in PTA and differential washout from thyroid and parathyroid. It has moderate sensitivity even for detection of ectopic adenomas. However, smaller lesions can be missed on planar images due to its poor spatial resolution. The addition of single-photon emission computed tomography (SPECT)/CT helped in improving diagnostic accuracy and sensitivity up to 78.9%.[5,6] Newer techniques such as 4D-CT and 18F-Fluorocholine (FCH) positron emission tomography/CT (PET/CT) are the recent developments in this series of investigations. Four-dimensional-CT (4D-CT) imaging is primary based on acquiring images in three orthogonal planes (axial, coronal, and sagittal) with one noncontrast and three contrast phases. The contrast dynamics information is considered as the fourth dimension. Recently, 4D imaging of parathyroid has also been tried using MRI, but its role in this context is not adequately evaluated. 18F-FCH PET/CT is a relatively new functional imaging modality with respect to hyperparathyroidism with limited data in the literature. The parathyroid adenoma/hyperplasia show increased cell proliferation/metabolism and upregulation of choline kinase activity leading to enhanced choline uptake. Based on this possible mechanism 18F-Choline, a choline analog is used for evaluation of parathyroid adenoma. However, not much data are available on a comparison of this modality with another highly efficient imaging technique like 4D-CT. In this study, we aimed to compare the diagnostic accuracy of 18F-FCH PET/CT and 4D-CT in detection and localization of eutopic and ectopic parathyroid adenomas in patients with hyperparathyroidism.
MATERIALS AND METHODS
Patients
Inclusion criteria for this study were patients with clinical suspicion of hyperparathyroidism and with elevated PTH (defined as serum iPTH >54 pg/ml), raised serum calcium (defined as serum calcium >10.4 mg/dl), and low serum phosphorus (defined as serum phosphate <2.5 mg/dl) and patients with normal renal function as measured by a serum creatinine level <1.3 mg %. Patients with a history of chronic renal disease and serum creatinine >1.3 mg %, clinical setting of secondary/tertiary hyperparathyroidism were excluded from the study. Totally five patients fulfilling this criterion underwent 18F-FCH PET/CT and 4D-CT [Table 1]. Of 5 patients, 3 were males and 2 were females. The mean age of patients was 24.4 years (range 11–38 years). The serum creatinine ranged from 0.3 to 0.6 mg %, and parathyroid hormone level was in the range of 86.29–1021 pg/ml. Patient characteristics are elaborated in Table 1.
Table 1.
Demographic details and blood parameters

Imaging
All patients underwent 18F-FCH PET/CT after 60 min of 5 mCi (185 MBq) intravenous 18F- FCH administration. No intravenous contrast was used. Images from head to mediastinum (three-bed position) were acquired on Siemens Biograph mCT scanner (Siemens, Erlangen, Germany). PET imaging was done at 3–5 min per bed position and images were reconstructed with iterative reconstruction using OSEM algorithm. Final scans were interpreted by two nuclear medicine physicians independently, and consensus was sought in case of difference of opinion.
These patients also underwent 4D-CT within 2 weeks of the 18F-FCH PET/CT. The study was done on 256 slice Dual energy CT scanner (Definition Flash, Siemens, Erlangen, Germany). Initially, noncontrast CT from hyoid bone till sternal notch was acquired followed by arterial phase from angle of mandible till carina (Fixed delay of 25 s). Arterial phase was acquired in dual energy mode (100/140 kV and care dose 4D modulation enabled). Seventy-five milliliters of iodinated contrast at 4 ml/s followed by saline chase was used. Finally, venous phase was acquired from angle of mandible till carina with fixed delay of 80s. Images were interpreted by a single endocrine radiologist blinded to PET/CT findings. Postoperative histopathology was considered as gold standard.
RESULTS
Both18F-FCH PET/CT and 4D-CT detected 7 lesions in 5 patients [Table 2]. Out of these 5 patients, 4 patients had a single lesion and 1 patient had 3 lesions. Of 7 lesions, 4 lesions were detected at eutopic location while 3 lesions were ectopically located. Eutopically located adenomas were seen at right inferior (n = 3) and left superior location (n = 1). However, ectopically located adenomas were detected at (a) suprasternal region [Figures 1 and 2], (b) posterior to left sternocleidomastoid muscle, and (c) at submandibular region. No additional lesion was detected on either modality in comparison to the other. All 5 patients underwent surgical excision of the localized lesions at our institution. All the seven lesions could be respected and final histopathology showed 4 adenomas and 3 hyperplasia. Thus, the present study demonstrated 100% concordance between these two modalities in localization of parathyroid lesions.
Table 2.
Parathyroid adenoma location
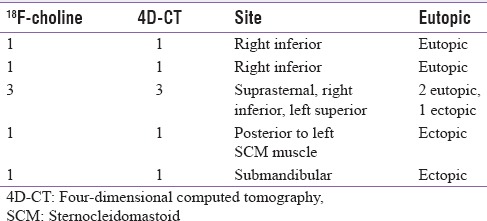
Figure 1.
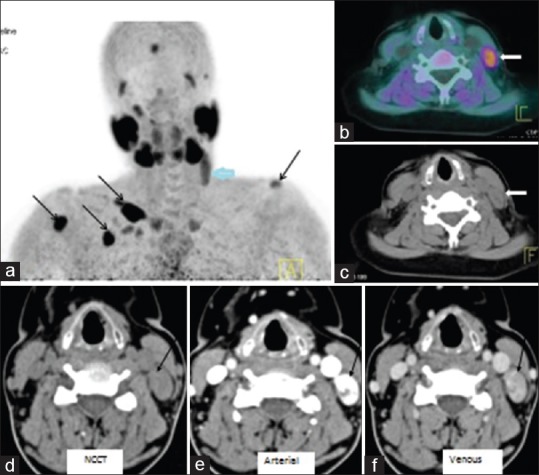
18F-fluorocholine positron emission tomography/computed tomography (a) MIP revealed focal radiotracer uptake in upper neck on the left side (thick arrow). In addition, multiple foci of increased fluorocholine uptake noted over left shoulder, chest wall and right arm regions (black arrows) corresponding to brown tumors. Fused positron emission tomography/computed tomography (b) and computed tomography (c) images showed soft tissue nodule in the left lateral neck, posterior to left sternocleidomastoid muscle (thick arrow). Four-dimensional – computed tomography (d-f) demonstrated an intensely enhancing lesion (arrow) on arterial phase with washout in venous phase posterior to the left jugular vein at thyroid cartilage level suggesting ectopically located PA
Figure 2.

18F-fluorocholine positron emission tomography/computed tomography (a) Maximum intensity image (MIP), showed focal fluorocholine uptake in lower neck in the region of suprasternal notch on the right side (thick arrow), (b and c) transaxial fused positron emission tomography/computed tomography and computed tomography images showed soft tissue density nodule in the region of right inferior parathyroid gland with focal increased fluorodeoxyglucose uptake. Four-dimensional computed tomography images (d-g) showing right inferior parathyroid adenoma (arrow) with intense enhancement on arterial phase and washout on venous phase
DISCUSSION
Overproduction of parathormone leads to pHPT which may manifest as psychiatric disturbances, renal stones, fatigue, constipation, and bone pain. These features are often nonspecific and can cause a delay in the diagnosis. Among the causes of pHPT, PTA is most common, followed by parathyroid hyperplasia and rarely parathyroid carcinoma.[1] Accurate preoperative localization of PTA is most important in the management of parathyroid adenoma. It enables minimally invasive parathyroid surgery to be performed with the use of smaller incisions and less complication rates instead of bilateral neck exploration which is associated with greater morbidity and complications such as hypoparathyroidism and recurrent laryngeal nerve palsy.
Usually, there are four parathyroid glands posterior to thyroid lobes, two on each side. The average size of an adenoma is around 1.5 cm[7] and thus requires high-resolution imaging modalities for localization. The superior parathyroid glands develop from the fourth branchial pouch along with thyroid gland and are located in relation to the thyroid gland. Inferior parathyroid glands, on the other hand, develop from the third branchial pouch along with thymus and can have variable location including in the mediastinum. This embryological origin necessitates the need for a modality with good sensitivity for detection of PTA located in the neck and in the mediastinum also. Many functional and anatomical modalities were studied in the evaluation of PTA. Functional imaging with 75Se-selenomethionine, 57Co-Vitamin B12, 131I-toluidine blue, and 123I-methylene blue is of little significance now. Further, 201 Tl – Thallous chloride in combination with pertechnetate was also used in recent past for parathyroid localization. 99m Tc-sestamibi is routinely performed for localization of parathyroid adenoma and addition of SPECT/CT improved its spatial resolution and sensitivity. Newer modalities such as 18F-FCH PET/CT and 4D-CT have also been recently evaluated in the localization of parathyroid adenoma.
18F-FCH has recently been reported as a possible novel PET agent for parathyroid localization preoperatively.[8,9,10,11,12,13,14] Increased cell proliferation/metabolism in the adenoma or hyperplasia possibly leads to increased choline uptake which on phosphorylation by choline kinase gets trapped to form a major membrane phospholipid called phosphatidylcholine. Hence, upregulation of choline kinase activity leads to enhanced choline uptake. Based on this possible mechanism 18F-choline, a choline analog is used for evaluation of parathyroid adenoma. Hodolic et al. and Cazaentre et al. have report edincidental parathyroidal uptake of 18F – choline.[9,10] Michaud et al.[11] conducted 18F-choline PET/CT on 12 patients with primary (n = 8) or secondary (n = 4) hyperparathyroidism. A per patient sensitivity of 92% (11/12 patients) and per lesion sensitivity of 89% (18 lesions total) was reported. One false positive and 2 false negatives were also reported. The study concluded that patients with hyperparathyroidism and with discordant or equivocal results on scintigraphy or on USG, adenomatous, or hyperplastic parathyroid glands can be localized by 18F-FCH PET/CT with good accuracy. Similarly, Orevi et al.,[12] have evaluated the role of 11C-choline PET/CT in localization of parathyroid adenomas. Preliminary results report that forty patients were recruited for this study. Out of 40 patients, 37 had positive findings while 3 patients were negative on 11C-choline PET/CT. Clear visualization of PTA was achieved in 33 of 37, whereas findings in 4 cases were suspicious for PTA. In 29 of 40 cases, choline and MIBI were concordant, but choline findings were clearer in 9 of these 29 studies.
In conclusion, choline PET/CT proved to be promising tool for PTA localization, providing clearer images than MIBI, equal or better accuracy, and quicker and easier acquisition. A pilot study by Lezaic et al.[13] compared 18F-FCH PET/CT with conventional 99 mTc – sestamibi. In total, 24 patients were with hyperparathyroidism were studied. The sensitivity of 92% and specificity of 100% was reported for 18F-FCH PET/CT compared to 64% sensitivity and 100% specificity for sestamibi scintigraphy.
Thus, 18F-FCH PET/CT a combination of functional and morphological imaging technique detects PTA with high sensitivity and accuracy. It also has added advantages over 11C-choline PET/CT that labeling with 18F which has a relatively longer half-life. This obviates the need of onsite cyclotron and also enables its supply and commercially availability to nearby PET/CT centers.
Role of 4D-CT in the localization of PTA also been evaluated in some studies.[15,16,17] The PTA shows unique contrast dynamics of intense arterial enhancement followed by venous washout.[4,5] Eichhorn-Wharry et al.[15] studied 135 consecutive patients who underwent preoperative sestamibi scanning, 4D-CT scanning, and parathyroidectomy for pHPT.
Their results revealed that 4D-CT scanning was significantly more accurate than sestamibi (73% vs. 62%, P = 0.016). In those with serum calcium levels < 10.8 mg/dL, 4D-CT scanning was significantly more accurate than sestamibi scanning for localization to a quadrant (45% vs. 29%, P = 0.013) and to a side (66% vs. 48%, P = 0.012). Furthermore, 4D-CT scanning was more accurate among patients with parathyroid gland weighing <500 mg (69% vs. 45%, P < 0.001). They concluded that 4D-CT provides better preoperative localization than sestamibi scanning, particularly in patients with mild hypercalcemia and smaller parathyroid adenomas. Chazen et al.[16] evaluated the accuracy of 4D-CT in 35 pathologically proven cases of PTA and hyperplasia who had preoperative 4D-CT were retrospectively reviewed. They found that of the 35 pathologically proven cases, 32 (sensitivity = 91%) patients were found positive for parathyroid disease using 4D-CT, including 3 cases of multigland disease. For lateralization of single-gland disease, 4D-CT demonstrated an accuracy of 93% and 4D-CT revealed a suboptimal sensitivity (44%), but 100% specificity, for multigland disease. A study concluded that 4D-CT demonstrated a high diagnostic accuracy for single and multigland disease and importantly, 4D-CT accurately lateralized single-gland adenomas in >90% of cases. In addition, 4D-CT showed a very high specificity for the detection of multigland disease. The advantages of this technique are, good spatial resolution, ability to differentiate thyroid nodules and lymph nodes from adenoma and detecting ectopic and multigland disease. These studies emphasize the importance of 4D-CT in accurate localization of PTA. Along with this it also gives information about vascularity of adenoma and anatomical details which would help in intraoperative localization and excision of PTA. However, the radiation dose of 4D-CT is relatively higher which is around 11–13 mSv.[4] Contraindication in patients with renal dysfunction and thus limited utility in patients with tertiary hyperparathyroidism is another limitation of this modality. Since 4D-CT was reported to be better than MIBI by few studies, we compared the role of F-Choline PET/CT with 4D-CT.
Although role of 18F-FCH PET/CT and 4D-CT have been evaluated separately, to the best of our knowledge, comparison of these two modalities in patients with PTA has not been published yet in the literature. In the present study, we compared these two modalities in the evaluation of parathyroid adenoma. Both 18F-FCH PET/CT and 4D-CT were equally accurate for detection of eutopically and ectopically located PTA with no discordance between them. These are initial results that we have and there are some limitations to this study. First, the number of patients in this study was less and therefore study with large sample size and long follow-up is required to validate our results. There is no long term follow-up available as of date to suggest complete recovery with no recurrence. This is important to ensure there are no false negative findings. Similarly, no false positive results were found in our study, larger studies may yield some different results since 18F-FCH uptake is known to be increased in various malignancies and some benign conditions as well. Another limitation of this study is that the exact incremental value of 18F-FCH PET/CT over Sestamibi is yet to be established, and a study is underway at our institution to assess the same. Thus, it remains to be seen if the use of 18F-FCH PET/CT can be routinely advisable.
CONCLUSION
Our initial results suggest that 18F-FCH PET/CT is comparable in performance to 4D-CT in pHPT, and may potentially have an added advantage in tertiary hyperparathyroidism in view of nonrequirement of IV contrast for the study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Ruda JM, Hollenbeak CS, Stack BC., Jr A systematic review of the diagnosis and treatment of primary hyperparathyroidism from 1995 to 2003. Otolaryngol Head Neck Surg. 2005;132:359–72. doi: 10.1016/j.otohns.2004.10.005. [DOI] [PubMed] [Google Scholar]
- 2.Johnson NA, Tublin ME, Ogilvie JB. Parathyroid imaging: Technique and role in the preoperative evaluation of primary hyperparathyroidism. AJR Am J Roentgenol. 2007;188:1706–15. doi: 10.2214/AJR.06.0938. [DOI] [PubMed] [Google Scholar]
- 3.Griffith B, Chaudhary H, Mahmood G, Carlin AM, Peterson E, Singer M, et al. Accuracy of 2-phase parathyroid CT for the preoperative localization of parathyroid adenomas in primary hyperparathyroidism. AJNR Am J Neuroradiol. 2015;36:2373–9. doi: 10.3174/ajnr.A4473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McDermott VG, Fernandez RJ, Meakem TJ, 3rd, Stolpen AH, Spritzer CE, Gefter WB. Preoperative MR imaging in hyperparathyroidism: Results and factors affecting parathyroid detection. AJR Am J Roentgenol. 1996;166:705–10. doi: 10.2214/ajr.166.3.8623655. [DOI] [PubMed] [Google Scholar]
- 5.Moka D, Voth E, Dietlein M, Larena-Avellaneda A, Schicha H. Technetium 99m-MIBI-SPECT: A highly sensitive diagnostic tool for localization of parathyroid adenomas. Surgery. 2000;128:29–35. doi: 10.1067/msy.2000.107066. [DOI] [PubMed] [Google Scholar]
- 6.Cheung K, Wang TS, Farrokhyar F, Roman SA, Sosa JA. A meta-analysis of preoperative localization techniques for patients with primary hyperparathyroidism. Ann Surg Oncol. 2012;19:577–83. doi: 10.1245/s10434-011-1870-5. [DOI] [PubMed] [Google Scholar]
- 7.Halenka M, Karasek D, Frysak Z. Four ultrasound and clinical pictures of parathyroid carcinoma. Case Rep Endocrinol. 2012;2012:363690. doi: 10.1155/2012/363690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Quak E, Lheureux S, Reznik Y, Bardet S, Aide N. F18-choline, a novel PET tracer for parathyroid adenoma? J Clin Endocrinol Metab. 2013;98:3111–2. doi: 10.1210/jc.2013-2084. [DOI] [PubMed] [Google Scholar]
- 9.Hodolic M, Huchet V, Balogova S, Michaud L, Kerrou K, Nataf V, et al. Incidental uptake of (18)F-fluorocholine (FCH) in the head or in the neck of patients with prostate cancer. Radiol Oncol. 2014;48:228–34. doi: 10.2478/raon-2013-0075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cazaentre T, Clivaz F, Triponez F. False-positive result in 18F-fluorocholine PET/CT due to incidental and ectopic parathyroid hyperplasia. Clin Nucl Med. 2014;39:e328–30. doi: 10.1097/RLU.0b013e3182a77b62. [DOI] [PubMed] [Google Scholar]
- 11.Michaud L, Burgess A, Huchet V, Lefèvre M, Tassart M, Ohnona J, et al. Is 18F-fluorocholine-positron emission tomography/computerized tomography a new imaging tool for detecting hyperfunctioning parathyroid glands in primary or secondary hyperparathyroidism? J Clin Endocrinol Metab. 2014;99:4531–6. doi: 10.1210/jc.2014-2821. [DOI] [PubMed] [Google Scholar]
- 12.Orevi M, Freedman N, Mishani E, Bocher M, Jacobson O, Krausz Y. Localization of parathyroid adenoma by 11C-choline PET/CT: Preliminary results. Clin Nucl Med. 2014;39:1033–8. doi: 10.1097/RLU.0000000000000607. [DOI] [PubMed] [Google Scholar]
- 13.Lezaic L, Rep S, Sever MJ, Kocjan T, Hocevar M, Fettich J. 18F-Fluorocholine PET/CT for localization of hyperfunctioning parathyroid tissue in primary hyperparathyroidism: A pilot study. Eur J Nucl Med Mol Imaging. 2014;41:2083–9. doi: 10.1007/s00259-014-2837-0. [DOI] [PubMed] [Google Scholar]
- 14.Michaud L, Balogova S, Burgess A, Ohnona J, Huchet V, Kerrou K, et al. A pilot comparison of 18f-fluorocholine PET/CT, ultrasonography and 123i/99mtc-sestamibi Dual-phase Dual-isotope scintigraphy in the preoperative localization of hyperfunctioning parathyroid glands in primary or secondary hyperparathyroidism: Influence of thyroid anomalies. Medicine (Baltimore) 2015;94:e1701. doi: 10.1097/MD.0000000000001701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Eichhorn-Wharry LI, Carlin AM, Talpos GB. Mild hypercalcemia: An indication to select 4-dimensional computed tomography scan for preoperative localization of parathyroid adenomas. Am J Surg. 2011;201:334–8. doi: 10.1016/j.amjsurg.2010.08.033. [DOI] [PubMed] [Google Scholar]
- 16.Chazen JL, Gupta A, Dunning A, Phillips CD. Diagnostic accuracy of 4D-CT for parathyroid adenomas and hyperplasia. AJNR Am J Neuroradiol. 2012;33:429–33. doi: 10.3174/ajnr.A2805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mekel M, Linder R, Bishara B, Kluger Y, Bar-On O, Fischer D. 4-dimensional computed tomography for localization of parathyroid adenoma. Harefuah. 2013;152:710–2. [PubMed] [Google Scholar]


