Abstract
Background:
There is a paucity of data on knowledge, awareness, and practices (KAP) of patients with hypothyroidism in India.
Aims and Objectives:
To study the KAP and adherence to treatment of participants with primary hypothyroidism.
Materials and Methods:
An observational cross-sectional study was conducted in Endocrinology Outpatient Department of Maharaja Agrasen Hospital, Punjabi Bagh, New Delhi. Two-fifty consecutive primary hypothyroidism participants, aged ≥18 years, who were on treatment for at least 3 months responded to a structured questionnaire, to assess their KAP about the disease and adherence to treatment.
Results:
A total of 250 patients completed the questionnaire. The mean age of the participants was 43.24 ± 10.80 years; with majority being females (85.6%). The median duration of hypothyroidism was 8 years (range: 3–10). Most were well educated, with 53.6% being graduates/postgraduates. Knowledge and awareness related to hypothyroidism was poor in majority of participants. Only 35.2% and 51.2% knew correct meaning of the terms “thyroid” and “hypothyroidism” respectively. Only 25.6% participants knew correctly that thyroxine (T4) is used to replace and normalize blood levels of thyroid hormone. Forty percent had false dietary beliefs in the context of hypothyroidism. Ten percent participants felt T4 can be stopped once laboratory reports return to normal. Only 36.4% participants knew correctly that T4 need to be continued during pregnancy. Many participants (30.4%) believed hypothyroidism can lead to weight gain in excess of 10 kg. Regarding adherence, 90.4% participants were adherent to T4, 2.4% were moderately adherent, and remaining 7.2% participants were nonadherent to T4.
Conclusion:
A large number of patients with primary hypothyroidism lack basic knowledge about disease and have dietary and treatment-related prejudices and poor treatment adherence. Public health measures are required to improve KAP in patients with primary hypothyroidism.
Keywords: Compliance, hypothyroidism, knowledge, awareness, practices, patient education
INTRODUCTION
Hypothyroidism denotes deficient production of thyroid hormone by the thyroid gland and can be primary (abnormality in thyroid gland itself) or secondary/central (as a result of hypothalamic or pituitary disease). Primary hypothyroidism is the etiology in approximately 99% of cases of hypothyroidism. The term subclinical hypothyroidism is used to define that grade of primary hypothyroidism, in which there is an elevated thyroid-stimulating hormone (TSH) concentration in the presence of normal serum free thyroxine (T4) and triiodothyronine concentrations.[1]
The worldwide prevalence of spontaneous overt hypothyroidism is between 1% and 2% and ten times more common in women than in men while approximately 8% of women and 3% men have subclinical hypothyroidism.[2] The disease seems equally or more common in the Indian scenario. The prevalence of overt hypothyroidism has been reported between 3.5% and 4.2% while subclinical hypothyroidism has been reported in 8.02%–19.3% of population in various studies across India.[3,4]
Hypothyroidism has profound impact on health and well-being. Globally, thyroid disorders continue to be common yet one of the most under-diagnosed and neglected chronic health conditions.[5,6] Patient's knowledge and awareness about the disease and its treatment is very important for good long-term outcome and compliance in any chronic disease. Studies have shown the importance of improving patient's knowledge through education and associated benefits of improving compliance with health-care appointments and medications for patients with hypertension and diabetes[7,8] although such data are scarce in the context of hypothyroidism. Such studies on hypothyroidism can help the physician to concentrate on specific issues during their first interaction with the patients as well as during follow-up.
There is a paucity of data on the knowledge, awareness, and practices (KAP) among the primary hypothyroidism patients in the Indian population. The present study was planned to assess KAP and adherence of treatment of patients with primary hypothyroidism who have been diagnosed and receiving treatment for at least 3 months and visited our center for the first time.
MATERIALS AND METHODS
An observational cross-sectional study was conducted in the Outpatient Department of Endocrinology Clinic at Maharaja Agrasen Hospital, Punjabi Bagh, New Delhi, a 400-bedded teaching, superspecialty, National Accreditation Board for Hospitals and Healthcare Providers and Joint Commission International Accredited Hospital. The study was approved by the Institutional Ethics Committee.
Consecutive subjects of primary hypothyroid with age ≥18 years, who were on treatment for at least 3 months and visited our center first time, were invited to participate in the study. The study was conducted during July 2015–October 2016. The patients, who gave informed written consent, were subjected to the questionnaire. Newly diagnosed patients, hypothyroidism secondary to pituitary/hypothalamic diseases, radioiodine ablation, surgery, neck irradiation, and drugs were excluded. Pediatric patients <18 years of age and patients with transient hypothyroidism were also excluded. Patients with significant mental retardation, who were otherwise incapable of answering questionnaires, were also excluded from the study.
A structured questionnaire was used to collect information on demographic parameters and to check subjects' KAP with respect to hypothyroidism and adherence of treatment. The questionnaire covered demographic parameters of study participants including their education level, duration of hypothyroidism, baseline TSH at diagnosis; current dose of levo-T4, current level of TSH if available, self-reported other comorbid medical conditions. The questionnaire covered issues such as meaning of medical terms “thyroid,” and “hypothyroidism,” patient's knowledge about the basis of the treatment, monitoring during treatment, correct method of medication intake and belief in alternative medications, common beliefs and misconceptions about hypothyroidism, and common symptoms perceived by patients related to hypothyroidism. Adherence to T4 therapy was assessed by asking the patients the number of doses missed in the last 1 month and was categorized as follows:[9]
Adherent to treatment: Missed <5% dose in the last 1 month
Moderately adherent to treatment: Missed ≥5% but <15% dose in the last 1 month
Nonadherent to treatment: Missed ≥15% dose in the last 1 month.
Statistical analysis
Categorical variables were presented in number and percentage (%), and continuous variables were presented as mean ± standard deviation. Quantitative variables were compared using unpaired t-test between males and females. P < 0.05 was considered statistically significant. The data were entered into MS Excel spreadsheet, and analysis was done using Statistical Package for Social Sciences (SPSS) (Chicago, Illinois, USA) version 21.0 software.
RESULTS
A total of 250 participants completed the questionnaire. The baseline demographic parameters of participants are summarized in Table 1. Two hundred and fourteen (85.6%) participants were female. The mean age of the participants was 43.24 ± 10.80 years. Majority of participants belonged to the age group between 41 and 50 years (30.4%). Median duration of hypothyroidism was 8 years (range: 3–10 years). Median baseline TSH at diagnosis was 13.10 mIU/L (range: 3–20.8). The mean current dose of levo-T4 was 81.60 ± 2.37 μg. Common associated comorbidities in these respondents were diabetes mellitus (24.8%) and hypertension (23.6%). Majority of participants were well educated, with 53.6% being graduates/postgraduates [Table 2].
Table 1.
Demographic parameter of study population
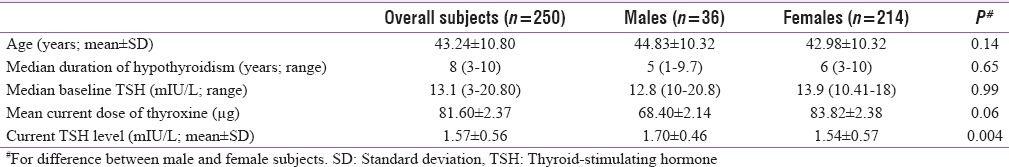
Table 2.
Education level of study participants (n=250)

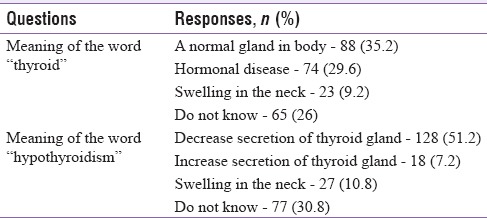
Regarding knowledge of terminologies, out of 250, only 88 (35.2%) participants were aware of correct meaning of the term “thyroid” [Table 3]. Similarly, only 128 (51.2%) participants were aware about correct meaning of the term “hypothyroidism.” Forty-five (18%) participants referred to “hypothyroidism” as a swelling in the neck or increased hormone production by the thyroid gland. Only 64 (25.6%) participants knew correctly that T4 is used to replace and normalize the blood level of thyroid hormone.
Table 3.
Knowledge of terminologies related to thyroid of the study participants
Symptoms perceived related to hypothyroidism by study participants were weight gain (93.6%), easy fatigability (80%), irregular menstrual cycle (65.2%), infertility (55.6%), constipation (51.2%), excessive hair fall (41.2%), and skin problems (38%). However, most participants believed that primary hypothyroidism can cause enormous weight gain. Nearly 11.6% participants believed that it can result in weight gain >15 kg while another 18.8% believed that maximum weight gain can be between 10 and 15 kg.
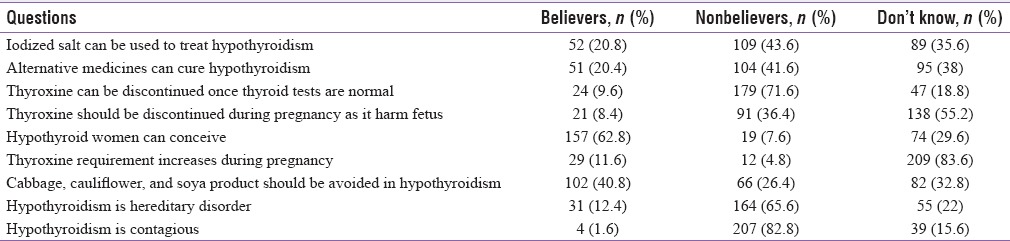
Beliefs of study participants related to disease, its treatment and dietary precautions in the context of hypothyroidism are summarized in Table 4. Regarding treatment, 20.4% participants believed that alternative therapy can cure hypothyroidism; while 20.8% believed that iodized salt can be used to treat hypothyroidism. A large number of participants (40.8%) believed that cabbage, cauliflower, and soya products should be avoided by patients with hypothyroidism. 9.6% participants felt that T4 can be stopped once lab reports return to normal level while 18.8% participants did not have any idea for same. Regarding conception, 7.6% participants thought that hypothyroid women cannot conceive, 62.8% thought they can conceive, while remaining 29.6% were not sure about it. Only 36.4% participants knew correctly that T4 needs to be continued during pregnancy. A fair number of participants (22.8%) did not follow the correct method of T4 administration with respect to meal; 20.4% participants were not keeping minimum 30 min gap between T4 and meal; while 2.4% were taking T4 either with meals or after meals. Only 62.2% participants answered TSH as single best test for monitoring of treatment of primary hypothyroidism. Regarding adherence, 90.4% participants were adherent to T4, 2.4% were moderately adherent, and remaining 7.2% participants were nonadherent to T4.
Table 4.
Study participants’ common beliefs regarding hypothyroidism
DISCUSSION
This observational cross-sectional study was conducted to assess the KAP and adherence to treatment in patients with primary hypothyroidism from a tertiary care teaching hospital in New Delhi. Knowledge and awareness about the disease among the patients is very important for better long outcome for any chronic disease. Our study shows that a large number of patients with primary hypothyroidism lack basic knowledge about the disease; fairly large number of patients have dietary as well as treatment-related false beliefs. There is a significant deficit regarding adherence to treatment.
There are limited studies regarding KAP among hypothyroid patients in India. Kannan et al. did a pilot study of 34 hypothyroid patients from Chennai, South India, to assess the KAP among these patients.[10] Singh et al. from Meerut did KAP study of 200 patients with thyroid swelling who attended cytology clinic at their institution.[11] Perumal et al. reported one cross-sectional study of 100 hypothyroid patients to assess their existing hypothyroidism related knowledge, health-seeking behavior, and health literacy among these patients.[12] Rai et al. reported one community-based cross-sectional study of 250 females of age group 18–50 years from different areas of Indore city of Madhya Pradesh belonging to different socioeconomic status and occupation to assess their knowledge about thyroid disorders, in this study only 20% females had either personal or family history of thyroid disorders.[13]
In our study, regarding the meaning of medical term “thyroid,” only 35.2% participants knew correctly that thyroid is a normal gland in the body, 29.6% considered thyroid as a hormonal disease, 9.2% as a swelling in the neck, and the remaining 26% did not have any idea about it. Only 51% knew that “hypothyroidism” is a clinical term for reduced secretion by thyroid gland, 11% participants thought hypothyroidism as a swelling in the neck, and 18% regarded it as increased secretion by thyroid gland, and remaining 31% had no idea regarding the same. In Kannan et al. study, 79.41% and 55.88% participants knew correct meaning of the terms “thyroid” and “hypothyroidism,” respectively. Similarly, in a study by Singh et al., 60% patients knew the correct meaning of the term “thyroid.” Knowledge of disease-related basic terminologies is very important for patients to acquire further knowledge regarding their disease.
In our study, only 25.6% participants knew correctly that T4 is used to replace and normalize the blood level of thyroid hormone while 36% participants considered it as means to stimulate thyroid gland to work normally. Others considered that T4 was a drug to reduce neck swelling or for weight reduction. Compared to this, in study by Kannan et al., 50% patients were aware that T4 is given to replace and normalize blood level of thyroid hormone. Regarding treatment in our study, 9.6% participants felt that thyroid medication can be stopped once laboratory reports return to normal while 71.6% thought otherwise and the remaining 18.8% had no idea regarding the same. Similarly, 8.4% patients felt that thyroid medication should be stopped during pregnancy as it can harm the fetus, 36.4% did not feel so and remaining 53.4% had no idea about same. In study by Kannan et al., 32.35% patients felt that thyroid medication should be stopped once laboratory reports return to normal and 26.47% patients believed that thyroid medications should be stopped during pregnancy.
Among alternative medication use, 20.4% participants believed that alternative medicines such as Ayurveda, Yoga, Unani, Siddha, and Homeopathy can cure hypothyroidism. Our results are comparable to the previous studies, 20.58% and 35% participants with hypothyroidism had faith in alternative medications in studies by Kannan et al. and Singh et al., respectively. Among other misconceptions, 20.8% patients believed that hypothyroidism can be treated using iodized salt corresponding figures were much higher in a study by Kannan et al. (55.88%) and Singh et al. (58.5%). Inappropriate knowledge regarding treatment leads to poor outcome of chronic diseases such as hypothyroidism. In India, large number of patients often discontinues T4, presenting with severe hypothyroid state. Considerable time needs to be spent in explaining the patient about the lifelong nature of the illness, need for long-term medication, and regular follow-up.
In our study, 62.8% participants believed that hypothyroid female patients can conceive while 7.6% believed that hypothyroid women cannot conceive and rest 29.6% were not sure about it. Hypothyroidism is a common cause of infertility which can be easily managed by correcting the hypothyroid state.[14] Inadequate knowledge about pregnancy and hypothyroidism has created a certain amount of blemish in the minds of patients and their relatives, which leads to mental trauma as well as social differences in relationships, especially among young females. This needs to be addressed not only just by patient education at the level of physician but also at a social level in the form of awareness campaigns involving mass education.
Symptoms perceived related to hypothyroidism by participants were weight gain (93.6%), easy fatigability (80%), irregular menstrual cycle (65.2%), infertility (55.6%), constipation (51.2%), excessive hair fall (41.2%), skin problems (38%), and sore throat/neck pain (35%). Patients commonly tend to attribute any symptom pertaining to neck (commonly sore throat) to their thyroid gland. Patients should be educated about various symptoms of thyroid disorders. The various misconceptions held by patients with respect to weight gain attributable to hypothyroidism are of clinical importance. It is well known that primary hypothyroidism does not cause an increase in weight gain of more than 3–5 kg. However, in our study, 11.6% participants believed that it can result in weight gain ≥15 kg while another 18.8% believed that weight gain can be between 11 and 15 kg. A study by Kannan et al. and Singh et al. also showed that a significant number of subjects believed that hypothyroidism causes excessive weight gain and obesity. However, in the previous studies, patient's perception about quantitative weight gain in hypothyroidism was not assessed. Physicians should always clarify to patients that hypothyroidism generally causes mild weight gain (<5 kg) and should lay emphasis on the importance of diet and exercise for weight loss.
Among dietary misconceptions, 40.8% believed in dietary restrictions such as avoiding cabbage, cauliflower, and soya products. Kannan et al. study results were almost similar to our study where 38.23% subjects believed in dietary restriction of cabbage, cauliflower, and soya products. In our study, 97.6% participants used to take T4 empty stomach in the morning while remaining 2.4% were taking it either with or after meal. Almost 20.4% participants were not keeping minimum advised gap of 30 min between T4 ingestion and meals. Regarding adherence, 90.4% participants were adherent to T4, 2.4% were moderately adherent, and remaining 7.2% participants were nonadherent to T4.
It is well known that thyroid disease is not a major cause of mortality. However, hypothyroidism can contribute to morbidity from osteoporosis, hypercholesterolemia, cardiovascularm, and neuropsychiatric diseases. Better knowledge and awareness regarding the disease in primary hypothyroid patients can significantly improve compliance of treatment and decrease the associated morbidity. In addition, this can further help even make patients spread correct facts and information regarding the disease to their relatives and friends in the society.[15] There are a lot of factors contributing to lack of knowledge among patients in our country. Lack of qualified physicians, less time spent by doctors on patient education because of high patient burden, lack of awareness, and not using available electronic media are some of them. Lot of awareness is still required at physician level in developing countries like India for optimum management of hypothyroid patients.[16] In addition, there is urgent need for endocrine nurses/counselors or dieticians who understand thyroidology and can spend time with patients explaining about their disease and its treatment.
CONCLUSION
Our study showed significant caveats in knowledge and awareness about the disease and its treatment in patients with primary hypothyroidism. In addition, a large number of patients had dietary as well as treatment-related misconceptions. There is a significant deficit regarding adherence to treatment. Public health measures are required to improve knowledge and awareness regarding the disease in patients with primary hypothyroidism.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Khandelwal D, Tandon N. Overt and subclinical hypothyroidism: Who to treat and how. Drugs. 2012;72:17–33. doi: 10.2165/11598070-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 2.Vanderpump MP, Tunbridge WM, French JM, Appleton D, Bates D, Clark F, et al. The incidence of thyroid disorders in the community: A twenty-year follow-up of the Whickham Survey. Clin Endocrinol (Oxf) 1995;43:55–68. doi: 10.1111/j.1365-2265.1995.tb01894.x. [DOI] [PubMed] [Google Scholar]
- 3.Marwaha RK, Tandon N, Ganie MA, Kanwar R, Sastry A, Garg MK, et al. Status of thyroid function in Indian adults: Two decades after universal salt iodization. J Assoc Physicians India. 2012;60:32–6. [PubMed] [Google Scholar]
- 4.Kalra S, Kumar A, Jarhyan P, Unnikrishnan AG. Indices of thyroid epidemiology. Indian J Endocrinol Metabol. 2015;19:844–7. doi: 10.4103/2230-8210.167543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kalra S, Unnikrishnan AG, Sahay R. The global burden of thyroid disease. Thyroid Res Pract. 2013;10:89–90. [Google Scholar]
- 6.Kalra S, Unnikrishnan AG, Baruah MP. Thyroid: Disorders of a lesser gland. Thyroid Res Pract. 2013;10:45–6. [Google Scholar]
- 7.Heisler M, Pietee JD, Spencer M, Kieffer E, Vijan S. The relationship between knowledge of recent HbA1c values and diabetes care understanding and self management. Diabetes Care. 2005;28:816–22. doi: 10.2337/diacare.28.4.816. [DOI] [PubMed] [Google Scholar]
- 8.Williams MV, Baker DW, Parker RM, Nurss JR. Relationship of functional health literacy to patients' knowledge of their chronic disease. A study of patients with hypertension and diabetes. Arch Intern Med. 1998;158:166–72. doi: 10.1001/archinte.158.2.166. [DOI] [PubMed] [Google Scholar]
- 9.Mithal A, Dharmalingam M, Tewari N. Are patients with primary hypothyroidism in India receiving appropriate thyroxine replacement? An observational study. Indian J Endocrinol Metab. 2014;18:83–8. doi: 10.4103/2230-8210.126582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kannan S, Mukundan L, Mahadevan S, Sathya A, Kumaravel V, Bhat RV, et al. Knowledge, awareness and practices (KAP) among patients with hypothyroidism attending endocrine clinics of community hospitals in Chennai. Thyroid Res Pract. 2010;7:11–5. [Google Scholar]
- 11.Singh A, Sachan B, Malik NP, Sharma VK, Verma N, Singh CP. Knowledge, awareness and practices (KAP) among patients with thyroid swelling attending Cytology Clinic in a Medical College, Meerut. Sch J Appl Med Sci. 2013;1:793–5. [Google Scholar]
- 12.Perumal SS, Prasad S, Surapaneni KM, Joshi A. Health information-seeking behavior among hypothyroid patients at Saveetha Medical College and Hospital. Ethiop J Health Sci. 2015;25:147–54. doi: 10.4314/ejhs.v25i2.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rai S, Sirohi S, Khatri AK, Dixit S, Saroshe S. Assessment of knowledge and awareness regarding thyroid disorders among women of a cosmopolitan city of central India. Natl J Community Med. 2016;7:219–22. [Google Scholar]
- 14.Davis LB, Lathi RB, Dahan MH. The effect of infertility medication on thyroid function in hypothyroid women who conceive. Thyroid. 2007;17:773–7. doi: 10.1089/thy.2007.0065. [DOI] [PubMed] [Google Scholar]
- 15.Nimmy NJ, Aneesh PM, Narmadha MP, Udupi RH, Binu KM. A survey on the prevalence of thyroid disorder induced by demography and food habits in South Indian population. Indian J Pharm Pract. 2012;5:49–52. [Google Scholar]
- 16.Surana V, Aggarwal S, Khandelwal D, Singla R, Bhattacharya S, Chittawar S, et al. A 2016 clinical practice pattern in the management of primary hypothyroidism among doctors from different clinical specialties in New Delhi. Indian J Endocrinol Metab. 2017;21:165–77. doi: 10.4103/2230-8210.196012. [DOI] [PMC free article] [PubMed] [Google Scholar]


