Abstract
Background:
Magnesium (Mg) is the 4th most common mineral and the 2nd most abundant intracellular cation in the body. It plays major roles in various physiological activities and has been implicated in many disease states.
Aim:
The aim of this study was to study the patterns and correlates of serum Mg in cohorts of type 2 diabetic patients in Nigeria.
Subjects and Methods:
One hundred and twenty-five patients comprising 63 with type 2 diabetes mellitus (T2DM) alone and 62 with diabetes and hypertension (HT) were compared with fifty controls matched for sex and age. Basic data, HbA1c, and fasting blood glucose (FBG) were obtained while serum Mg was measured by colorimeter. Relationship between serum Mg and glucose control was considered while serum Mg < 1.6 mg/dl was considered as hypomagnesemia.
Results:
The mean serum Mg of all patients was 2.06 ± 0.49 mg/dl, not statistically different from controls at 2.22 ± 0.48 mg/dl. About ¼ (23.2%) of the patients had hypomagnesemia which was significantly more than 12% of controls. Although the patients with diabetes and HT were older and more of females than those with DM alone, the mean serum Mg was comparable (2.03 ± 0.49 vs. 2.09 + 0.50 mg/dl). Twenty-seven percent (27%) of patients who had DM alone was more than 19.3% with HT and diabetes combined. Whereas the FBG was comparable in patients with hypomagnesemia and normal serum Mg, HbA1c was significantly higher in the hypomagnesemia group (8.39 ± 0.98 vs. 6.75 ± 1.22%, P = 0.021).
Conclusion:
Hypomagnesemia is common in T2DM outpatients occurring approximately one in four patients. It is associated with poor long-term control.
Keywords: Control, diabetes, glucose, hypertension, magnesium, Nigeria
INTRODUCTION
Although magnesium (Mg) remains the 4th most common mineral and the 2nd most abundant intracellular divalent cation in the body, its study, clinical application, and relevance remain in the background when compared with other minerals such as sodium, calcium, or potassium.[1,2] Only about 1% of it is in the blood, its residence being mainly in the bones and organs.[1]
It plays major roles in physiological activities of the body including normal nerve and muscle function, cardiac excitability, and insulin metabolism. Its deficiency has consequently been associated with chronic diseases such as migraine, hypertension (HT), and type 2 diabetes mellitus (T2DM).[3] The foods highest in Mg include unrefined whole grains, spinach, nuts, and tubers.[3,4] The recommended dietary reference intake is about 301–420 mg/day, <60% of people in USA consume this amount.[5]
Mg plays a role in glucose and insulin metabolism through tyrosine kinase activity. It transfers phosphate from ATP to proteins. It also releases glucose-1-phosphate from glycogen thereby affecting the phosphorylase b activity. It directly affects glucose transporter protein activity 4 thereby helping to regulate glucose translocation into cells.[3] In HT, it is involved in blood pressure (BP) regulation by hindering calcium depolarization and release of nitric oxide leading to vascular relaxation.[6]
The normal serum Mg is about 1.6–2.5 mg/dl. The prevalence of hypomagnesemia ranges from 13.5% to 47.7% in T2DM patients.[7,8] In a recent Indian study, the prevalence of serum Mg <1.6 mg/dl was put at 11.3%.[9] Hypomagnesemia has been implicated in various disease states including migraines, headaches, HT, cardiovascular diseases, stroke, and T2DM.[2] However, it is its role in T2DM and metabolic syndrome that has been most studied.
Prospective studies have shown that those with higher Mg intake are 10%–47% less likely to develop T2DM.[10] In intervention studies, Mg supplement has been shown to improve insulin sensitivity in diabetic and obese patients and even in experimental animals.[2,11,12] Hypomagnesemia has also been postulated as a factor that increase gastrointestinal transit time in both normal and diabetic animals.[13]
This study seeks to investigate the pattern of serum Mg in our cohorts of T2DM patients. It also seeks to correlate the effects of hypomagnesemia in control of diabetes mellitus.
SUBJECTS AND METHODS
One hundred and twenty-five patients comprising 63 with T2DM alone and 62 with diabetes and HT who gave informed consent were recruited into the study from the outpatient clinics and medical wards of our hospital. They were compared with fifty normal controls who were sex and age matched. Those on loop diuretics or taking any Mg supplement were excluded from the study. Basic data were obtained and the HbA1c and the fasting blood glucose (FBG) were obtained while serum Mg was measured by colorimetry. Serum Mg <1.6 mg/dl was considered to be hypomagnesemia.
Ethical approval was obtained from our Institution Board and study conformed to the Declaration of Helsinki.
Statistical data were analyzed by SPSS window 20. Continuous variables were expressed as mean ± standard deviation while categorical variables were expressed as percentages. Groups were compared by the Student's t-test. P <0.05 was considered statistically significant.
RESULTS
The study subjects consisted of 125 patients with T2DM of whom 62 were also hypertensive. They were compared with fifty normal controls.
The mean serum Mg of all the diabetic subjects was 2.06 ± 0.49 mg/dl though this tended to be lower than 2.22 ± 0.48 for the control subjects, which did not reach statistical significance [Table 1]. There were 29 (23.2%) subjects with hypomagnesemia which was significantly more than 6 (12.0%) in the controls. The patients with diabetes had higher body mass index and lower serum triglyceride than the control subjects. Furthermore, more diabetics tended to take alcohol than the controls. All the other parameters were comparable in both groups.
Table 1.
Demographic characteristics of all study subjects
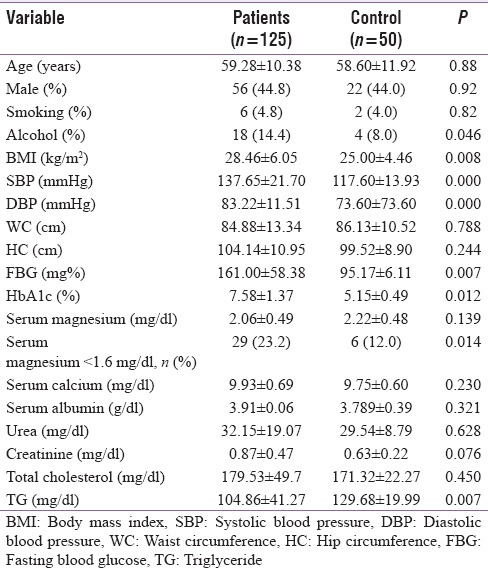
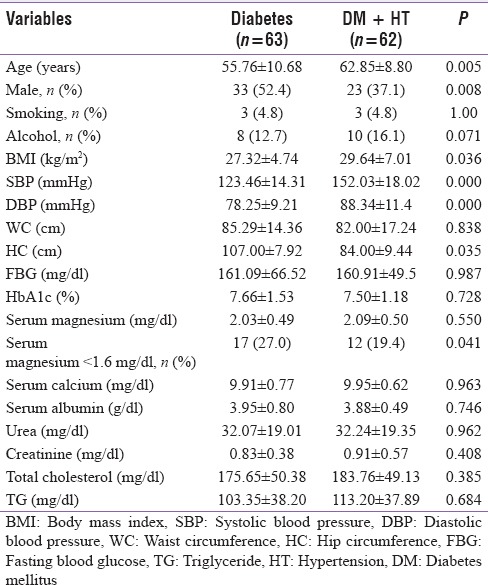
Table 2 compares the patients with only T2DM with those who had both diabetes and HT. There were about equal number of patients in both groups. The patients with diabetes and HT were older, more of females, and had higher body mass index. The mean serum Mg at 2.03 ± 0.49 and 2.09 ± 0.50 was not significantly different. They were both within normal limits. Seventeen (27.0%) patients with diabetes alone who had hypomagnesemia were significantly more than 19.3% of patients with diabetes and HT. The hip circumference was significantly more in patients with diabetes alone. All other parameters except those directly related to HT were comparable.
Table 2.
Comparison between the patients with diabetes alone and diabetes with hypertension
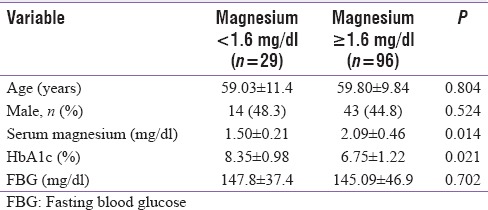
When the 29 patients with hypomagnesemia were compared with the 96 with normal serum Mg, there was no difference in the sex distribution and mean ages [Table 3]. The HbA1c was higher in patients with low Mg (8.39% ±0.98% vs. 6.75% ±1.22%, P = 0.021). The FBG was, however, comparable in both groups. The serum Mg in the hypomagnesemia group was 1.50 ± 0.21 mg/dl while the normal cohort was 2.09 ± 0.46 mg/dl, P = 0.024.
Table 3.
Comparison of the patients with hypomagnesemia and normal serum magnesium
DISCUSSION
The mean serum Mg in the diabetic patients in this study is comparable and within normal limits as that of the controls. However, more diabetic patients had hypomagnesemia when compared with the controls. Many studies have confirmed this finding,[3,8,9] with deleterious consequences. Dasgupta et al. noted that apart from poor glycemic control, hypomagnesemia is associated with retinopathy, nephropathy, and foot ulcers.[9]
The prevalence of hypomagnesemia at 23.2% is comparable with the general trend at 13.5%–47.7% study is similar to the finding of Dasgupta et al.[10] The prevalence of hypomagnesemia in normal controls in this study is comparable with the Swiss study but much higher than a Bangladesh study in which the prevalence was about 6%.[8,14]
A tendency for Mg deficiency in diabetic patients is well established. Changes in serum Mg levels may have a bearing on diabetic comorbidities and complications with strong association with obesity, HT, and diabetic retinopathy.[15] Guerrero-Romero et al. in a review of 681 healthy individuals reported that dietary Mg intake but not obesity or overweight is the one that is associated with hypomagnesemia and concluded that hyperglycemia might be a cause of hypoglycemia in nondiabetic individuals.[16] A meta-analysis of 34 trials involving 2028 participants, Zhang et al. reported that 368 mg of supplemental Mg daily for 3 months will lower systolic BP by 2 mmHg and diastolic BP by 1.78 mmHg. This effect is most pronounced in those with severe hypomagnesemia.[17] In another review of 31,876 participants, higher consumption of Mg is associated with lower risks of developing metabolic syndrome. The authors, however, cautioned that the association between serum Mg and metabolic syndrome though significant is heterogeneous and requires further confirmation.[18]
The causes of hypomagnesemia are multifactorial. They include poor intake of food rich in Mg and osmotic diuresis leading to high Mg excretion. Insulin resistance which may affect intracellular Mg transport may cause increased extracellular Mg loss and reduced tubular Mg reabsorption. Other causes include frequent use of loop and thiazide diuretics and also diabetic autonomic neuropathy.[9,19] Sodium-glucose cotransporter 2 acts in proximal nephron blocking glucose reabsorption and could account for increasing Mg urinary loss during osmotic diuresis thereby worsening hypomagnesemia.
Approximately half of the T2DM patients were also adjudged hypertensive, a figure slightly lower than the Swiss study.[14] It is known that many diabetic patients if they live long enough will develop elevated BP. This study revealed that patients with T2DM and HT were older than those with diabetes alone. Development of HT on already established diabetes does not seem to confer tendency to developing hypomagnesemia. There were more patients with hypomagnesemia who had only diabetes than those with diabetes and HT combined.
This study revealed that long-term diabetes control as demonstrated by HbA1c was better in patients with normal serum Mg though FBG did not differ. Many studies have demonstrated poorer control in T2DM patients with hypomagnesemia[8,9,20] while some did not experience this effect.[14] FBG is a spot analysis of glycemic control, unlike HbA1c, and did not show any difference in this study. HbA1c depicts long-term control while FBG shows short-term control, it is possible that Mg as a cofactor has more influence on long-term rather than short-term control. This will require further work. Furthermore, insulin early phase secretion increases after glucose load which is absent in fasting state, hence effect on postprandial.
The limitation of this study includes the relatively small sample size and measurement of serum Mg as an indication of the body Mg. Serum Mg has been observed to be the least sensitive of estimating total body Mg status except in severe deficiency as compared with ionized Mg, red blood cell Mg, or urinary Mg by the Mg loading test.[21] However, our focus in this study is not total body Mg but serum Mg. Whereas it is well recognized that parathyroid hormone (PTH) may have modulatory effects on Mg metabolism, this was not particularly considered in this study and constituted a limitation. It has, however, been observed that suppression of intact PTH (iPTH) can result from severely decreased total body Mg with clinical features of neuromuscular irritability due primarily to hypocalcemia and Mg therapy alone has been shown to correct hypocalcemia secondary to iPTH suppression.[22]
We did not also set out to investigate the details of Mg excretion in these patients; this is also a limitation which could be addressed in further work.
CONCLUSION
The conclusion of this study is that hypomagnesemia is common in our T2DM patients occurring approximately in 1 in 4 patients. It is associated with poor long-term glycemic control.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Elin RJ. Magnesium: The fifth but forgotten electrolyte. Am J Clin Pathol. 1994;102:616–22. doi: 10.1093/ajcp/102.5.616. [DOI] [PubMed] [Google Scholar]
- 2.Pham PC, Pham PA, Pham SV, Pham PT, Pham PM, Pham PT. Hypomagnesemia: A clinical perspective. Int J Nephrol Renovasc Dis. 2014;7:219–30. doi: 10.2147/IJNRD.S42054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Volpe SL. Magnesium in disease prevention and overall health. Adv Nutr. 2013;4:378S–83S. doi: 10.3945/an.112.003483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.US Department of Agriculture. Agriculture Research Service 2011. USDA National Nutrient Database for Standard Reference Release 24. Nutrient Data Laboratory Home PAGE. Available from: http://www.ars.usda.gov/ba/bhnrc/ndl .
- 5.Nielsen FH. Magnesium, inflammation, and obesity in chronic disease. Nutr Rev. 2010;68:333–40. doi: 10.1111/j.1753-4887.2010.00293.x. [DOI] [PubMed] [Google Scholar]
- 6.Paolisso G, Barbagallo M. Hypertension, diabetes mellitus, and insulin resistance: The role of intracellular magnesium. Am J Hypertens. 1997;10:346–55. doi: 10.1016/s0895-7061(96)00342-1. [DOI] [PubMed] [Google Scholar]
- 7.Pham PC, Pham PM, Pham SV, Miller JM, Pham PT. Hypomagnesemia in patients with type 2 diabetes. Clin J Am Soc Nephrol. 2007;2:366–73. doi: 10.2215/CJN.02960906. [DOI] [PubMed] [Google Scholar]
- 8.Azad KM, Sutradhar SR, Khan NA, Haque MF, Sumon SM, Barman TK, et al. Serum magnesium in hospital admitted diabetic patients. Mymensingh Med J. 2014;23:28–34. [PubMed] [Google Scholar]
- 9.Dasgupta A, Sarma D, Saikia UK. Hypomagnesemia in type 2 diabetes mellitus. Indian J Endocrinol Metab. 2012;16:1000–3. doi: 10.4103/2230-8210.103020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dong JY, Xun P, He K, Qin LQ. Magnesium intake and risk of type 2 diabetes: Meta-analysis of prospective cohort studies. Diabetes Care. 2011;34:2116–22. doi: 10.2337/dc11-0518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hruby A, Meigs JB, O'Donnell CJ, Jacques PF, McKeown NM. Higher magnesium intake reduces risk of impaired glucose and insulin metabolism and progression from prediabetes to diabetes in middle-aged Americans. Diabetes Care. 2014;37:419–27. doi: 10.2337/dc13-1397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Abayomi AI, Adewoye EO, Olaleye SB, Salami AT. Effect of Magnesium pre-treatment on alloxan induced hyperglycemia in rats. Afr Health Sci. 2011;11:79–84. [PMC free article] [PubMed] [Google Scholar]
- 13.Adewoye EO, Ige AO. Effect of magnesium on gastrointestinal transit time in normal and diabetic rats: Possible mechanism of action. Afr J Med Med Sci. 2012;41:373–8. [PubMed] [Google Scholar]
- 14.Wälti MK, Zimmermann MB, Spinas GA, Hurrell RF. Low plasma magnesium in type 2 diabetes. Swiss Med Wkly. 2003;133:289–92. doi: 10.4414/smw.2003.10170. [DOI] [PubMed] [Google Scholar]
- 15.Sharma A, Dabla S, Agrawal RP, Barjatya H, Kochar DK, Kothari RP. Serum magnesium: An early predictor of course and complications of diabetes mellitus. J Indian Med Assoc. 2007;105:16, 18, 20. [PubMed] [Google Scholar]
- 16.Guerrero-Romero F, Flores-García A, Saldaña-Guerrero S, Simental-Mendía LE, Rodríguez-Morán M. Obesity and hypomagnesemia. Eur J Intern Med. 2016;34:29–33. doi: 10.1016/j.ejim.2016.06.015. [DOI] [PubMed] [Google Scholar]
- 17.Zhang X, Li Y, Del Gobbo LC, Rosanoff A, Wang J, Zhang W, et al. Effects of magnesium supplementation on blood pressure: A meta-analysis of randomized double-blind placebo-controlled trials. Hypertension. 2016;68:324–33. doi: 10.1161/HYPERTENSIONAHA.116.07664. [DOI] [PubMed] [Google Scholar]
- 18.Sarrafzadegan N, Khosravi-Boroujeni H, Lotfizadeh M, Pourmogaddas A, Salehi-Abargouei A. Magnesium status and the metabolic syndrome: A systematic review and meta-analysis. Nutrition. 2016;32:409–17. doi: 10.1016/j.nut.2015.09.014. [DOI] [PubMed] [Google Scholar]
- 19.Barbagallo M, Dominguez LJ. Magnesium metabolism in type 2 diabetes mellitus, metabolic syndrome and insulin resistance. Arch Biochem Biophys. 2007;458:40–7. doi: 10.1016/j.abb.2006.05.007. [DOI] [PubMed] [Google Scholar]
- 20.Ramadass S, Basu S, Srinivasan AR. SERUM magnesium levels as an indicator of status of diabetes mellitus type 2. Diabetes Metab Syndr. 2015;9:42–5. doi: 10.1016/j.dsx.2014.04.024. [DOI] [PubMed] [Google Scholar]
- 21.Arnaud MJ. Update on the assessment of magnesium status. Br J Nutr. 2008;99(Suppl 3):S24–36. doi: 10.1017/S000711450800682X. [DOI] [PubMed] [Google Scholar]
- 22.Mutnuri S, Fernandez I, Kochar T. Suppression of parathyroid hormone in a patient with severe magnesium depletion. Case Rep Nephrol. 2016;2016:2608538. doi: 10.1155/2016/2608538. [DOI] [PMC free article] [PubMed] [Google Scholar]


