Abstract
Aim
Little is known about the amount of physical parent–infant closeness in neonatal intensive care units (NICUs), and this study explored that issue in six European countries.
Methods
The parents of 328 preterm infants were recruited in 11 NICUs in Finland, Estonia, Sweden, Norway, Italy and Spain. They filled in daily diaries about how much time they spent in the NICU, in skin‐to‐skin contact (SSC) and holding their babies in the first two weeks of their hospitalisation.
Results
The parents' NICU presence varied from a median of 3.3 (minimum 0.7–maximum 6.7) to 22.3 (18.7–24.0) hours per day (p < 0.001), SSC varied from 0.3 (0–1.4) to 6.6 (2.2–19.5) hours per day (p < 0.001) and holding varied from 0 (0–1.5) to 3.2 (0–7.4) hours per day (p < 0.001). Longer SSC was associated with singleton babies and more highly educated mothers. Holding the baby for longer was associated with gestational age. The most important factor supporting parent–infant closeness was the opportunity to stay overnight in the NICU. Having other children and the distance from home to the hospital had no impact on parent–infant closeness.
Conclusion
Parents spent more time in NICUs if they could stay overnight, underlining the importance that these facilities play in establishing parent–infant closeness.
Keywords: Family‐centred care, Kangaroo care, Preterm infants, Single‐family room parent–infant closeness, Skin‐to‐skin care
Abbreviations
- NICU
Neonatal intensive care unit
- PICU
Paediatric intensive care unit
- SSC
Skin‐to‐skin contact
Key notes.
Little is known about the amount of physical parent–infant closeness in neonatal intensive care units (NICUs), and this study explored that issue in six European countries.
The parents' presence ranged from a few hours per day to almost 24 hours, and skin‐to‐skin contact ranged from an average of half an hour to nine hours per day.
Allowing parents to stay overnight in NICUs was the most important factor in establishing parent–infant closeness.
Introduction
The developing brain of a preterm infant, and its developmental outcome, is affected by their environment. The natural environment for a newborn infant is close to their caregiver, which is ensured by the many biological mechanisms that contribute to the bond and attachment between the mother and her newborn child 1. The formation of this bond is at risk in preterm infants, and physical separation almost invariably occurs because neonatal intensive care units (NICUs) traditionally limit the presence of parents 2. However, supporting the parents' presence in the neonatal unit may improve the long‐term prognosis of preterm infants 3.
Skin‐to‐skin contact (SSC) is one of the first ways for parents to be part of their infants’ care and provides physical closeness 4, and it is feasible and safe, even for very immature infants 5, 6, 7. SSC has been shown to promote breastfeeding, infant growth and development, infant–parent relationships and parental well‐being 8. However, restrictions on SSC and holding are common in NICUs 9 and contribute to parental stress 10.
Parents' presence and parent–infant physical closeness, including SSC and holding, are part of evidence‐based neonatal care. However, little is known about how well this evidence is implemented in clinical practice. The aim of this study was to find out whether there were any differences in the amount of physical parent–infant closeness between European NICUs, and we examined potential factors that explained the differences. We hypothesised that there would be differences in the amount of parent–infant closeness, as defined by the parents' presence in the unit, SSC and holding their infant.
Patients and methods
The International Closeness Survey was conducted in 11‐level II‐IIIc NICUs in six European countries as a part of research carried out by the Separation and Closeness Experiences in Neonatal Environment (SCENE) Study Group from September 2013 to August 2014. SCENE is a multidisciplinary group of international professionals who are undertaking research to identify, construct, implement and evaluate best practices in supporting physical and emotional parent–infant closeness during neonatal care (https://www.utu.fi/scene).
The units participating in the International Closeness Survey were in Finland (Turku), Estonia (Tallinn and Tartu), Sweden (Danderyd, Huddinge and Uppsala), Norway (Bergen, Drammen and Tromso), Italy (Como) and Spain (Madrid). The study protocol was approved by the boards of ethics of all the participating hospitals or countries.
About the units
The units were different in size, case mix and level of care, as defined by American Academy of Pediatrics 11 (Table 1). The units reported the barriers for SSC. In addition, the overnight facilities for parents who wanted to stay were organised differently. The parents were allowed to stay in all of the neonatal units for 24 hours, except for the two paediatric intensive care units (PICUs) in Estonia. In this study, we defined an opportunity to stay in the unit as the presence of either a single‐family room or a ‘bed‐in‐the‐unit’ or most of the families in the unit. A single‐family room was defined as a private room for the infant that included at least one bed for a parent in the same room. A ‘bed‐in‐the‐unit’ was defined as a bed that was available for the parents outside the infant's room, but inside the unit. The main features are described as follows.
Table 1.
Unit characteristics
| Turku | Uppsala | Danderyd | Huddinge | Tallinn MH | Tartu MH | Como | Madrid | Drammen | Bergen | Tromsø | Indicated by gray | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Tallinn PICU | Tartu PICU | |||||||||||
| Tallinn stepdown unit | Tartu stepdown unit | |||||||||||
| Level of care | III B | III B | IIIA | III B | IIIA | II | III A | III C | III A | III B | III B | |
| IIIB | IIIC | |||||||||||
| II | II | |||||||||||
| Admissions per year | 638 | 414 | 1031 | 646 | 479 | 411 | 210 | 401 | 468 | 326 | >500 | |
| 150 | 135 | 935 | ||||||||||
| 598 | 412 | |||||||||||
| Opportunity to stay overnight in the unit | No | Yes | Yes | Yes | Yes | Yes | No | No | Yes | No | No | Yes |
| No | No | |||||||||||
| Yes | Yes | |||||||||||
| Single‐family rooms | 1 | 11 | 12 | 15 | 10 | 6 | 2 | 0 | 15 | 3 | 2 | <50% |
| 0 | 0 | |||||||||||
| 4–10 | 8 | |||||||||||
| Permanent beds for parents in infant's room | 0 | 20 (100) | 12 (86) | 15 (100) | 0 | 0 | 0 | 0 | 17 (100) | 0 | 3 (20) | 100% |
| 0 | 0 | |||||||||||
| 10 (100) | 0 | |||||||||||
| Other beds in the unit for parents | 1 | 20 | 24 | 30 | 14 | 0 | 0 | 0 | 30 | 0 | 6 | 100% |
| 0 | 0 | |||||||||||
| 25 | 18 | |||||||||||
| Beds outside the unit for parents | 4 | 4 | 4 | 0 | 0 | 0 | 6 | 0 | 0 | 8 | 20 | |
| 0 | 9 | |||||||||||
| 0 | 0 | |||||||||||
| Barrier for skin‐to‐skin contact always or frequently | Chest tube | Ventilator, chest tube | UC, CPAP, lack of privacy, unit daily routine | Ventilator, chest tube, PT | Ventilator, chest tube, UC, arteria, PT | Ventilator, chest tube | ||||||
| Arterial line, CPAP | UC, Arterial line, unit daily routine |
MH = Maternity hospital; PICU = Paediatric intensive care unit; UC = Umbilical catheter; PT = Phototherapy.
The highlighted grey colour is explained in the last column.
In Turku, Finland, the NICU was located in the maternity hospital and provided care until discharge to home. During the study year, the unit only had one family room that was used for an overnight stay before the infant was discharged. The parents had reclining chairs available throughout the stay.
In Uppsala, Sweden, the NICU was located in the maternity hospital. Intensive care was provided in rooms that were divided into four sections, which each included the infant's space and a bed for a parent. When intensive care was not indicated, the infants were cared for in single‐family rooms where parents were encouraged to stay around the clock.
The NICUs in the Danderyd and Huddinge hospitals in the Stockholm area of Sweden were located in the maternity hospital and provided care until the infants were discharged home. Parents had sleeping facilities that were adjacent to the infants’ beds during intensive care. From the point of delivery, mothers and their preterm infants received couplet care, which means they were cared for together 12. Reclining chairs were available for the parents throughout the stay. When intensive care was not indicated, the infants were cared for in single‐family rooms, where the parents were encouraged to stay around the clock.
In Tallinn and Tartu, Estonia, the infants were treated in three separate units. All newborns requiring long‐term assisted ventilation or neonatal surgery were transferred from the maternity hospitals to the PICUs. After initial care at the maternity hospital or intensive care, the infant was transferred to the step‐down unit, which provided the longest periods of care. The PICUs provided reclining chairs for the parents. At the maternity hospitals and step‐down units, the parents had the opportunity to stay overnight, and there were reclining chairs for the parents in the infants’ rooms. There were a limited number of single‐family rooms for stable infants and a separate room in the unit where the mothers of other infants could stay.
At the Sant'Anna Hospital in Como, Italy, the NICU was located in the maternity hospital and provided care until the infant was discharged home. There were no overnight facilities for parents inside the unit, but there were reclining chairs close to the infant's bed.
In the Hospital Gregorio Marañón in Madrid, Spain, the NICU was located in the maternity hospital and provided care until the infants were discharged home. Intensive care and step‐down care were provided in separate rooms. There were no facilities for parents to stay overnight inside the unit, but there was one reclining chair and one normal chair provided for the parents of each infant.
The NICUs in Drammen, Bergen and Tromso were located in the maternity hospitals and provided care until the infants were discharged home. Drammen provided single‐family rooms for all families, where the parents were encouraged to stay around the clock, Tromso had two single‐family rooms, and Bergen did not provide facilities for parents to stay overnight inside the unit.
Parent–infant characteristics
All the parents of preterm infants born below 35 gestational weeks who were admitted were prospectively approached about participation until the predetermined number of 30 families per unit was reached or the recruitment process had lasted one full year. Families were excluded if they did not understand any of the nine study languages: Estonian, English, Finnish, Hungarian, Italian, Norwegian, Russian, Swedish or Spanish. We also excluded mothers who had delivered triplets, or more babies, or if the infant who was admitted was likely to die. Parents were given oral and written information about the study. The data collection started as soon as was appropriate after the signed informed consent was obtained, and by the sixth day of life at the latest.
A log was kept of all the eligible families to evaluate the dropout rate. The log included the patient's gestational age, birthweight, length of hospital stay and distance from the hospital to home.
The parents filled in a questionnaire about the infant and parent characteristics. The infant characteristics included gestational age, birthweight, birth head circumference, sex, mode of delivery, any need for incubator care, whether the infant was a singleton or twin and whether they had any siblings. The parental characteristics included their age, education, socio‐economic situation and the distance from the hospital to their home (Table S1).
Parental closeness diary
Physical closeness data were collected using a parental closeness diary (Fig. 1), which was filled in by the parents. The diaries were kept in a closed folder next to the infant's bed. The parents were asked to fill in the diaries for two weeks after recruitment. If the infant was still at the hospital at one month of age, the families were asked to fill in an extra week of diaries. Physical closeness was divided into three categories: the amount of time parents were present in the NICU, the duration of SSC and how long the parents spent holding their infant. The presence was defined as parents being inside the neonatal unit. SSC was defined as the baby lying on the parent's bare chest dressed only in a diaper and maybe a cap. Holding was defined as the baby being in the parent's arms, away from the incubator, cot or bed.
Figure 1.
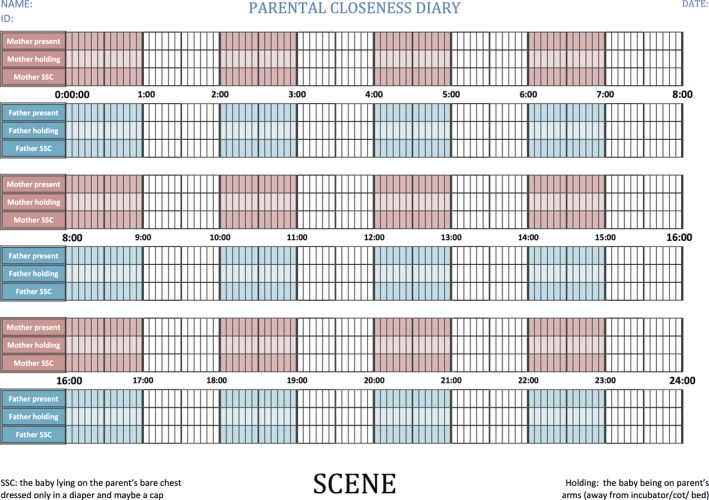
Parental closeness diary. One page corresponded to 24 hours with six timelines: mother present, mother skin‐to‐skin contact (SSC), mother holding, father present, father SSC and father holding.
Statistical methods
The response variables – duration of presence, holding and SSC – are presented as medians or mean values per day for each unit. We first calculated the mean value for each infant using the first two weeks of diaries and then the mean value of each unit using the mean values of the infants. This strategy was chosen to give every infant the same weight in the final analysis, regardless of the number of days with diary entries during the first two weeks. When we compared the units, the mean values of the two infants were used for twin pairs.
The background variables included a number of infant characteristics: gestational age, birthweight, birth length, birth head circumference, sex, singleton versus twin, mode of delivery and duration of care in an incubator. They also included a number of parental characteristics: the mother's and father's age, language, education and socio‐economic status, whether they had one or more children living at home, whether one or more of the mother's or father's previous children had been admitted to the NICU, if the family owned a car and whether the parents lived together or not (Table S1) Because of the large number of explanatory variables, only background variables with a univariate connection of p < 0.10 were included in the multifactorial analyses. The excluded factors were the infant's sex, whether the family owned a car and whether a previous child of the mother or father had been admitted to a NICU.
A paired sample t‐test was used to compare the units with the opportunity to stay overnight to the other units. A logistic regression analysis was used to study the associations between the parents’ presence, holding the infant, SSC and background variables controlling for the unit. Univariate associations between continuous background variables and the neonatal units were studied using linear models. Binary background variables were compared between the neonatal units using logistic regression, and ordinal background variables were compared between the neonatal units using cumulative logit models. Generalised linear models with negative binomial distribution and log link were used to study the association between the response variables, namely the parents’ presence, holding the infant and SSC, and predictor variables of the unit and background factors. A paired sample t‐test was used to compare the duration of the parental presence, holding and SSC at two time points. Statistical analyses were carried out using SAS for Windows version 9.4 (SAS Institute Inc., Cary, NC, USA). p‐Values below 0.05 were considered statistically significant.
Results
The parents of 328 infants were recruited (Fig. 2), and they included 103 twins, as one twin died. The families who were not approached did not differ in gestational age or in travelling time from home to hospital, but a higher birthweight increased the possibility of not being recruited in the study, with a odds ratio (OR) of 1.05 (p = 0.02). There were no differences in the background factors of the families who agreed and declined to participate.
Figure 2.
Flow chart of the patient recruitment process and the reasons for dropout.
Parent–infant closeness data are presented from the infant's perspective, namely how much either mother or father was present and how much they engaged in SSC or held the infant during the first two weeks of life (Table 2). There were wide variations between the units with regard to the parents’ median and minimum and maximum presence: the longest duration was a median of 22.3 (18.7–24.0) hours per day in Huddinge, Sweden, and the shortest duration was 3.3 (0.7–6.7) hours in Como, Italy (p < 0.001). The six units that provided parents with the opportunity to stay overnight recorded a longer duration for the parents’ presence than the other units, with a mean of 19.7 hours and a standard deviation (SD) of 5.3 versus 5.5 hours and an SD of 2.6 hours (p < 0.001) (Fig. 3A). There were also wide variations among the units in terms of SSC: the longest duration was a median of 6.6 (2.2–19.5) hours per day in Uppsala, Sweden, and the shortest was 0.3 (0–1.4) hours per day in Tartu, Estonia (p < 0.001 hours). The duration of SSC in the six units that offered parents the opportunity to stay overnight was a mean 4.00 hours (SD 4.51) compared to 1.74 hours (SD 1.54) in the other units (p < 0.001) (Fig. 3C). The amount of time that parents spent holding the infant ranged from a median of 3.2 (0–14.3) hours per day in Drammen, Norway, to 0 (0–1.0) hours in Uppsala, Sweden (p < 0.001). The duration of holding in the six units that provided parents with an opportunity to stay overnight was a mean of 1.81 hours (SD 2.08) compared to 1.49 hours (SD 1.84) in the other units (p = 0.15) (Fig. 3B).
Table 2.
The amount mother's or father's presence, holding and skin‐to‐skin contact (SSC) during the first two weeks of life
| Unit | Variable | N | Mean | SD | Min | Q1 | Median | Q3 | Max |
|---|---|---|---|---|---|---|---|---|---|
| Turku | Presence | 41 | 6.04 | 1.87 | 2.25 | 4.72 | 5.81 | 7.54 | 10.61 |
| Holding | 41 | 1.33 | 1.52 | 0.00 | 0.00 | 0.78 | 1.94 | 4.97 | |
| SSC | 41 | 2.20 | 1.21 | 0.19 | 1.03 | 2.39 | 2.98 | 4.72 | |
| Uppsala | Presence | 31 | 14.77 | 5.82 | 5.14 | 8.58 | 15.81 | 20.72 | 23.13 |
| Holding | 31 | 0.10 | 0.26 | 0.00 | 0.00 | 0.00 | 0.00 | 1.01 | |
| SSC | 31 | 8.86 | 6.09 | 2.17 | 3.47 | 6.63 | 16.57 | 19.49 | |
| Danderyd | Presence | 20 | 21.40 | 3.40 | 12.69 | 19.90 | 22.87 | 24.00 | 24.00 |
| Holding | 20 | 0.29 | 0.52 | 0.00 | 0.00 | 0.00 | 0.29 | 1.49 | |
| SSC | 20 | 8.01 | 2.92 | 1.80 | 6.46 | 7.93 | 9.96 | 13.75 | |
| Huddinge | Presence | 23 | 22.43 | 1.58 | 18.67 | 21.50 | 22.30 | 24.00 | 24.00 |
| Holding | 23 | 1.71 | 1.98 | 0.00 | 0.25 | 0.94 | 2.75 | 7.64 | |
| SSC | 23 | 3.83 | 2.56 | 0.63 | 1.93 | 3.13 | 5.07 | 10.41 | |
| Tallinn | Presence | 37 | 21.51 | 4.50 | 1.14 | 22.22 | 22.86 | 23.14 | 24.00 |
| Holding | 37 | 2.51 | 1.71 | 0.00 | 1.10 | 2.16 | 3.38 | 7.28 | |
| SSC | 37 | 1.05 | 1.00 | 0.00 | 0.22 | 0.64 | 1.77 | 3.58 | |
| Tartu | Presence | 31 | 17.48 | 6.55 | 0.64 | 14.06 | 20.80 | 22.44 | 23.34 |
| Holding | 31 | 2.21 | 2.32 | 0.00 | 0.43 | 1.47 | 3.67 | 10.09 | |
| SSC | 31 | 0.31 | 0.32 | 0.00 | 0.04 | 0.27 | 0.43 | 1.36 | |
| Como | Presence | 34 | 3.41 | 1.50 | 0.65 | 2.49 | 3.25 | 4.42 | 6.68 |
| Holding | 34 | 1.51 | 1.66 | 0.00 | 0.22 | 0.80 | 2.66 | 6.11 | |
| SSC | 34 | 0.49 | 0.62 | 0.00 | 0.00 | 0.26 | 0.72 | 1.99 | |
| Madrid | Presence | 39 | 4.95 | 1.92 | 1.78 | 3.65 | 4.37 | 6.13 | 9.18 |
| Holding | 39 | 0.95 | 1.22 | 0.00 | 0.00 | 0.13 | 2.28 | 3.54 | |
| SSC | 39 | 1.48 | 1.02 | 0.00 | 0.83 | 1.22 | 2.20 | 4.23 | |
| Drammen | Presence | 34 | 21.19 | 3.21 | 13.05 | 19.33 | 22.32 | 23.76 | 24.00 |
| Holding | 34 | 3.19 | 2.32 | 0.00 | 1.13 | 3.17 | 4.70 | 7.38 | |
| SSC | 34 | 3.90 | 3.05 | 0.00 | 1.36 | 3.21 | 5.51 | 14.29 | |
| Bergen | Presence | 30 | 7.06 | 3.04 | 0.00 | 5.33 | 7.17 | 8.96 | 13.79 |
| Holding | 30 | 2.40 | 2.74 | 0.00 | 0.00 | 1.30 | 5.32 | 7.79 | |
| SSC | 30 | 2.47 | 2.08 | 0.00 | 0.73 | 2.21 | 3.48 | 8.16 | |
| Tromso | Presence | 8 | 9.21 | 2.75 | 4.97 | 6.77 | 9.94 | 11.23 | 12.81 |
| Holding | 8 | 1.60 | 1.70 | 0.17 | 0.27 | 0.83 | 3.00 | 4.42 | |
| SSC | 8 | 3.23 | 1.85 | 0.50 | 1.79 | 3.28 | 4.87 | 5.49 |
Figure 3.
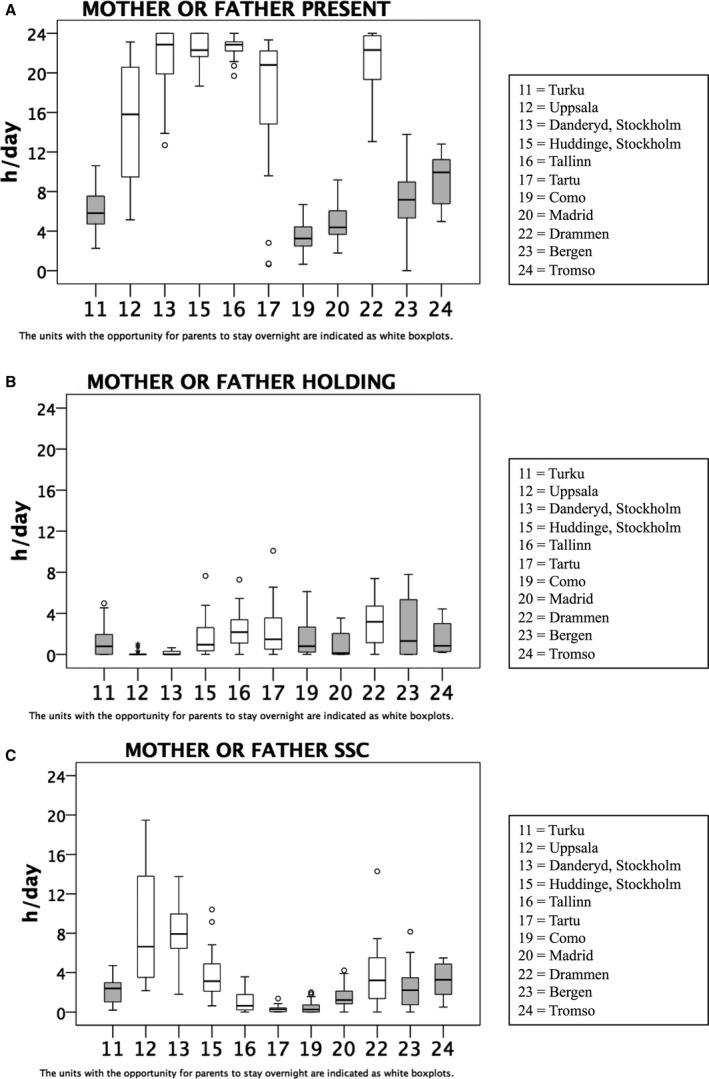
(A) Mother's or father's presence in the neonatal intensive care unit (NICU) during the first two weeks of infant's life. (B) Mother or father holding their infant in the NICU during the first two weeks of infant's life. (C) Mother or father having skin‐to‐skin contact with their infant during the first two weeks of the infant's life.
In six units, the parents were present most of the night between 10 p.m. and 7 a.m. (Fig. 4A), and in five of those, the median duration of the parents’ presence was more than seven hours during that nine‐hour period. Night‐time SSC was often only provided in two units: the median duration of night‐time SSC was 1.8 hours in Danderyd, Sweden, and 0.9 hours in Uppsala, Sweden. The Uppsala data showed that some families provided SSC throughout the night (Fig. 4C). Night‐time holding was rare in all of the units (Fig. 4B).
Figure 4.
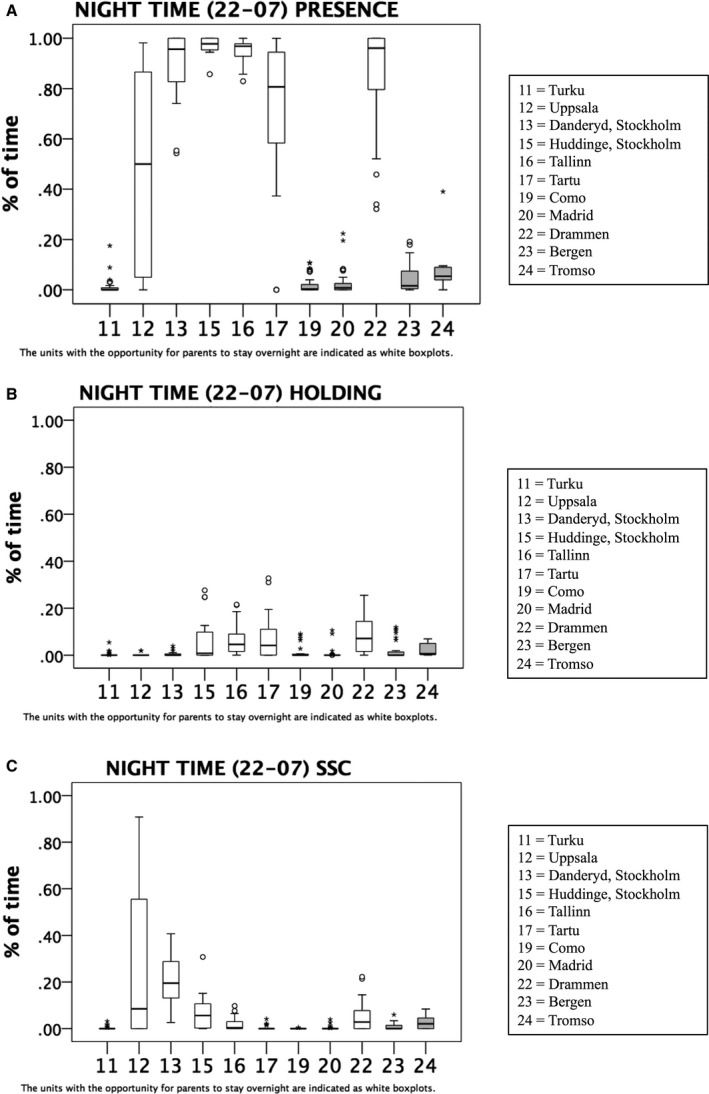
(A) Mother's or father's presence during the night‐time (10 p.m. to 7 a.m.) during the first two weeks of infant's life. (B) Mother or father holding their infant during the night‐time (10 p.m. to 7 a.m.) during the first two weeks of infant's life. (C) Mother or father in skin‐to‐skin contact with their infant during the night‐time (10 p.m. to 7 a.m.) during the first two weeks of infant's life.
The fathers’ contribution to the total parental presence varied between the units from 12% to 46% (p < 0.001) and accounted for 14–43% of the time the infants were held (p = 0.11) and 10–37% of the SSC (p < 0.001). The fathers with the highest proportion of the parental presence were in the Swedish units.
In multivariate analyses, the parents’ presence, holding and SSC during the first two weeks of life varied between the neonatal units. There were associations between mothers who were younger and those who had a higher level of education and spending more time in the NICU. Parents who lived together also spent more time in the units than those who did not. The mother having a higher level of education was also associated with more time providing SSC. In addition, being singleton increased the time for SSC, with a median of 2.3 (0–19.5) hours for singletons and median of 1.2 (0–8.4) hours for twins (p < 0.001). However, the time spent holding the infant or infants was not different in singletons versus twins, with a median of 0.9 (0–10) and 0.9 (0–6.8) hours, respectively (p = not significant). Higher gestational age at birth was associated with a higher amount of holding. Having other children or the distance from the family home to the hospital did not explain any differences in presence, holding or SSC (Table 3).
Table 3.
The magnitude of effect of background variables on parent–infant closeness (shown as hours)
| Parents’ presence | Holding | Skin‐to‐skin contact | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Neonatal unit | p < 0.0001 | p < 0.0001 | p < 0.0001 | ||||||
| Infant characteristics | |||||||||
| β ‐estimate | Confidence limits | β ‐estimate | Confidence limits | ||||||
| Gestational age (per one week) | 0.386 | 0.283 | 0.490 | ||||||
| Twins | −0.53 | −0.74 | −0.32 | ||||||
| Parent characteristics | |||||||||
| β ‐estimate | Confidence limits | β ‐estimate | Confidence limits | ||||||
| Mother's age (per five years) | −0.05 | −0.10 | −0.010 | ||||||
| Mother's education (university versus lower) | −0.09 | −0.18 | −0.01 | −0.30 | −0.52 | −0.09 | |||
| Parents living together (no versus yes) | 0.33 | 0.04 | 0.61 | ||||||
The data provided us with an opportunity to analyse time trends for the 81 patients who stayed in the NICUs for longer than 30 days. On average, the parental presence and holding increased to a mean of 77 minutes (SD 307 minutes, p = 0.03) and a mean of 115 minutes (SD 134 minutes, p < 0.001), respectively, and the duration of SSC decreased to a mean of 34 minutes (SD 130 minutes, p = 0.02).
Discussion
There were significant differences between the European countries and between the units within the countries, in all the measured aspects of physical parent–infant closeness: presence, holding and SSC. More parent–infant closeness was found in units that provided parents with the opportunity to stay with their infant overnight.
The units that provided opportunities for overnight stays for at least one parent had a significantly higher parental presence in this study. In several NICUs and countries, some infants had a parental presence 24 hours per day, which has always been the aim of the single‐family room NICU design 13. In contrast to other studies, neither the distance from home to the hospital nor the presence of other children at home explained the differences in parental presence 14, 15. Interestingly, younger mothers spent more time in the unit than older mothers in this study, in contrast to earlier findings 16. The shortest daily presence of parents was around three to four hours, which is in agreement with earlier prospective studies 14, 17. However, the results are not directly comparable because only the mothers’ presence was measured in the earlier reports. None of the units in this European survey had regulations that restricted parental presence and that could explain the differences between the units.
Earlier studies from NICUs have reported SSC from 0.48 hours per day 18 to 5.17 hours per day 19. In the present study, the amount of daily SSC was over eight hours in two units that both provided a ‘bed‐in‐a‐unit’ set‐up and below one hour in two other units, one that provided a ‘bed‐in‐a‐unit’ set‐up and one that did not. This finding suggests that providing a bed for a parent is necessary for prolonged SSC, but that this is not sufficient on its own and an appropriate culture of care is also required. Some parents had SSC with their infant for 19 hours a day on average, which can be considered Kangaroo mother care, as defined by the World Health Organization 20. The parents with the highest education seemed to provide more SSC.
Having a single‐family room has been shown to increase parents’ presence, satisfaction and privacy 3, 21, 22, 23. This is in line with the present findings that parents are more likely to be present and provide more SSC when there is a ‘bed‐in‐a‐unit’ or single‐family room. Lester et al. 3 showed that single‐family room units were associated with earlier enteral feeding, better infant growth, fewer infections, fewer medical procedures and less pain than open bay units. The effects on an infant's attention, stress, pain, weight gain and medical procedures for fever were mediated by their mother's presence and developmental support from an occupational therapist 3. In addition, the infants were in a more balanced neurobehavioral state at discharge when they were cared for in a single‐family room. This European survey identified five different architectural models that supported the parents’ presence in the NICUs, ranging from a separate room providing accommodation for a mother inside the NICU to an integrated room for both parents and the infant. The units were classified as ‘bed‐in‐a‐unit’ and single‐family room units if most parents were provided with the opportunity to stay overnight in the unit from the start of the infant's hospital care. Because of the variations in the single‐family rooms that were provided, it is important to describe the type of architectural model in each study. Flacking and Dykes reported in their ethnographic study that having a bed or chair for the parents emphasised their importance and expectations as parents. However, having a room made the parents feel more at home in the hospital 23.
Skin‐to‐skin contact decreased during the first month of the infant's life and seemed to be replaced by holding. There has limited research about holding or cuddling a clothed infant during neonatal hospitalisation. In this study, holding and SSC were treated as two distinct types of physical closeness. Holding is important to the parents and improves cortisol coregulation between the mother and the infant 24, but SSC provides a larger range of benefits 25. The fact that holding increased in relation to the infant's age was consistent with earlier studies 17, and this may indicate that the type of parent–infant interaction changed based on the infant's development. As gestational age increases, preterm infants develop a capacity to maintain eye contact and use it in interaction situations. In addition to increased holding, the parents’ presence increased as the infant got older. Earlier studies have reported that parents’ presence 17 and visits 26, 27 reduced as the infant got older. This may suggest differences in the cultures and practices of the European units regarding parental support than older studies or different societies.
This study was carried out prospectively using diary data derived directly from the parents. Thernström–Blomqvist reported that reports of SSC by parents and staff were reliable 19. If there was a bias in the parental reporting, it is probably because the parents forgot to report some episodes of presence, SSC or holding, and therefore, the amounts were underreported rather than overreported. Earlier studies have usually described the parents’ presence or SSC from data recorded by staff or patient charts 9, 14, 17. The rate of participation in this study was high, even in this vulnerable patient population, which shows how acceptable the diary method was. The diary data also made it possible to analyse the duration of presence and physical closeness, whereas most of the earlier studies only reported the number of visits 26, 28 or episodes of SSC 18, 27.
The present study included 11 European NICUs from six wealthy countries in Northern and Southern Europe with reasonable social benefits. The length of maternity leave, with maternity pay, varied between four and 18 months and paternity leave varied between 0 and 60 days. Four countries – Estonia, Finland, Norway and Sweden – provided for seven months to 18 months of additional parental leave that could be taken by either the mother or the father. In addition, three countries – Finland, Norway and Sweden – provided different paternity pay for fathers to cover the days when the infant was in a hospital. These benefits supported the parent–infant closeness of hospitalised infants, but large differences were found, even within countries. Therefore, unit‐specific factors explained the differences within the countries, as the social benefits were similar.
It is clear that the units differed from each other in many respects, and these differences were evaluated using simple questions. We acknowledge that these questions did not cover all of the features of the units. We described variations in the care cultures of these units in previous publications 29, 30. In this study, the care culture was approached from the perspective of parent–infant closeness and one major factor that affected this was identified: the opportunity for at least one parent to stay in the unit overnight. We cannot know how much this ‘bed‐in‐a‐unit’ was a proxy for a different care culture, namely whether those units that provided physical facilities for parents had also developed a family‐centred care culture. It is unlikely that units that are not interested in the development of their family‐centred care take part in research to map out the differences in parent–infant closeness.
More studies are needed to understand what underlies and explains the differences between care cultures. The diary measure proved to be a feasible method and could be used in many settings to evaluate the effects of various architectural and care culture interventions on parent–infant closeness. A validation process of the parental closeness diary is ongoing in a larger population. Observational studies would also be valuable as they would deepen our understanding of how the design of NICUs can be used to remodel the culture of care.
Conclusion
This prospective study evaluated physical parent–infant closeness in a European multicentre setting of 11 NICUs in six countries. There was a higher level of parental presence in the units that provided facilities for the parents to stay overnight, and younger mothers, in particular, took advantage of the opportunity to stay close to their infants. These results highlight the significance of a ‘bed‐in‐a‐unit’ design for parent–infant closeness in NICUs.
Conflict of interest
The authors have no conflict of interests to declare.
Funding
This study did not receive any external funding.
Supporting information
Table S1 Parent‐infant characteristics.
Acknowledgements
We want to thank the research assistants who recruited the patients and collected the data, including Cecilia Ewald, Annika Örtenstrand, Kari Fokstuen, Mario Barbarini, Luciana Leva, Anna Maria Alessi, Belen Aragonés Corral, Sonia Dominguez Barbachano, Miriam Gonzalez Villalba, Laura Hernández, Gloria Sanz Prades, Silvia Massip Pi, Maria Mateo Martinez, Gema Moral López, Elena Beatriz Sadornil Gonzalez, Hege Grundtin, Marianne Nordhov, Pille Andresson, Birgit Kiilaspää, Kati Korjus, Marina Mkrtõtšjan, Svetlana Müürsepp, Angeelika Plaaser, Jana Retpap, Sirje Keerdo, Mirje Kristmann and Heili Varendi. We also want to thank Jaakko Matomäki for the statistical analyses.
References
- 1. Flacking R, Lehtonen L, Thomson G, Axelin A, Ahlqvist S, Moran VH, et al. Closeness and separation in neonatal intensive care. Acta Paediatr 2012; 101: 1032–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Greisen G, Mirante N, Haumont D, Pierrat V, Pallás‐Alonso CR, Warren I, et al. Parents, siblings and grandparents in the Neonatal Intensive Care Unit A survey of policies in eight European countries. Acta Paediatr 2009; 98: 1744–50. [DOI] [PubMed] [Google Scholar]
- 3. Lester BM, Hawes K, Abar B, Sullivan M, Miller R, Bigsby R, et al. Single‐family room care and neurobehavioural and medical outcomes in preterm infants. Pediatrics 2014; 134: 754–60. [DOI] [PubMed] [Google Scholar]
- 4. Raiskila S, Axelin A, Rapeli S, Vasko I, Lehtonen L. Trends in care practices reflecting parental involvement in neonatal care. Early Hum Dev 2014; 90: 863–7. [DOI] [PubMed] [Google Scholar]
- 5. Maastrup R, Greisen G. Extremely preterm infants tolerate skin‐to‐skin contact during the first weeks of life. Acta Paediatr 2010; 99: 1145–9. [DOI] [PubMed] [Google Scholar]
- 6. Mörelius E, Angelhoff C, Eriksson J, Olhager E. Time of initiation of skin‐to‐skin contact in extremely preterm infants in Sweden. Acta Paediatr 2012; 101: 14–8. [DOI] [PubMed] [Google Scholar]
- 7. Karlsson V, Heinemann AB, Sjörs G, Nykvist KH, Ågren J. Early skin‐to‐skin care in extremely preterm infants: thermal balance and care environment. J Pediatr 2012; 161: 422–6. [DOI] [PubMed] [Google Scholar]
- 8. Moore E, Anderson GC, Bergman N. Early skin‐to‐skin contact for mothers and their healthy newborn infants. Cochrane Database Syst Rev 2007; 5: CD003519. [DOI] [PubMed] [Google Scholar]
- 9. Olsson E, Andersen RD, Axelin A, Jonsdottir RB, Maastrup R, Eriksson M. Skin‐to‐skin care in neonatal intensive care units in the Nordic countries: a survey of attitudes and practices. Acta Paediatr 2012; 101: 1140–6. [DOI] [PubMed] [Google Scholar]
- 10. Miles MS, Funk SG, Carlson J. Parental Stressor Scale: neonatal intensive care unit. Nurs Res 1993; 42: 148–52. [PubMed] [Google Scholar]
- 11. AAP . Levels of neonatal care. Pediatrics 2012; 130: 587–97. [DOI] [PubMed] [Google Scholar]
- 12. Westrup B. Family‐centered developmentally supportive care. NeoReviews 2014; 15: e325–35. [Google Scholar]
- 13. Ortenstrand A, Westrup B, Broström EB, Sarman I, Akerström S, Brune T, et al. The Stockholm Neonatal Family Centered Care Study: effects on length of stay and infant morbidity. Pediatrics 2010; 125: e278–85. [DOI] [PubMed] [Google Scholar]
- 14. Franck LS, Spencer C. Parent visiting and participation in infant caregiving activities in a neonatal unit. Birth 2003; 30: 31–5. [DOI] [PubMed] [Google Scholar]
- 15. Giacoia GP, Rutledge D, West K. Factors affecting visitation of sick newborns. Clin Pediatr 1985; 24: 259–62. [DOI] [PubMed] [Google Scholar]
- 16. Brown LP, York R, Jacobsen B, Gennaro S, Brooten D. Very low birth‐weight infants: parental visiting and telephoning during initial infant hospitalization. Nurs Res 1989; 38: 233–6. [PubMed] [Google Scholar]
- 17. Reynolds LC, Duncan MM, Smith GC, Mathur A, Neil J, Inder T, et al. Parental presence and holding in the neonatal intensive care unit and associations with early neurobehavior. J Perinatol 2013; 33: 636–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Gonya J, Nelin LD. Factors associated with maternal visitation and participation in skin‐to‐skin care in an all referral level IIIc NICU. Acta Paediatr 2013; 102: 53–6. [DOI] [PubMed] [Google Scholar]
- 19. Blomqvist YT, Rubertsson C, Nyqvist KH. Parent‐infant skin‐to‐skin contact; How do parent records compare to nurse records? Acta Paediatr 2011; 100: 773–5. [DOI] [PubMed] [Google Scholar]
- 20. Organization WH . WHO recommendations on interventions to improve preterm birth outcomes. Geneva: World Health Organization, 2015. Available at: https://www-ncbi-nlm-nih-gov.ezproxy.utu.fi/books/NBK321160/ (accessed on November 10, 2016). [PubMed] [Google Scholar]
- 21. Stevens DC, Helseth CC, Akram Khan M, Munson DP, Reid EJ. A comparison of parent satisfaction in an open‐ bay and single‐family room neonatal intensive care unit. HERD 2011; 4: 110–23. [DOI] [PubMed] [Google Scholar]
- 22. Shahheidari M, Homer C. Impact of the design of Neonatal Intensive Care Units on neonates, staff, and families: a systematic literature review. J Perinat Neonatal Nurs 2012; 26: 260–6. [DOI] [PubMed] [Google Scholar]
- 23. Flacking R, Dykes F. ‘Being in a womb’ or ‘playing musical chairs’: the impact of place and space on infant feeding in NICUs. BMC Pregnancy Childbirth 2013; 13: 179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Neu M, Laudenslager ML, Robinson J. Coregulation in salivary cortisol during maternal holding of premature infants. Biol Res Nurs 2009; 10: 226–40. [DOI] [PubMed] [Google Scholar]
- 25. Conde‐Agudelo A, Díaz‐Rossello José L. Kangaroo mother care to reduce morbidity and mortality in low birthweight infants. Cochrane Database Syst Rev 2014; 4: CD002771. [DOI] [PubMed] [Google Scholar]
- 26. Latva R. Preterm birth and hospitalisation experiences of mother and child. Tampere: Tampere University Press, 2009. [Google Scholar]
- 27. Greene MM, Rossman B, Patra K, Kratovil A, Khan S, Meier PP. Maternal psychological distress and visitation to the neonatal intensive care unit. Acta Paediatr 2015; 104: e306–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Latva R, Lehtonen L, Salmelin RK, Tamminen T. Visiting less than every day a marker for later behavioral problems in Finnish preterm infants. Arch Pediatr Adolesc Med 2004; 158: 1153–7. [DOI] [PubMed] [Google Scholar]
- 29. Dykes F, Thomson G, Gardner C, Moran VH, Flacking R. Perceptions of European medical staff on the facilitators and barriers to physical closeness between parents and infants in neonatal units. Acta Paediatr 2016; 105: 1039–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Raiskila S, Lehtonen L, Tandberg BS, Normann E, Ewald U, Caballero S, et al. Parent and nurse perceptions on the quality of family‐centered care in 11 European NICUs. Aust Crit Care 2016; 29: 201–9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1 Parent‐infant characteristics.


