Abstract
Context:
Medial tibial stress syndrome (MTSS) is a common condition in active individuals and presents as diffuse pain along the posteromedial border of the tibia.
Objective:
To use cross-sectional, case-control, and cohort studies to identify significant MTSS risk factors.
Data Sources:
Bibliographic databases (PubMed, Scopus, CINAHL, SPORTDiscus, EMBASE, EBM Reviews, PEDRo), grey literature, electronic search of full text of journals, manual review of reference lists, and automatically executed PubMed MTSS searches were utilized. All searches were conducted between 2011 and 2015.
Study Selection:
Inclusion criteria were determined a priori and included original research with participants’ pain diffuse, located in the posterior medial tibial region, and activity related.
Study Design:
Systematic review with meta-analysis.
Level of evidence:
Level 4.
Data Extraction:
Titles and abstracts were reviewed to eliminate citations that did not meet the criteria for inclusion. Study characteristics identified a priori were extracted for data analysis. Statistical heterogeneity was examined using the I2 index and Cochran Q test, and a random-effects model was used to calculate the meta-analysis when 2 or more studies examined a risk factor. Two authors independently assessed study quality.
Results:
Eighty-three articles met the inclusion criteria, and 22 articles included risk factor data. Of the 27 risk factors that were in 2 or more studies, 5 risk factors showed a significant pooled effect and low statistical heterogeneity, including female sex (odds ratio [OR], 2.35; CI, 1.58-3.50), increased weight (standardized mean difference [SMD], 0.24; CI, 0.03-0.45), higher navicular drop (SMD, 0.44; CI, 0.21-0.67), previous running injury (OR, 2.18; CI, 1.00-4.72), and greater hip external rotation with the hip in flexion (SMD, 0.44; CI, 0.23-0.65). The remaining risk factors had a nonsignificant pooled effect or significant pooled effect with high statistical heterogeneity.
Conclusion:
Female sex, increased weight, higher navicular drop, previous running injury, and greater hip external rotation with the hip in flexion are risk factors for the development of MTSS.
Keywords: medial tibial stress syndrome, risk factors, meta-analysis
Medial tibial stress syndrome (MTSS) is a common condition in active individuals, including athletes and military personnel.3,5,26,32,37,43,44 MTSS presents as diffuse pain along the posteromedial border of the tibia associated with activity. Although symptoms of MTSS are located at the interface of the crural fascia and bone, there is evidence that MTSS is associated with specific bone changes.10,11,20,21
Nomenclature for MTSS historically has included such terms as shin splints, medial tibial syndrome, tibial stress syndrome, and soleus syndrome.7,25,33,38 In this systematic review, MTSS was defined as including 3 characteristics: (1) pain along the posteromedial border of the tibia, (2) diffuse pain, and (3) pain that is activity related.
Over the past 2 decades, there has been an increase in obesity prevalence in the United States, with a concomitant increase in associated chronic disease conditions, including type II diabetes, heart disease, and stroke.6,17,30 While the health benefits of physical activity in addressing these conditions are well known, physical activity may result in such overuse conditions as MTSS. The failure to successfully prevent MTSS is a reflection of our limited understanding of the risk factors. The purpose of this systematic review was to identify cross-sectional, case-control, and cohort studies that included MTSS risk data and to use a meta-analysis to identify significant risk factors across those studies.
Methods
Data Sources and Search Strategy
Between October 2011 and May 2012, searches of electronic and print information sources were conducted to identify all potentially relevant articles. The data sources used in the search are available in the supplementary web materials (see Appendix 1, available at http://sph.sagepub.com/content/suppl). A PubMed search strategy was developed using 3 concepts: (1) the nomenclature used for MTSS, (2) anatomical location of MTSS, and (3) activity related to the development of MTSS, each with relevant medical subject headings (MeSH) and text words. The PubMed strategy was adapted for syntax and controlled vocabulary for the other electronic databases. No restrictions to publication year or language were applied to the searches. All citations were imported into a bibliographic management software program (EndNote; Thomson Reuters). The detailed search strategy for PubMed is located in the supplementary web materials (see Appendix 2, available at http://sph.sagepub.com/content/suppl).
Study Selection
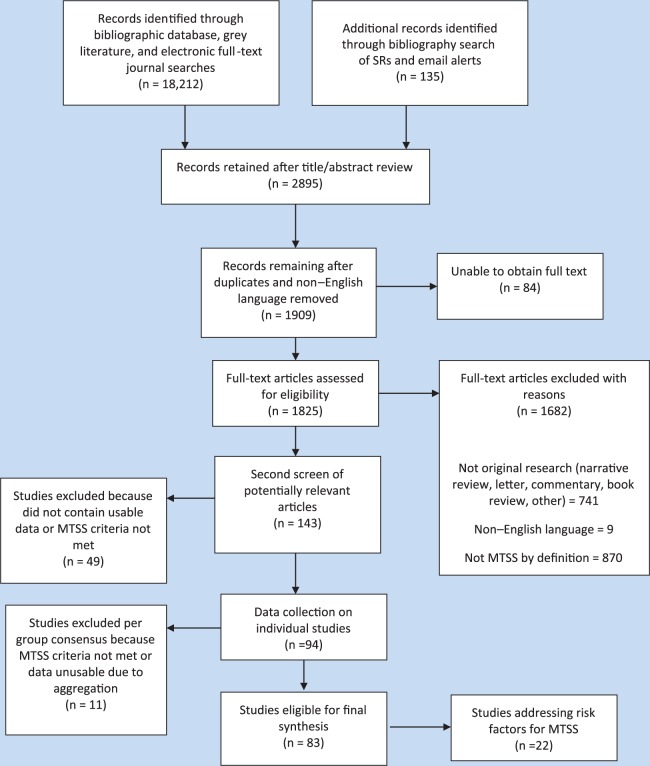
Criteria for study inclusion were established a priori. To be included, studies had to be original research and participants’ pain had to be diffuse, located in the posterior medial tibial region, and activity related. The selection of included studies began with title and abstract review, and irrelevant citations were eliminated. After the title and abstract review, duplicate citations were removed and the full-text articles for potentially relevant citations were obtained. A training set of full-text articles was selected and used by the authors to pilot test the determination of study inclusion/exclusion. After this pilot process and development of decision rules, the complete set of full-text articles selected for possible inclusion was divided into 2 subsets, and 2 pairs of authors reviewed their assigned subsets for inclusion/exclusion. Within each pair, articles were reviewed independently, and consensus was used to resolve disagreements. If the pair of authors could not reach consensus, the article was reviewed by all authors, with consensus used to determine possible eligibility. A final set of studies was selected that met the MTSS inclusion criteria (Figure 1).
Figure 1.
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flow diagram of process. MTSS, medial tibial stress syndrome; SR, systematic review.
Data Collection and Extraction
Prior to data extraction from the selected studies, a preliminary data collection form was developed and a training set of articles was selected. Pilot testing of the form and data extraction was similar to the previous pilot testing used for inclusion/exclusion. The set of studies selected for inclusion was again divided between the same pairs of authors for data extraction. The following key data, among others, were recorded for each individual study: study purpose, study design, setting, participant characteristics, activity associated with MTSS, definition of MTSS, diagnostic tests for MTSS, length of follow-up, risk factors, and risk factor results. When needed, selected study authors were contacted to obtain specific data.
Quality Analysis
Quality indicators were developed a priori from several sources.8,12,14,22,28,40 For this systematic review, 2 quality indicators, not based on past literature, were added a priori. These 2 indicators included whether the reliability of risk factor(s) measures was reported and whether the risk factor(s) measures were direct or indirect. Quality items were scored as “met,” “mixed” (met for some but not all risk factors), “not met,” “unclear,” and “not reported.” Decision rules were used to clarify scoring of quality items. For example, the quality item “analysis” was deemed “met” when a multivariate technique was used to analyze the data. Before quality assessments of the final set of articles were reviewed, all authors discussed the items to further clarify and agree on scoring.
Two authors (R.R.R. and M.M.K.) independently reviewed the full text of the included studies for quality indicators. Consensus was used to resolve disagreements. When needed, consensus among all authors was used. Table 1 includes the quality indicators for all included studies.
Table 1.
Study quality
| Quality Items
a
|
|||||||||
|---|---|---|---|---|---|---|---|---|---|
| Study | Design | Homogeneous Participants | Follow-up Length b | Follow-up ≥80% | Reliability of Risk Factor(s) | Risk Factor(s) Direct c | Diagnosis of MTSS d | Adjustments e | Analysis f |
| Bennett et al3 | P | ||||||||
| Burne et al5 | P | ||||||||
| Hubbard et al16 | P | ||||||||
| Magnusson et al21 | P | ||||||||
| Moen et al26 | P | ||||||||
| Plisky et al32 | P | ||||||||
| Raissi et al34 | P | ||||||||
| Yagi et al43 | P | ||||||||
| Yates and White44 | P | ||||||||
| Bandholm et al1 | CS | NA | NA | ||||||
| Bartosik et al2 | CS | NA | NA | ||||||
| Eickhoff et al9 | CS | NA | NA | ||||||
| Franklyn et al10 | CS | NA | NA | ||||||
| Lee18 | CS | NA | NA | Multiple analyses | Multiple analyses | ||||
| Madeley et al19 | CS | NA | NA | ||||||
| Magnusson et al20 | CS | NA | NA | ||||||
| Messier and Pittala24 | CS | NA | NA | ||||||
| Rathleff et al36 | CS | NA | NA | ||||||
| Tweed et al41 | CS | NA | NA | ||||||
| Viitasalo and Kvist42 | CS | NA | NA | ||||||
| Rathleff et al35 | CC | NA | NA | ||||||
| Sommer and Vallentyne39 | CC | NA | NA | ||||||
CC, case-control; CS, cross-sectional; MTSS, medial tibial stress syndrome; P, prospective.
Color code: green, met; red, not met; yellow, mixed (met for some but not all risk factors); grey, not clear; orange, not reported.
Athletes followed by season; recreational and military, 6 weeks.
Risk factors were measured directly.
Made by a health care provider.
History of MTSS or orthotic use was controlled for in design or analysis.
Statistical analysis appropriate for the design of the study.
Data Analysis
All included studies were reviewed for clinical heterogeneity by examining differences in measurement methods for risk factors. The risk factor data were extracted from each study, and the data were entered into meta-analysis software (Comprehensive Meta-Analysis, version 2.2.064; Biostat). Statistical heterogeneity was examined using the I2 index and the Cochran Q test.15 A random-effects model was used to calculate the meta-analysis. Because the included studies were not likely to have a common effect size, a random-effects model was chosen.4 The random-effects model also is more conservative than the fixed-effects model.4 Pooled summary results for risk factors were calculated when 2 or more studies reported on the risk factor.
Results
The initial search of the bibliographic databases, grey literature, and electronic full-text journal searches yielded 18,212 articles. An additional 135 articles were located through searching the reference lists of systematic reviews and automated PubMed searches of MTSS. Title and abstract review combined with removal of duplicates, and non–English language articles resulted in 1825 full-text articles assessed for eligibility. These articles were reviewed to assess whether they met inclusion criteria, provided usable risk factor data, and had comparable measurement methodology to allow for comparison. From the 1825 articles, 83 articles met inclusion criteria based on the definition of MTSS. These 83 articles were reviewed, and 22 articles with MTSS risk factor data were selected for this systematic review (Figure 1). From these 22 articles, 27 different risk factors were selected based on the availability of risk data from 2 or more studies and low clinical heterogeneity based on risk factor measurement techniques (Table 2). The supplementary web materials provide the study characteristics for all 22 selected studies (see Appendix 3, available at http://sph.sagepub.com/content/suppl). The risk factors selected for analysis were organized into 7 categories: demographics/body composition, static posture, gait variables, training variables, injury history, joint mobility, and muscle strength. From the meta-analysis, risk factors were placed into 1 of 4 groups (Table 3) based on the presence or absence of a statistically significant pooled effect and the extent of statistical heterogeneity based on the I2 index and Cochran Q value. To be considered low statistical heterogeneity, I2 was less than 32.5% and/or the Cochran Q value was nonsignificant (P > 0.05).
Table 2.
Risk factors by study
| Study | Age | Dflex ROM With Knee ext | Dflex ROM With Knee flex | BMI | Dflex isom Strength | Eversion isom Strength | Eversion ROM With Running | Eversion ROM | Hip ext rot ROM With Hip flex | Female Sex | Height | Hx MTSS | Hip int rot ROM With Hip flex | Inversion ROM | Inversion isom Strength | Lean Calf Girth | Leg Length Difference | Navicular Drop | PFlex ROM | Previous Running Injury | Q Angle | Stand Foot Angle | Tibial Varum | Walking Speed | Weekly Mileage | Weight | Years Running |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Bennett et al3 | • | • | |||||||||||||||||||||||||
| Burne et al5 | • | • | • | • | • | • | • | • | • | ||||||||||||||||||
| Hubbard et al16 | • | • | • | • | • | • | • | • | • | • | • | ||||||||||||||||
| Magnusson et al21 | • | • | |||||||||||||||||||||||||
| Moen et al26 | • | • | • | • | • | • | • | • | • | • | • | • | |||||||||||||||
| Plisky et al32 | • | • | • | • | • | ||||||||||||||||||||||
| Raissi et al34 | • | • | • | • | |||||||||||||||||||||||
| Yagi et al43 | • | • | • | • | • | • | • | • | • | • | |||||||||||||||||
| Yates and White44 | • | • | • | • | • | • | |||||||||||||||||||||
| Bandholm et al1 | • | ||||||||||||||||||||||||||
| Bartosik et al2 | • | • | • | • | • | • | |||||||||||||||||||||
| Eickhoff et al9 | • | ||||||||||||||||||||||||||
| Franklyn et al10 | • | • | • | ||||||||||||||||||||||||
| Lee18 | • | • | • | • | • | • | • | • | • | • | • | • | • | • | • | ||||||||||||
| Madeley et al19 | • | • | • | ||||||||||||||||||||||||
| Magnusson et al20 | • | • | |||||||||||||||||||||||||
| Meisser and Pittala24 | • | • | • | ||||||||||||||||||||||||
| Rathleff et al36 | • | • | • | • | |||||||||||||||||||||||
| Tweed et al41 | • | ||||||||||||||||||||||||||
| Viitasalo et al42 | • | • | • | ||||||||||||||||||||||||
| Rathleff et al35 | • | • | |||||||||||||||||||||||||
| Sommer and Vallentyne39 | • | • |
Dflex, dorsiflexion; ext, extended; ext rot, external rotation; flex, flexed; int rot, internal rotation; isom, isometric; MTSS, medial tibial stress syndrome; Pflex, plantarflexion; ROM, range of motion.
Table 3.
MTSS risk factors grouping based on pooled effect and statistical heterogeneity
| Significant Pooled Effect |
Nonsignificant Pooled Effect |
||
|---|---|---|---|
| Low Heterogeneity | Moderate-High Heterogeneity | Moderate-High Heterogeneity | Low Heterogeneity |
| Female sex Higher weight Higher navicular drop Previous running injury Greater hip ext rot with hip flexed |
Higher BMI Greater eversion with running |
Lean calf girth Hip int rot with hip flexed Leg length difference Q-angle Dflex ROM with knee extended Dflex ROM with knee flexed Inversion isom strength Pflex ROM Standing foot angle Years running History of MTSS |
Age Height Eversion ROM Inversion ROM Dflex isom strength Eversion isom strength Tibial varum Walking speed Weekly mileage |
BMI, body mass index; Dflex, dorsiflexion; ext rot, external rotation; int rot, internal rotation; isom, isometric; MTSS, medial tibial stress syndrome; Pflex, plantarflexion; ROM, range of motion.
Demographics/Body Composition
Two of the 6 risk variables in this category (sex and weight) had a significant pooled effect with low heterogeneity (I2 < 31%) across studies (8 studies included sex, 7 studies included weight). The meta-analysis revealed that female sex (Figure 2) and increased weight (Figure 3) were both risk factors for MTSS. Although greater body mass index (BMI) was a risk factor for MTSS based on the pooled effect, the 9 studies were moderately heterogeneous (I2 = 61%). While 8 of the 9 studies found greater mean BMI in the MTSS group, Lee18 found BMI to be lower in the MTSS group. The other 3 risk factors in this category (age, height, and lean calf girth) were not significant risk factors for MTSS based on pooled analysis. Both age (8 studies) and height (9 studies) had low heterogeneity across studies; the lean calf girth variable was examined in 2 studies with high heterogeneity (I2 = 74%). Moen et al26 found the MTSS group to have a greater lean calf girth, whereas Burne et al5 reported smaller calf girth in the MTSS group.
Figure 2.
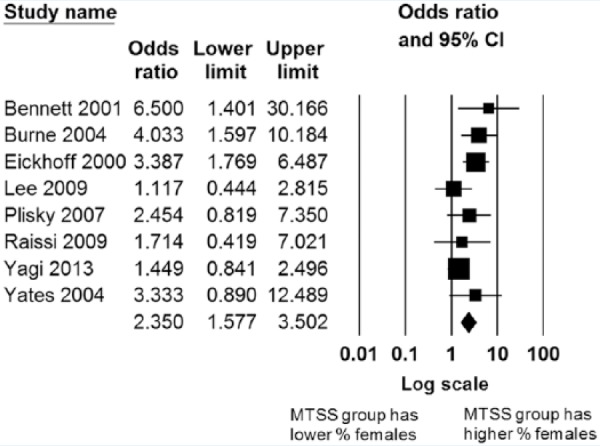
Forest plot for female sex as a risk factor for medial tibial stress syndrome (MTSS).
Figure 3.
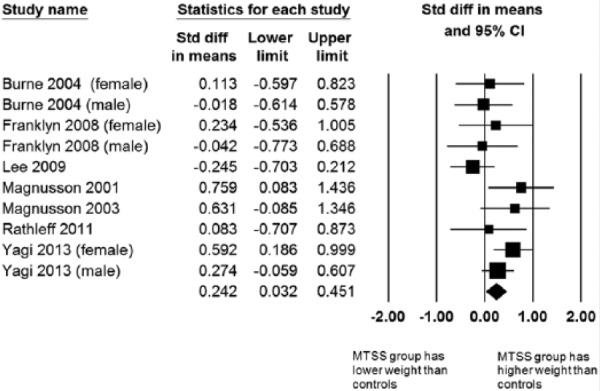
Forest plot for weight as a risk factor for medial tibial stress syndrome (MTSS).
Static Posture
The only postural variable that was a significant predictor of MTSS based on the meta-analysis was a greater navicular drop value (Figure 4). The 8 studies that examined navicular drop had low to moderate heterogeneity (I2 = 39%) with a nonsignificant Q value. Standing foot angle (SFA), Q angle, tibial varum, and limb-length discrepancy were nonsignificant as risk factors for MTSS based on pooled analyses. The 2 studies16,42 that reported tibial varum data had low heterogeneity (I2 = 0%). Conversely, there was high heterogeneity across the studies that reported SFA (I2 = 74%), Q angle (I2 = 68%), and limb-length difference (I2 = 86%). Sommer and Vallentyne39 reported that subjects (folk dancers) with an SFA < 140° were at greater risk for MTSS, but Moen et al26 did not corroborate that finding. For Q angle, 2 studies reported a smaller Q angle as a risk for MTSS,34,43 and 3 studies18,24,43 reported the Q angle was greater in the MTSS group. Finally, the results of the 4 studies examining limb-length differences and MTSS had highly variable and nonsignificant results.
Figure 4.
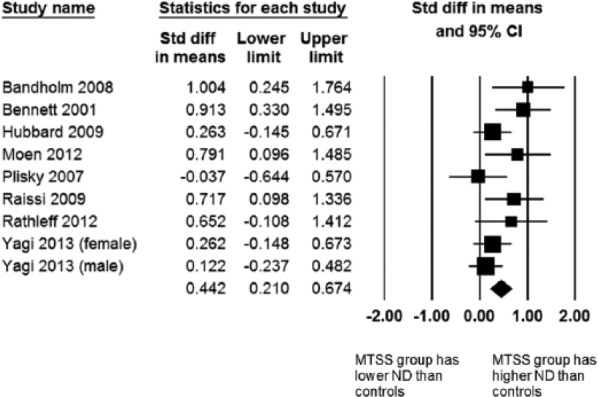
Forest plot for navicular drop (ND) as a risk factor for medial tibial stress syndrome (MTSS).
Gait Variables
Only 2 gait variables were assessed for MTSS risk in 2 or more studies. The pooled effect of rearfoot eversion during running revealed significantly greater eversion in the MTSS groups as compared with controls, but the 3 pooled studies were highly heterogeneous (I2 = 92%). Self-selected walking speed was not a significant predictor variable for MTSS, with very low heterogeneity (I2 = 0%).
Training Variables
Neither of the 2 training variables (years of running experience and weekly training mileage) were risk factors for MTSS based on the meta-analysis. The statistical heterogeneity for years running was high (I2 = 87%), as Hubbard et al16 reported that fewer years running was a risk factor for MTSS whereas Lee18 reported that more years of running was a risk factor for MTSS. Plisky et al32 did not find years running to be risk factor for MTSS in high school runners. Weekly mileage was not a risk factor based on pooled data from 2 studies,16,18 and the studies had low heterogeneity (I2 = 24.3%).
Injury History
Pooled analysis revealed that a previous running injury was a risk factor for MTSS (Figure 5), with low heterogeneity (I2 = 0%) across 2 studies.32,34 History of MTSS did not have a significant pooled effect, and the 2 studies16,44 providing these data had high heterogeneity (I2 = 93%). Hubbard et al16 reported a significant risk ratio of 5.3 (95% CI, 3.43-8.21), whereas the risk ratio reported by Yates and White44 was 1.5 (95% CI, 0.78-3.0).
Figure 5.
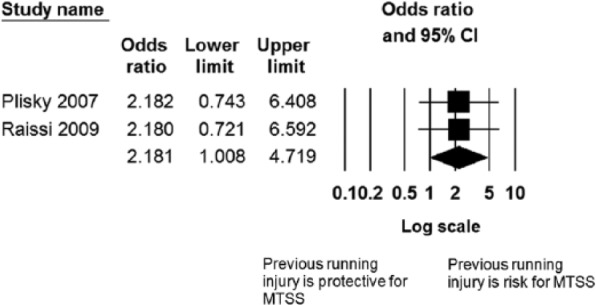
Forest plot for previous running injury as a risk factor for medial tibial stress syndrome (MTSS).
Joint Mobility
Greater hip external rotation range of motion (ROM) with the hip flexed had a significant pooled effect as a risk factor for MTSS (Figure 6) across 3 studies5,26,43 with low heterogeneity (I2 = 0%), whereas the pooled effect of hip internal rotation ROM was not significant with the same 3 studies showing high heterogeneity (I2 = 85%) for this variable. Both eversion and inversion ROM were not risk factors for MTSS based on the meta-analysis (nonsignificant pooled effect), although both factors had low statistical heterogeneity (I2 < 23%). Neither dorsiflexion ROM with the knee flexed nor with the knee extended were risk factors for MTSS based in the pooled effect, and both factors showed high statistical heterogeneity (I2 > 83%). Plantarflexion ROM with the knee extended also was not a significant risk factor for MTSS, and the 2 studies examining this factor18,26 also showed high statistical heterogeneity.
Figure 6.
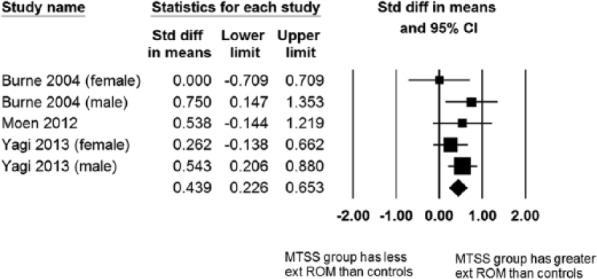
Forest plot for hip external range of motion (ROM) with hip flexed as a risk factor for medial tibial stress syndrome (MTSS).
Muscle Strength
None of the 3 isometric ankle strength factors (inversion, eversion, or dorsiflexion) were significant risk factors for MTSS. Two studies16,18 investigated these 3 strength variables, and for both eversion and dorsiflexion isometric strength, the heterogeneity was very low (I2 = 0%) while the pooled effect was nonsignificant. The inversion strength variable results were markedly different between the 2 studies with high heterogeneity (I2 = 82%), as Hubbard et al16 found no difference between groups with and without MTSS but Lee18 found that weaker isometric inversion was a risk factor for MTSS.
Discussion
The purpose of this systematic review was to identify cohort, case-control, and cross-sectional studies that included MTSS risk data and to use a meta-analysis to identify significant risk factors across those studies. A total of 22 studies were included in this systematic review and meta-analysis, representing a total of 235 potential risk factors. However, only 27 risk factors were identified that could be analyzed in the meta-analysis. Either there was unusable data or there was only a single study that examined a particular risk factor and, as such, there was no opportunity to pool results. We recognize that of those 208 risk factors not subject to meta-analysis, some may, in fact, be risk factors for MTSS but, at present, that conclusion is based on a single study.
Our level of confidence in the identification of significant or nonsignificant risk factors was based on the pooled effect and the statistical heterogeneity of the risk factor. Table 3 summarizes the 27 risk factors by a cross-tabulation of the pooled effect and heterogeneity. Five factors (female sex, higher weight, higher navicular drop, previous running injury, and greater hip external rotation with the hip in flexion) were found to have a significant pooled effect and low heterogeneity (see Figures 2-6). These are the factors in which we have high confidence for increased risk for the occurrence of MTSS. On the other end of the spectrum, 9 factors (age, height, eversion ROM, inversion ROM, dorsiflexion isometric strength, eversion isometric strength, tibial varum, walking speed, and weekly training mileage) did not show a significant pooled effect and had low statistical heterogeneity. These are factors that likely do not increase the risk for MTSS occurrence. The other 2 categories include 13 risk factors that display moderate to high heterogeneity in pooled analysis, limiting the confidence in the results of the meta-analysis regarding whether the factor actually is or is not a risk factor for MTSS (see Appendix 4, available at http://sph.sagepub.com/content/suppl).
Female sex increases the risk for MTSS, which is in agreement with the systematic review and meta-analysis by Newman et al31 and the critical review by Moen et al.27 The mechanism by which female sex causes this increased risk is not known at this time. Newman et al31 proposed that this increased risk may be related to differences in running kinematics between men and women, but this has not been subject to investigation at present. In their study of MTSS among naval recruits, Yates and White44 found that female recruits were at greater risk of MTSS and suggested this might have been related to women training with men and “overstriding” to match the men’s cadence in marching.
Hamstra-Wright et al13 and Newman et al31 both found BMI to be a risk factor for MTSS. Hamstra-Wright et al13 used 4 studies in their meta-analysis and we used those 4 plus an additional 6 studies that met our inclusion criteria. Newman et al31 used 5 studies in their meta-analysis: 3 common to our analysis, 1 that did not meet our inclusion criteria, and the study by Hubbard et al,16 which reported height and weight for the participants but did not directly report BMI values. We also found a significant pooled effect, but the heterogeneity was moderate (I2 = 60.7%) so we did not include BMI as a high-confidence risk factor for MTSS. We did find, however, that increased weight was a risk factor for MTSS when pooling the results across 7 studies (see Figure 3). Our meta-analysis indicated that difference in height was not a risk factor for MTSS, so the findings of BMI as a risk factor reported by Hamstra-Wright et al13 and by Newman et al31 may be related to differences in weight between the MTSS and non-MTSS groups.
A greater navicular drop emerged from the meta-analysis as a risk factor for MTSS, which is consistent with the findings of both Hamstra-Wright et al13 and Newman et al.31 This measurement is employed by clinicians as a measure of foot pronation29 and has been shown to have a relationship with rearfoot motion during walking.23 Of the 8 studies included in the meta-analysis for navicular drop, 5 reported a significantly greater navicular drop in the MTSS groups1,3,26,34,35 (MTSS group: range, 6.0-7.7 mm; noninjured athletes: range, 3.6-5.4 mm). In 2 of the other 3 studies,16,43 the MTSS group had a greater navicular drop value than the non-MTSS group, but the difference was not significant. Plisky et al32 found no difference in the percentage of athletes with MTSS who had a navicular drop >10 mm as compared with athletes without MTSS.
Previous injury history is commonly identified as a risk for a lower extremity overuse injury. Newman et al31 reported that a history of MTSS was a risk factor for the repeat occurrence of MTSS, but this was not confirmed by Hamstra-Wright et al.13 Our meta-analysis showed that history of MTSS had a nonsignificant pooled effect for relative risk and displayed high statistical heterogeneity (I2 = 88%). Newman et al31 based their conclusion on the meta-analysis of 6 studies, but only 2 of those 6 studies16,44 met our inclusion criteria. We did, however, find that history of any previous running injury was a significant risk factor for the development of MTSS. The pooled odds ratio for any running injury as an MTSS risk was 2.181 with low heterogeneity (I2 = 0%), although the lower limit of the 95% confidence interval is very close to an odds ratio of 1 (1.008).
Based on the meta-analysis, the final factor that increases risk for MTSS is greater hip external rotation with the hip flexed. Our findings are consistent with both previously published meta-analyses on MTSS risk factors.13,31 In 2 of the 3 studies used in our meta-analysis,5,43 the authors analyzed and reported male and female hip ranges of motion separately. In both of those studies, we treated the male and female data as separate data sets, resulting in 5 data sets for the meta-analysis. Newman et al31 reported that in both studies, the differences in male hip external ROM were significant and the female differences were not significant. However, in the study by Moen et al,26 the male and female subjects were combined in the analysis, which did not reveal a significant difference between groups. We are in agreement with Hamstra-Wright et al13 that the mechanism underlying the increased risk for MTSS as a result of increased hip external rotation ROM is not known at this time. The difference in this risk factor between men and women also remains unclear. We did not find that pooled effect for hip internal ROM was significant, and this factor also exhibited high statistical heterogeneity between studies (I2 = 85%).
Limitations
One feature of this systematic review that differentiates it from other MTSS systematic reviews was our use of a strict definition of MTSS. As stated earlier, for a study to be included in this review, the definition of MTSS used in the study had to include 3 characteristics: (1) pain located along the posteromedial border of the tibia, (2) diffuse pain, and (3) pain that was activity related. This strict definition can be viewed as a limitation of our study as it restricted the number of studies included in our review. However, we believe that this strict definition increased our confidence that the diagnostic entity was consistent across studies and minimized the clinical heterogeneity with respect to the condition of interest.
A second limitation of this meta-analysis is that we used a random-effects model for all pooled effect calculations. We made this decision based on the variations across studies both in terms of participants and how the studies were conducted. As the random-effects model is more conservative than the fixed-effect model, this model is less likely to show significant pooled effects. Newman et al31 made the decision to use random-effects modeling when the I2 value was >25% and to used fixed-effects modeling if the I2 was ≤25%. Hamstra-Wright et al13 used random-effects modeling when the I2 value was ≥20% and used fixed-effects modeling if the I2 was <20%. In this meta-analysis, we found that the 5 factors (years running, history of MTSS, standing foot angle, plantarflexion ROM, and inversion strength) showed a significant pooled effect when we used a fixed-effects model, but the pooled effect was not significant when we used a random-effects model. In all of these cases, the I2 value was >70%. Newman et al31 found both years running and history of MTSS to be significant risk factors using random-effects modeling, whereas we did not find either to have a significant pooled effect. Hamstra-Wright et al13 found plantarflexion to be a significant risk factor using a fixed-effects model based on the heterogeneity of the 4 studies (I2 = 0%), whereas we did not find a significant pooled effect based on the results of the 2 studies that met our inclusion criteria with high heterogeneity (I2 = 85%).
The 2 risk factors that were common to the 2 previously published meta-analyses on MTSS risk factors13,31 and our study are increased navicular drop and increased hip external ROM with hip flexed. Both Newman et al31 and our study also found female sex to be a significant risk factor; Hamstra-Wright et al13 did not study sex as the authors only considered continuous variables. Therefore, these 3 risk factors were common to all 3 systematic reviews with meta-analysis.
Conclusion
This systematic review and meta-analysis revealed 5 risk factors that showed a significant pooled effect and low statistical heterogeneity: female sex, higher weight, higher navicular drop, previous running injury, and greater hip external rotation with the hip in flexion. Based on our strict definition of MTSS and requirement for risk factor measurement consistency, these factors also had low clinical heterogeneity, contributing to our confidence in these findings. The risk factors that did not show a significant pooled effect and had low statistical and clinical heterogeneity were age, height, eversion ROM, inversion ROM, dorsiflexion isometric strength, eversion isometric strength, tibial varum, walking speed, and weekly training mileage. Based on these results, we believe that these factors do not likely increase the risk for MTSS. Identification of risk factors is critical in the prevention of overuse injuries in active individuals, and the pooling of data across multiple studies increases our confidence in those risk factors that need to be considered in preventative strategies.
Supplementary Material
Footnotes
The authors report no potential conflicts of interest in the development and publication of this article.
References
- 1. Bandholm T, Boysen L, Haugaard S, Zebis MK, Bencke J. Foot medial longitudinal-arch deformation during quiet standing and gait in subjects with medial tibial stress syndrome. J Foot Ankle Surg. 2008;47:89-95. [DOI] [PubMed] [Google Scholar]
- 2. Bartosik KE, Sitler M, Hillstrom HJ, Palamarchuk H, Huxel K, Kim E. Anatomical and biomechanical assessments of medial tibial stress syndrome. J Am Podiatr Med Assoc. 2010;100:121-132. [DOI] [PubMed] [Google Scholar]
- 3. Bennett JE, Reinking MF, Pluemer B, Pentel A, Seaton M, Killian C. Factors contributing to the development of medial tibial stress syndrome in high school runners. J Orthop Sports Phys Ther. 2001;31:504-510. [DOI] [PubMed] [Google Scholar]
- 4. Borenstein M, Hedges LV, Higgins JPT, Rothstein HR. Introduction to Meta-Analysis. Chichester, UK: Wiley; 2009. [Google Scholar]
- 5. Burne SG, Khan KM, Boudville PB, et al. Risk factors associated with exertional medial tibial pain: a 12 month prospective clinical study. Br J Sports Med. 2004;38:441-445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Chowdhury PP, Mawokomatanda T, Xu F, et al. Surveillance for certain health behaviors, chronic diseases, and conditions, access to health care, and use of preventive health services among states and selected local areas—Behavioral Risk Factor Surveillance System, United States, 2012. MMWR Surveill Summ. 2016;65:1-142. [DOI] [PubMed] [Google Scholar]
- 7. Clement DB. Tibial stress syndrome in athletes. J Sports Med. 1974;2:81-85. [DOI] [PubMed] [Google Scholar]
- 8. Degen RM, Hoppe DJ, Petrisor BA, Bhandari M. Making decisions about prognosis in evidence-based practice. Hand Clin. 2009;25:59-66. [DOI] [PubMed] [Google Scholar]
- 9. Eickhoff CA, Hossain SA, Slawski DP. Effects of prescribed foot orthoses on medial tibial stress syndrome in collegiate cross-country runners. Clin Kines. 2000;54(4):76-80. [Google Scholar]
- 10. Franklyn M, Oakes B, Field B, Wells P, Morgan D. Section modulus is the optimum geometric predictor for stress fractures and medial tibial stress syndrome in both male and female athletes. Am J Sports Med. 2008;36:1179-1189. [DOI] [PubMed] [Google Scholar]
- 11. Gaeta M, Minutoli F, Vinci S, et al. High-resolution CT grading of tibial stress reactions in distance runners. AJR Am J Roentgenol. 2006;187:789-793. [DOI] [PubMed] [Google Scholar]
- 12. Guyatt G, Rennie D, Meade MO, Cook DJ. Users’ Guides to the Medical Literature: Essentials of Evidence-Based Clinical Practice. 2nd ed. New York, NY: McGraw-Hill Medical; 2008. [Google Scholar]
- 13. Hamstra-Wright KL, Bliven KC, Bay C. Risk factors for medial tibial stress syndrome in physically active individuals such as runners and military personnel: a systematic review and meta-analysis. Br J Sports Med. 2015;49:362-369. [DOI] [PubMed] [Google Scholar]
- 14. Hayden JA, Cote P, Bombardier C. Evaluation of the quality of prognosis studies in systematic reviews. Ann Intern Med. 2006;144:427-437. [DOI] [PubMed] [Google Scholar]
- 15. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557-560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Hubbard TJ, Carpenter EM, Cordova ML. Contributing factors to medial tibial stress syndrome: a prospective investigation. Med Sci Sports Exerc. 2009;41:490-496. [DOI] [PubMed] [Google Scholar]
- 17. Johnson NB, Hayes LD, Brown K, Hoo EC, Ethier KA; Centers for Disease Control and Prevention (CDC). CDC National Health Report: leading causes of morbidity and mortality and associated behavioral risk and protective factors—United States, 2005-2013. MMWR Suppl. 2014;63(4):3-27. [PubMed] [Google Scholar]
- 18. Lee SY. Direct and Indirect Effects of Alignment, Range of Motion, and Gait Measures on Medial Tibial Stress Syndrome Status of Runners [dissertation]. Charlottesville: University of Virginia; 2009. [Google Scholar]
- 19. Madeley L, Munteanu S, Bonanno D. Endurance of the ankle joint plantar flexor muscles in athletes with medial tibial stress syndrome: a case-control study. J Sci Med Sport. 2007;10:356-362. [DOI] [PubMed] [Google Scholar]
- 20. Magnusson HI, Ahlborg HG, Karlsson C, Nyquist F, Karlsson MK. Low regional tibial bone density in athletes with medial tibial stress syndrome normalizes after recovery from symptoms. Am J Sports Med. 2003;31:596-600. [DOI] [PubMed] [Google Scholar]
- 21. Magnusson HI, Westlin NE, Nyqvist F, Gardsell P, Seeman E, Karlsson MK. Abnormally decreased regional bone density in athletes with medial tibial stress syndrome. Am J Sports Med. 2001;29:712-715. [DOI] [PubMed] [Google Scholar]
- 22. Mak K, Kum CK. How to appraise a prognostic study. World J Surg. 2005;29:567-569. [DOI] [PubMed] [Google Scholar]
- 23. McPoil TG, Cornwall MW. The relationship between static lower extremity measurements and rearfoot motion during walking. J Orthop Sports Phys Ther. 1996;24:309-314. [DOI] [PubMed] [Google Scholar]
- 24. Messier SP, Pittala KA. Etiologic factors associated with selected running injuries. Med Sci Sports Exerc. 1988;20:501-505. [PubMed] [Google Scholar]
- 25. Michael RH, Holder LE. The soleus syndrome: a cause of medial tibial stress (shin splints). Am J Sports Med. 1985;13:87-94. [DOI] [PubMed] [Google Scholar]
- 26. Moen MH, Bongers T, Bakker EW, et al. Risk factors and prognostic indicators for medial tibial stress syndrome. Scand J Med Sci Sports. 2012;22:34-39. [DOI] [PubMed] [Google Scholar]
- 27. Moen MH, Tol JL, Weir A, Steunebrink M, De Winter TC. Medial tibial stress syndrome: a critical review. Sports Med. 2009;39:523-546. [DOI] [PubMed] [Google Scholar]
- 28. Moons KG, Royston P, Vergouwe Y, Grobbee DE, Altman DG. Prognosis and prognostic research: what, why, and how? BMJ. 2009;338:b375. [DOI] [PubMed] [Google Scholar]
- 29. Mueller MJ, Host JV, Norton BJ. Navicular drop as a composite measure of excessive pronation. J Am Podiatr Med Assoc. 1993;83:198-202. [DOI] [PubMed] [Google Scholar]
- 30. National Institutes of Health, National Heart, Lung, and Blood Institute. Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults: The Evidence Report. Bethesda, MD: National Institutes of Health; 1998. [Google Scholar]
- 31. Newman P, Witchalls J, Waddington G, Adams R. Risk factors associated with medial tibial stress syndrome in runners: a systematic review and meta-analysis. Open Access J Sports Med. 2013;4:229-241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Plisky MS, Rauh MJ, Heiderscheit B, Underwood FB, Tank RT. Medial tibial stress syndrome in high school cross-country runners: incidence and risk factors. J Orthop Sports Phys Ther. 2007;37:40-47. [DOI] [PubMed] [Google Scholar]
- 33. Puranen J. The medial tibial syndrome: exercise ischaemia in the medial fascial compartment of the leg. J Bone Joint Surg Br. 1974;56-B:712-715. [DOI] [PubMed] [Google Scholar]
- 34. Raissi GR, Cherati AD, Mansoori KD, Razi MD. The relationship between lower extremity alignment and medial tibial stress syndrome among non-professional athletes. Sports Med Arthrosc Rehabil Ther Technol. 2009;1:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Rathleff MS, Kelly LA, Christensen FB, Simonsen OH, Kaalund S, Laessoe U. Dynamic midfoot kinematics in subjects with medial tibial stress syndrome. J Am Podiatr Med Assoc. 2012;102:205-212. [DOI] [PubMed] [Google Scholar]
- 36. Rathleff MS, Samani A, Olesen CG, Kersting UG, Madeleine P. Inverse relationship between the complexity of midfoot kinematics and muscle activation in patients with medial tibial stress syndrome. J Electromyogr Kinesiol. 2011;21:638-644. [DOI] [PubMed] [Google Scholar]
- 37. Sharma J, Golby J, Greeves J, Spears IR. Biomechanical and lifestyle risk factors for medial tibia stress syndrome in army recruits: a prospective study. Gait Posture. 2011;33:361-365. [DOI] [PubMed] [Google Scholar]
- 38. Slocum DB. The shin splint syndrome: medical aspects and differential diagnosis. Am J Surg. 1967;114:875-881. [DOI] [PubMed] [Google Scholar]
- 39. Sommer HM, Vallentyne SW. Effect of foot posture on the incidence of medial tibial stress syndrome. Med Sci Sports Exerc. 1995;27:800-804. [PubMed] [Google Scholar]
- 40. Straus SE, McAlister FA. A clinician’s guide to journal articles about prognosis. ACP J Club. 1999;130(3):A13-A15. [PubMed] [Google Scholar]
- 41. Tweed JL, Campbell JA, Avil SJ. Biomechanical risk factors in the development of medial tibial stress syndrome in distance runners. J Am Podiatr Med Assoc. 2008;98:436-444. [DOI] [PubMed] [Google Scholar]
- 42. Viitasalo JT, Kvist M. Some biomechanical aspects of the foot and ankle in athletes with and without shin splints. Am J Sports Med. 1983;11:125-130. [DOI] [PubMed] [Google Scholar]
- 43. Yagi S, Muneta T, Sekiya I. Incidence and risk factors for medial tibial stress syndrome and tibial stress fracture in high school runners. Knee Surg Sports Traumatol Arthrosc. 2013;21:556-563. [DOI] [PubMed] [Google Scholar]
- 44. Yates B, White S. The incidence and risk factors in the development of medial tibial stress syndrome among naval recruits. Am J Sports Med. 2004;32:772-780. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.