Abstract
Context:
Sudden cardiac death (SCD) in a young athlete is a tragic event and is the leading medical cause of death in this population. The precise incidence of SCD in young athletes has been subject of debate, with studies reporting drastically different rates (1:917,000 athlete-years (AYs) to 1:3000 AYs) depending on the methodological design of the investigation or the targeted population.
Evidence Acquisition:
A literature search was performed in PubMed using the terms: incidence, sudden cardiac death, sudden death, sudden cardiac arrest, etiology, pathology, registry, athlete, young, children, and adolescents. Articles were reviewed for relevance and included if they contained information on the incidence of SCD in athletes or young persons up to the age of 35 years.
Study Design:
Clinical review.
Level of Evidence:
Level 5.
Results:
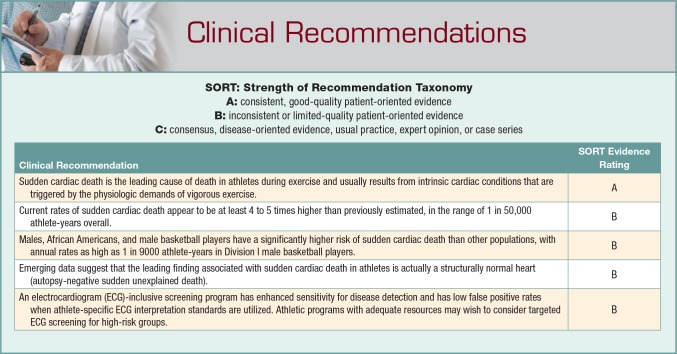
Studies of high quality and rigor consistently yield an incidence of 1:50,000 AYs in college athletes and between 1:50,000 and 1:80,000 AYs for high school athletes, with certain subgroups that appear to be at particularly high risk, including the following: men, basketball players, and African Americans. Initial reports suggest that the most common cause of SCD is hypertrophic cardiomyopathy (HCM). However, more comprehensive investigations in the United States and international populations—athletes, nonathletes, and military—support that the most common finding on autopsy in young individuals with SCD is actually a structurally normal heart (autopsy-negative sudden unexplained death).
Conclusion:
SCD is the leading cause of death in athletes during exercise and usually results from intrinsic cardiac conditions that are triggered by the physiologic demands of vigorous exercise. Current rates of SCD appear to be at least 4 to 5 times higher than previously estimated, with men, African Americans, and male basketball players being at greatest risk. Emerging data suggest that the leading finding associated with SCD in athletes is actually a structurally normal heart (autopsy-negative sudden unexplained death).
Keywords: athlete, incidence, etiology, cardiovascular screening
Sudden cardiac death (SCD) during sport is a tragic event that has a significant impact on friends, families, communities, and athletic departments. Athletic trainers play a pivotal role in the prevention, management, and aftermath of sudden cardiac arrest (SCA) in young athletes. As such, it is critical for this group to be familiar with the latest research related to SCD in this population. The objective of this article is to provide a comprehensive review of the incidence and etiology of SCD in young athletes and offer a framework for how this might relate to SCD prevention programs.
Methods
A literature search was performed in PubMed using the following terms: incidence, sudden cardiac death, sudden death, sudden cardiac arrest, etiology, pathology, registry, athlete, young, children, and adolescents. Articles were reviewed for relevance and included if they contained information on the incidence of SCD in athletes or young persons up to the age of 35 years. The reference lists from each article were reviewed for other relevant material. This information was synthesized and included in the following review.
SCD is defined as a sudden unexpected death due to cardiac causes, or sudden death in a structurally normal heart that had no other explanation and a history consistent with cardiac-related death, that occurred within 1 hour of symptom onset in a person without known cardiac disease or an unwitnessed death occurring within 24 hours of the person having been alive and symptom free. SCA is defined as an instance where a heart stopped beating unexpectedly but the individual was revived and survived the event.
The Importance of Numerators and Denominators
The incidence of SCD in athletes has been widely debated. Rates as high as 1 in 3000 athlete-years (AYs) have been reported in National Collegiate Athletic Association (NCAA) Division I male basketball players, while 1 study in Minnesota high school athletes estimated the rate of SCD to be as low as 1:917,000 AYs.20,44 Multiple factors influence the calculation needed to provide an incidence of SCD. Heterogeneity in current estimates is related primarily to differences in methodology and variations in the populations being studied. Understanding the factors involved with developing incidence numbers is critically important when evaluating the literature.
An accurate rate hinges on a precise numerator (cases identified) and a defined denominator (population). Studies that use estimates of numerators, denominators, or both are at high risk for erroneous reporting of the incidence of SCD. Specific elements that can affect numerators and denominators include the following: the definition of an athlete, type of athlete, age of the population being studied, data acquisition (eg, media reports, insurance claims, registries, etc), whether data reporting is mandatory versus voluntary, inclusion or exclusion of certain cardiac events based on time and location, lack of standardization for autopsy protocols, and whether calculations include SCDs only versus SCDs + SCAs.23
Including Exertional Deaths Versus All Deaths: Does it Matter?
SCD is the leading cause of death during exertion, with the majority (60%) of SCD cases occurring during exercise.20 However, pathological conditions associated with SCD can manifest with lethal arrhythmias during rest or sleep. Since the athlete health care team is responsible for the overall health of the athlete in any setting, incidence of SCD calculations should ideally include deaths that occur both inside and outside of sport.
Questions exist regarding the relative risk of SCD in competitive athletes versus the general population. Much of this is due to the heterogeneous nature of studies within the athletic and general populations, and current epidemiologic studies do not provide a complete understanding of the comparative risk of SCA/D in athletes versus nonathletes. It is generally accepted that exercise and intense physical exertion is a trigger for SCA in those with underlying cardiovascular abnormalities and is the basis for cardiovascular screening currently performed in athletes. An Italian study identified a 2.5-times relative risk for SCD in adolescents and young adults engaged in competitive sports versus an age-matched nonathletic population, and a French investigation found the relative risk of sports-related sudden death was 4.5 times greater in competitive young athletes ages 10 to 35 years compared with noncompetitive sports participants of the same age.5,26 In addition, a prospective study examining SCA/D in over 4,000,000 US high school youth found athletes were 2.7 times more likely to suffer SCA/D than nonathletes.51 In contrast, studies in Denmark found exertional SCD in competitive athletes to occur less frequently than SCD occurring at any time in the general population.24,43 Differences in SCD rates between high school and college athletes may be due to differences in case identification, selection bias (those with cardiovascular abnormalities are selected out before entering college either because of death or because of an inability to perform at a higher level), or because some cardiomyopathies do not present phenotypically until an athlete is older.
Sudden Cardiac Arrest as an Endpoint
SCA is also an important endpoint to consider when analyzing risk. Historically, there has been variability on whether incidence calculations strictly examine SCD or also include those with SCA. Most estimates include only SCD primarily because it is difficult to capture SCAs using current reporting mechanisms. New public access to defibrillation (PAD) programs have improved survival rates after SCA, which may decrease the overall incidence of SCD.51 However, because primary prevention programs should identify all athletes at risk for SCA, the incidence of both SCA with survival and SCD would be preferred.
Media Reports, Insurance Claims, and Mandatory Reporting Systems: What is the Difference?
One of the major factors involved in incidence calculations is the method of case identification. Mandatory reporting systems offer the most reliable information, but few of these types of programs exist outside of the military. Reporting mechanisms that rely on passive collection methods are at risk for ascertainment and selection bias, which can lead to an underestimation of incidence calculations.
Historically, the most commonly cited values for the incidence of SCD have been between 1:200,000 and 1:300,000 AYs.30,53 Closer examination of study designs for these investigations reveals the potential for missed cases. In 1995, the first study to report on the incidence of SCD in high school and college athletes utilized a retrospective cohort design through the National Center for Catastrophic Sports Injury Research (NCCSIR) database from 1983 to 1993.53 The passive nature of the collection methods, reliance on media reporting for deaths in an era that preceded the Internet, and limitation to deaths that only occurred during school-sponsored sports activities led to incomplete case identification. Additionally, the denominator was estimated, leading to further inaccuracy. Overall, the study assessed the incidence of SCD to be 1:300,000 AYs, with much lower rates in women (1:1,300,000 AYs).53
Another early study of high school athletes utilized a retrospective cohort design but employed a different method of case identification using insurance claims.30 The study focused on Minnesota high school athletes and included only SCDs that occurred during a school-sponsored event and occurred with exertion. This study found an overall incidence of SCD of 1:217,000 AYs.30 This analysis, along with the investigation from the NCCSIR, became starting points for discussions surrounding the incidence of SCD in athletes but included only a subset of deaths.
While studies such as these originally contributed to a previously unchartered area of research, limitations in study design inhibit applicability in the modern era. In fact, more recent studies have shown that media reports and insurance claims are not effective methods for identifying all cases of SCD.20,21 A retrospective study of high-profile collegiate athletes found that media reports identified only 56% of cases even in this heavily scrutinized population.20 In fact, use of media reports for case identification appears to be even more deficient in lower profile athletes. In a recent study, media reports captured 87% of SCD cases in NCAA Division I athletes but only 44% in Division III.20 Similarly, an international study from Denmark reported that only 20% of the athlete deaths identified through death certificate review were found by searching media reports.24 In a follow-up report using analogous methods, the media identified only 2% of sports-related SCD.43 Likewise, insurance claims only capture 11% to 14% of athlete SCDs in the United States.20,21 As a result, relying solely on media searches or insurance claim data for case identification will underestimate the incidence of SCD.
US Collegiate Athletes
Since the incidence of SCD varies considerably with age, it is important to assess populations with more narrowly defined age ranges. The US NCAA athlete population is a well-defined population with approximately 450,000 athletes per year. Demographics and participation rates are published each year in the NCAA Sports Sponsorship and Participation Rates Report and the NCAA Student Athlete Ethnicity Report. In the NCAA population, there have been 4 retrospective cohort investigations examining the incidence of SCD in college athletes aged 17 to 24 years, with rates ranging from 1:43,000 to 1:67,000 AYs.17,20,21,31
An initial study surveyed NCAA institutions and calculated the rate of SCD to be 1:67,000 based on the response of 244 collegiate programs.17 A second study pooled information from the NCAA Resolutions List, deaths captured through a systematic media database, and sudden deaths reported through insurance claims.20 The database initially examined 5 years of data and found an overall rate of SCD to be 1:43,000, with approximately 8 to 10 deaths in the NCAA per year attributed to SCD.20 The 10-year follow-up study between 2003 and 2013 with over 4,000,000 AYs of surveillance found the rate of SCD was 1:53,703 per athlete per year (or 1:13,426 over a 4-year career if the assumption is made that the relative risk for SCD is the same each year).21 Importantly, certain subgroups appear to be at higher risk, including men (1:37,790 AYs; incidence rate ratio, 3.2 compared with women), African American athletes (1:21,491 AYs; incidence rate ratio, 3.2 compared with Caucasian athletes), and basketball players (1:8978 AYs).21 In fact, Division I male basketball players were found to have a rate of SCD of 1:5200 AYs (1:1300 over a 4-year career).21 A study that combined information from the US Registry for Sudden Death in Athletes (USRSDA) and the NCAA Resolutions List between 2002 and 2011 determined the incidence of SCD to be 1:62,000 AYs.31 Despite differing methodology, it appears that the incidence of SCD in collegiate athletes is approximately 1:50,000 AYs (1:12,500 over a 4-year career). Groups such Division I male basketball players (incidence of SCD, 1:1300 over a 4-year career) may be candidates for targeted advanced screening programs. Further investigations are necessary to determine the reasoning for the high rates of death in these groups (Table 1).
Table 1.
Incidence studies in college athletes
| Study | Year | Country | Study Design | Case Identification | Denominator | Exertional Deaths or All? | SCD or SCA + SCD | Years Studied | Incidence a | Age Range, y | Cardiac Deaths, n |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Drezner et al17 | 2005 | US | Retrospective survey | Survey answered by 244/326 (75%) Division I NCAA institutions | Number of athletes at surveyed schools | All | SCD | — | 1:67,000 | — | 5 |
| Harmon et al20 | 2011 | US | Retrospective cohort | Media database + NCAA database + insurance claims | Participation data from NCAA | All | SCD | 2004-2008 | 1:43,000 | 18-26 | 37 |
| Maron et al32 | 2014 | US | Retrospective cohort | US Registry for Sudden Death in Athletes and NCAA Resolutions List for cardiac cases | Participation data from NCAA | All | SCD | 2002-2011 | 1:83,000 confirmed; 1:62,000 presumed | 17-26 | 64 |
| Harmon et al21 | 2015 | US | Retrospective cohort | Media database + NCAA database + insurance claims | Participation data from NCAA | All | SCD | 2003-2013 | 1:56,000 | 17-26 | 79 |
NCAA, National Collegiate Athletic Association; SCA, sudden cardiac arrest; SCD, sudden cardiac death.
All incidence rates in athlete-years.
In August 2014, the NCAA began requiring that all SCAs/SCDs be reported directly to the NCAA Sports Science Institute through the NCCSIR. In the unfortunate case of an SCD, athletic trainers are in the best position to assume the role of acquiring information surrounding the circumstances and history of death, coordinating pertinent information with family members or the athletic department, and reporting deaths directly to the NCAA. Ultimately, this information can be used to better define rates of death and improve policies for prevention.
US High School Athletes
The high school age (14-18 years) offers another well-defined group that could potentially be studied. The primary challenge, however, has been heterogeneity of case identification methods. As a result, there is wide variation in reported rates, which range from 1:23,000 to 1:917,000 AYs17,44 (Table 2).
Table 2.
Incidence studies in high school students
| Study | Year Published | Country | Study Design | Case Identification | Denominator | Exertional Deaths or All? | SCD or SCA + SCD | Years studied | Incidence a | Age Range, y | Mean Age, y | Cardiac Deaths, n |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Drezner et al16 | 2009 | US | Cross-sectional survey | 1710 high schools with AEDs surveyed for SCA or SCD | Number of student athletes reported by schools | SCA or SCD occurring on campus | SCA + SCD | 2006-2007 | 1:23,000 SCA + SCD, 1:46,000 SCD | 14-17 | 16 | 14 |
| Maron et al31 | 2013 | US | Retrospective cohort | US Registry of Sudden Death in Athletes | Minnesota State High School League | Exertional | SCD | 1986-2011 | 1:150,000 | 12-18 | 16 | 13 |
| Roberts and Stovitz44 | 2013 | US | Retrospective cohort | Insurance claims data | Minnesota State High School League | Exertional during school-sponsored sport | SCD | 1993-2012 | 1:416,666, over last decade 1:917,000 | 12-19 | — | 4 |
| Toresdahl et al51 | 2014 | US | Prospective observational | 2149 schools followed for SCA + SCD that occurred on school campus | Number of student athletes reported by schools | SCA or SCD occurring on campus | SCA + SCD | 2009-2011 | 1:87,719 SCA + SCD, 1:57,000 male SCA + SCD | 14-18 | — | 18 SCA + SCD, 2 SCD |
| Drezner et al15 | 2014 | US | Retrospective cohort | Media reports | NFHS | All | SCA + SCD | 2003-2013 | 1:153,846 SCD, 1:71,428 SCA, 1:21,277 male basketball | 14-18 | — | 6 SCD, 7 SCD |
AED, automated external defibrillator; NFHS, National Federation of State High School Associations; SCA, sudden cardiac arrest; SCD, sudden cardiac death.
All incidence rates are in athlete-years.
An examination of incidence calculations in the state of Minnesota provides insight into some of the dilemmas. A recent study of Minnesota athletes limited to insurance claims over a 19-year period reported an incidence of 1:417,000 AYs (4 cases of SCD), with an incidence of 1:917,000 AYs over the past decade.44 However, insurance claims capture deaths that occur during school-sponsored events or practices only, which means that they are likely to significantly underestimate the incidence of SCD. In fact, to highlight this point, a retrospective review of the same Minnesota high school athlete population over the past decade found 13 cardiac cases through media reports (6 cases of SCD + 7 cases of SCA) compared with the 1 reported by an insurance claim.16 Several of the deaths that did not result in an insurance claim occurred while athletes were exercising during club sports participation. Interestingly, during a similar time period, the USRSDA identified 13 deaths during an overlapping 26 years, which emphasizes the limitations of insurance claims as a sole method for case identification.31
Other studies have found higher rates of SCD in high school athletes, including a cross-sectional survey of 1710 high schools where the rate of SCD was 1:46,000 AYs, and 1:23,000 AYs when both SCD and SCA were included.16 A prospective 2-year cross-sectional survey of 2149 high schools demonstrated a combined rate of SCD and SCA to be 1:88,000 AYs.51 Still, the inclusion of only school-based events limits the ability to capture deaths that occur during club sports or while sleeping.
These studies highlight the complexity of calculating incidence rates in the high school population, especially given the differences in variables and data collection methods. Many of the investigations examined deaths during school hours, focused on deaths during school-sponsored activities, included cases of death but not cardiac arrest, or relied on media reports or insurance claims for case identification. These inherent study design limitations result in missed cardiovascular events and an underestimation in incidence calculations. Based on the best-available evidence, however, the rate of SCD in high school athletes, at a minimum, appears to be 1:50,000 AYs to 1:80,000 AYs.
The Military and Other Countries
A comprehensive study of military personnel provides an example of an ideal investigation given the defined target population, mandatory reporting of death, and standardized postmortem protocols. A rate of SCD of 1:25,000 person-years was found in those younger than 35 years over a 10-year period and 15.2 million person-years of active surveillance.19 An investigation of military recruits, which may simulate the intense training of young athletes and is another well-defined population, demonstrated the rate of SCD to be 1:10,000 recruit-years.18
In the Veneto region of Italy, a mandatory reporting mechanism exists and athletes are required to register in the system, resulting in both an accurate numerator and denominator. A prospective study from 1979 to 1999 found the rate of SCD was 1:47,000 in athletes aged 12 to 35 years prior to the use of advanced cardiovascular screening, which mirrors the rate found in US collegiate athletes.6 Interestingly, the rate of SCD for this Italian subset of athletes dropped by 89% after the implementation of an electrocardiogram (ECG)-inclusive screening program. An Israeli study using a retrospective search of 2 newspapers for case identification (numerator) and an estimation for population size (denominator) between the years 1985 and 2009 found the rate of SCD in this cohort to be 1:38,000 AYs, although the reliance on media reports and estimated denominator may not result in an accurate incidence.47 Both the Italian and Israeli studies support that the rates of SCD are likely much higher than originally reported; however, it is worth noting that these populations may differ compared with the United States (Table 3).
Table 3.
Incidence studies in the military and general population
| Study | Year | Country | Study Design | Case Identification | Denominator | Exertional Deaths or All? | SCD or SCA + SCD | Years Studied | Population | Incidence a | Age Range, y | Cardiac Deaths, n |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Corrado et al6 | 2003 | Italy | Prospective cohort study | Mandatory death reporting | Registered Italian athletes | All | SCD | 1979-1999 | Athletes and young people | 1:47,600 athletes, 1:142,900 young people | 12-35 | 55 |
| Eckart et al18 | 2004 | US | Retrospective cohort | Mandatory reporting of all deaths to DoD recruit mortality registry with autopsy data | Numbers from DoD | All | SCD | 1977-2001 | Military recruits | 1:10,000 b | 18-35 | 108 |
| Eckart et al19 | 2011 | US | Retrospective cohort | Mandatory reporting of all deaths to DoD mortality registry with autopsy data | DoD statistics | All | SCD | 1998-2008 | Military | < 20 y, 1:29,673 20-24 y, 1:40,983 25-29 y, 1:30,120 30-35 y, 1:25,000 | 18-34 | 298 |
| Steinvil et al47 | 2011 | Israel | Retrospective cohort | Retrospective review of 2 Israeli newspapers by 2 media researchers | 45,000 registered competitive athletes in 2009, extrapolated the growth of the Israeli population age10-40 y since 1985 based on that figure and allowed for a presumed doubling of the sporting population | All | SCD | 1985 - 1997 1998 - 2009 | Athletes | 1st: 1:39,370 2nd: 1:37,593 | 12-44 | 24 |
DoD, Department of Defense; SCA, sudden cardiac arrest; SCD, sudden cardiac death.
Unless noted otherwise, all incidence rates in person-years.
Incidence is in recruit-years and represents an annual risk.
Hypertrophic Cardiomyopathy Versus Sudden Unexplained Death
Hypertrophic cardiomyopathy (HCM) has typically been reported as the most common etiology of SCD in the United States; however, more recent information casts doubt on this assumption. In 2009, a 25-year analysis of 1866 deaths from the USRSDA were analyzed, and 36% of cardiovascular deaths were reported due to HCM.29 A closer look at this investigation reveals that 1049 deaths were presumed due to an inherited cardiovascular disorder. However, 359 of these deaths were excluded from the final analysis despite being considered cardiac in nature. Those deaths were removed because there were no structural abnormalities present on postmortem examination or no autopsy was available.29 It is unclear how many of the 359 cases had structurally normal hearts or how many autopsies were missing; however, if those deaths are included in the cohort as sudden unexplained death (SUD), then SUD represents 34% of the total cardiovascular deaths and HCM 24%.
Data supporting autopsy-negative SUD as the leading finding associated with SCD can be found in national and international investigations.18,19,22,24,25,41,48 This includes athletes,22,24 nonathletes,36 the general population,25,41 and the military.18,19,24 For example, an Italian study between 1979 and 1996 demonstrated 49 cases of SCD (44 men, 5 women; mean age, 23 years) and found that 25% of cases were associated with a structurally normal heart, with only 1 death (2%) attributed to hypertrophic cardiomyopathy.7 Another international study from Denmark between 2000 and 2006 (age range, 12-35 years) reported that the most common discovery associated with SCD was a structurally normal heart (27%), whereas HCM only accounted for 7% of cases.24 Similar findings were reported in a retrospective analysis in the United Kingdom between 1996 and 2008 (mean age, 28 years), where 23% of deaths were associated with a structurally normal heart but only 11% with HCM9 (Table 4).
Table 4.
Studies of the etiologies of sudden cardiac death in young people
| Study | Year | Country | Exertional Death vs All Deaths | Population | Age Range, y | Number of Deaths | HCM, % | AN-SUD, % |
|---|---|---|---|---|---|---|---|---|
| Studies in athletes | ||||||||
| Corrado et al6 | 2003 | Italy | All | Competitive athletes | 12-35 | 55 | 2 | 7 |
| de Noronha et al10 | 2009 | UK | All | Athletes | 1-35 | 89 | 12 | 19 |
| Maron et al29 | 2009 | US | All | Athletes | 8-39 | 690 | 36 | — |
| Holst et al24 | 2010 | Denmark | Exertional | Competitive athletes | 12-35 | 15 | 0 | 27 |
| Suarez-Mier et al48 | 2011 | Spain | Exertional | Recreational athletes | 9-35 | 81 | 10 | 23 |
| Harmon et al20 | 2011 | US | All | Competitive athletes | 18-26 | 36 | 3 | 32 |
| Harmon et al21 | 2015 | US | All | Competitive athletes | 17-26 | 64 | 8 | 25 |
| Studies in the general population | ||||||||
| Corrado et al5 | 2006 | Italy | All | General population | 1-35 | 269 | 7 | 15 |
| Puranik et al41 | 2005 | Australia | All | General population | 5-35 | 241 | 6 | 29 |
| Papadakis et al38 | 2009 | UK | All | General population | 1-35 | 3409 | 5 | 14 |
| Solberg et al46 | 2010 | Norway | Exertional | General population | 15-34 | 23 | 4 | 9 |
| Margey et al25 | 2011 | Ireland | All | General population | 15-35 | 116 | 15 | 27 |
AN-SUD, autopsy-negative sudden unexplained death; HCM, hypertrophic cardiomyopathy.
Studies in US collegiate athletes have yielded conflicting results. In 1 retrospective study from 2002 to 2011 using data from the USRSDA, autopsies from 47 cases of athlete SCD were reviewed and reported 27% of cases with a structurally normal heart, while 33% had autopsy findings consistent with HCM.31 Another retrospective study of the same population during a similar 10-year period (2003-2013) reviewed autopsies using a multidisciplinary panel of cardiac pathologists, cardiologists, and sports medicine physicians.21 The most common finding at death in this study was a structurally normal heart (25%), whereas confirmed HCM was present in only 8% of cases.21 Reasons for the discrepant results could include referral bias, inclusion of varying SCD cases, or differing pathologic criteria. Common causes for sudden cardiac death in young athletes are included in Table 5.
Table 5.
Causes of sudden cardiac death in young athletes
| Cause | Prevalence |
|---|---|
| Hypertrophic cardiomyopathy | 1:500 |
| Arrhythmogenic right ventricular cardiomyopathy | 1:2000 to 1:5000 |
| Dilated cardiomyopathy | 1:2500 |
| Coronary artery anomaly | 1:100 |
| Marfan syndrome | 1:5000 |
| Bicuspid aortic valve | 1:100 |
| Long QT syndrome | 1:2500 |
| Wolff-Parkinson-White | 1:750 |
| Brugada syndrome | 1:2000 to 1:5000 |
| Catecholaminergic polymorphic ventricular tachycardia | 1:10,000 |
| Short QT syndrome | 1:2000 |
Difficulty with Autopsy Data
The lack of standardized autopsy protocols has hampered the ability to accurately attribute a cause of death during an SCD. In 1 study from the United Kingdom, 720 consecutive cases of young patients who suffered an SCD were referred from coroners and pathologists to a specialized cardiac pathologist.9 The most common diagnosis yielded by the cardiac pathologist was a structurally normal heart (45%), followed by cardiomyopathy (29%), and coronary artery anomaly (10%).9 Interestingly, there was disparity in the diagnosis produced by the referring pathologist and the specialized pathologist in 41% of cases, suggesting diagnosis by a nonspecialist may not be accurate.9 Current autopsy data in the United States are also limited by the lack of standardized autopsy protocols, differences in training of local coroners and medical examiners, and budget limitations in autopsy investigations. Therefore, etiology studies relying on local autopsy reports are limited.
Implications for Screening
A precise understanding of the incidence and etiology of SCD in athletes is important to develop appropriately targeted prevention strategies. While initial incidence calculations estimated SCD to be in the range of 1:200,000 to 1:300,000 AYs, more reliable studies demonstrate rates that are at least several-fold higher, around 1:50,000 AYs. SCD occurs despite the majority of athletes—especially in the college setting where it is a requirement—receiving standardized cardiovascular screening as part of a preparticipation examination with a history and physical. Part of the difficulty in identifying those at risk is that the majority of athletes (60%-80%) are asymptomatic prior to their arrest.2,4,18,34 Thus, using a symptom-based preparticipation screening strategy poses inherent flaws for detecting those who may suffer SCD. To optimize the ability of clinicians to know which questions/answers raise concern for potentially lethal conditions, require further workup, or referral to a specialist, a 2-part symposium was published through collaboration between primary care sports medicine practitioners and cardiologists. This tool is freely available and is a valuable resource for those who conduct preparticipation examinations.49,50
The athlete health care team must recognize high-risk warning signs and symptoms that may be suggestive of underlying cardiovascular abnormalities and in need of an appropriate workup or referral. These signs and symptoms include those who present with exertional syncope, unexplained seizures, or a family history of early sudden death.14 The importance of a positive family history was demonstrated in a large epidemiologic study from Denmark that identified all SCD victims aged 1 to 35 years between 2000 and 2006 and prospectively compared the standardized incidence ratios (SIRs) of cardiovascular disease in their first- and second-degree relatives with that of the rest of the population. In the 11-year follow-up period, the SIR was highest among first-degree relatives younger than 35 years in which the risk for cardiomyopathy and ventricular arrhythmias was an astonishing 17.91 and 19.15, respectively.1,42 Additional research is needed to improve the sensitivity and specificity of the medical history questions used during cardiovascular screening, but a family history of SCD in those younger than 35 years may be an important predictor of SCD.
There is debate regarding the inclusion of a 12-lead ECG into preparticipation screening. The ECG offers enhanced sensitivity to detect diseases at risk for SCD, and many American professional sporting organizations (National Football League, Major League Baseball, National Basketball Association, Major League Soccer, National Hockey League) as well as FIFA and the International Olympic Committee have adopted the policy to include an ECG during cardiovascular screening.
The American Heart Association supports ECG screening programs that are locally driven, systematically organized, and well supported.27,35 Most would agree that the ECG has an increased ability to detect cardiovascular disease compared with the traditional history and physical while providing a more objective assessment of cardiac disease. The ECG has been shown to detect more than 95% of cases of SCD caused by HCM and has a negative predictive value that approaches 100% for the major diseases of HCM, long QT syndrome, and Wolff-Parkinson-White syndrome.33,45 As such, the ECG appears to be a practical screening tool for structural abnormalities, ion channel disorders, and inherited arrhythmias. Concerns of an ECG screening program have historically included high false-positive rates, low cost-effectiveness, and lack of sufficient infrastructure to conduct screening.
Early concerns with ECG screening were largely related to high false-positive rates, which lead to poor cost efficiency. When traditional ECG interpretation parameters were used to interpret athlete ECGs, the false positive rates were reported to be as high as 15% to 40%.28,39 However, athlete-specific ECG interpretation standards that account for physiologic changes associated with exercise have the capability to reduce false-positive rates and improve cost efficiency.11 Several recent consensus statements detail the difference between normal physiologic changes in response to exercise from findings suggesting cardiac pathology.8,12,13,17,52 With these guidelines, false positive rates for ECG screening in athletes have been dramatically reduced to rates that are lower than other lethal diseases (eg, breast cancer).37 For example, a comprehensive cardiovascular screening study in high school athletes where every athlete received a history, physical examination, ECG, and echocardiogram demonstrated that an ECG interpreted with modern interpretation standards yielded a false-positive rate of only 2.8%.40 Further studies with refined ECG interpretation parameters may continue to reduce false positive rates; however, caution is required to avoid doing so at the expense of the sensitivity of the screening tool. While an ECG does not detect all cardiac pathology, such as coronary artery anomalies or dilated aortic roots, it does provide enhanced disease detection for the most common cardiomyopathies, arrhythmias, and channelopathies known to cause SCD in athletes.
The primary difficulty in implementing ECG screening in the United States is the development of an infrastructure to appropriately obtain and interpret the ECG, as well as what specific steps (eg, referral, secondary testing, etc) to take when an abnormal result is obtained.11 Other concerns about adding an ECG to the screening process include accurate and reliable interpretation along with a concern for adding false-positive results to the overall preparticipation examination screening process. Last, the natural history of cardiac diseases in athletes is largely unknown, with limited outcomes-based data. This is true for diseases that might be detected with history and physical examination or through an ECG, which might question the utility of screening by any method.
For those who do wish to perform ECG screening, infrastructure development is key. A large portion of this infrastructure development must include appropriate athletic trainer and physician education and training in athlete-specific ECG interpretation standards. Comprehensive online training modules for ECG interpretation in athletes are freely accessible for programs that opt to use modern ECG interpretation standards during screening.3
As demonstrated in the NCAA incidence studies, current data from the National Center for Catastrophic Injury Research, and past data from the US National Registry for Sudden Death in Sports, there are some athlete groups (male basketball, football, and soccer players) that comprise approximately 75% of all SCDs and present the highest risk groups. Since the current strategy of screening with a history and physical is limited in the ability to detect disease, one option could be to perform advanced screening broadly across the athletic population. On the other hand, another strategy might include using advanced screening protocols in groups that are deemed high-risk based on the incidence data. Institutions need to consider the politics of screening individual groups; however, the rate of SCD in high-risk populations seems to warrant the consideration for innovative and advanced cardiac screening measures. Given the resources and oversight, this type of screening might be easier to perform in the collegiate setting. If ECG screening is performed, it is imperative that clinicians complete training in ECG interpretation and collaborate with cardiology consultants to provide oversight and resources for the secondary investigation of potential abnormalities. Ultimately, this will lead to the development of an improved standard of cardiovascular care for the athlete.
Conclusion
As the central player in the athlete health care team, athletic trainers must understand the epidemiology of conditions that can cause significant morbidity and mortality in the athletic population. Emerging data support that SCD occurs at a much higher rate compared with traditional estimates and that the leading finding associated with SCD is a structurally normal heart (autopsy-negative SUD). Ultimately, this information may bear importance when developing new SCD prevention strategies, especially for those at highest risk.
Footnotes
The authors report no potential conflicts of interest in the development and publication of this article.
References
- 1. Asif IM, Drezner JA. Detecting occult cardiac disease in athletes: history that makes a difference. Br J Sports Med. 2013;47:669. [DOI] [PubMed] [Google Scholar]
- 2. Basso C, Maron BJ, Corrado D, Thiene G. Clinical profile of congenital coronary artery anomalies with origin from the wrong aortic sinus leading to sudden death in young competitive athletes. J Am Coll Cardiol. 2000;35:1493-1501. [DOI] [PubMed] [Google Scholar]
- 3. BMJ Learning. ECG interpretation in athletes. http://learning.bmj.com/learning/course-intro/.html?courseId=10042239. Accessed January 26, 2017.
- 4. Corrado D, Basso C, Fontaine G. Clinical profile of young competitive athletes who died suddenly of arrhythmogenic right ventricular cardiomyopathy/dysplasia: a multicenter study. Pacing Clin Electrophysiol. 2002;25:544. [Google Scholar]
- 5. Corrado D, Basso C, Pavei A, Michieli P, Schiavon M, Thiene G. Trends in sudden cardiovascular death in young competitive athletes after implementation of a preparticipation screening program. JAMA. 2006;296:1593-1601. [DOI] [PubMed] [Google Scholar]
- 6. Corrado D, Basso C, Rizzoli G, Schiavon M, Thiene G. Does sports activity enhance the risk of sudden death in adolescents and young adults? J Am Coll Cardiol. 2003;42:1959-1963. [DOI] [PubMed] [Google Scholar]
- 7. Corrado D, Basso C, Schiavon M, Thiene G. Screening for hypertrophic cardiomyopathy in young athletes. N Engl J Med. 1998;339:364-369. [DOI] [PubMed] [Google Scholar]
- 8. Corrado D, Pelliccia A, Heidbuchel H, et al. Recommendations for interpretation of 12-lead electrocardiogram in the athlete. Eur Heart J. 2010;31:243-259. [DOI] [PubMed] [Google Scholar]
- 9. de Noronha SV, Behr ER, Papadakis M, et al. The importance of specialist cardiac histopathological examination in the investigation of young sudden cardiac deaths. Europace. 2014;16:899-907. [DOI] [PubMed] [Google Scholar]
- 10. de Noronha SV, Sharma S, Papadakis M, Desai S, Whyte G, Sheppard MN. Aetiology of sudden cardiac death in athletes in the United Kingdom: a pathological study. Heart. 2009;95:1409-1414. [DOI] [PubMed] [Google Scholar]
- 11. Drezner JA. ECG screening in athletes: time to develop infrastructure. Heart Rhythm. 2011;8:1560-1561. [DOI] [PubMed] [Google Scholar]
- 12. Drezner JA, Ackerman MJ, Anderson J, et al. Electrocardiographic interpretation in athletes: the ‘Seattle Criteria’. Br J Sports Med. 2013;47:122-124. [DOI] [PubMed] [Google Scholar]
- 13. Drezner JA, Fischbach P, Froelicher V, et al. Normal electrocardiographic findings: recognising physiological adaptations in athletes. Br J Sports Med. 2013;47:125-136. [DOI] [PubMed] [Google Scholar]
- 14. Drezner JA, Fudge J, Harmon KG, Berger S, Campbell RM, Vetter VL. Warning symptoms and family history in children and young adults with sudden cardiac arrest. J Am Board Fam Med. 2012;25:408-415. [DOI] [PubMed] [Google Scholar]
- 15. Drezner JA, Harmon KG, Marek JC. Incidence of sudden cardiac arrest in Minnesota high school student athletes: the limitations of catastrophic insurance claims. J Am Coll Cardiol. 2014;63:1455-1456. [DOI] [PubMed] [Google Scholar]
- 16. Drezner JA, Rao AL, Heistand J, Bloomingdale MK, Harmon KG. Effectiveness of emergency response planning for sudden cardiac arrest in United States high schools with automated external defibrillators. Circulation. 2009;120:518-525. [DOI] [PubMed] [Google Scholar]
- 17. Drezner JA, Rogers KJ, Zimmer RR, Sennett BJ. Use of automated external defibrillators at NCAA Division I universities. Med Sci Sports Exerc. 2005;37:1487-1492. [DOI] [PubMed] [Google Scholar]
- 18. Eckart RE, Scoville SL, Campbell CL, et al. Sudden death in young adults: a 25-year review of autopsies in military recruits. Ann Intern Med. 2004;141:829-834. [DOI] [PubMed] [Google Scholar]
- 19. Eckart RE, Shry EA, Burke AP, et al. Sudden death in young adults: an autopsy-based series of a population undergoing active surveillance. J Am Coll Cardiol. 2011;58:1254-1261. [DOI] [PubMed] [Google Scholar]
- 20. Harmon KG, Asif IM, Klossner D, Drezner JA. Incidence of sudden cardiac death in National Collegiate Athletic Association athletes. Circulation. 2011;123:1594-1600. [DOI] [PubMed] [Google Scholar]
- 21. Harmon KG, Asif IM, Maleszewski JJ, et al. Incidence, cause, and comparative frequency of sudden cardiac death in National Collegiate Athletic Association Athletes: a decade in review. Circulation. 2015;132:10-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Harmon KG, Drezner JA, Maleszewski JJ, et al. Pathogeneses of sudden cardiac death in National Collegiate Athletic Association athletes. Circ Arrhythm Electrophysiol. 2014;7:198-204. [DOI] [PubMed] [Google Scholar]
- 23. Harmon KG, Drezner JA, Wilson MG, Sharma S. Incidence of sudden cardiac death in athletes: a state-of-the-art review. Br J Sports Med. 2014;48:1185-1192. [DOI] [PubMed] [Google Scholar]
- 24. Holst AG, Winkel BG, Theilade J, et al. Incidence and etiology of sports-related sudden cardiac death in Denmark—implications for preparticipation screening. Heart Rhythm. 2010;7:1365-1371. [DOI] [PubMed] [Google Scholar]
- 25. Margey R, Roy A, Tobin S, et al. Sudden cardiac death in 14- to 35-year-olds in Ireland from 2005 to 2007: a retrospective registry. Europace. 2011;13:1411-1418. [DOI] [PubMed] [Google Scholar]
- 26. Marijon E, Tafflet M, Celermajer DS, et al. Sports-related sudden death in the general population. Circulation. 2011;124:672-681. [DOI] [PubMed] [Google Scholar]
- 27. Maron BJ. Counterpoint: mandatory ECG screening of young competitive athletes. Heart Rhythm. 2012;9:1897. [DOI] [PubMed] [Google Scholar]
- 28. Maron BJ, Bodison SA, Wesley YE, Tucker E, Green KJ. Results of screening a large group of intercollegiate competitive athletes for cardiovascular disease. J Am Coll Cardiol. 1987;10:1214-1221. [DOI] [PubMed] [Google Scholar]
- 29. Maron BJ, Doerer JJ, Haas TS, Tierney DM, Mueller FO. Sudden deaths in young competitive athletes: analysis of 1866 deaths in the United States, 1980-2006. Circulation. 2009;119:1085-1092. [DOI] [PubMed] [Google Scholar]
- 30. Maron BJ, Gohman TE, Aeppli D. Prevalence of sudden cardiac death during competitive sports activities in Minnesota high school athletes. J Am Coll Cardiol. 1998;32:1881-1884. [DOI] [PubMed] [Google Scholar]
- 31. Maron BJ, Haas TS, Ahluwalia A, Rutten-Ramos SC. Incidence of cardiovascular sudden deaths in Minnesota high school athletes. Heart Rhythm. 2013;10:374-377. [DOI] [PubMed] [Google Scholar]
- 32. Maron BJ, Haas TS, Murphy CJ, Ahluwalia A, Rutten-Ramos S. Incidence and causes of sudden death in U.S. college athletes. J Am Coll Cardiol. 2014;63:1636-1643. [DOI] [PubMed] [Google Scholar]
- 33. Maron BJ, Roberts WC, Epstein SE. Sudden death in hypertrophic cardiomyopathy: a profile of 78 patients. Circulation. 1982;65:1388-1394. [DOI] [PubMed] [Google Scholar]
- 34. Maron BJ, Shirani J, Poliac LC, Mathenge R, Roberts WC, Mueller FO. Sudden death in young competitive athletes. Clinical, demographic, and pathological profiles. JAMA. 1996;276:199-204. [PubMed] [Google Scholar]
- 35. Maron BJ, Thompson PD, Ackerman MJ, et al. Recommendations and considerations related to preparticipation screening for cardiovascular abnormalities in competitive athletes: 2007 update: a scientific statement from the American Heart Association Council on Nutrition, Physical Activity, and Metabolism: endorsed by the American College of Cardiology Foundation. Circulation. 2007;115:1643-1455. [DOI] [PubMed] [Google Scholar]
- 36. Meyer L, Stubbs B, Fahrenbruch C, et al. Incidence, causes, and survival trends from cardiovascular-related sudden cardiac arrest in children and young adults 0 to 35 years of age: a 30-year review. Circulation. 2012;126:1363-1372. [DOI] [PubMed] [Google Scholar]
- 37. Mushlin AI, Kouides RW, Shapiro DE. Estimating the accuracy of screening mammography: a meta-analysis. Am J Prev Med. 1998;14:143-153. [DOI] [PubMed] [Google Scholar]
- 38. Papadakis M, Sharma S, Cox S, Sheppard MN, Panoulas VF, Behr ER. The magnitude of sudden cardiac death in the young: a death certificate-based review in England and Wales. Europace. 2009;11:1353-1358. [DOI] [PubMed] [Google Scholar]
- 39. Pelliccia A, Maron BJ, Culasso F, et al. Clinical significance of abnormal electrocardiographic patterns in trained athletes. Circulation. 2000;102:278-284. [DOI] [PubMed] [Google Scholar]
- 40. Price DE, McWilliams A, Asif IM, et al. Electrocardiography-inclusive screening strategies for detection of cardiovascular abnormalities in high school athletes. Heart Rhythm. 2014;11:442-449. [DOI] [PubMed] [Google Scholar]
- 41. Puranik R, Chow CK, Duflou JA, Kilborn MJ, McGuire MA. Sudden death in the young. Heart Rhythm. 2005;2:1277-1282. [DOI] [PubMed] [Google Scholar]
- 42. Ranthe MF, Winkel BG, Andersen EW, et al. Risk of cardiovascular disease in family members of young sudden cardiac death victims. Eur Heart J. 2013;34:503-511. [DOI] [PubMed] [Google Scholar]
- 43. Risgaard B, Winkel BG, Jabbari R, et al. Burden of sudden cardiac death in persons aged 1 to 49 years: nationwide study in Denmark. Circ Arrhythm Electrophysiol. 2014;7:205-211. [DOI] [PubMed] [Google Scholar]
- 44. Roberts WO, Stovitz SD. Incidence of sudden cardiac death in Minnesota high school athletes 1993-2012 screened with a standardized pre-participation evaluation. J Am Coll Cardiol. 2013;62:1298-1301. [DOI] [PubMed] [Google Scholar]
- 45. Rodday AM, Triedman JK, Alexander ME, et al. Electrocardiogram screening for disorders that cause sudden cardiac death in asymptomatic children: a meta-analysis. Pediatrics. 2012;129:e999-e1010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Solberg EE, Gjertsen F, Haugstad E, Kolsrud L. Sudden death in sports among young adults in Norway. Eur J Cardiovasc Prev Rehabil. 2010;17:337-341. [DOI] [PubMed] [Google Scholar]
- 47. Steinvil A, Chundadze T, Zeltser D, et al. Mandatory electrocardiographic screening of athletes to reduce their risk for sudden death proven fact or wishful thinking? J Am Coll Cardiol. 2011;57:1291-1296. [DOI] [PubMed] [Google Scholar]
- 48. Suarez-Mier MP, Aguilera B, Mosquera RM, Sanchez-de-Leon MS. Pathology of sudden death during recreational sports in Spain. Forensic Sci Int. 2013;226:188-196. [DOI] [PubMed] [Google Scholar]
- 49. The Cardiovascular Preparticipation Evaluation (PPE) for the primary care and sports medicine physician, part I. Curr Sports Med Rep. 2015;14:246. [DOI] [PubMed] [Google Scholar]
- 50. The Cardiovascular Preparticipation Evaluation (PPE) for the primary care and sports medicine physician, part II. Curr Sports Med Rep. 2015;14:333. [DOI] [PubMed] [Google Scholar]
- 51. Toresdahl BG, Rao AL, Harmon KG, Drezner JA. Incidence of sudden cardiac arrest in high school student athletes on school campus. Heart Rhythm. 2014;11:1190-1194. [DOI] [PubMed] [Google Scholar]
- 52. Uberoi A, Stein R, Perez MV, et al. Interpretation of the electrocardiogram of young athletes. Circulation. 2011;124:746-757. [DOI] [PubMed] [Google Scholar]
- 53. Van Camp SP, Bloor CM, Mueller FO, Cantu RC, Olson HG. Nontraumatic sports death in high school and college athletes. Med Sci Sports Exerc. 1995;27:641-647. [PubMed] [Google Scholar]