Abstract
Background:
Injury rates among professional baseball players may reach as high as 5.8 per 1000 encounters, with pitchers being most vulnerable on account of the excessive biomechanical load on the upper extremity during the throwing motion. Anatomically, the shoulder is the most common site of pitching-related injury, accounting for 30.7% of injuries, closely followed by the elbow at 26.3%. Characteristic valgus loading imparts a predictable constellation of stresses on the joint, including medial tension, lateral compression, and posterior medial shearing. The degenerative cohort of tissue changes that result are readily detected on magnetic resonance imaging (MRI). It is not yet known whether such findings predict future placement on the disabled list (DL) in asymptomatic Major League pitchers.
Hypothesis:
Abnormal soft tissue and osseous changes detected on MRI of the throwing elbow in asymptomatic professional pitchers will impart an increased risk of subsequent transfer to the DL in the season after MRI.
Study Design:
Retrospective cohort study.
Level of Evidence:
Level 3.
Methods:
The study aimed to examine a potential association between the total number of innings pitched (approximate lifetime valgus load) and the typical MRI degenerative changes, hypothesizing a rejection of the null hypothesis. A total of 26 asymptomatic professional pitchers from a single Major League Baseball (MLB) organization and its various minor league affiliates underwent MRI of their dominant elbow from 2003 to 2013 as a condition of their contract signing or trade. Twenty-one of those pitchers played at the Major League level while 5 played with the team’s minor league affiliates including both the AA and AAA levels. Asymptomatic was defined as no related stints on the DL due to elbow injury in the 2 seasons prior to MRI. A fellowship-trained musculoskeletal radiologist reevaluated the studies after being blinded to patient name, injury history, and baseball history. A second investigator collected demographic data; this included total career number of innings pitched and any subsequent DL reports for each subject while remaining blinded to the MRI results.
Results:
The mean age at the time of MRI was 29.6 years (range, 19-39 years). The mean number of innings pitched was 1111.7. Of the 26 pitchers, 13 had scar remodeling of the anterior bundle of the ulnar collateral ligament (UCL). Of those, 4 had partial-thickness tears of the anterior bundle of the UCL, ranging from 10% to 90% of the total thickness. Twelve had articular cartilage loss within the posteromedial margin of the ulnohumeral joint, and 12 had posteromedial olecranon marginal osteophytes. Seven pitchers had degeneration of the common extensor tendon origin, 10 had degeneration of the flexor pronator mass, 9 had insertional triceps tendinosis, 2 had enthesopathic spurs at the sublime tubercle, 3 had osteochondral intra-articular bodies, and 2 subjects had joint effusions. In the year after MRI, 6 pitchers were placed on the DL for elbow-related injuries. There was no robust correlation between any single MRI finding and subsequent transfer to the DL, and no statistically significant correlation between number of innings pitched and MRI findings, although some trends were observed for both.
Conclusion:
MRI findings in asymptomatic MLB pitchers were not associated with placement on the DL within the subsequent year. While a trend was observed with olecranon osteophytes and subsequent DL placement (P = 0.07), this finding did not reach statistical significance. Furthermore, there was no robust correlation between the number of innings pitched with the presence of any of the aforementioned degenerative changes on MRI.
Clinical Relevance:
The characteristic structural transformation that occurs in the throwing elbow of professional pitchers is predictable and readily detectable on MRI. However, this study suggests that these changes are not predictive of near-term placement on the DL in those who are asymptomatic. Abnormal findings on MRI, even high-grade partial UCL tears, do not correlate with near-term placement on the DL, mitigating their potential negative impact on signing decisions.
Keywords: MRI, pitcher, professional baseball, elbow
Baseball is one of the most widely played sports across the globe, and its participants comprise a broad range of ages and skill levels. Injury rates among players are variable depending on both position and skill level, with incidence rates reaching as high as 5.8 per 1000 on the professional level.11
Among all positions, pitchers experience a significantly greater incidence of overall injury, particularly of the upper extremity. Posner et al11 demonstrated a 34% greater injury rate for pitchers compared with position players. The cost of such injuries is significant considering both direct and indirect measures. Recent data examining disabled list (DL) stints during the 2014 MLB season approximates $253,000,000 in lost revenue resulting from pitchers spending time on the DL.12 In addition, these reported numbers fail to account for revenue that is lost indirectly; a pitching-deficient roster may significantly impact the success of an organization, resulting in lost postseason prospects and a withering fan presence.
While shoulder injuries are historically more costly in terms of individual length of DL time, data from 2008 to 2014 shows that over this time there was a decrease in time spent on the DL due to shoulder injury and an increase in that due to elbow injury. Total days lost to shoulder injuries reached almost 7000 in 2008 but decreased to fewer than 3000 in 2014. Conversely, the number of days lost to elbow injuries increased from approximately 5000 in 2008 to more than 8000 in 2014.14 This observation may possibly be related to more optimal shoulder stabilization exercises that propagate the force distally into the valgus overloaded elbow.
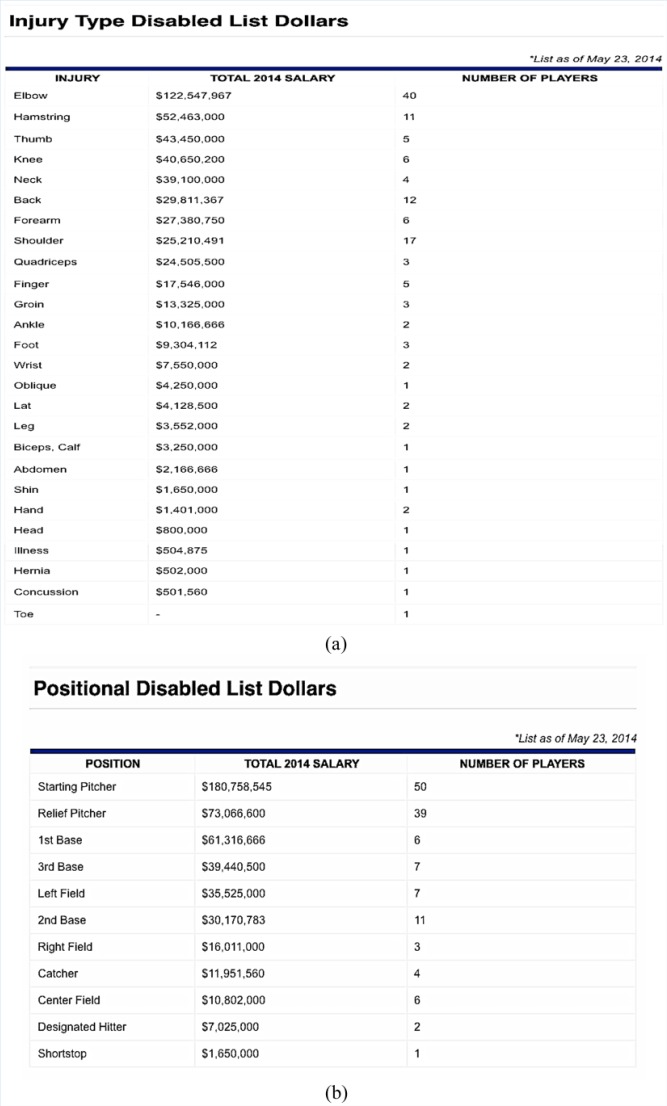
Recent data herald the elbow as not only the dominant DL-necessitating injury location but also as professional baseball’s single most costly injury by a substantial margin, with MLB incurring $122,547,967 in paid salaries for elbow-injured players during the 2014 season. This represents more than two times the $52,463,000 in paid salaries for players with the second most costly injury (hamstring strains) (Figure 1).12
Figure 1.
Total cost in paid salaries to players on the disabled list (DL) during the 2014 Major League Baseball season listed by (a) injury type and (b) position.
Elbow-related morbidity to the pitcher is of paramount importance, affecting individual player longevity, success, and economics of professional baseball franchises. Thus, early detection and intervention are pivotal concerns in the effort of minimizing the cost and disability incurred after the onset of injury and/or symptomatology.
The pathologic alterations related to the throwing elbow have been well documented within the spectrum of valgus extension overload syndrome that describes the intense biomechanical valgus loading on the pitching elbow.13 The load is delivered as such that it imparts a characteristic signature of stresses about the different compartments of the elbow that peak in the late-cocking to early acceleration phase, where the elbow experiences approximately 64 N·m of valgus torque, approaching the fatigue strength of the soft tissue stabilizers that dominate at that phase of the pitch.8 The end result is a triad of medial traction, lateral compression, and posteromedial shearing, the effects of which are frequently seen on magnetic resonance imaging (MRI).
MRI is both sensitive and specific in the detection of the characteristic alterations that accompany valgus extension overload syndrome.2 As a result of the repeated valgus loads, a predictable set of changes is frequently encountered. Ulnar collateral ligament (UCL) degeneration and/or tear along with signal changes in the flexor pronator mass both reflect the tensile load delivered to the medial structures. Additional common findings include olecranon and/or capitellar cartilage injuries induced by lateral compression as well as shear-induced posteromedial olecranon osteophyte formation.2
Given the frequency with which these changes are encountered in evaluation of the throwing elbow, it is not uncommon to demonstrate multiple changes in both the symptomatic and asymptomatic setting. The primary purpose of this investigation was to analyze the significance of these findings in the asymptomatic elbow as a risk factor for subsequent throwing-related elbow injury that required a stay on the DL. A secondary purpose of the study was to determine whether any of the previously described asymptomatic MRI findings correlated with the total number of innings pitched. The hypotheses were that (1) particular imaging findings on MRI would be predictive of placement on the DL for an elbow-related injury during the subsequent season and (2) the total number of innings pitched would correlate with the presence soft tissue and chondral injury on MRI.
Methods
Approval was obtained from the institutional review board before initiating the investigation. From 2003 to 2013, 26 asymptomatic players from a single Major League Baseball (MLB) organization underwent MRI of their dominant elbow as a condition of their contract signing or trade. For the purposes of this study, “asymptomatic” was defined as no stay on the DL for the dominant elbow in the prior 2 years and no elbow complaints at the time of the MRI. The MRI protocol can be found in Appendix 1 (available in the online version of this article).
MRI Qualitative Analysis
All images were reviewed on a PACS (picture archiving and communication system) workstation with diagnostic quality monitors. A fellowship-trained musculoskeletal radiologist with more than 15 years of experience who was blinded to the original MRI interpretations, the subjects’ injury status, and the subjects’ throwing history (total number of innings pitched) independently evaluated all 26 MRIs. Particular attention was paid to the UCL, ulnohumeral and radiocapitellar articular cartilage, ulnohumeral osteophytes (with special note if posteromedial), joint effusions, and abnormal signal in the triceps, biceps, brachialis, and extensor and flexor-pronator tendons. Ligament and tendon tears were characterized as intact, partial-thickness tear, and full-thickness tear as well as for tear location. Tendons and ligaments were also evaluated for signal hyperintensity relative to skeletal muscle on fluid-sensitive sequences, and tendons were characterized as normal (homogeneous low signal intensity), tendinosis (intermediate signal, less than fluid signal but higher than low signal), partial-thickness tear (fluid signal intensity within part of the tendon), or full-thickness tear (fluid signal intensity with complete loss of tendon continuity). MR grading of articular cartilage lesions was based on the International Cartilage Repair Society (ICRS) classification and defined as grade 0 (normal cartilage), grade 1 (increased T2-weighted signal in articular cartilage without defect or loss of thickness), grade 2 (fibrillation or thinning involving less than 50% of the thickness), grade 3 (defects greater than 50% of the cartilage thickness), and grade 4 (full-thickness articular cartilage defects).
Each subject’s pitching history was then recorded for his total professional and collegiate career up to and including the season preceding MRI. The total number of innings pitched was calculated combining all collegiate, minor league, and major league innings. Any elbow injury that required a stay on the DL throughout the season after MRI was also recorded from the subject’s records. The Fisher exact test was used to determine whether a correlation existed between MRI findings and DL placement, with statistical significance set at P < 0.05. The Mann-Whitney U test was also used, with statistical significance set at P < 0.05, to evaluate for any correlation between innings pitched and MRI findings.
Results
A total of 26 MRIs of asymptomatic professional baseball pitchers were examined. Mean player age at the time of MRI was 29.6 years (range, 19-39 years). The mean number of innings pitched prior to MRI was 1111.7, with significant variation within the group (range, 186-3182 innings). The mean number of innings pitched after MRI until the study’s completion was 168.8. Any elbow or proximal forearm injury that required a stay on the DL in the season after MRI was recorded from the subject’s records.
There were 18 right-handed pitchers (69%) and 8 left-handed pitchers (31%). Nine of the 26 players were placed on the 15- or 60-day DL within 1 year of MRI. Of those, 6 were due to elbow-related injuries. The remaining 3 resulted from shoulder injuries and were therefore considered within the non-DL group based on the absence of elbow-related injury. None had a surgical procedure performed as a result of the injury.
Of the 26 pitchers, 13 had scar remodeling of the anterior bundle of the UCL, as defined by abnormal thickening and intermediate signal intensity on coronal proton density sequences. Of those, 4 had partial-thickness tears of the anterior bundle of the UCL, as defined by discontinuity of ligament fibers on coronal proton density fat-suppressed images, ranging from 10% to 90% of the total thickness. Twelve had articular cartilage loss within the posteromedial margin of the ulnohumeral joint (4 grade I, 5 grade II, 3 grade III), and 12 had posteromedial olecranon marginal osteophytes. None of the subjects had visible trochlear or radiocapitellar chondral wear. Seven had degeneration at the common extensor tendon origin, without tear or surrounding soft tissue edema, 10 had degeneration of the flexor pronator mass (8 mild, 1 moderate, 1 severe), 9 had mild insertional triceps tendinosis, 2 had UCL traction spurs at the sublime tubercle, and 3 had osteochondral intra-articular bodies. Two subjects had joint effusions (small). No player had insertional biceps or brachialis tendinosis. Given the small number of osteochondral intra-articular bodies, UCL tears, UCL spurs, and joint effusions, limited statistical power precluded statistical analysis for these particular findings.
None of the previously detailed MRI findings rendered a statistically significant prediction of subsequent placement on the DL for asymptomatic pitchers in the season after MRI. Furthermore, an analysis of players with multiple findings, arbitrarily defined as 3 or more of any of the above, also failed to show any association with DL placement (P = 0.2). However, olecranon osteophytes trended toward statistical significance (P = 0.07).
When MRI findings were analyzed and compared with the total number of innings pitched, several trends were observed that did not reach statistical significance. Several findings were associated with a greater number of mean innings pitched. Of the 26 pitchers, 9 had triceps tendinosis. Pitchers with triceps tendinosis (mean, 1255 innings pitched) threw an average of 219 more innings than those without it (mean, 1036 innings pitched), a difference that nearly reached statistical significance (P = 0.07). There were 12 pitchers with olecranon osteophytes. Pitchers with olecranon osteophytes (mean, 1374 innings pitched) threw an average of 488 more innings than those without (mean, 887), a difference that also neared statistical significance (P = 0.19). Finally, there were 15 pitchers with multiple findings (arbitrarily defined as 3 or more of any of the aforementioned findings), versus 11 with less than 3. Pitchers with multiple findings (mean, 1293 innings pitched) threw an average of 392 more innings than those without (mean, 901 innings pitched; P = 0.27) (Tables 1-4).
Table 1.
Magnetic resonance imaging findings by disabled list (DL) status and innings pitched a
| Disabled List Status |
Innings Pitched |
||||
|---|---|---|---|---|---|
| Yes | No | P 1 b | Mean (Range) | P 2 c | |
| UCL tear d | 0.12 | 0.93 | |||
| Yes | 2 | 2 | 696 (442-1099) | ||
| No | 4 | 18 | 1187 (186-3182) | ||
| UCL degeneration | 0.65 | 0.53 | |||
| Yes | 4 | 9 | 1053 (186-3182) | ||
| No | 2 | 11 | 1171 (273-2941) | ||
| Olecranon cartilage injury | >0.99 | 0.52 | |||
| Yes | 3 | 9 | 1191 (186-3182) | ||
| No | 3 | 11 | 1044 (273-2694) | ||
| Common extensor origin signal | >0.99 | 0.69 | |||
| Yes | 1 | 6 | 871 (273-1555) | ||
| No | 5 | 14 | 1200 (186-3182) | ||
| Flexor pronator signal | 0.64 | 0.43 | |||
| Yes | 3 | 7 | 1028 (186-3182) | ||
| No | 3 | 13 | 1164 (307-2941) | ||
| Triceps tendinosis | 0.38 | 0.07 | |||
| Yes | 1 | 8 | 1255 (481-2694) | ||
| No | 5 | 12 | 1036 (186-3182) | ||
| Osteophytes | 0.07 | 0.19 | |||
| Yes | 5 | 7 | 1374 (307-3182) | ||
| No | 1 | 13 | 887 (186-1555) | ||
| Multiple findings e | 0.2 | 0.27 | |||
| Yes | 5 | 10 | 1293 (307-3182) | ||
| No | 1 | 10 | 901 (186-1555) | ||
UCL, ulnar collateral ligament.
Associations between innings pitched and disabled list placement with loose body, UCL spur, effusion, and biceps tendonitis were not examined secondary to limited statistical power/variation in subjects.
P1 values from Fisher exact tests.
P2 values from Wilcoxon rank-sum tests.
Group included 2 high-grade and 2 low-grade chronic tears. Both patients with high-grade tears were later placed on the disabled list. Of the 4 patients with UCL tear, all had intrasubstance degeneration as well.
Multiple findings were defined 3 or more of any of the above findings.
Table 2.
Age and total innings pitched by disabled list (DL) status
| DL Status | Subjects | Age, y |
Total Innings |
||
|---|---|---|---|---|---|
| Median | Range | Median | Range | ||
| No | 20 | 26-39 | 31.5 | 1047.4 | 273-3182 |
| Yes | 6 a | 19-36 | 30 | 1326.2 | 462-2941 |
Six patients represent those transferred to the DL for elbow injuries only.
Table 3.
Magnetic resonance imaging findings by disabled list status
| Total | Disabled List Status |
||
|---|---|---|---|
| Yes | No | ||
| UCL tear | 4 | 2 | 2 |
| UCL degeneration | 13 | 4 | 9 |
| Olecranon cartilage injury | 12 | 3 | 9 |
| Common extensor origin signal | 7 | 1 | 6 |
| Flexor pronator signal | 10 | 3 | 7 |
| Triceps tendinosis | 9 | 1 | 8 |
| Osteophytes | 12 | 5 | 7 |
| Multiple findings | 15 | 5 | 10 |
UCL, ulnar collateral ligament.
Table 4.
Magnetic resonance imaging findings by innings pitched
| Magnetic Resonance Finding With Innings Pitched, Median (Range) |
|||
|---|---|---|---|
| Yes | No | P Value | |
| UCL degeneration | 1053 (186-3182) | 1171 (273-2941) | 0.53 |
| Olecranon cartilage injury | 1191 (186-3182) | 1044 (273-2694) | 0.52 |
| Common extensor origin signal | 871 (273-1555) | 1200 (186-3182) | 0.69 |
| Flexor pronator signal | 1028 (186-3182) | 1164 (307-2941) | 0.43 |
| Triceps tendinosis | 1255 (481-2694) | 1036 (186-3182) | 0.07 |
| Osteophytes | 1374 (307-3182) | 887 (186-1555) | 0.19 |
| Multiple findings | 1293 (307-3182) | 901 (186-1555) | 0.27 |
| UCL tear | 696 (442-1099) | 1187 (186-3181) | 0.93 |
UCL, ulnar collateral ligament.
Discussion
The characteristic structural transformation that occurs in the throwing elbow is predictable based on the nature of the applied load and structural stabilizers that absorb it. The osseous geometry of the elbow joint is the main contributor of stability to valgus stress at levels of flexion below 20 degrees. During overhead throwing involving greater flexion angles, the UCL is subjected to loads at or near its fatigue strength.8 Morrey and An8 demonstrated in a cadaveric study that the UCL is responsible for supplying 54% of the varus torque needed to resist a valgus load when the elbow is flexed to 90°. The load to failure of the UCL is approximately 32 ± 9.6 N·m when producing varus torque. During the overhead throwing motion, the UCL is experiencing levels of force at or near its fatigue strength.2,8,9,13
Further stability to valgus loading is conferred by the dynamic stabilization of the flexor-pronator mass (FPM). The anatomic location of the flexor carpi ulnaris provides secondary stabilization to the UCL during all degrees of extension. In fact, incompetence of the UCL appears to correlate with tearing and degeneration of the FPM due to load transference, often leading to combined UCL-FPM injuries.9
The ulnohumeral compartment is wider during valgus stress resulting in shearing and impingement of the posteromedial olecranon as well as compression of the lateral radiocapitellar joint.1,13 The result is chondral damage, loose osteochondral body formation, and osteophyte formation. In vitro analysis of cadaveric elbows subject to static valgus loads at 90° of flexion before and after sectioning of the anterior bundle of the UCL have demonstrated increased pressure, decreased contact area, and a medial shift of the contact point of the ulnohumeral joint consistent with the location of chondromalacia observed in overhead throwing athletes.3 Asymptomatic professional baseball pitchers have demonstrated increased medial joint space widening during valgus stress radiographs when comparing dominant with nondominant arms,10 further supporting the hypothesis that an increase in medial elbow laxity may be a key causative alteration in the pathologic findings that accompany valgus extension overload.
The primary hypothesis that the structural MRI alterations would be predictive of DL-necessitating injury was not supported by the data. Of the above findings, posteromedial olecranon osteophytes came closest to statistical significance (P = 0.07), potentially suggesting a trend if studied in a cohort of greater power. This finding is a well-known source of elbow-related symptomatology, as functional ulnar nerve impingement can occur even in the presence of tiny olecranon osteophytes that may encroach the nerve in the extremes of valgus overload.1,10
Based on the breadth of evidence suggesting the role of a predictable valgus torque as the stimulus for the distinctive adaptive and degenerative structural anomalies that occur in the throwing elbow, it was also hypothesized that the total number of innings pitched would correlate with an increase in imaging findings on MRI. While no robust correlation was established between MRI changes in the elbow and the total number of career innings pitched, some trends did emerge. Patients with triceps tendinosis (mean, 1255 innings pitched) threw an average of 219 more innings than those without (mean, 1036 innings pitched), a difference that neared statistical significance (P = 0.07).
There were several limitations to this study. First, this was a retrospective review, and thus has the limitations inherent to such. The MRIs in this investigation were performed at multiple locations and thus did not have a standardized protocol. Furthermore, 2 MRI arthrograms were included within the 26 total studies, adding another potential confounder in that arthrograms may have different sensitivity and specificity than routine MRIs for evaluating UCL tears, osteochondral bodies, and chondral damage.5 Thus, abnormalities may have been present that were not detected. Also, only 1 radiologist reviewed the images, limiting the study as no interobserver statistical evaluation could be performed. Another potentially interesting factor that was considered but not included (because of the lack of recorded data in international players), was the number of innings pitched prior to becoming a professional, which would have increased the cumulative pitching load.
Most important, the data presented are limited by a small sample size (n = 26) as well as lack of an adequate sample size calculation, which places significant restrictions on the breadth of its potential extrapolation and warrants especially careful consideration of any clinical applications inspired by its claims. Therefore, negative statistical correlation cannot be estimated. More subjects would have been needed to increase statistical power and potentially find a relationship.
Although our limited sample size does dilute the accuracy of its yield, our primary conclusion is corroborated by similar data that suggested the null hypothesis when exploring MRI findings in the asymptomatic shoulder, finding no correlation with total career innings pitched and future DL placement.7 Additional, albeit less direct support can be loosely extrapolated from findings published by Kooima et al,6 who analyzed MRI findings of 16 asymptomatic pitchers, 87% of which exhibited UCL abnormalities and 13 of 16 demonstrated changes typical for posteromedial impingement. While the raw numbers presented here are slightly discordant in that this study found 50% and 45% with UCL degeneration and posteromedial osteophytes, respectively, it does support the primary conclusion that these changes are common, even in adolescents,4 and do not imply clinical significance.
Conclusion
Although limited by small sample size, these results demonstrate no correlation in asymptomatic pitchers between the number of innings pitched and any 1 of the characteristic MRI findings encountered with a high frequency in the throwing elbow. Furthermore, these changes were not predictive of future placement on the DL in the season after MRI. Thus, strong vigilance is advised before using any such imaging alterations in the asymptomatic elbow to steer clinical or roster-based decisions for professional pitchers, as preliminary data suggest that MRI findings may have no future (at least near-term) clinical import and could result in unnecessary interventions and profoundly affect a player’s career and marketability.
Supplementary Material
Footnotes
The authors report no potential conflicts of interest in the development and publication of this article.
References
- 1. Altchek D, Dines JS, Andrews J. Ulnar collateral ligament tears: special considerations. In: Dines JS, Altchek DW, Andrews J, ElAttrache NS, Wilk KE, Yocum LA, eds. Sports Medicine of Baseball. Philadelphia, PA: Lippincott Williams & Wilkins; 2012:248-252. [Google Scholar]
- 2. Banks KP, Ly JQ, Beall DP, Grayson DE, Bancroft LW, Tall MA. Overuse injuries of the upper extremity in the competitive athlete: magnetic resonance imaging findings associated with repetitive trauma. Curr Probl Diagn Radiol. 2005;34:127-142. [DOI] [PubMed] [Google Scholar]
- 3. Conte SA, Fleisig GS, Dines JS, et al. Prevalence of ulnar collateral ligament surgery in professional baseball players. Am J Sports Med. 2015;43:1764-1769. [DOI] [PubMed] [Google Scholar]
- 4. Hurd WJ, Jazayeri R, Mohr K, Limpisvasti O, Elattrache NS, Kaufman KR. Pitch velocity is a predictor of medial elbow distraction forces in the uninjured high school-aged baseball pitcher. Sports Health. 2012;4:415-418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kaplan LJ, Potter HG. MR imaging of ligament injuries to the elbow. Radiol Clin North Am. 2006;44:583-594. [DOI] [PubMed] [Google Scholar]
- 6. Kooima CL, Anderson K, Craig JV, Teeter DM, van Holsbeeck M. Evidence of subclinical medial collateral ligament injury and posteromedial impingement in professional baseball players. Am J Sports Med. 2004;32:1602-1606. [DOI] [PubMed] [Google Scholar]
- 7. Lesniak BP, Baraga MG, Jose J, Smith MK, Cunningham S, Kaplan LD. Glenohumeral findings on magnetic resonance imaging correlate with innings pitched in asymptomatic pitchers. Am J Sports Med. 2013;41:2022-2027. [DOI] [PubMed] [Google Scholar]
- 8. Morrey BF, An KN. Articular and ligamentous contributions to the stability of the elbow joint. Am J Sports Med. 1983;11:315-319. [DOI] [PubMed] [Google Scholar]
- 9. Osbahr DC, Swaminathan SS, Allen AA, Dines JS, Coleman SH, Altchek DW. Combined flexor-pronator mass and ulnar collateral ligament injuries in the elbow of older baseball players. Am J Sports Med. 2010;38:733-739. [DOI] [PubMed] [Google Scholar]
- 10. Patel RM, Lynch TS, Amin NH, Calabrese G, Gryzlo SM, Schickendantz MS. The thrower’s elbow. Orthop Clin North Am. 2014;45:355-376. [DOI] [PubMed] [Google Scholar]
- 11. Posner M, Cameron KL, Wolf JM, Belmont PJ, Owens BD. Epidemiology of Major League Baseball injuries. Am J Sports Med. 2011;39:1676-1680. [DOI] [PubMed] [Google Scholar]
- 12. TCA Physical Science. MLB injuries costs for 2014 disabled list. http://www.sportsinjuryalert.com/2014/05/mlb-injuries-costs-for-2014-disabled.html. Accessed October 7, 2015.
- 13. Wilson FD, Andrews JR, Blackburn TA, McCluskey G. Valgus extension overload in the pitching elbow. Am J Sports Med. 1983;11:83-88. [DOI] [PubMed] [Google Scholar]
- 14. Zimmerman J. Payroll amounts for players on the DL in 2010. http://www.fangraphs.com/blogs/payroll-amounts-for-players-on-the-disabled-list-in-2010. Accessed October 7, 2015.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.