Abstract
Context
The role of glycated haemoglobin (HbA1c) in the prediction of ischaemic stroke in individuals without diabetes is underestimated.
Aims
We performed a study to analyse the role of HbA1c in the risk prediction of ischaemic stroke in Pakistani population without diabetes. We further studied the difference between HbA1c values of individuals with diabetes and without diabetes with stroke.
Settings and design
Single centre, case–control.
Materials and methods
In phase I, a total of 233 patients without diabetes with ischaemic stroke and 245 as controls were enrolled. Association of HbA1c levels, lipid profiles and blood pressure recordings with ischaemic stroke was analysed. In phase II, comparison was done between diabetics and non-diabetics with stroke.
Statistical analysis
Comparison of the mean variables was performed with Student's t-tests. Logistic regression analysis with ischaemic stroke as the dependent variable was performed for phase I.
Results
In phase I, the ischaemic stroke group had significantly higher HbA1c levels (5.9±2.9% vs 5.5±1.6%) compared with controls (p<0.05). Triglyceride cholesterol, high-density lipoprotein cholesterol, systolic blood pressure, diastolic blood pressure and HbA1c were the significant determinants of stroke (p<0.05). In phase II, mean HbA1c values were significantly higher in the diabetes group (7.6±2.1 vs 6.1±2.3) (p<0.05) but other parameters were not statistically significantly different (p>0.05).
Conclusions
Higher HbA1c indicated a significantly increased risk for ischaemic stroke. An HbA1c value above 5.6% (prediabetic range) predicted future risk of stroke and efforts to maintain glucose level within the normal range (≤5.6%) in individuals with high cardiovascular risk are important.
Keywords: Ischemic Stroke, Risk factors, Glycosylated haemoglobin (HbA1c), Diabetes mellitus, Prediabetes
Introduction
The socioeconomic prospects of Asia have recently taken a dramatic change including changes in lifestyle, diet and urban localisation. This has brought changes in risk of cardiovascular diseases especially stroke.1 2 Prevalence of diabetes and prediabetes has increased in Asia including Pakistan in the past decade, nearly doubling during this era.3–5 Diabetes and prediabetes both show increased risk for ischaemic stroke and are associated with poor patient outcomes.6 7 With the increased risk of diabetes and ischaemic stroke in Asians, the importance of predictive value of glycated haemoglobin (HbA1c) has been an area of active study in recent years.8 9
The aim of this study was to analyse the role of HbA1c in the risk prediction of ischaemic stroke in Pakistani population without diabetes. We further studied the difference between HbA1c values of individuals with and without diabetes with stroke.
Subjects and methods
This single centre, descriptive, case–control study was carried out on indoor and outdoor patients. Patients were selected from the stroke registry database of the department of neurology while controls from a Health Check-up database, from January 2014 to June 2015. All the patients of both genders ≥12 years of age were included in the study.
The study was approved by the hospital ethical committee and carried out according to international ethical standards of the responsible committee on human experimentation and with the latest version of Helsinki Declaration of 1975. All patients underwent a detailed history taking and physical examination and all relevant investigations were performed.
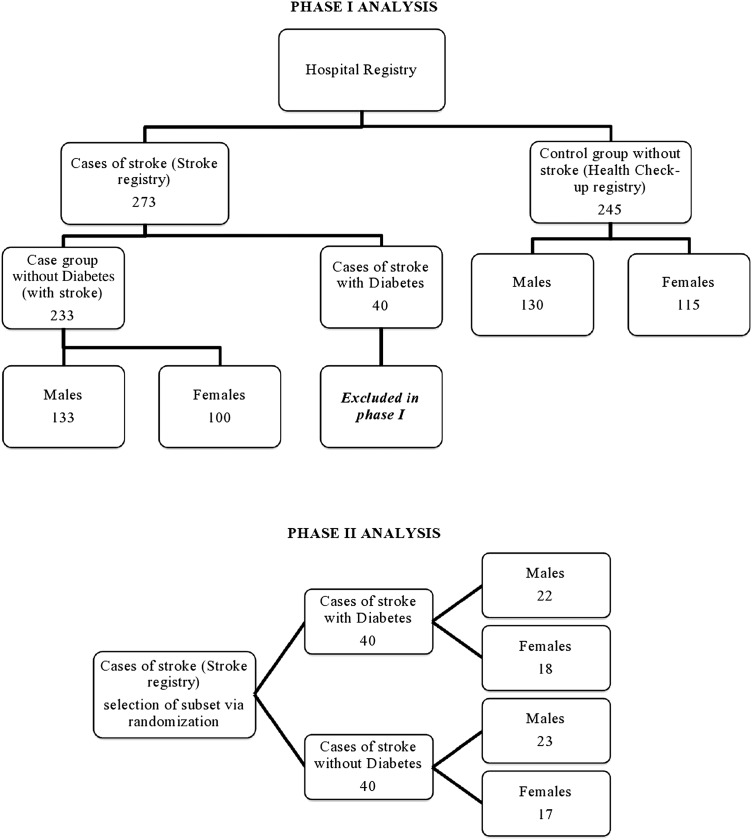
The study was divided into two phases for the purpose of statistical analysis; phase I and phase II (figure 1). In phase I, two groups were defined, from the hospital registry, namely patients with stroke, and controls without stroke. Both these groups consisted of individuals without diabetes. A total of 233 patients without diabetes with ischaemic stroke and 245 age and gender frequency matched individuals without stroke selected from a Health Check-up database as controls were enrolled in phase I. HbA1c levels, fasting glucose levels (BSF), random blood glucose (BSR), lipid profiles and blood pressure (BP) were recorded for all individuals. HbA1c levels were recorded at the time of stroke when patients were initially admitted. BSF, BSR, BP and lipid profile values were taken from the database of the registry of these patients which was already available with the hospital and was not more than 4 weeks old (averaged over previous visits). Height and weight were measured and body mass index (BMI) was calculated by dividing the weight (kg) by the height (m2). Smoking history was noted. In phase II, a subset of patients was selected randomly from the stroke registry, half of them being patients with diabetes and the other half being without diabetes (40 each) and their HbA1c, BSF, BSR, lipid profiles and BP were recorded.
Figure 1.
Summary of selection of study population and phase division.
All patients taken in either phase with stroke had suffered from focal symptoms of stroke and were observed within 1 week of symptom onset. Relevant lesions on CT or MR diffusion-weighted imaging and apparent diffusion coefficient (MR-DWI and ADC respectively) brain were identified. Individuals without HbA1c and BSF data were excluded from the study. Patients with a history of diabetes, BSF ≥126 mg/dL or fulfilling ADA criteria for diabetes were also excluded from the phase I analysis.4 The diagnosis of stroke was made by the consultant neurologist on the basis of history revealing focal symptoms, clinical examination supporting it and by neuroimaging ie, CT scan and/or MRI brain. Furthermore, patients from the stroke registry with otherwise unclear or suspicious diagnosis of stroke were also not included for analysis. The following laboratory investigations were performed as a part of routine work up of stroke registry: complete blood counts, liver function tests, renal function tests, electrolytes, ECG, Chest X-ray, erythrocyte sedimentation rate, blood sugar fasting (BSF), blood sugar random (BSR), hepatitis serology, urine routine examination, echocardiography, coagulation profile, HbA1c and lipid profile. Lipid profile panel consisted of total cholesterol (TC), high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C) and triglyceride cholesterol (TGL-C) levels. For phase II, diagnosis of diabetes was made based on ADA criteria for diabetes. Patients fulfilling the inclusion criteria were enrolled after taking informed written consent from the patients or relatives. The data collected was entered in a specifically designed proforma prospectively using the non-probability, consecutive sampling technique.
All individuals were examined after overnight fasting. The hexokinase method (Autoanalyzer) was used to measure fasting blood glucose levels. An enzymatic colorimetric test was used to measure TC and TG concentrations. The selective inhibition method was used to measure the level of HDL-C and a homogeneous enzymatic calorimetric test was used to measure the level of LDL-C. HbA1c was measured using an immunoturbidimetric assay with an automatic analyser with a reference value of 4.4–6.4%. The methodology was aligned with the Diabetes Control and Complications Trial and National Glycosylated haemoglobin Standardization Program standards. Systolic blood pressure (SBP) and diastolic blood pressure (DBP) was recorded by the standard clinical method at the brachial artery by the auscultatory method using an appropriate size cuff and after at least 5 min of resting in sitting position using a calibrated mercury sphygmomanometer.
Individuals were divided into four groups according to the quartiles of HbA1c level for the assessment of risk for ischaemic stroke as follows: 1st quartile=HbA1c≤5.3%; 2nd quartile=5.3<HbA1c≤5.6%; 3rd quartile=5.6<HbA1c≤6.0%; and 4th quartile=HbA1c>6.0%.
The data was analysed using SPSS V.17.0. Descriptive analysis was carried out and reported as mean±SD for continuous variables whereas frequencies and percentages were calculated for categorical variables. Associations of the variables and the presence or absence of ischaemic stroke were analysed in phase I. Case–controlled analyses was performed in the two groups to assess the risk of ischaemic stroke according to HbA1c. Comparison of the mean variables like age, BMI, BSF, HbA1c, HDL-C, LDL-C, TGL-C, TC, SBP and DBP, between patients with ischaemic stroke and control individuals was performed using the Student's t-tests. Logistic regression analysis with ischaemic stroke as the dependent variable was performed with age, gender, BMI, BSF, HDL-C, LDL-C, TGL-C, TC, SBP and DBP, smoking and quartile of HbA1c included in the model in phase I.
In phase II, a comparison was made between age, gender, BMI, smoking, BSF, HbA1c, HDL-C, LDL-C, TGL-C, TC, SBP and DBP values on a subset of patients in two groups; with diabetes versus without diabetes with ischaemic stroke (figure 1). p Values <0.05 were considered statistically significant.
Results
Phase I
Phase I comprised 233 patients and 245 controls. The mean age was 54.6±1.6 (range: 15–105) years in the case group and 50.3±1.4 (range: 17–97) in the control group. Among the patients, 133 (57.0%) were males while 100 (42.9%) were females. Among the controls, 130 (53.0%) were males while 115 (46.9%) were females. Mean age and gender were not statistically significantly different between the two groups (p>0.05; table 1).
Table 1.
Comparison between patients (with stroke) and controls (without stroke) for patients without diabetes: phase I
| Variables | Patients (with stroke) (n=233) | Controls (healthy matches) (n=245) | p Value |
|---|---|---|---|
| Age (years) | 54.69±1.60 | 50.33±1.44 | 0.96 |
| Gender/sex (males) n (%) | 133 (57.08) | 130 (53.06) | 0.31 |
| Gender/sex (females) n (%) | 100 (42.91) | 115 (46.93) | |
| BSF (mg/dL) | 112.43±5.76 | 98.7±8.98 | 0.84 |
| HbA1c (%) | 5.93±2.97 | 5.57±1.65 | 0.03 |
| HDL-C (mg/dL) | 43.00±1.95 | 46.54±2.43 | 0.02 |
| LDL-C (mg/dL) | 96.40±7.96 | 87.78±9.83 | 0.07 |
| TGL-C (mg/dL) | 221±37.89 | 176±27.89 | 0.00 |
| TC (mg/dL) | 178.50±27.66 | 169.76±26.76 | 0.21 |
| SBP (mm Hg) | 147.63±35.64 | 126.78±23.34 | 0.04 |
| DBP (mm Hg) | 90.56±16.64 | 81.24±8.90 | 0.04 |
| BMI (kg/m2) | 24.23±2.34 | 23.95±2.12 | 0.18 |
| Smoking n (%) | 143 (61.37) | 52 (21.22) | 0.02 |
Bold indicates significant p Values. Comparison between patients and controls for patients without diabetes: phase I: values are presented as mean±SD.
BMI, body mass index; BSF, blood sugar fasting; DBP, diastolic blood pressure; HbA1c, glycated haemoglobin; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol; SBP, systolic blood pressure; TC, total cholesterol; TGL-C, triglyceride cholesterol.
The ischaemic stroke group had significantly higher HbA1c levels (5.9±2.9%) compared to HbA1c levels of the age and gender-matched controls (5.5±1.6%) (p<0.05) (table 1). Mean values for BSF, BMI, TC and LDL-C were not statistically significantly different between the two groups (p>0.05). Mean HDL-C level was significantly lower and mean TGL-C level was significantly higher in patients with ischaemic stroke compared to the control individuals (p<0.05; table 1). The mean SBP and DBP values were significantly higher in patients with ischaemic stroke compared to control individuals (p<0.05; table 1). History of smoking was significant (p<0.05; table 1).
When logistic regression analysis was performed with ischaemic stroke being the dependent variable, HDL-C, TGL-C, SBP and DBP, smoking and increasing HbA1c were the significant predictors for ischaemic stroke (p<0.05; table 2). After adjusting for confounding variables, patients in the highest HbA1c quartile showed 7.8-fold increased odds for ischaemic stroke compared with those in the lowest HbA1c quartile (p<0.05; table 2).
Table 2.
Logistic regression analysis for patients with stroke (patients) as dependent variable: patients without diabetes: phase I
| Variables | OR | CI (95%) | p Value |
|---|---|---|---|
| Age (years) | 1.23 | 0.76 to 1.14 | 0.22 |
| Gender/sex (males) | 1(reference) | – | – |
| Gender/sex (females) | 1.22 | 0.77 to 1.43 | 0.34 |
| BSF (mg/dL) | 1.25 | 0.89 to 1.76 | 0.27 |
| HDL-C (mg/dL) | 0.78 | 0.87 to 0.99 | 0.00 |
| LDL-C (mg/dL) | 0.88 | 0.78 to 1.45 | 0.12 |
| TGL-C (mg/dL) | 1.91 | 0.90 to 1.43 | 0.00 |
| TC (mg/dL) | 0.88 | 0.78 to 1.98 | 0.54 |
| SBP (mm Hg) | 1.45 | 1.56 to 1.97 | 0.01 |
| DBP (mm Hg) | 1.33 | 0.87 to 1.56 | 0.03 |
| BMI (kg/m2) | 1.12 | 0.97 to 1.24 | 0.12 |
| Smoking | 28.32 | 11.14 to 62.31 | 0.02 |
| HbA1c ≤5.3 (%) | 1(reference) | – | – |
| >5.3 HbA1c ≤5.6 (%) | 1.67 | 0.67 to 5.44 | 0.11 |
| >5.6 HbA1c ≤6.0 (%) | 3.46 | 1.63 to 9.87 | 0.04 |
| HbA1c >6.0 (%) | 7.89 | 3.24 to 19.59 | 0.00 |
Bold indicates significant p Values. Logistic regression analysis for patients with stroke as dependent variable: phase I.
BMI, body mass index; BSF, blood sugar fasting; DBP, diastolic blood pressure; HbA1c, glycated haemoglobin; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol; SBP, systolic blood pressure; TC, total cholesterol; TGL-C, triglyceride cholesterol.
Phase II
Phase II comprised of 40 individuals with diabetes and 40 without diabetes with stroke. Mean age was 55.6±2.2 (range: 19–95) years in diabetes group and 51.7±1.4 (range: 21–96) in without diabetes group. Among the individuals with diabetes, 22 (55%) were males while 18 (45%) were females. Among individuals without diabetes, there were 23 males (57.5%) and 17 females (42.5%). Mean age and gender were not statistically significantly different between the two groups (p>0.05; table 3).
Table 3.
Comparison between individuals with diabetes and without diabetes with stroke: phase II
| Variables | Individuals without diabetes | Individuals with diabetes | p Value |
|---|---|---|---|
| Age (years) | 51.75±1.48 | 55.65±2.28 | 0.78 |
| Gender/sex (males) n (%) | 23 (57.50) | 22 (55.00) | 0.54 |
| Gender/sex (females) n (%) | 17 (42.50) | 18 (45.00) | |
| BSF (mg/dL) | 119.56±6.45 | 134.27±5.78 | 0.34 |
| HbA1c (%) | 6.11±2.31 | 7.65±2.15 | 0.00 |
| HDL-C (mg/dL) | 47.33±2.32 | 44.00±5.19 | 0.67 |
| LDL-C (mg/dL) | 96.43±6.46 | 98.43±8.85 | 0.93 |
| TGL-C (mg/dL) | 165.43±32.44 | 189.12±25.56 | 0.55 |
| TC (mg/dL) | 166.50±24.56 | 179.56±25.62 | 0.35 |
| SBP (mm Hg) | 161.00±50.28 | 172.55±18.29 | 0.13 |
| DBP (mm Hg) | 91.11±19.96 | 95.87±7.40 | 0.16 |
| BMI (kg/m2) | 24.21±2.34 | 25.12±13 | 0.32 |
| Smoking n (%) | 16 (40.00) | 19 (47.50) | 0.11 |
Bold indicates significant p Values. Comparison between individuals with diabetes and without diabetes with stroke: phase II: values are presented as mean±SD.
BMI, body mass index; BSF, blood sugar fasting; DBP, diastolic blood pressure; HbA1c, glycated haemoglobin; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol; SBP, systolic blood pressure; TC, total cholesterol; TGL-C, triglyceride cholesterol.
When HbA1c values were compared between individuals with diabetes and individuals without diabetes with stroke, mean HbA1c values were significantly higher in diabetes group (7.6±2.1 vs 6.1±2.3) (p<0.05) but other parameters were not statistically significantly different (p>0.05; table 3).
Discussion
Diabetes mellitus is a metabolic disease prevalent throughout the world and its burden has been increasing with the passage of time.9 10 The diversity of this disease varies greatly throughout the world in respect to cut-off values, prevalence and associations.10 11 The prevalence, incidence and cut-off values for diagnosis differ between Asians and non-Asians. According to international literature, prevalence of diabetes has recently increased from 3.5–6.0% to 9.9–13.1% in Pakistan, that is, in South East Asia.3 The prevalence of prediabetes has shown a similar increasing trend with current value around 9.20%.3 The current prevalence of diabetes and prediabetes in India is between 5.3–13.6% and 8.1–14.6%, respectively.3 Studies have shown that in China the current prevalence of diabetes is around 9.7% while that of prediabetes is around 15.5%.3
HbA1c level is an indicator of mean glucose control in the previous 60–90 days in patients with or without diabetes mellitus. HbA1c level is a good diagnostic tool but is also helpful for prognosis and to monitor therapeutic effects of drugs in diabetes. Well controlled and steady blood glucose levels can help prevent cardiovascular complications in patients with diabetes mellitus.4
Although blacks and whites differ in their HbA1c values, the trend for increased risk of stroke with higher HbA1c values is comparable between the two.8–11 Asian countries comprise almost two-third of the world's total mortality due to stroke.8 10 11 The role of HbA1c in the prediction of ischaemic stroke in individuals without diabetes is underestimated. While little data from around the world is available for review, data from Asia is scarce and from Pakistan is almost non-existent. The primary goal of this study was to analyse the role of HbA1c in the risk prediction of ischaemic stroke in non-diabetic Pakistani population.
Current study showed that patients with ischaemic stroke had significantly higher mean HbA1c level (5.9±2.9% vs 5.5±1.6%, p<0.05) compared to their age and gender frequency matched controls in patients without diabetes. The OR for ischaemic stroke increased with the quartile of HbA1c. The highest quartile of HbA1c (>6%) showed nearly eightfold increased odds of having ischaemic stroke compared with the lowest quartile (≤5.3%) (p<0.05) after adjusting for confounding variables. The increased odds with increased HbA1c quartile from first to the fourth suggested that higher HbA1c is associated with increased risk for ischaemic stroke even in individuals without diabetes. Fasting blood glucose on the other hand was not found to be significantly associated with baseline variables (p<0.05) suggestive of its poor predictive power.
Comparing our results to the internationally available literature, we found that authors worldwide have shown variable results for association of HbA1c with cardiovascular disease. A study from USA on a cohort of 26 563 patients concluded that HbA1c cannot predict cardiovascular disease (CVD) but only diabetes in patients without diabetes.8 A study by Park et al on 1239 individuals without diabetes demonstrated baseline HbA1as a better predictor of cardiovascular mortality. They compared HbA1c values to fasting plasma glucose and postchallenge plasma glucose levels. According to them, relative hazard for those in the highest quintile of HbA1c (≥6.7%) compared with lower levels was 2.3 for fatal CVD (p=0.00) and 2.4 for ischaemic heart disease (p=0.02).9 In another prospective study, a 1% increase in HbA1c was associated with a relative risk of death from any cause with mortality of 1.2 (p<0.00) in men and 1.2 (p<0.00) in women. They further concluded that 15% of the deaths occurred in persons with diabetes (HbA1c≥7% by their criteria) but 72% occurred in persons with HbA1c concentrations between 5% and 6.9%. The risk for CVD and total mortality associated with increasing HbA1c concentrations increased continuously through their cohort. Most of events noted by them occurred in population having moderately elevated HbA1c values. Therefore, they suggested the need for prospective randomised trials to reduce HbA1c concentrations in persons without diabetes and to see the effect of former on future outcomes regarding stroke.10
A study carried out over a period of more than a decade in individuals without diabetes concluded that increasing HbA1c concentrations are associated almost linearly with increased risk of diabetes, CVD and mortality. The results were significantly profound for HbA1c values compared to fasting glucose levels.11 Myint et al carried out a study on a population of more than 10 000 patients and found that 164 incident strokes were identified over 88 652 person-years. After adjustment for confounding variables (age, sex and cardiovascular risk factors), the relative risks for stroke with HbA1c concentrations 5–5.4%, 5.5–6.9% and ≥7% were 0.7, 0.8 and 2.8, respectively, compared with those with HbA1c <5%. In contrast to previous studies suggesting a linear relationship between blood glucose level and risk of coronary artery disease and stroke, a threshold relationship was advocated by Myint et al.12
The famous Hoorn study suggested that when adjusted for gender, hypertension, dyslipidemia and smoking, HbA1c was not significantly associated with the all-cause and cardiovascular mortality.5 Similar results were reported by Blake et al.13 Hjalmarsson et al on the other hand found that HbA1c was a good predictor of acute (p=0.01) and long-term mortality (p=0.02). Furthermore, HbA1c >6% was significantly correlated with severity of acute stroke (p=0.04). It was suggested that it predicted a worse functional outcome at 12 months (p=0.02). The authors reported that poor glycaemic control estimated via baseline HbA1c prior to stroke is an independent risk factor for poor survival. They further concluded that higher baseline HbA1c was a significant biochemical marker for increased stroke severity and unfavourable long-term functional outcome.14
A Mexican study concluded that diabetes and prediabetes are highly prevalent in hospitalised patients with ischaemic stroke. They suggested introducing the routine screening for diabetes and prediabetes via HbA1c testing in all patients with ischaemic stroke.15 Based on their suggestions and our findings, we also advocate the same. Similarly, a study from India suggested that prediction of future risk and prevention strategies for ischaemic stroke could be conceived by utilising HbA1c levels in both diabetic and non-diabetic population.16
Among diabetics, HbA1c has been associated with cardiovascular diseases including coronary artery disease as well as stroke. Zhao et al in their study suggested an association between HbA1c and the risk of stroke among women with type 2 diabetes. At different levels of HbA1c, the trend of association according to them was as follows: for HbA1c <6.0%, 6.0–6.9%, 7.0–7.9%, 8.0–8.9%, 9.0–9.9% and ≥10.0%, trend was 0.9, 1.0, 1.0, 1.1, 1.1 and 1.2 (p=0.66) for men and 1.0, 1.0, 1.0, 1.1, 1.3 and 1.4 (p=0.00) for women, respectively.17 A recent study from Israel reported that HbA1c is directly associated with risk of future stroke. Moreover, they proposed the idea that HbA1c per se improves the predictive accuracy for stroke in patients with diabetes with atrial fibrillation.18
In our study, mean values for total cholesterol were not statistically significantly different between individuals without diabetes with and without stroke. On the other hand, mean HDL-C level was significantly lower while mean TGL-C level was significantly higher in patients with ischaemic stroke compared to control patients. A similar result was seen when evaluating differences in mean BP levels. The mean SBP and DBP values were significantly higher in patients with ischaemic stroke. On logistic regression analysis, HDL-C, TGL-C and SBP and DBP were the significant predictors for ischaemic stroke. This means that the same patients with higher HbA1c levels who are at risk of future stroke, also have higher mean TGL-C and BP and a low HDL-C. This may suggest that the coexistence of these multiple risk factors might be related and contribute concomitantly towards the risk of stroke.
When HbA1c values were compared between individuals with diabetes and without diabetes with stroke, mean HbA1c values were significantly higher in the diabetes group (7.6±2.1 vs 6.1±2.3) (p<0.05) but other parameters were not statistically significantly different (p>0.05) (phase II) (table 3). The second part (phase II) findings were meant to point out that even other risk factors did not differ, HbA1c in individuals with diabetes was significantly higher than individuals without diabetes though individuals without diabetes were found to have high HbA1c value as a predictor of stroke. This could signify that diabetics having higher HbA1c than those of individuals without diabetes could be at greater risk of stroke (perhaps >eightfolds which was found for individuals without diabetes) and that higher HbA1c itself above a certain threshold could signify many fold increase in the risk of stroke with increasing HbA1c values. This may suggest that there might be a certain threshold value of HbA1c up to which the trend for other risk factors (namely BP and lipid profile) significantly affects the future risk of stroke, but above it, HbA1c alone might be a more powerful independent predictor. This however needs to be validated via conducting large population-based prospective studies adopting a model based on incremental associations of HbA1c with other risk factors for stroke.
Limitations
Like any other study, our study too had its limitations. First, we selected patients who had a stroke from a single centre registry but our centre being the largest specialised unit in the country renders services to nearly one-fifth of the population of Pakistan. Moreover, baseline characteristics of patients who had a stroke in this study were comparable to those of nationwide stroke data, so the groups could be representative of patients who had a stroke in Pakistan to some extent. The second limitation was that the diagnosis of diabetes was based on history, previous health records, levels of fasting glucose and HbA1c but glucose challenge test was not performed as a part of this study. Although recent guidelines recommend that fasting glucose and HbA1c levels are sufficient to diagnose diabetes, there is still a possibility that individuals with diabetes could have been included in phase I.4
In spite of these limitations, our study presented meaningful results. It was the first to report association of increasing HbA1c with risk for ischaemic stroke in Pakistani adults without diabetes. Moreover, it identified a cut-off value for HbA1c above which the risk of stroke increases even in individuals without diabetes in our setup. We therefore suggest the need of routine HbA1c testing in all patients with ischaemic stroke for secondary prevention and routine screening in hospital registry for patients with high cardiovascular risk for primary prevention. By conducting more sophisticated prospective studies on larger population cohorts, the association between level of HbA1c and risk of ischaemic stroke can be more clearly defined in Pakistani population without diabetes.19–21
Conclusions
Higher HbA1c indicated a significantly increased risk for ischaemic stroke after adjusting for other confounding variables in Pakistani population without diabetes. HbA1c quartile >6% showed eightfold increase in risk of stroke compared to quartile ≤5.3%. An HbA1c value above 5.6% (prediabetic range) predicted future risk for ischaemic stroke and efforts to maintain glucose level within the normal range (≤5.6%) especially in individuals with high cardiovascular risk are important. We suggest the need for routine HbA1c testing in all patients with ischaemic stroke for secondary prevention and routine screening in hospital registry for patients with high cardiovascular risk for primary prevention.
Footnotes
Funding: This work has been carried out without any grants or funds. It has been completed without external financial support and the expenses whatsoever for the purpose of this study have been contributed solely by the author's themselves and no one else.
Competing interests: None declared.
Patient consent: Obtained.
Ethics approval: Hospital Ethics Committee copy submitted.
Provenance and peer review: Commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1.Burke TA, Venketasubramanian RN. The epidemiology of stroke in the East Asian region: a literature-based review. Int J Stroke 2006;1:208–15. doi:10.1111/j.1747-4949.2006.00060.x [DOI] [PubMed] [Google Scholar]
- 2.Ramachandran A, Ma RC, Snehalatha C. Diabetes in Asia. Lancet 2010;375:408–18. doi:10.1016/S0140-6736(09)60937-5 [DOI] [PubMed] [Google Scholar]
- 3.Qureshi MS, Iqbal M, Nomani AZ. Rapidly increasing prevalence and associations of diabetes mellitus in a rural community of Pakistan. J Diabetol 2014;3:3 http://www.journalofdiabetology.org [Google Scholar]
- 4.American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care 2011;34(Suppl 1):S62–9. doi:10.2337/dc11-S062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.de Vegt F, Dekker JM, Ruhé HG, et al. Hyperglycaemia is associated with all-cause and cardiovascular mortality in the Hoorn population: the Hoorn Study. Diabetologia 1999;42:926–3. doi:10.1007/s001250051249 [DOI] [PubMed] [Google Scholar]
- 6.Selvin E, Coresh J, Shahar E, et al. Glycaemia (haemoglobin A1c) and incident ischaemic stroke: the Atherosclerosis Risk in Communities (ARIC) Study. Lancet Neurol 2005;4:821–6. doi:10.1016/S1474-4422(05)70227-1 [DOI] [PubMed] [Google Scholar]
- 7.Hu GC, Hsieh SF, Chen YM, et al. Relationship of initial glucose level and all-cause death in patients with ischaemic stroke: the roles of diabetes mellitus and glycated hemoglobin level. Eur J Neurol 2012;19:884–91. doi:10.1111/j.1468-1331.2011.03647.x [DOI] [PubMed] [Google Scholar]
- 8.Pradhan AD, Rifai N, Buring JE, et al. Hemoglobin A1c predicts diabetes but not cardiovascular disease in nondiabetic women. Am J Med 2007;120:720–7. doi:10.1016/j.amjmed.2007.03.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Park S, Barrett-Connor E, Wingard DL, et al. GHb is a better predictor of cardiovascular disease than fasting or postchallenge plasma glucose in women without diabetes. The Rancho Bernardo Study. Diabetes Care 1996;19:450–6. doi:10.2337/diacare.19.5.450 [DOI] [PubMed] [Google Scholar]
- 10.Khaw KT, Wareham N, Bingham S, et al. Association of hemoglobin A1c with cardiovascular disease and mortality in adults: the European prospective investigation into cancer in Norfolk. Ann Intern Med 2004;141:413–20. doi:10.7326/0003-4819-141-6-200409210-00006 [DOI] [PubMed] [Google Scholar]
- 11.Selvin E, Steffes MW, Zhu H, et al. Glycated hemoglobin, diabetes, and cardiovascular risk in nondiabetic adults. N Engl J Med 2010;362:800–11. doi:10.1056/NEJMoa0908359 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Myint PK, Sinha S, Wareham NJ, et al. Glycated hemoglobin and risk of stroke in people without known diabetes in the European Prospective Investigation into Cancer (EPIC)-Norfolk prospective population study: a threshold relationship? Stroke 2007;38: 271–5. doi:10.1161/01.STR.0000254549.75763.5f [DOI] [PubMed] [Google Scholar]
- 13.Blake GJ, Pradhan AD, Manson JE, et al. Hemoglobin A1c level and future cardiovascular events among women. Arch Intern Med 2004;164:757–61. doi:10.1001/archinte.164.7.757 [DOI] [PubMed] [Google Scholar]
- 14.Hjalmarsson C, Manhem K, Bokemark L, et al. The role of prestroke glycemic control on severity and outcome of acute ischemic stroke. Stroke Res Treat 2014;2014:694569 doi:10.1155/2014/694569 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Huisa BN, Roy G, Kawano J, et al. Glycosylated hemoglobin for diagnosis of pre-diabetes in acute ischemic stroke patients. J Stroke Cerebrovasc Dis 2013;22:e564–7. doi:10.1016/j.jstrokecerebrovasdis.2013.06.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Singh AS, Atam V, Chaudhary SC, et al. Relation of glycated hemoglobin with carotid atherosclerosis in ischemic stroke patients: an observational study in Indian population. Ann Indian Acad Neurol 2013;16: 185–9. doi:10.4103/0972-2327.112462 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhao W, Katzmarzyk PT, Horswell R, et al. Sex differences in the risk of stroke and HbA(1c) among diabetic patients. Diabetologia 2014;57:918–26. doi:10.1007/s00125-014-3190-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Saliba W, Barnett-Griness O, Elias M, et al. Glycated hemoglobin and risk of first episode stroke in diabetic patients with atrial fibrillation: a cohort study. Heart Rhythm 2015;12:886–92. doi:10.1016/j.hrthm.2015.01.025 [DOI] [PubMed] [Google Scholar]
- 19.Heo SH, Lee SH, Kim BJ, et al. Does glycated hemoglobin have clinical significance in ischemic stroke patients? Clin Neurol Neurosurg 2010;112:98–102. doi:10.1016/j.clineuro.2009.08.024 [DOI] [PubMed] [Google Scholar]
- 20.Rivera JJ, Choi EK, Yoon YE, et al. Association between increasing levels of hemoglobin A1c and coronary atherosclerosis in asymptomatic individuals without diabetes mellitus. Coron Artery Dis 2010;21:157–63. doi:10.1097/MCA.0b013e328337ff9b [DOI] [PubMed] [Google Scholar]
- 21.Khealani BA, Khan M, Tariq M, et al. Ischemic strokes in Pakistan: observations from The National acute ischemic stroke database. J Stroke Cerebrovasc Dis 2014;23:1640–7. doi:10.1016/j.jstrokecerebrovasdis.2014.01.009 [DOI] [PubMed] [Google Scholar]