Abstract
Background
Carotid atherosclerotic plaque is identified as one of the main sources of ischaemic stroke. However, the prevalence of carotid high-risk atherosclerotic plaque in Chinese patients with ischaemic cerebrovascular events has been inconsistently reported and needs to be investigated in a large population.
Objectives
The primary objective of CARE II study was to determine the prevalence and characteristics of high-risk features of atherosclerotic plaques in the carotid arteries in Chinese patients with recent ischaemic stroke or transient ischaemia attack (TIA). The relationship between carotid plaque features and cerebral infarcts, the differences of carotid plaque patterns among different regions of China and the gender specific characteristics of carotid plaque will be also determined.
Study design
The CARE II study will enrol 1000 patients with recent ischaemic stroke or TIA and carotid plaque from 13 hospitals and medical centres across China. In this cross-sectional, non-randomised, observational, multicentre study, all patients will undergo carotid artery MRI of bilateral carotid arteries and routine brain MRI with standardised protocols. The MRI will be interpreted at core reading centres to evaluate the characteristics of morphology and compositions of carotid plaque.
Conclusions
This is a cross-sectional, multicentre study to investigate the prevalence and characteristics of high-risk atherosclerotic carotid plaque in Chinese patients with stroke and TIA by using high-resolution MRI of vessel wall. This trial is sufficiently powered to demonstrate the prevalence of carotid high-risk plaque and to explore regional differences in Chinese patients who suffered stroke.
Trial registration number
Keywords: Atherosclerosis, Plaque, Stenosis, Vessel Wall, MRI
Introduction
Stroke is the second most common cause of death and the third most common cause of disability worldwide.1 2 Carotid atherosclerotic plaque is identified as one of the main sources of ischaemic stroke. Fibrous cap rupture of atherosclerotic plaque is believed to be the key event that leads to thrombus formation and clinical events. Many recent studies have focused on the identification of features of ‘high-risk’ plaques that pose increased risk of rupture, especially using non-invasive in vivo imaging techniques. Histologically, major determinants of plaques prone to rupture include plaque compositional features, such as intraplaque haemorrhage (IPH) and large lipid-rich necrotic core (LRNC).3 Carotid atherosclerotic plaque MRI (CMRI) is capable of accurately characterising plaque morphology and composition and is validated by histology.4–6 Many recent studies have focused on the use of CMRI to evaluate carotid plaque features that predict future stroke or transient ischaemic attack (TIA) in prospective settings.7–9 Recently, two systematic reviews and meta-analyses summarised the key plaque features on CMRI that are associated with cerebrovascular events.10 11
Recent findings about high-risk plaques suggest the need to include vessel wall imaging as part of carotid artery examination. The current clinical diagnosis of carotid atherosclerotic plaque, however, is based on the measurement of luminal stenosis by ultrasound and/or other angiographic imaging modalities.12 13 It is well established that stenosis measurement to decide carotid plaque severity and treatment options has many limitations.14 Angiographic imaging does not provide information of the pathological changes of the vessel wall and may underestimate the severity of atherosclerotic disease due to positive remodelling.15 For example, investigators found that more than 20% of carotid arteries with lower grade stenosis (<50% stenosis) had high-risk features, such as IPH and fibrous cap rupture,16 17 and these features can also occur in 8–9% of carotid arteries with normal lumen size.18 Recent studies have also suggested that a portion of cryptogenic strokes may actually be caused by carotid atherosclerotic plaque with moderate and/or minor stenosis.19 20
CMRI, even though promising, remains an experimental procedure. Researchers in different institutions have used different approaches for CMRI. But in general, the commonly accepted approach is to include ‘multiple-contrast’ image acquisitions to provide comprehensive information of plaque morphology and composition.5 21 22 Despite many studies reporting the use of CMRI in relatively small or single-centre studies, there have been limited reports of using a single standardised imaging protocol in large multicentre studies to evaluate carotid atherosclerosis in a symptomatic population.
Stroke is the number one killer in China and there has been much attention directed to identify strokes that are caused by carotid atherosclerotic plaque.23 Findings from these studies, have been inconsistent, however. A study by Jeng et al24 reported that 13% of patients (48/367) with ischaemic stroke had severe carotid stenosis (>50% stenosis or occlusion). In contrast, Liu et al25 showed that severe carotid stenosis could be seen in 41.7% of patients who suffered stroke. More interestingly, a pilot study by Saam et al26 showed that carotid plaque composition differs between Chinese and American Caucasian symptomatic patients. In addition, the prevalence of cerebrovascular atherosclerotic disease may vary among different regions of China. A recent study has shown that the proportion of patients with severe intracranial atherosclerosis (stenosis >50%) was significantly higher in north China than in south China (50.2% vs 41.9%; p<0.0001).27 However, the difference in carotid atherosclerotic plaque characteristics between patients in south and north areas of China is unclear. Thus, an imaging study to examine the carotid atherosclerotic plaque status in patients with recent stroke may provide critical information on the prevalence of carotid plaque and their compositional features and regional differences in China. This information will help to understand the natural status of carotid atherosclerotic plaque in patients who suffered stroke and to identify the best prevention and treatment options.
Methods
Carotid Atherosclerosis Risk Assessment (CARE II) study is conceived based on the needs to assess carotid atherosclerotic plaque in Chinese patients who recently suffered stroke and/or TIA using identical, state-of-the-art CMRI technique (NCT02017756). It is a cross-sectional, non-randomised, observational, multicentre study evaluating the carotid atherosclerotic plaque by CMRI in Chinese patients who suffered stroke. It is supported by funding from the Chinese government and by industrial partners. In collaboration with 13 medical centres and hospitals in China equipped with 3 T MRI scanner and with the Vascular Imaging Laboratory (VIL) of the University of Washington, this study intended to consecutively recruit 1000 patients with recent stroke or TIA and atherosclerotic plaque in at least one carotid artery, to undergo CMRI of bilateral carotid arteries and routine brain MRI. Core reading centres situated in the Center for Biomolecular Imaging Research (CBIR, Beijing, China) and VIL (Seattle, Washington, USA) conducted quantitative review of the carotid plaque, as detailed below.
This study intended to recruit patients in different regions of China using a single standardised CMRI protocol with centralised, blinded review and analysis. IRB approvals were obtained for the entire study and for each participating institution and all study participants provided written informed consent.
Study objectives
The primary objective of the CARE-II study is to determine the prevalence and characteristics of high-risk features of atherosclerotic plaques in the carotid arteries in Chinese patients with recent ischaemic stroke or TIA. Main secondary objectives are to evaluate: (1) the relationship between carotid plaque features and cerebral infarcts; (2) the differences of carotid plaque patterns among different regions of China, particularly south and north areas; (3) gender specific characteristics of carotid artery atherosclerotic disease in Chinese patients who suffered stroke.
Targeted population
This study intends to consecutively recruit 1000 patients with recent stroke or TIA (within 2 weeks after onsets of symptoms) and atherosclerotic plaque in at least one carotid artery determined by B-mode ultrasound scan (intima-media thickness ≥1.5 mm). The age of study population ranges from 18 to 80 years old. The exclusion criteria are as follows: (1) patients with evidence of cardiogenic stroke; (2) patients with haemorrhagic stroke; (3) history of radiation therapy in the neck; (4) claustrophobia; and (5) contraindication to MRI examination.
Patient recruitment and MRI
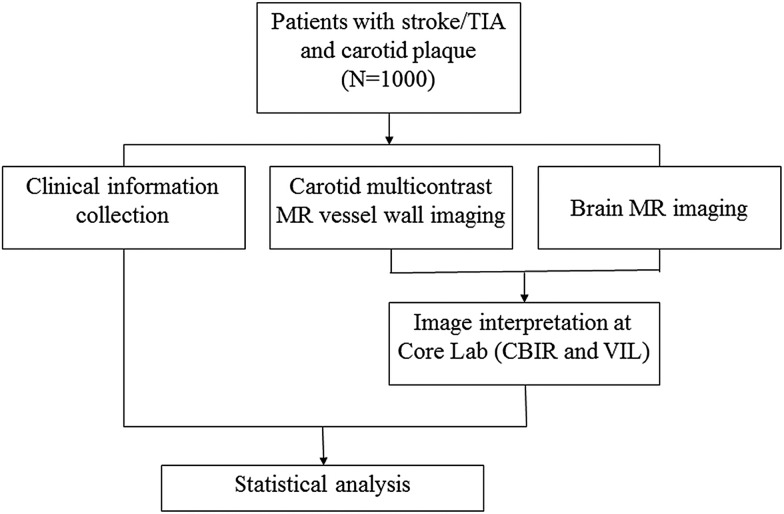
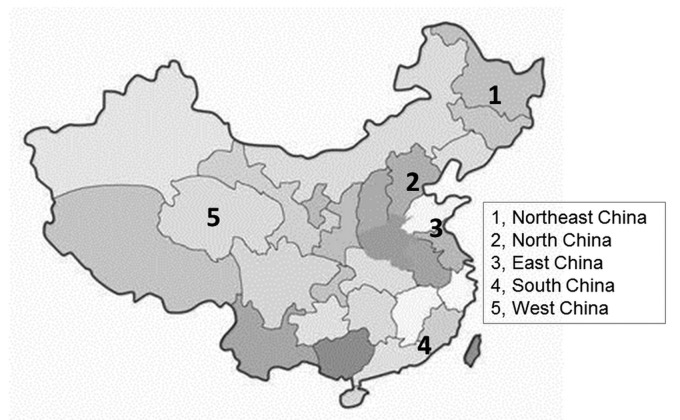
A flow chart of the study protocol is presented in figure 1. Hospitals and imaging centres must have a stroke unit, defined as a multidisciplinary team which has been designated for the care of patients who suffered stroke, and it must be equipped with a 3 T whole body MRI scanner capable of running the standardised carotid imaging protocol prescribed in the study. Hospitals distributed in the following regions were selected to investigate geographical differences in carotid plaque features of patients: Northeast, North, East, South and West areas (figure 2). Participating radiologists and MRI technologists were trained on image acquisition and quality evaluation by CBIR. Phantom and human volunteer scans were conducted at each participating site and evaluated by the core laboratory in CBIR for protocol adherence and image quality before recruitment of patients was allowed.
Figure 1.
Flow chart of study protocol. CBIR, Center for Biomolecular Imaging Research; VIL, Vascular Imaging Laboratory.
Figure 2.
Regional distribution of imaging sites across China.
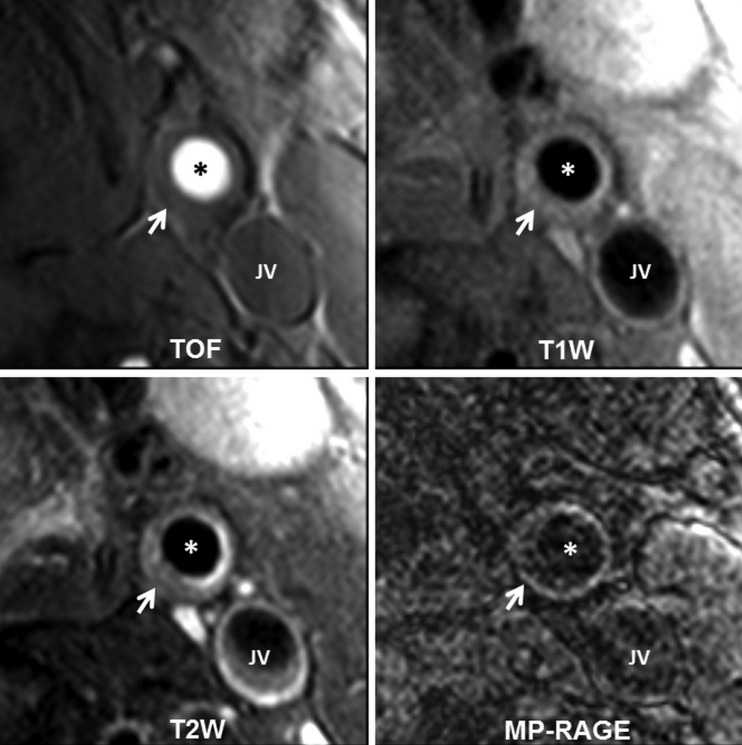
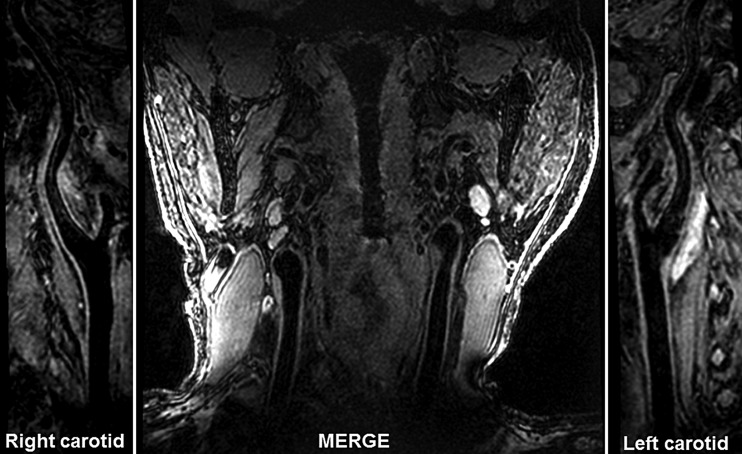
All the MRI is performed on a 3.0 T MRI scanner with 8-channel phase array coil. In this multicentre study, an identical high resolution, multicontrast vessel wall imaging protocol is used for carotid plaque imaging. The imaging protocol includes three-dimensional (3D) time-of-flight (TOF), T1-weighted (T1-W) quadruple inversion recovery (QIR),28 T2-weighted (T2-W) multislice double inversion recovery (MDIR),29 and Magnetisation Prepared Gradient Recalled Echo (MP-RAGE) imaging sequences. The localisation of carotid plaque imaging is centred to the bifurcation of index carotid artery. A 3D imaging sequence of Motion sensitised driven Equilibrium prepared Rapid Gradient Echo (MERGE)30 with large longitudinal coverage is also acquired for describing the distribution of atherosclerotic plaques in different segments of extracranial carotid arteries. The imaging parameters are detailed in table 1. In addition, a standard protocol including 3D TOF MR angiography (MRA), T2-fluid-attenuated inversion recovery (FLAIR) and diffusion-weighted image (DWI) sequences was used for brain imaging. Figures 3 and 4 show examples of carotid vessel wall images acquired.
Table 1.
Imaging parameters of CMRI
| Standardised multicontrast imaging protocol | 3D sequence | ||||
|---|---|---|---|---|---|
| TOF | T1W | T2W | MP-RAGE | MERGE | |
| Sequence | FFE | TSE | TSE | FFE | FFE |
| Black blood | None | QIR | MDIR | MSDE | |
| Repeat time, ms | 20 | 800 | 4800 | 8.8 | 10 |
| Echo time, ms | 4.9 | 10 | 50 | 5.3 | 4.8 |
| Flip angle | 20° | 90° | 90° | 15° | 6° |
| Field of view, cm | 14×14 | 14×14 | 14×14 | 14×14 | 25×16×7 |
| Matrix | 256×256 | 256×256 | 256×256 | 256×256 | 356×357 |
| Scan plane | axial | axial | axial | axial | coronal |
| Slice thickness, mm | 1 | 2 | 2 | 1 | 0.7 |
FFE, Fast field echo; MDIR, multislice double inversion recovery; MP-RAGE, Magnetisation Prepared Gradient Recalled Echo; MSDE, Motion Sensitised Driven Equilibrium; TOF, time-of-flight; TSE, turbo spin echo; QIR, quadruple inversion recovery.
Figure 3.
Example of 2D multicontrast carotid vessel wall imaging protocol including TOF, T1W, T2W and MP-RAGE sequences. The lumen (*) and outer wall boundaries are well delineated on vessel wall images. A lipid-rich atherosclerotic lesion can be seen in the left common carotid artery (arrow). JV represents jugular vein. 2D, two-dimensional; MP-RAGE, Magnetisation Prepared Gradient Recalled Echo; TOF, time-of-flight; T1-W and T2-W, T1 and T2-weighted image.
Figure 4.
Example of 3D MERGE vessel wall imaging with large longitudinal coverage. The middle and the bilateral panels represent original MERGE image and left and right carotid artery images after curved reconstruction, respectively. 3D, three-dimensional; MERGE, Motion sensitised driven Equilibrium prepared Rapid Gradient Echo.
Clinical information collection
Clinical information is acquired from the medical records prior to carotid MRI for all patients. Demographic characteristics including age, gender, height and weight were recorded. History of hypertension (defined as diastolic blood pressure ≥90 mm Hg or systolic blood pressure ≥140 mm Hg), diabetes, smoking, statin use and cardiovascular disease is collected. The levels of lipoprotein including high-density lipoprotein, low-density lipoprotein, total cholesterol and triglycerides are recorded. In addition, the index artery which is defined as carotid arteries associated with symptoms is determined when such information is available.
Image interpretation
All MRI acquired from the image sites are transferred to the core laboratories of Center for Biomedical Imaging Research (CBIR) at Tsinghua University, Beijing, China and Vascular Imaging Laboratory (VIL) at University of Washington, Seattle, USA.
Carotid artery image review
The vessel wall images of bilateral carotid arteries are interpreted by trained reviewers with >3 years' experience in cardiovascular plaque imaging using custom-designed software (CASCADE; University of Washington, Seattle, USA). Each axial image is reviewed by two reviewers blinded to clinical information and brain image findings with consensus. The lumen and wall boundaries are outlined manually to measure the lumen area, wall area, total vessel area and wall thickness (WT) at each axial location. The presence or absence of calcification, LRNC, IPH and fibrous cap rupture is identified using the published criteria.5 31 The size of each plaque's compositional feature is also measured. The carotid 3D MERGE images are analysed at an MR workstation to measure the maximum WT of plaque in each segment of the carotid artery (common carotid artery, bulb, and internal carotid artery (ICA)) when present. Three-dimensional TOF MRA images are reconstructed by maximum intensity projection to measure the luminal stenosis of carotid arteries using North American Symptomatic Carotid Endarterectomy Trial (NASCET) algorithm.32
Brain image review
The intracranial 3D TOF MRA images are reconstructed by maximum intensity projection. The luminal stenosis is measured at each arterial segment using the following categories: 0%, 1–29%, 30–49%, 50–69%, 70–99% and 100% (occlusion) according to the WASID method.33 The segments of intracranial arteries include intracranial ICA, middle cerebral artery, anterior cerebral artery, posterior cerebral artery and basilar artery. The volume and location of acute cerebral infarcts which are hyperintense on DWI images and white matter lesions (WML) which show hyperintense on FLAIR images are evaluated using custom-designed software. The severity of WML is stratified using a previously published method.34
Statistical analysis and sample size considerations
To address the primary study objective, the prevalence of plaque components and features including calcification, LRNC, IPH and fibrous cap rupture will be estimated from the entire study sample and from important subgroups defined by gender, age and geographic region. Within the same groups, the distributions of carotid vessel morphology, including wall volume, per cent wall volume, maximum WT and maximum per cent wall area and volumes of components (calcification, LRNC and IPH) will be summarised using means and SDs as well as percentiles.
As part of the secondary objectives, plaque features and measurements will be compared between demographic and regional subgroups using logistic regression (for binary features) and other generalised linear models (for continuous measurements, which may be normally distributed or skewed). Multiple models will be considered, which will adjust for (1) gender and age; (2) gender, age and other traditional risk factors; and (3) gender, age, risk factors and plaque size. Similarly, multivariate logistic regression will be used to evaluate associations between the presence and absence of acute cerebral infarcts, WML or severe intracranial stenosis and carotid plaque features, while generalised linear models will be used to evaluate associations between acute infarct or WML volumes and carotid plaque features.
Based on the target sample size of 1000 and assuming a 10% loss rate due to missing data or image quality issues (final N=900), precision (95% CIs) for our prevalence estimates will be within ±3.3% in the full sample and ±7.7% in subgroups that are one-fifth the size of the full sample. All power calculations assumed two-sided tests with a significance level of 0.05. Calculations were performed using R (V.3.1.1, R Foundation for Statistical Computing, Vienna, Austria) and GPower (V.3.1.9.2, University of Kiel, Germany).35
Discussion
This is one the first multicentre studies targeting patients who have had recent stroke and TIA using a standardised CMRI. It is likely to provide critical information of the prevalence of carotid atherosclerotic plaque and its characteristics beyond luminal narrowing. Furthermore, this study will test the feasibility of using one multicontrast imaging protocol to evaluate carotid atherosclerosis in a multicentre setting and the usefulness of this protocol. Owing to the distribution of imaging centres across China, this study may also provide useful information of the differences in prevalence in carotid atherosclerosis in different regions and plaque compositional features regional dependencies.
The design incorporates centralised training, quality assurance, image review of both carotid and brain images, adds more confidence of the overall analysis.
Limitations
This is a cross-sectional study and the patient recruitment scheme does not rule out strokes potentially caused by intracranial atherosclerotic plaques or aortic arch disease. Although efforts are made to exclude patients with cardioembolic stroke, cardiogenic sources cannot be definitively ruled out. For example, not all patients currently undergo long-term monitoring for paroxysmal arrhythmias.
Conclusion
This is a cross-sectional, multicentre study to investigate the prevalence and characteristics of high-risk atherosclerotic carotid plaque in Chinese patients with stroke and TIA by using high-resolution vessel wall MRI. This trial is sufficiently powered to demonstrate the prevalence of carotid high-risk plaque and to explore regional differences in Chinese patients who suffered stroke.
Footnotes
Contributors: XZ and CY conceived this study. RL provided technical supports. DSH conducted statistical analysis. XZ interpreted the data. XZ and DSH drafted this manuscript and CY and TSH made critical revisions. CY supervised this study.
Funding: This study is supported by grants of Natural Science Foundation of China (81271536, 61271132 and 81361120402) and Philips Healthcare.
Competing interests: None declared.
Patient consent: Obtained.
Ethics approval: The Institutional review Board of Tsinghua University School of Medicine.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Lozano R, Naghavi M, Foreman K, et al. . Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the global burden of disease study 2010. Lancet 2012;380:2095–128. doi:10.1016/S0140-6736(12)61728-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Murray CJ, Vos T, Lozano R, et al. . Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the global burden of disease study 2010. Lancet 2012;380:2197–223. doi:10.1016/S0140-6736(12)61689-4 [DOI] [PubMed] [Google Scholar]
- 3.Falk E, Shah PK, Fuster V. Coronary plaque disruption. Circulation 1995;92:657–71. doi:10.1161/01.CIR.92.3.657 [DOI] [PubMed] [Google Scholar]
- 4.Toussaint JF, LaMuraglia GM, Southern JF, et al. . Magnetic resonance images lipid, fibrous, calcified, hemorrhagic, and thrombotic components of human atherosclerosis in vivo. Circulation 1996;94:932–8. doi:10.1161/01.CIR.94.5.932 [DOI] [PubMed] [Google Scholar]
- 5.Cai JM, Hatsukami TS, Ferguson MS, et al. . Classification of human carotid atherosclerotic lesions with in vivo multicontrast magnetic resonance imaging. Circulation 2002;106:1368–73. doi:10.1161/01.CIR.0000028591.44554.F9 [DOI] [PubMed] [Google Scholar]
- 6.Clarke SE, Hammond RR, Mitchell JR, et al. . Quantitative assessment of carotid plaque composition using multicontrast MRI and registered histology. Magn Reson Med 2003;50:1199–208. doi:10.1002/mrm.10618 [DOI] [PubMed] [Google Scholar]
- 7.Takaya N, Yuan C, Chu B, et al. . Association between carotid plaque characteristics and subsequent ischemic cerebrovascular events: a prospective assessment with MRI—initial results. Stroke 2006;37:818–23. doi:10.1161/01.STR.0000204638.91099.91 [DOI] [PubMed] [Google Scholar]
- 8.Altaf N, MacSweeney ST, Gladman J, et al. . Carotid intraplaque hemorrhage predicts recurrent symptoms in patients with high-grade carotid stenosis. Stroke 2007;38:1633–5. doi:10.1161/STROKEAHA.106.473066 [DOI] [PubMed] [Google Scholar]
- 9.Kwee RM, Hofman PAM, Gronenschild EHBM, et al. . Association between carotid plaque characteristics and cerebral white matter lesions: one-year follow-up study by MRI. PLoS ONE 2011;6:e17070 doi:10.1371/journal.pone.0017070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gupta A, Baradaran H, Schweitzer AD, et al. . Carotid plaque MRI and stroke risk a systematic review and meta-analysis. Stroke 2013;44:3071–7. doi:10.1161/STROKEAHA.113.002551 [DOI] [PubMed] [Google Scholar]
- 11.Saam T, Hetterich H, Hoffmann V, et al. . Meta-analysis and systematic review of the predictive value of carotid plaque hemorrhage on cerebrovascular events by magnetic resonance imaging. J Am Coll Cardiol 2013;62:1081–91. doi:10.1016/j.jacc.2013.06.015 [DOI] [PubMed] [Google Scholar]
- 12.Randoux B, Marro B, Koskas F, et al. . Carotid artery stenosis: prospective comparison of CT, three-dimensional gadolinium-enhanced MR, and conventional angiography. Radiology 2001;220:179–85. doi:10.1148/radiology.220.1.r01jl35179 [DOI] [PubMed] [Google Scholar]
- 13.Herzig R, Burval S, Krupka B, et al. . Comparison of ultrasonography, CT angiography, and digital subtraction angiography in severe carotid stenoses. Eur J Neurol 2004;11:774–81. doi:10.1111/j.1468-1331.2004.00878.x [DOI] [PubMed] [Google Scholar]
- 14.Wasserman BA, Wityk RJ, Trout HH III, et al. . Low-grade carotid stenosis: looking beyond the lumen with MRI. Stroke 2005;36:2504–13. doi:10.1161/01.STR.0000185726.83152.00 [DOI] [PubMed] [Google Scholar]
- 15.Glagov S, Weisenberg E, Zarins CK, et al. . Compensatory enlargement of human atherosclerotic coronary arteries. N Engl J Med 1987;316:1371–5. doi:10.1056/NEJM198705283162204 [DOI] [PubMed] [Google Scholar]
- 16.Saam T, Underhill HR, Chu B, et al. . Prevalence of American Heart Association type VI carotid atherosclerotic lesions identified by magnetic resonance imaging for different levels of stenosis as measured by duplex ultrasound. J Am Coll Cardiol 2008;51:1014–21. doi:10.1016/j.jacc.2007.10.054 [DOI] [PubMed] [Google Scholar]
- 17.Zhao X, Underhill HR, Zhao Q, et al. . Discriminating carotid atherosclerotic lesion severity by luminal stenosis and plaque burden: a comparison utilizing high-resolution magnetic resonance imaging at 3.0 tesla. Stroke 2011;42:347–53. doi:10.1161/STROKEAHA.110.597328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dong L, Underhill HR, Yu W, et al. . Geometric and compositional appearance of atheroma in an angiographically normal carotid artery in patients with atherosclerosis. AJNR Am J Neuroradiol 2010;31:311–16. doi:10.3174/ajnr.A1793 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Freilinger TM, Schindler A, Schmidt C, et al. . Prevalence of nonstenosing, complicated atherosclerotic plaques in cryptogenic stroke. JACC Cardiovasc Imaging 2012;5:397–405. doi:10.1016/j.jcmg.2012.01.012 [DOI] [PubMed] [Google Scholar]
- 20.Hyafil F, Schindler A, Sepp D, et al. . High-risk plaque features can be detected in non-stenotic carotid plaques of patients with ischaemic stroke classified as cryptogenic using combined F-FDG PET/MR imaging. Eur J Nucl Med Mol Imaging 2016;43:270–9. doi:10.1007/s00259-015-3201-8 [DOI] [PubMed] [Google Scholar]
- 21.Luo Y, Polissar N, Han C, et al. . Accuracy and uniqueness of three in vivo measurements of atherosclerotic carotid plaque morphology with black blood MRI. Magn Reson Med 2003;50:75–82. doi:10.1002/mrm.10503 [DOI] [PubMed] [Google Scholar]
- 22.Saam T, Ferguson MS, Yarnykh VL, et al. . Quantitative evaluation of carotid plaque composition by in vivo MRI. Arterioscler Thromb Vasc Biol 2005;25:234–9. doi:10.1161/01.ATV.0000149867.61851.31 [DOI] [PubMed] [Google Scholar]
- 23.Liu L, Wang D, Wong KS, et al. . Stroke and stroke care in China: huge burden, significant workload, and a national priority. Stroke 2011;42:3651–4. doi:10.1161/STROKEAHA.111.635755 [DOI] [PubMed] [Google Scholar]
- 24.Jeng JS, Chung MY, Yip PK, et al. . Extracranial carotid atherosclerosis and vascular risk factors in different types of ischemic stroke in Taiwan. Stroke 1994;25:1989–93. doi:10.1161/01.STR.25.10.1989 [DOI] [PubMed] [Google Scholar]
- 25.Liu HM, Tu YK, Yip PK, et al. . Evaluation of intracranial and extracranial carotid steno-occlusive diseases in Taiwan Chinese patients with MR angiography: preliminary experience. Stroke 1996;27:650–3. doi:10.1161/01.STR.27.4.650 [DOI] [PubMed] [Google Scholar]
- 26.Saam T, Cai JM, Cai YQ, et al. . Carotid plaque composition differs between ethno-racial groups: an MRI pilot study comparing mainland Chinese and American Caucasian patients. Arterioscler Thromb Vasc Biol 2005;25:611–16. doi:10.1161/01.ATV.0000155965.54679.79 [DOI] [PubMed] [Google Scholar]
- 27.Pu Y, Liu L, Wang Y, et al. . Geographic and sex difference in the distribution of intracranial atherosclerosis in China. Stroke 2013;44:2109–14. doi:10.1161/STROKEAHA.113.001522 [DOI] [PubMed] [Google Scholar]
- 28.Yarnykh VL, Yuan C. T1-insensitive flow suppression using quadruple inversion-recovery. Magn Reson Med 2002;48:899–905. doi:10.1002/mrm.10292 [DOI] [PubMed] [Google Scholar]
- 29.Yarnykh VL, Yuan C. Multislice double inversion-recovery black-blood imaging with simultaneous slice reinversion. J Magn Reson Imaging 2003;17:478–83. doi:10.1002/jmri.10278 [DOI] [PubMed] [Google Scholar]
- 30.Balu N, Yarnykh VL, Chu B, et al. . Carotid plaque assessment using fast 3D isotropic resolution black-blood MRI. Magn Reson Med 2011;65:627–37. doi:10.1002/mrm.22642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chu B, Kampschulte A, Ferguson MS, et al. . Hemorrhage in the atherosclerotic carotid plaque: a high-resolution MRI study. Stroke 2004;35:1079–84. doi:10.1161/01.STR.0000125856.25309.86 [DOI] [PubMed] [Google Scholar]
- 32.North American Symptomatic Carotid Endarterectomy Trial Collaborators. Beneficial effect of carotid endarterectomy in symptomatic patients with high-grade carotid stenosis. N Engl J Med 1991;325:445–53. doi:10.1056/NEJM199108153250701 [DOI] [PubMed] [Google Scholar]
- 33.Chimowitz MI, Lynn MJ, Howlett-Smith H, et al. . Comparison of warfarin and aspirin for symptomatic intracranial arterial stenosis. N Engl J Med 2005;352:1305–16. doi:10.1056/NEJMoa043033 [DOI] [PubMed] [Google Scholar]
- 34.Liao D, Cooper L, Cai J, et al. . Presence and severity of cerebral white matter lesions and hypertension, its treatment, and its control. The ARIC study. Atherosclerosis risk in communities study. Stroke 1996;27:2262–70. [DOI] [PubMed] [Google Scholar]
- 35.Faul F, Erdfelder E, Buchner A, et al. . Statistical power analyses using G*Power 3.1: tests for correlation and regression analyses. Behav Res Methods 2009;41:1149–60. doi:10.3758/BRM.41.4.1149 [DOI] [PubMed] [Google Scholar]