Abstract
Ischaemic stroke is a major cause of neurological morbidity and mortality. The objective of this review article is to summarise facts pertaining to acute ischaemic stroke and its various aspects in a developing country like Pakistan, where resources are limited and the healthcare system is underdeveloped. No large-scale epidemiological studies are available to determine the true incidence of stroke in Pakistan. We reviewed the available literature on stroke from Pakistan and through this article we primarily aim to present the current acute ischaemic stroke management in Pakistan in juxtaposition to that of the developed world. We also intend to highlight areas for future development and improvement in management. The routine practice in Pakistan is that of using stat dose of aspirin in emergency (ER) at large with only a handful of centres offering thrombolytic therapy with recombinant tissue plasminogen activator for acute ischaemic stroke. This too is faced with the problem of long window periods before the patient reaches a proper stroke care centre. The facilities of interventional therapies like arterial thrombolysis and endovascular surgery are non-existent and rehabilitation facilities limited. The opportunities for training physicians in acute stroke are also scarce. Stroke in children is underdiagnosed and that in women not availing facilities at stroke care centres. While basic research has gained pace regarding local demographic data, advanced research and genetic studies are extremely limited. The field of stroke neurology needs to grow at a substantial pace in Pakistan to be at par with the developed world.
Keywords: Cerebrovascular accident, acute ischemic stroke, recombinant tissue Plasminogen Activator, window period, Pakistan stroke management.
Introduction
Stroke is a debilitating illness rendering thousands disabled and leading a significant proportion of people to death worldwide. Its incidence in Asia, according to a rough estimate, has been increasing recently. Among Asian countries, Pakistan shares a significant burden of this devastating disease contributing towards an exponential expenditure of resources, finances, community manpower, health services and the economy as a whole.1 2
Traditional and well-known risk factors of stroke like diabetes and hypertension have also been recognised to be increasing in Asian countries. The burden of stroke is following a similar trend. According to recently published literature, Pakistan currently has an enormous proportion of its population suffering either from diabetes or hypertension or both.1 2 Unfortunately, a majority of people are unaware of their comorbid conditions. This primarily is due to a lack of awareness for routine medical checkup, availability of screening services for endemic diseases locally and ignorance on the part of the community regarding personal healthcare. Even those who have been timely diagnosed do not mostly follow the standard practice of a regular follow-up and/or compliance with medications. At the same time, poor updated knowledge of local physicians not associated with tertiary care setups contributes towards the use of obsolete and relatively less effective medical healthcare delivery.
Local literature on stroke published from Pakistan is scarce. The current incidence and prevalence of stroke in Pakistan is not exactly known. Several reported case series in literature highlighting significant differences in terms of stroke epidemiology, risk factors and stroke subtypes have been published but full-text original research articles are not more than a handful. Considering a high population suffering from stroke in our country, it would be highly beneficial to collect and interpret local epidemiological data. Its consequences can range from countering physical disability and conserving millions of dollars against the social and economic consequences brought up on by stroke.2–5
The objective of this review article is to summarise the facts regarding acute ischaemic stroke and its various aspects in a third world country, that is, Pakistan, where resources are limited and healthcare system is underdeveloped. No large-scale epidemiological studies are available to determine the true incidence of stroke in Pakistan. We reviewed the available literature on stroke from Pakistan and through this article we primarily aim to present the current acute ischaemic stroke management in Pakistan in juxtaposition to that of the developed world. We also intend to highlight areas for future development and improvement in management.
Literature search
PubMed, MEDLINE, Medline Plus, PubMed Central and Pakmedinet search was undertaken using the keywords ‘cerebrovascular accident, acute ischemic stroke, recombinant tissue Plasminogen Activator, window period, feasibility, third world country, Pakistan, stroke management’. Full articles were reviewed; all available relevant statistics were searched and included if mentioned by the authors.
Epidemiology
Twenty per cent of the world's population resides in South Asia. This region has the most dense concentration of cardiovascular diseases. As stroke affects the elderly exceedingly, an increase in the average lifespan has automatically led to an increased number of stroke cases reported.2 5 6
Stroke and transient ischaemic stroke are rampant in Pakistan. The risk of stroke has plumped by 100% or more in the past decade, especially in third world countries where it accounts for more than 85% of all stroke-related mortality. The mean population age of patients with stroke in developing countries like Pakistan is a decade or younger than that of their western counterparts as reported by Ali and colleagues in 2016. This leads to an increased overall lifetime burden of functional disability and consequent economic losses.1 2 5–10
Transient ischaemic attack (TIA) defines a subset of patients having a high risk of getting a stroke. These patients may benefit from timely intervention, most likely thrombolysis or endovascular procedures. The immediate risk of stroke is about 10% in the first 90 days after TIA, the initial 48 hours being the most critical. Papers presented from Pakistan report an almost similar statistical result. Early intervention after TIA has shown an 80% relative risk reduction in the emergence of stroke in western cohorts. While this revolutionised treatment strategy in the field of neurology has now been practised for over a decade in the western world, it is still in a stage of infancy in Pakistan with a juvenile infrastructure. Only a few centres in Pakistan offer thrombolysis. That too is offered to a very select number of cases and usually to that portion of the population who can afford its cost. This is because meeting the window period deadline is a major problem and expenses for thrombolysis are solely borne by the patient and their family. Virtually no endovascular surgical facilities are yet available.11–15
Risk stratification
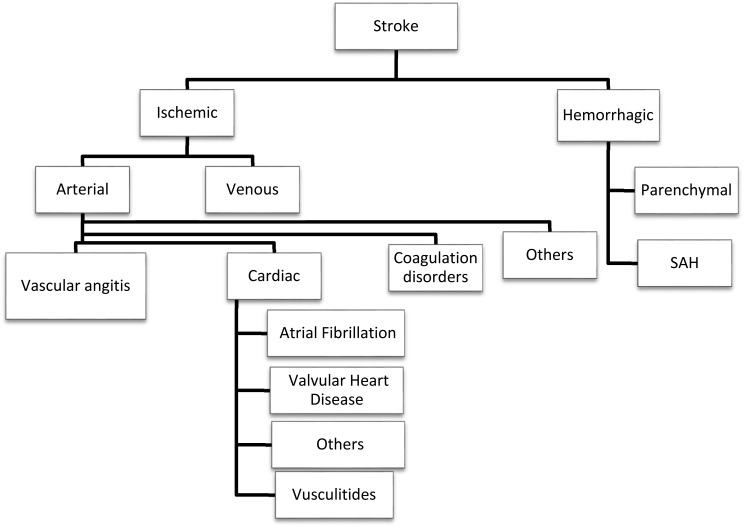
Risk factors for stroke range from common ailments like diabetes mellitus, hypertension, hyperlipidaemia, atrial fibrillation, aneurysms, arterio venous malformation (AVM) and smoking to factors observed in otherwise seemingly healthier individuals like antiphospholipid syndrome, procoagulopathies, vasculitides and Moyamoya disease. By 2020, Pakistan is expected to rank fourth among the most populous countries around the globe with respect to the burden of diabetes and every third person above the age of 45 years is anticipated to suffer from hypertension.2 3 5 9 10 15 16 The current prevalence of diabetes in Pakistan has been estimated to be around 9–10% as published by Qureshi and colleagues in 2014. Even the prediabetes prevalence is higher as compared with western countries. People aged 15 years or higher have an overall 19% prevalence of hypertension. Obesity is another major problem in South Asians and their body mass index has been estimated to have lower cut-off values for quantification of diseases like diabetes and cardiovascular diseases. Obesity has a prevalence ranging from 20% to 30% in South Asia.9 10 17 Apart from the above, various understudied and underestimated risk factors are shown in figure 1.
Figure 1.
Risk factors for ischaemic stroke. An algorithm showing the risk factors for ischaemic stroke. SAH, subsarachnoid hemorrhage.
Stroke referral protocols
There is no systematic referral system or organised general practice (GP) in Pakistan. There is no continued medical education programme for GPs in Pakistan and no official collaboration network available for keeping in touch with tertiary care setups and teaching hospitals. While most GPs are able to identify strokes pertaining to anterior circulation, those related to posterior circulation presenting with subtle signs like homonymous hemianopsia, signs of cerebellar and brainstem dysfunction are usually missed. Similarly, owing to the unavailability of CT scan facilities in most of the areas outside major cities, stroke is usually missed or remains undiagnosed for days before the patient arrives at a tertiary care setup. Therefore, there is a dire need of a comprehensive programme for GPs with an aim to teach proper and prompt identification and referral of such cases.2–5 18–20
Recognition of clinical presentation
Identification of stroke is encouraged to be made at the community level worldwide by introduction of acronyms like FAST, that is, Facial drooping/deviation/weakness, Arm weakness (arm paralysis/paresis/pronator drift), Speech difficulties (aphasia/dysphasia/slurring) and Time as shown in figure 2. There is no national awareness campaign or educational platform for the general public to get awareness about the signs of early stroke. Such signs are not even recognised by rescue operators or ambulance service personnel. The first person usually to identify these is the doctor at hospital setups. It is only at the level of medical specialists or neurologists that most of these patients are quickly and correctly diagnosed. This is very crucial in the current perspective of treatment of acute ischaemic strokes and TIAs as the window period for administering thrombolysis is just 4.5 hours at present. Loss of these ‘golden hours’ makes all the difference in active management of stroke.8 13 18–26
Figure 2.
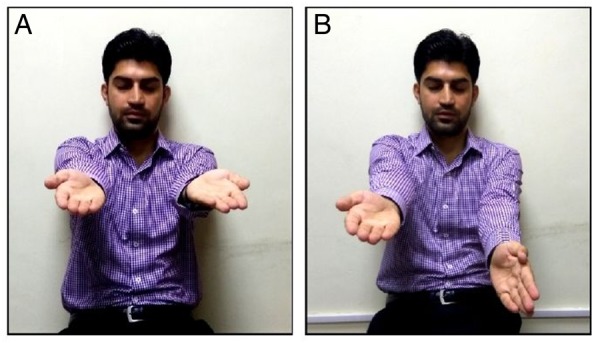
Bedside clinical signs to be noted in stroke; (A) a patient who has not suffered a stroke can generally hold the arms in an extended position with eyes closed. (B) A patient with stroke will often display ‘arm drift’ (pronator drift)—one arm will remain extended when held outwards with eyes closed, but the other arm will drift or drop downwards and pronate (palm turned downwards).
Stroke code
The stroke code system in Pakistan is almost non-existent.
Local event sight protocols and transportation services
The transporting facility of ambulances is rudimentary as compared with international standard protocols. While internationally in-transit neuroimaging and administration of tissue plasminogen activator (tPA) in ambulances is the next big thing, we are struggling with timely transportation of patients to the hospital. This probably is due to resource deficits including a low number of ambulances, poor road infrastructure and lack of on-call services for transport from rural suburbs to major cities.2–6 9 10 19–25 A transport facility by the name of 1122 was introduced in major cities a decade back. The staff is trained and well equipped to manage acute cardiovascular events and road traffic accidents. However, there is limited knowledge of stroke, its presentation variants and management protocols.
Transit times
The travelling time from suburbs and even major districts to facilities designated for ‘neurology and stroke care’ is quite long. There are many reasons like unpaved roads, major traffic blocks and greater travelling distances. Using air transport facilities is a dream far from realisation in the near future.2–6 22–25
In-hospital emergency services
The patient receiving policies at district-level hospitals is also not at par with international standards. There are usually no CT scan facilities except in major cities and patients are immediately referred to tertiary care setups. However, it takes the referral procedure almost an hour or 2; this time lapse combined with transport delays leads to patients usually falling out of the window period when they arrive at tertiary care setups. At tertiary setups, while immediate CT scan and stroke identification is the norm, the sophisticated code of calculating and limiting the care service provided for such patients in the form of door to CT time (target <25 min), CT to needle time (target <20 to 35 min) and door to needle time (target <45 to 60 min) is non-existent because of otherwise non-existent thrombolysis centres. Only individual efforts by certain units to minimise the duration up to needle time are practised, that too for selected cases and patients already coming with short histories, feasible for thrombolysis and mostly within the immediate vicinity of the stroke care centre. This also includes an urgent emergency laboratory workup to rule out contraindications to the above like complete blood counts, platelet count, partial thromboplastin time, international normalised ratio, electrolytes, serum creatinine levels, serum glucose, troponin levels, liver function tests and blood grouping.2–4 20 21–27
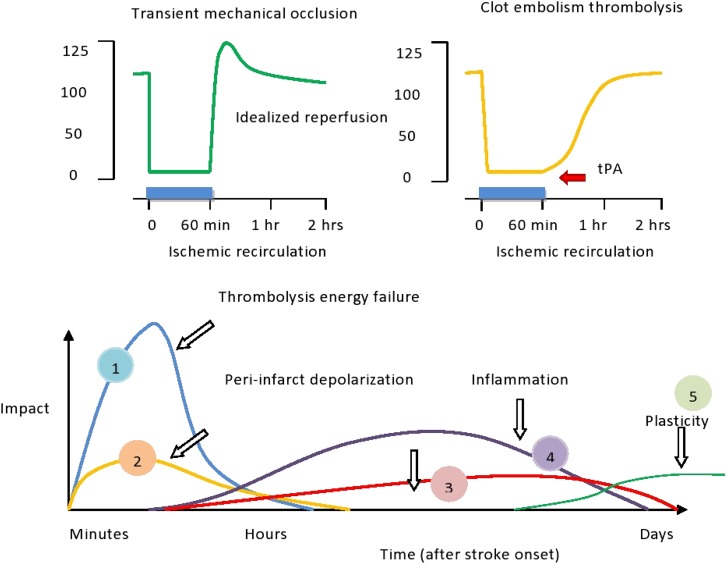
According to a book recently published by Ali and colleagues from Pakistan, the mean alarm to door time was reported to be 255.88±112.63 min (4.26±1.87 hours), mean door to CT time as 37.75±20.13 min (0.62±0.33 hours) and mean alarm to drug time as 314.88±116.12 min (5.24±1.93 hours). According to them, out of a total of 100 studied patients, only 29% reached their stroke care setup within the 4.5 hours window period as shown in figure 3. According to the authors, only 29% patients were feasible for thrombolysis. If their study results are observed, one can clearly see that after the patient is received at a tertiary care setup, the triage of events is quite practical in making thrombolysis possible (door to CT time of 0.62±0.33 hours). However, the major loss of precious window time period is not within the hospital but outside the premises, that is, alarm/stroke to door time (4.26±1.87 hours). The overall result is a late alarm to drug time (5.24±1.93 hours). This highlights the fact that the untimely diagnosis and arrival of patients with stroke at stroke care centres is another major contributor towards the failure of achieving a successful thrombolysis target protocol in Pakistan. The fact that brain tissue is viable to be salvaged within a given period of time is the key concept in understanding why the time frame for delivering thrombolysis or intervention is so crucial in acute ischaemic stroke as shown in figure 4.28–40
Figure 3.
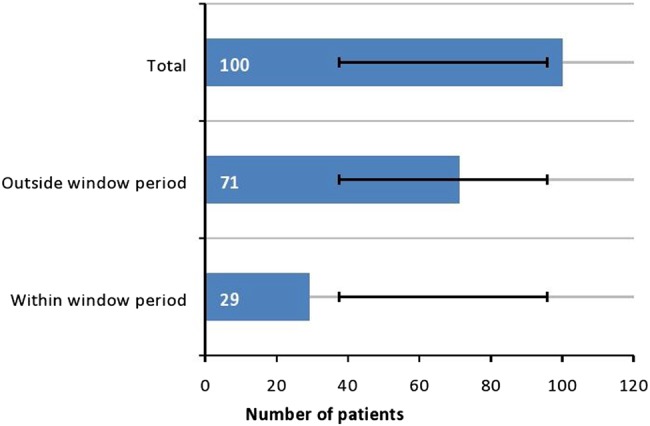
Graphical representation of patients within and outside window period for IV thrombolysis in a study conducted by Ali and colleagues in 2015–2016 (adapted from ref. 28). Out of the cohort of 100 patients, 29% had presented within the window period for IV thrombolysis. IV, intravenous.
Figure 4.
Process of tissue damage and time intervals for possible salvage in acute ischaemic stroke.
Current facilities for acute ischaemic stroke in Pakistan
The current stroke treatment in Pakistan can be divided into the following categories:
Intravenous thrombolysis: availability and expenses
Currently, only two centres provide the facility of ER triage of thrombolysis for acute ischaemic stroke and TIAs. These centres too have intervened in a limited number of cases so far. They receive no more than 55–65 acute ischaemic stroke cases per year as reported and the yearly intravenous (IV) thrombolysis rate is around 12–15/year. The data published on this experience are also sparse. Moreover, the cost of thrombolysis in Pakistan at these centres is between US$3000 and US$4500. The cost of IV recombinant tPA (rtPA) injection itself is around US$2250. The per capita income in Pakistan is US$450 on average. The rtPA is not authorised by the Ministry of Health in Pakistan as a registered medical product under licence of the Government of Pakistan yet and can only be arranged by individual hospitals on their own. All these issues need to be addressed separately and seriously. For this, neurologists all over the country have put forward a petition to convince the government to ponder on this fragile situation.4–6 20–26 33–38
Intra-arterial thrombolysis
Up until now, no centre in Pakistan has the expertise to offer intra-arterial rtPA. Various research publications have reported variable results for this mode of therapy and interest in its advancement is growing. This modality is under research and available only in a few centres around the globe for selected patients.4 5 23–26 33–38
Endovascular surgery
Endovascular surgery (EVS) is indicated for cases with a thrombus size >5 mm, which is not amenable to treatment with IV rtPA. No centre in Pakistan has the setup and expertise to offer the services of EVS. There is no trained EV surgeon/interventionist available in Pakistan at present. Those getting their training from abroad usually do not prefer to come back due to limited resources and scope of growth in their fields.24–26 33–38
Current treatment protocols
The current targeted treatment of acute ischaemic stroke in Pakistan includes the administration of aspirin as a loading dose of 300 mg combined within first 24 hours of event in the emergency. Along with this, supportive therapy is offered in the form of lipid-lowering medication, IV fluids, control of blood pressure and serum glucose levels, proton pump inhibitors, bladder and bowel care, mouth care, nursing care and bedside physiotherapy. The current acute stroke management in Pakistan practised at large at specialised stroke units is as shown in tables 1–4.2–6 20–26 33–39
Table 1.
Acute ischaemic stroke: an ER protocol (routinely followed protocols across Pakistan)
| Acute ischaemic stroke: an ER protocol | ||||
|---|---|---|---|---|
| 1. | Please carry out the following orders as appropriate | Yes | No | Date and time |
| 2. | Plain CT head STAT | |||
| 3. | CBC and platelet count | |||
| 4. | prothrombin time (PT), INR | |||
| 5. | Electrolytes, creatinine, glucose, Trop, liver function tests (LFTs) | |||
| 6. | 0.9% normal saline (NS) at 100 to 120 mL/hour for 24 hours. No dextrose saline (if congestive cardiac failure (CCF), use 0.9% NS at ≤60 to 70 mL/hour) | |||
| 7. | If systolic BP>185 mm Hg or diastolic BP>110 mm Hg for ≥2 readings taken 5–10 min apart, use hypertension management protocol | |||
| 8. | If random blood glucose >150 mg/dL, use S/C insulin protocol | |||
| 9. | Metoclopramide 10 mg IV every 8 hours (for nausea/vomiting) | |||
| 10. | Acetaminophen 1000 mg IV every 8 hours (for headache or fever >37.5°C) | |||
| 11. | Aspirin 300 mg loading dose PO in ER if haemorrhagic stroke ruled out | |||
BP, blood pressure; CBC, complete blood count; INR, international normalised ratio; IV, intravenous; PO, orally; S/C, subcutaneous; Trop, troponin.
Table 2.
Hypertension management protocol (routinely followed protocols across Pakistan)
| Hypertension management protocol | ||||
|---|---|---|---|---|
| 12. | Please carry out the following orders as appropriate | Yes | No | Date and time |
| 13. | If systolic BP>185 mm Hg or diastolic BP>110 mm Hg for ≥2 readings taken 5–10 min apart, use hypertension management protocol | |||
| 14. | If systolic BP>185 mm Hg or diastolic BP>110 mm Hg, treat with labetalol bolus or infusion | |||
| 15. | Give: IV labetalol 10–20 mg over 1–2 min | |||
| 16. | If still elevated after 10–15 min:The dose may be repeated every 10–15 min up to a total of no more than 300 mg/24 hours or give labetalol initial loading dose followed by infusion at 2–8 mg/min | |||
| 17. | Hold treatment if BP<185/110 mm Hg | |||
BP, blood pressure; IV, intravenous.
Table 3.
Clinical pathway for acute ischaemic stroke (routinely followed protocols across Pakistan)
| Clinical pathway for acute ischaemic stroke | ||||
|---|---|---|---|---|
| 18. | Please carry out the following orders as appropriate | Yes | No | Date and time |
| 19. | Admit to stroke unit or ICU for 48–72 hours (at a few centres only), then shift to general ward if stable | |||
| 20. | National Institute of Health Stroke Scale (NIHSS)/GCS (individual centre adapted protocols may differ) once/twice daily | |||
| 21. | CT scan of head repeated STAT if decreased level of consciousness or new deficit | |||
| 22. | Monitor vital signs (BP, HR, cardiac rhythm, scores, metabolic acidemia, pulse oximeter (SaPO2) (give oxygen as indicated), Temp and respiratory rate (RR)) | |||
| 23. | Monitor vital signs: every 30×3; every 1 hour×every 6 hours, then every 3 hours×every 10 hours (individual centre adapted protocols may differ) | |||
| 24. | Start mobilisation (in bed or chair) if stable (after functional assessment) | |||
| 25. | Bed rest for 24 hours | |||
| 26. | Keep nothing per oral (NPO) until swallowing screen done (if dysphagia present, keep NPO and repeat screen in 24 hours) | |||
BP, blood pressure; GCS, Glasgow Coma Scale; ICU, intensive care unit; NPO, nothing per oral; SaPO2, scores, metabolic acidemia, pulse oximeter; Temp, temperature.
Table 4.
Clinical stroke extended management pathway (routinely followed protocols across Pakistan)
| Clinical stroke extended management pathway | ||||
|---|---|---|---|---|
| 27. | Please carry out the following orders as appropriate | Yes | No | Date and time |
| 28. | Extracranial imaging: carotid Doppler, CTA, MRA) in 2–7 days | |||
| 29. | ECG in 2–7 days (trans thoracic echocardiography (TTE)/trans esophageal echocardiography (TEE) as indicated) | |||
| 30. | DVT prophylaxis | |||
| 31. | Stroke educational material for patient and family | |||
| 32. | Removal of Foley's catheter and start bladder management (if stable and feasible) | |||
| 33. | Discharged on:
|
|||
| 34. | Fasting lipid profile, HbA1c | |||
| 35. | Holter monitor (if indicated | |||
| 36. | Specialised workup for young stroke (like anti nuclear antibody (ANA), extractable Nuclear Antigen (eNA), etc) | |||
| 37. | Referral to:
|
|||
| 38. | Follow-up | |||
CTA, CT angiography; HbA1c, glycated haemoglobin; MRA, MR angiography.
Follow-up and rehabilitation
Follow-up protocols are defined at the level of tertiary care setups. However, practical implementation of these protocols is poor, especially for cases referred from smaller districts and villages. This emphasises the utmost need for establishing local stroke rehabilitation centres in the suburbs which can follow these patients and lessen the burden on the bigger stroke centres. Moreover, only a few centres are specialised in rehabilitation medicine where full-time support to stroke affectees is offered.2–5 21–26 33–37
Neuroradiological support
The radiological support in the diagnosis of acute stroke is also limited. Only the tertiary care teaching units are equipped with CT and MRI machines. After office hours, MRI facility is not available. The availability of functional MRI, perfusion scans and positron emission tomography/single-photon emission CT and digital subtraction angiography (DSA) is virtually non-existent.2 3 24–26 33–37
Stroke neurology training facility
There is no neurovascular training facility in Pakistan at present, except for a single centre in Karachi with only one fellow trained per year. The total number of neurologists registered until now date in Pakistan is fewer than 200 according to the statistical records updated in 2016. More than half of these are residing abroad. So the lack of trained personnel in the face of limited resources and poor financial support culminates in a system lagging far behind in treatment of acute stroke in Pakistan.41
Role of Pakistan Stroke Society and Pakistan Society of Neurology in awareness and advocacy
The Pakistan Stroke Society (PSS) was established in 2001. Its main objective is to improve prevention and care of stroke in Pakistan by increasing the public and physicians’ awareness. The PSS is affiliated with the International Stroke Society, which is an advisory body to the WHO. The society has more than 200 physician members.42
The society is actively working for the past 15 years holding seminars, public awareness sessions and walks with/for patients with stroke. The first International Stroke Conference was held in 2004 in Lahore followed by its successive chapters over the years. Every year, international speakers participate in an annual stroke conference from all over the world including participants from the USA, Canada, Emirates, India, Japan, Greece, China and many more. In the recent 2016, several conferences were held on neurology including an annual meeting in Quetta on stroke prevention and management. A comprehensive stroke course was held which included eight workshops and trained over 400 doctors specifically in stroke. There were also more than 20 seminars on stroke recognised countrywide and given substantial media coverage. Awareness was made by organising public awareness days like Stroke Day and National Disability Day and has become a norm on the part of PSS and Pakistan Society of Neurology (PSN). To further engage the general public, there were 8 press conferences, 20 media appearances, 6 newspaper articles and more than 1000 news items published covering various perspectives of stroke. Billboards, posters and brochures were used as well. Additionally, the PSN has recently launched a Facebook page and website. Guidelines for stroke in Pakistan have been published providing detailed national guidance under the circumstances of having limited resources. Of a total of 40 neurology centres, 18 have been approved for Fellowship of College of Physicians and Surgeons (FCPS) training by the efforts of PSS and PSN. This year, more than 30 medical doctors passed FCPS neurology, amounting to a total of 200 neurologists in the country and contributing towards handling the heavy stroke burden in Pakistan. The Pakistan Journal of Neurological Sciences is a good quality quarterly journal where contributions from members and associated faculty of PSS and PSN have been substantial. Currently, it is available on the web, E-commons, Higher Education Commission (HEC), Pakistan Medical and Dental Council (PMDC) and WHO-Regional Office for the Eastern Mediterranean (EMRO) and plans to be on PubMed by 2017/2018. Moreover, it is a premier journal for stroke and related neurosciences in Pakistan. Furthermore, a public awareness magazine Jehan-e-Aesab is being published since January 2016 creating countrywide awareness about stroke. It aims to promote medical writing in Urdu, and is targeting media, faculty, lay people, patients and attendants to create awareness about stroke and other neurological diseases in the local and national languages for a more effective process of communication.41 42
National stroke care guidelines43
As of 2010, the national stroke care guidelines provide a comprehensive and clear strategy for care of patients with stroke in Pakistan. The salient features of the guidelines state:
Prehospital recognition and stroke triage: to decrease delays in presentation to care via a track record of admitting and managing patients with stroke.43
In-hospital management: by following strict protocols at subsequent stroke care steps.
Emergency department
Rapid airway, breathing and circulation management.
Rapid assessment of neurological deficits.
Determination of time of onset of stroke symptoms.
Determination of presence of risk factors.
Standardised use of NIHSS stroke scale score.
If rtPA is available at the facility, use of National Institute of Neurological Disorders and Stroke (NINDS) recommendations for stroke chain of survival: 10 min for the emergency physician evaluation, specialist (neurologist) assessment within 10 min, and 25 min to CT scan, allowing rtPA administration within 45 min to an hour.
Imaging of the brain: an emergency non-contrast head CT.
Ancillary testing at the very least should consider a 12 lead ECG, blood tests for diabetes, abnormal lipids, coagulopathy and screen for chronic renal failure.
Control of blood pressure with those who receive IV rtPA requiring strict control of blood pressure to below 185/110 mm hg.
The Food and Drug Administration (FDA) approved treatment protocol for thrombolysis for acute stroke presenting within 3–4.5 hours of symptom onset using IV rtPA.43
Other parameters
Control of core body temperature.
A desired level of glucose between 80 and 140 mg/dL.
Urgent anticoagulation with the goal of preventing early recurrent stroke, halting worsening or improving outcomes after ischaemic stroke is not recommended. This is regardless of the aetiology of stroke, for example, cardioembolic stroke. Anticoagulation is contraindicated within 24 hours of administration of rtPA.
Antiplatelet therapy with aspirin 160–325 mg daily, given orally (or per rectum in patients who cannot swallow), and started within 48 hours of onset of presumed ischaemic stroke.
Patients should receive isotonic hydration and free fluids should be avoided. Nutritional supplementation is not necessary.
Evaluation for aspiration is needed prior to initiation of diet and the diet should be modified accordingly.
Screening for the presence of swallowing problems with the water swallowing tests and modifications in the diet should be made accordingly. Patients who fail the initial swallowing screen should get a nasogastric tube placed for medications and feeds. Those who are having difficulty handling even their basic secretions may actually benefit from nil per oral policy in the initial 24 hours.
All patients unable to mobilise independently should ideally be provided with a pressure relieving mattress as an alternative to a standard hospital mattress. Also, there should be standing instructions for repositioning these patients every 2 hours to avoid pressure sores.
Avoidance of deep vein thrombosis in immobilised patients via frequent movements and the use of low-dose subcutaneous heparin is suggested in the acute phase. Intermittent compression devices are recommended in those where the risk of intracerebral hemorrhage (ICH) is high.
Early rehabilitation.
Avoid routine use of steroids.
Avoid injudicious use of neuroprotection and neurotonics.43
- Posthospital management:
- Aspirin in a dose ranging from 75 to 300 mg is efficacious in stroke prevention. Clopidogrel is marginally better at increased cost and is therefore suggested in those with concomitant peripheral vascular disease and/or intolerance to aspirin.
- Combination therapy in patients with stroke with aspirin and clopidogrel has higher risks of symptomatic ICH and should be used only for TIA.
- Dose-adjusted warfarin is suggested in an international normalised ratio 2–3 for those who have intermittent or continuous atrial fibrillation.
- Goal to reduce blood pressure and any antihypertensive which will ensure compliance in the long run is preferable. Therefore, the drug should be selected depending on the availability and the financial status of the patient.
- Patients with ischaemic stroke or TIA with elevated cholesterol, comorbid coronary artery disease or evidence of an atherosclerotic origin should be counselled regarding lifestyle modification, dietary guidelines and statins are recommended.
- The recommendations for glucose control should be the same for patients with and without a prior stroke. Control of other modifiable cardiovascular risk factors in a patient with diabetes like aggressive blood pressure control and lipid control is warranted.
- Physicians should ask their patients repeatedly to quit smoking for primary and secondary prevention.
- More aggressive dietary control and regular physical activity.
- Dietary salt restriction.
- Early identification and management of depression poststroke is vital to ensure early recovery and to prevent cognitive impairment. Conventional tricyclic antidepressants are contraindicated among patients with stroke due to their adverse effects. selective serotonin reuptake inhibitor (SSRIs) have a low adverse effect profile and a good efficacy, making them invaluable in patients with multiple comorbidities.43
Paediatric stroke in Pakistan
According to internationally available literature, ischaemic stroke in children occurs in 55% of all strokes, the rest being haemorrhagic. This is in contrast to adult demographics among whom ischaemic stroke comprising 80–85% of all strokes. Delay in diagnosis is common in the paediatric population and thus opportunities for timely intervention are substantially limited. Experience of thrombolysis in paediatric stroke is non-existent. Furthermore, the risk factor account for stroke in children is more versatile than that in the adult population. Among these are central nervous system infections, cardiac diseases (congenital as well as acquired), vasculopathies (fibromuscular dysplasia and Moyamoya disease), vasculitides, sickle cell disease, coagulopathies and arterial dissection.44
A local study from Pakistan by Chand and colleagues identified a total of 29 paediatric patients with acute ischaemic stroke over a period of 5 years. Their mean age was ∼4.5 years with 76% over infancy. Male-to-female ratio was 3:1 and mean duration of symptoms at the time of presentation was ∼5.75 hours. Seizures (mostly generalised tonic–clonic), loss of consciousness and paresis were the most common clinical presentations as observed by them. Other common features included fever, vomiting, cranial nerve palsies, delayed development, headache and blindness. They reported a positive family history of stroke among these children to be only 3.5%. Unique ECG findings particular to the paediatric population included myocarditis tetralogy of Fallot, complex congenital heart disease and ventricular septal defect. Hypercoagulopathy (protein S and/or protein C deficiency) was found in 37.5% for those having its workup done. They conclude that multiple strokes, cardiovascular diseases and age below 1 year were associated with higher mortality.44
Another observational study conducted by Siddiqui et al45 concluded that the main aetiology of stroke in children was causing strokes in 56.09% of children and the majority of children (78.26%) in this group were below 5 years.44
In the background of the aforementioned studies, it is clear that characteristics of stroke described for the paediatric population differ significantly from those for adults but scarce data, more so in this age group, make understanding limited.44 45 It is therefore of utmost importance that stroke should not be considered only a disease of adults, but a national database registry should be set up for children with stroke. Furthermore, stroke centres should be established separately as an integral part of a paediatric care hospital having a recognised department for paediatric neurology.
Stroke in women in Pakistan
There are very limited data of hospital-based studies and stroke registries about stroke in women, especially in young women in South Asia. There is poor reporting of stroke in women in South Asia, despite it being a leading cause of death in women aged above 60 years. This is probably because women with stroke or cardiac arrest in this part of the world are less likely to be taken to hospital than men with these conditions due to various reasons including level of education, socioeconomic status, overall literacy rate, local social values and community beliefs. Two studies on stroke in young women from eight Asian countries found that large-vessel thrombosis (24%), cortical vein thrombosis (CVT) (21%) and cardioembolism (19%) were the most common mechanisms of stroke in this population with a significant proportion related to pregnancy, especially postpartum.7
Genetic aspects of stroke in Pakistan
Genetic aspects of stroke have been studied to a very limited extent until now in South Asia and almost none in Pakistan. While basic research has gained pace regarding local demographic data, advanced research and genetic studies are almost non-existent.7
Epidemiological studies of families, homozygous and heterozygous twins have shown a distinct genetic component in the predisposition to stroke. In this regard, three polymorphisms in the phosphodiesterase 4D (PDE4D) gene were evaluated in 200 patients with stroke compared with 250 controls from a single study in Pakistan. The study concluded that there is an association between the single nucleotide polymorphism (SNP) SNP83 and patients with ischaemic stroke.
An India-based study showed that SNP41, SNP56 and a novel SNP in the PDE4D gene were associated with various stroke subtypes. Some studies have shown significantly positive associations between the E-selectin gene polymorphism Ser128Arg and ischaemic stroke. Others have suggested a link between the ACE and AAD1 genes and extracranial and intracranial atherosclerosis contributing to ischaemic stroke. A study from Chennai, India showed that paraoxonase 1 (PON1) activity and PON1 Gln192Arg genotypes are associated with ischaemic stroke.7
A recent database for genetic studies has been started to gather data on such patients by individual efforts at a few centres across Pakistan but a national database registry specifically for studying genetic aspects has not yet been formulated in this regard. This needs to be done in the near future to help determine patients who might be at risk of stroke among the Pakistani population.
Future perspectives
While Pakistan is lagging behind countries of the developed world in stroke neurology in general and management of acute ischaemic stroke in particular, there has been some commendable progress in recent times. In Karachi, Aga Khan University Hospital has the facility to deliver state-of-the-art stroke management. It has recently been established and has treated a decent number of patients with thrombolysis in the past 2 years. In Islamabad, Shifa International Hospital has an ongoing research study in which they have successfully treated more than a dozen patients with acute ischaemic stroke in the year 2015 with IV thrombolysis. Coming to public sector hospitals, the neurology department of Pakistan Institute of Medical Sciences has put forward a proposal to the federal government for the establishment of an acute stroke unit and is also sending one of its neurologists abroad for training in vascular neurology. The future of stroke seems promising in Pakistan with the newly established Centre of Neurosciences in Lahore, which is to be inaugurated this year. A much larger scale project is on its way to start within a year or so in Islamabad, especially to deliver stroke management expertise. The establishment of new stroke centres and allocation of funds for the progress of stroke neurology in Pakistan is encouraging and that day is not far when Pakistan will be at par with the West in modern fundamentals of stroke neurology.2 4 5 20–26 39–42
Footnotes
Competing interests: None declared.
Provenance and peer review: Commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1.Khealani BA, Hameed B, Mapari UU. Stroke in Pakistan. J Pak Med Assoc 2008;58:400–3. [PubMed] [Google Scholar]
- 2.Kamal AK, Itrat A, Murtaza M, et al. The burden of stroke and transient ischemic attack in Pakistan: a community-based prevalence study. BMC Neurol 2009;9:58 doi:10.1186/1471-2377-9-58 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Murray CJ, Lopez AD. Mortality by cause for eight regions of the world: Global Burden of Disease Study. Lancet 1997;349:1269–76. doi:10.1016/S0140-6736(96)07493-4 [DOI] [PubMed] [Google Scholar]
- 4.Feigin VL. Stroke epidemiology in the developing world. Lancet 2005;365:2160–1. doi:10.1016/S0140-6736(05)66755-4 [DOI] [PubMed] [Google Scholar]
- 5.World Health Organization (WHO). The Atlas of Heart Disease and Stroke. http://www.who.int/cardiovascular_diseases/resources/atlas/en/
- 6.Kamal AK, Taj F, Junaidi B, et al. The Karachi Intracranial Stenosis Study (KISS) protocol: an urban multicenter case-control investigation reporting the clinical, radiologic and biochemical associations of intracranial stenosis in Pakistan. BMC Neurol 2009;9:31 doi:10.1186/1471-2377-9-31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wasay M, Khatri IA, Kaul S. Stroke in South Asian countries. Nat Rev Neurol 2014;10:135–43. doi:10.1038/nrneurol.2014.13 [DOI] [PubMed] [Google Scholar]
- 8.Khan RA, Khan MW, Rauf A, et al. A review on alarming stroke situation in Pakistan. PGJMMS 2015;1:26–030. [Google Scholar]
- 9.Nomani AZ, Nabi S, Ahmed S, et al. High HbA1c is associated with higher risk of ischaemic stroke in Pakistani population without diabetes. Stroke Vasc Neurol 2016;1:133–9. doi:10.1136/svn-2016-000018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nomani AZ, Iqbal M, Jamil U, et al. Etiology of stroke in young Pakistani adults; results of a single center study. Pak J Neurol Sci 2015;10:18–22. [Google Scholar]
- 11.Burke TA, Venketasubramanian RN. The epidemiology of stroke in the East Asian region: a literature-based review. Int J Stroke 2006;1:208–15. doi:10.1111/j.1747-4949.2006.00060.x [DOI] [PubMed] [Google Scholar]
- 12.Johnston SC, Gress DR, Browner WS, et al. Short-term prognosis after emergency department diagnosis of TIA. JAMA 2000;284:2901–6. [DOI] [PubMed] [Google Scholar]
- 13.Kamal A, Khimani F, Raza R, et al. Characteristics of TIA and its management in a tertiary care hospital in Pakistan. BMC Res Notes 2008;1:73 doi:10.1186/1756-0500-1-73 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rothwell PM, Giles MF, Chandratheva A, et al. , Early use of Existing Preventive Strategies for Stroke (EXPRESS) study. Effect of urgent treatment of transient ischaemic attack and minor stroke on early recurrent stroke (EXPRESS study): a prospective population-based sequential comparison. Lancet 2007;370:1432–42. [DOI] [PubMed] [Google Scholar]
- 15.Kennedy J, Hill MD, Ryckborst KJ, et al. , FASTER Investigators. Fast assessment of stroke and transient ischaemic attack to prevent early recurrence (FASTER): a randomized controlled pilot trial. Lancet Neurol 2007;6:961–9. [DOI] [PubMed] [Google Scholar]
- 16.Easton JD, Saver JL, Albers GW, et al., American Heart Association; American Stroke Association Stroke Council; Council on Cardiovascular Surgery and Anesthesia, et al. Definition and evaluation of transient ischemic attack: a scientific statement for healthcare professionals from the American Heart Association/American Stroke Association Stroke Council; Council on Cardiovascular Surgery and Anesthesia; Council on Cardiovascular Radiology and Intervention; Council on Cardiovascular Nursing; and the Interdisciplinary Council on Peripheral Vascular Disease. The American Academy of Neurology affirms the value of this statement as an educational tool for neurologists. Stroke 2009;40: 2276–93. doi:10.1161/STROKEAHA.108.192218 [DOI] [PubMed] [Google Scholar]
- 17.Qureshi MS, Iqbal M, Nomani AZ. Rapidly increasing prevalence and associations of diabetes mellitus in a rural community of Pakistan. Journal of Diabetology. 2014;3:3. [Google Scholar]
- 18.Mayhew G, Carhart E. Differential diagnosis: Bell's palsy vs. stroke. They can look similar, but it's important to tell them apart. EMS World 2015;44:47–53. [PubMed] [Google Scholar]
- 19.Ko Y, Lee S, Chung JW, et al. MRI-based algorithm for acute ischemic stroke subtype classification. J Stroke 2014;16:161–72. doi:10.5853/jos.2014.16.3.161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hjalmarsson C, Manhem K, Bokemark L, et al. The role of prestroke glycemic control on severity and outcome of acute ischemic stroke. Stroke Res Treat 2014;2014:694569 doi:10.1155/2014/694569 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Khealani BA, Khan M, Tariq M, et al. Ischemic strokes in Pakistan: observations from the national acute ischemic stroke database. J Stroke Cerebrovasc Dis 2014;23:1640–7. doi:10.1016/j.jstrokecerebrovasdis.2014.01.009 [DOI] [PubMed] [Google Scholar]
- 22.Xu ZP, Li HH, Li YH, et al. Feasibility and outcomes of intravenous thrombolysis 3–4.5 hours after stroke in Chinese patients. J Clin Neurosci 2014;21:822–6. doi:10.1016/j.jocn.2013.08.014 [DOI] [PubMed] [Google Scholar]
- 23.Sharma VK, Tsivgoulis G, Tan JH, et al. Feasibility and safety of intravenous thrombolysis in multiethnic Asian stroke patients in Singapore. J Stroke Cerebrovasc Dis 2010;19:424–30. doi:10.1016/j.jstrokecerebrovasdis.2009.07.015 [DOI] [PubMed] [Google Scholar]
- 24.Khan M, Kamal AK. Acute administration of rt-PA for acute stroke in Pakistani patients—what does the available evidence teach us? J Pak Med Assoc 2010;60:967–9. [PubMed] [Google Scholar]
- 25.Mahmood A, Sharif MA, Ali UZ, et al. Time to hospital evaluation in patients of acute stroke for alteplase therapy. Rawal Med J 2009;34:43–6. [Google Scholar]
- 26.Buchan AM, Barber PA, Newcommon N, et al. Effectiveness of t-PA in acute ischemic stroke: outcome relates to appropriateness. Neurology 2000;54:679–84. doi:10.1212/WNL.54.3.679 [DOI] [PubMed] [Google Scholar]
- 27.Butcher K, Shuaib A, Saver J, et al. Thrombolysis in the developing world: is there a role for streptokinase? Int J Stroke 2013;8:560–5. doi:10.1111/j.1747-4949.2012.00923.x [DOI] [PubMed] [Google Scholar]
- 28.Nomani AZ, Ahmed S, Nabi S. Ischemic stroke patients presenting in IV rTPA window period: a single public sector hospital experience in Pakistan. Scholars' Press 2015:76–81. [Google Scholar]
- 29.Paul CL, Levi CR, D'Este CA, et al. , Thrombolysis ImPlementation in Stroke (TIPS) Study Group. Thrombolysis ImPlementation in Stroke (TIPS): evaluating the effectiveness of a strategy to increase the adoption of best evidence practice—protocol for a cluster randomised controlled trial in acute stroke care. Implement Sci 2014;9:38 doi:10.1186/1748-5908-9-38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fonarow GC, Zhao X, Smith EE, et al. Door-to-needle times for tissue plasminogen activator administration and clinical outcomes in acute ischemic stroke before and after a quality improvement initiative. JAMA 2014;311:1632–40. doi:10.1001/jama.2014.3203 [DOI] [PubMed] [Google Scholar]
- 31.Ford AL, Williams JA, Spencer M, et al. Reducing door-to-needle times using Toyota's lean manufacturing principles and value stream analysis. Stroke 2012;43:3395–8. doi:10.1161/STROKEAHA.112.670687 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Heidenreich PA, Trogdon JG, Khavjou OA, et al., American Heart Association Advocacy Coordinating Committee; Stroke Council; Council on Cardiovascular Radiology and Intervention, et al. Forecasting the future of cardiovascular disease in the United States a policy statement from the American heart association. Circulation 2011;123:933–44. doi:10.1161/CIR.0b013e31820a55f5 [DOI] [PubMed] [Google Scholar]
- 33.Khealani BA, Wasay M. The burden of stroke in Pakistan. Int J Stroke 2008;2:1–4. [DOI] [PubMed] [Google Scholar]
- 34.Kamal AK, Khealani BA, Ansari SA, et al. Early ischemic stroke presentation in Pakistan. Can J Neurol Sci 2009;36:181–6. doi:10.1017/S0317167100006545 [DOI] [PubMed] [Google Scholar]
- 35.Khealani BA, Syed NA, Maken S, et al. Predictors of ischemic verses hemorrhagic stroke in hypertensive patients. J Coll Physicians Surg Pak 2005;15:22–5. doi:01.2005/JCPSP.2225 [PubMed] [Google Scholar]
- 36.Basharat RA, Yousaf M, Iqbal J, et al. Frequency of known risk factors for stroke in poor patients admitted to Lahore general hospital in 2000. Pak J Med Sci 2002;18:280–3. [Google Scholar]
- 37.Siddiqui M, Khan FS, Khatri IA. Clinical patterns and risk factors for stroke in 120 stroke patients in a tertiary care hospital with designated stroke center. Pak J Neurological Sci 2006;1:58. [Google Scholar]
- 38.Ahmad A, Usman F, Hassan A. Risk factors and pattern of stroke in Islamabad, Pakistan. Rawal Med J 2009;34:47–50. [Google Scholar]
- 39.Memon TF, Lakhair MA, Shaikh M, et al. Socio-demographic risk factors for hemorrhagic and ischemic stroke: a study in tertiary care hospital of Hyderabad. Pak J Neurol Sci 2016;11:24–9. [Google Scholar]
- 40.Siddiqi SA, Kamran SH, Almadni AA. From tip to tpa. Pak J Neurol Sci 2016;11:44–5. [Google Scholar]
- 41.Wasay M. Present and future of neurology in Pakistan. Pak J Neurol Sci 2016;11:1–2. [Google Scholar]
- 42.Pakistan Stroke Society—Pakistan Society of Neurology. http://pakneurology.net/pages/StrokeSociety.asp
- 43.Kamal AK, Itrat A, Naqvi I, et al. Ischemic stroke care—official guidelines from the Pakistan Society of Neurology. Pak J Neurol Sci 2010;51:38–43. http://ecommons.aku.edu/pakistan_fhs_mc_med_med/128 [Google Scholar]
- 44.Chand P, Ibrahim S, Matloob Muhammad A, et al. “Acute childhood ischemic stroke: a Pakistani tertiary care hospital experience,” Pakistan J Neurol Sci (PJNS) 2016;11:2 http://ecommons.aku.edu/pjns/vol11/iss1/2 [Google Scholar]
- 45.Siddiqui TS, Rehman AU, Ahmed B. Etiology of strokes and hemiplegia in children presenting at Ayub Teaching Hospital, Abbottabad. J Ayub Med Coll Abbottabad 2006;18:60–3. [PubMed] [Google Scholar]