Abstract
Ninety-four unilateral CI patients with bimodal listening experience (CI plus HA in contralateral ear) completed a questionnaire that focused on attitudes toward hearing aid use postimplantation, patterns of usage, and perceived bimodal benefits in daily life. Eighty participants continued HA use and 14 discontinued HA use at the time of the questionnaire. Participant responses provided useful information for counseling patients both before and after implantation. The majority of continuing bimodal (CI plus HA) participants reported adapting to using both devices within 3 months and also reported that they heard better bimodally in quiet, noisy, and reverberant conditions. They also perceived benefits including improved sound quality, better music enjoyment, and sometimes a perceived sense of acoustic balance. Those who discontinued HA use found either that using the HA did not provide additional benefit over the CI alone or that using the HA degraded the signal from the CI. Because there was considerable overlap in the audiograms and in speech recognition performance in the unimplanted ear between the two groups, we recommend that unilateral CI recipients are counseled to continue to use the HA in the contralateral ear postimplantation in order to determine whether or not they receive functional or perceived benefit from using both devices together.
Keywords: bimodal hearing, cochlear implant, hearing aid, bimodal benefit
Introduction
As criteria for cochlear implantation have become less restrictive, the number of people with a unilateral cochlear implant (CI) and usable residual hearing in the contralateral ear is increasing. Hearing in the unimplanted ear can vary over a very wide range. Unilateral cochlear implantees now include persons with bilateral moderate to profound sensorineural hearing loss. Persons with normal to moderate low-frequency hearing and steeply sloping high-frequency loss can also qualify for a CI. These unilateral CI recipients can benefit from using a hearing aid (HA) in the unimplanted ear (bimodal stimulation).
It has been recommended that bimodal fittings be prescribed for all cochlear implantees who have usable residual hearing in the unimplanted ear (e.g., Ching, Incerti, & Hill, 2004; Dorman & Gifford, 2010; Offeciers et al., 2005). The HA can provide complementary low-frequency information not available from the CI and thus improve speech recognition performance in quiet and in noise (e.g., Ching et al., 2004; Zhang, Dorman, & Spahr, 2010). Availability of low-frequency acoustic information in combination with the signal from the CI also can result in improved sound quality (e.g., Ching et al., 2004; Flynn & Schmidtke, 2004; Potts, Skinner, Litovsky, Strube, & Kuk, 2009) and better music perception (e.g., Crew, Galvin, Landsberger, & Fu, 2015; Kong, Stickney, & Zeng, 2005; Sucher & Mcdermott, 2009). Bimodal device users also report improved quality of life (Farinetti et al., 2015). Use of both CI and contralateral HA also provides some benefits of binaural hearing such as improved ability to recognize speech in noise and improved sound localization (e.g., Ching et al., 2004; Morera et al., 2012).
The prevalence of bimodal use is lower than might be expected based on the number of unilateral CI recipients with residual hearing in the contralateral ear (e.g., Fitzpatrick, Séguin, Schramm, Chenier & Armstrong, 2009, Scherf & Arnold, 2014; Yamaguchi & Goffi-Gomez, 2013). Surveys of “cochlear implant audiologists” reveal that clinicians need guidelines for bimodal candidacy and management (Fielden & Kitterick, 2016; Scherf & Arnold, 2014; Siburt & Holmes, 2015). For instance, it would be helpful to have guidelines regarding the audiologic characteristics of those who actually continue to use a HA postimplantation. A recent study by Devocht et al. (2015) reported that of 77 persons identified as potential bimodal users, 49 persons continued HA use, and 28 persons discontinued use by 1 year postimplantation. The two groups shared similar demographics, but differed in the degree of hearing loss and in speech recognition performance in the unimplanted ear. Those who continued to use a HA had significantly better hearing in the unimplanted ear. The mean pure-tone average (PTA, mean of thresholds at 500, 1000, and 2000 Hz) of the continuing HA group was 92.3 dB HL and the mean unaided consonant-nucleus-consonant (CNC) score was 38.2%. The mean PTA of the discontinued group was 102.1 dB HL and the mean unaided CNC score was 16.3%. Mean speech recognition performance with the CI did not differ significantly between groups (52.7% for continuing group, 59% for those who discontinued). Other retrospective studies also provide evidence that those who discontinue HA use have less residual hearing in the unimplanted ear than those who continue HA use. In two other studies, mean PTA of nonbimodal users exceeded 100 dB HL in the unimplanted ear (e.g., Farinetti et al., 2015; Fitzpatrick et al., 2009).
While there is agreement about the potential benefits of bimodal use, few data are available about how patients decide whether or not to continue using their HA after implantation. Fitzpatrick and colleagues developed questionnaires to investigate attitudes of unilateral CI patients toward using the HA after implantation, patterns of usage, and perceived benefits or lack of bimodal benefit in daily life. One questionnaire focused on unilateral CI participants who continued to use a HA postimplantation (Fitzpatrick et al., 2009). The second questionnaire focused on those who discontinued HA use postimplantation (Fitzpatrick & Leblanc, 2010). Fitzpatrick et al. (2009) reported that approximately 25% of 124 unilateral CI patients who were implanted between 1993 and 2005 continued to use a HA for at least 3 months after implantation. A questionnaire regarding HA usage, patterns of usage, and benefits of bimodal use was sent to these 31 patients and was completed by 24 bimodal users. Only 15 of these respondents used the CI + HA regularly (HA use more than 50% of the time) and 4 respondents used the HA <50% of the time. Five people reported discontinuing the HA within 6 months of implantation. Bimodal users reported that they adapted quickly to using the HA with the CI and the majority preferred using both devices in all situations (quiet, noisy, and reverberant). A smaller number preferred using the CI alone in various listening situations. The majority of the bimodal users reported that they did not require modification to their HA after implantation and that they adjusted the volume control of either the HA or the CI when they used the devices together.
Fitzpatrick and Leblanc (2010) focused on those who discontinued HA use. They identified 49 persons with unilateral CI (implanted between 1999 and 2009) who had used a HA in the unimplanted ear prior to receiving a CI and discontinued use of HA immediately or within 6 months of using a CI. Only 28 (of 49) questionnaires were completed. The majority of respondents indicated full-time use of a HA in the unimplanted ear before receiving a CI, and that they had found amplification to be helpful. Before implantation, respondents had not decided whether they would use a HA in the unimplanted ear after CI activation. The majority of respondents also indicated that their audiologist discussed possible use of the HA after implantation. Only 5 of the 28 respondents tried using the HA with the CI for more than 1 month. Nine tried using the HA for more than 1 week and nine did not try using the HA at all. Those who tried using the HA reported using it full time. Fitzpatrick and Leblanc (2010) identified several factors underlying the decision to discontinue HA use. These included a negative perception of the helpfulness of the HA prior to implantation and the fact that the CI was perceived as being much better than the HA. Additional reasons for discontinuing HA use included lack of added benefit from using the HA with the CI, better sound quality from the CI than the HA, and degraded sound when using the HA with the CI.
These studies have raised important questions about how unilateral CI users decide whether or not to continue HA use. More information about the experience of those using the HA postimplantation is needed because of the small number of respondents in these studies. It is also difficult to know how representative the experience of these respondents might be compared with unilateral CI users who use the CI + HA consistently for longer periods of time. The aim of the current study is to describe the experiences with device usage by a group of unilateral CI recipients in our center who continued to use a HA in the contralateral ear for at least 3 months after implantation. The practice in our Center is to recommend that persons receiving a unilateral CI who use a HA in the contralateral ear prior to implantation continue to use the HA on a regular basis. Patients are counseled to use the HA most of the day, but to practice using the CI alone for 2 h a day in order to adjust to the signal from the CI. We administered a questionnaire in order to obtain information about how these patients actually use the CI and HA after implantation, their attitudes toward both devices, their patterns of HA and CI usage, and perceived benefits or disadvantages of using a HA and CI together. We extracted demographic and audiometric data from clinical files in order to identify possible differences between the subgroups of bimodal patients who continued or did not continue to use their HA.
Methods
This study was approved by the Institutional Review Board of the New York University School of Medicine.
Questionnaire
A questionnaire was administered to elicit information about the experience of our bimodal patients with their HA before and after cochlear implantation. The questionnaire is based on the questionnaires developed by Fitzpatrick et al. (2009) and by Fitzpatrick and Leblanc (2010) and includes additional questions relevant to HA use. For a list of the questions and potential responses see Supplementary Material 1.
The questionnaire consisted of three sections. The first section of the questionnaire was to be completed by all participants. Questions focused on (a) experience with HAs before receiving the CI, (b) experience with the CI, and (c) the decision to use a HA after implantation. The second section was only for those who continued to use the HA at the time they were completing the questionnaire. Questions focused on (a) information about their HA, (b) their pattern of HA and CI usage, (c) perceived benefits of the devices, (d) their adaptation to the HA and follow-up care/modifications to the HA postimplantation. The third section of the questionnaire was to be completed by participants who discontinued HA use. Questions focused on (a) length of HA use and frequency/pattern of usage, (b) information about follow-up care/modifications to the HA postimplantation, (c) their perception of speech with CI + HA, and (d) their reasons for discontinuing HA use. Each question was followed by a set of potential responses. The task of the participant was to check the box that best reflected his or her answer to the question. Additional space was provided for the participant’s comments.
Data Collection
Questionnaires were distributed to potential participants either during a visit to our laboratory (as participants in unrelated research projects relevant to bimodal hearing) or during their appointment for clinical services at the NYU Cochlear Implant Center. All participants were given the questionnaire with a preaddressed, stamped return envelope. They were asked to complete the questionnaire at home and return the completed questionnaire by mail. Some of these participants elected to complete the questionnaire on site, while others took the questionnaire home and mailed it back to our center.
Demographic and audiometric data for the participants were extracted from the patient’s file from the clinical appointment date closest to questionnaire completion. Audiometric data for the unimplanted ear consisted of the unaided and aided pure tone thresholds, as well as aided speech recognition scores on CNC words (Peterson & Lehiste, 1962) and the AZBio Sentence Test in noise (Spahr et al., 2012). The speech recognition scores were obtained with the personal HA, the everyday CI MAP, and when using both CI + HA. The clinical speech recognition protocol is carried out using recorded test materials in soundfield (speech level is 60 dBA).
Participants
All participants were unilateral CI recipients recruited at the NYU Cochlear Implant Center. Each had at least 3 months experience using their CI and were documented as having used a HA in the contralateral ear for at least 3 months after implantation. One hundred and one questionnaires were distributed. Ninety-four participants completed and returned the questionnaires. Sixty-five of these participants were also participating in CI-related studies at our laboratory. The remaining participants were patients being seen for care at the Cochlear Implant Center.
The responses to the questionnaires were used to determine how many of the participants continued to use the HA and how many no longer used a HA. Eighty of the participants continued to use the HA with the implant on a daily basis (we will refer to these participants as “continuing hearing aid users”) and 14 reported that they had discontinued use of the HA (we will refer to these participants as “discontinued hearing aid users”).
Demographic information for the participants appears in Table 1 and information about the CI used by participants in Table 2. In these two tables, data are presented separately for those who continued to use a HA and those who discontinued using a HA. Information about the HA used by continuing HA participants appears in Table 3.
Table 1.
Demographic Information for 80 Participants Who Continued HA Use and 14 Participants Who Discontinued HA Use.
| Continue HA use (N = 80) | Discontinued HA use (N = 14) | |
|---|---|---|
| Age (years): M (SD) | 64.5 (16.3) | 64.8 (12.9) |
| Gender (N) | 29 M, 51 F | 7 M, 7 F |
| Hearing loss (years): M (SD) | 32.7 (16.3) | 33.6 (19.6) |
| HA use (years): M (SD) | 23.3 (15.3) | 27.0 (20.4) |
| CI use (years): Mdn (range) | 1.3 (.21–12.8) | 2.9 (0.89–11.9) |
| Mdn LF PTA HA ear (250 and 500 Hz) | 61.25 dB HL (unaided) 40.0 dB HL (aided) | 73.8 dB HL (unaided) 43.75 dB HL*(aided) |
| Mdn PTA HA ear (500, 1000, and 2000 Hz) | 81.67 dB HL (unaided) 44.17 dB HL (aided) | 92.2 dB HL (unaided) 48.33 dB HLa (aided) |
| Etiology (N) |
Etiology (N) | |
| Unknown | 32 | 4 |
| Noise induced | 10 | 2 |
| Meniere’s | 6 | 1 |
| Otosclerosis | 9 | 0 |
| Ototoxicity | 2 | 1 |
| Trauma | 2 | 0 |
| Genetic | 5 | 4 |
| Other | 14 | 2 |
| Ear implanted | 50 right, 30 left | 4 right, 5 left, 5 bilateral |
Note. HA = hearing aid; M = mean, SD = standard deviation; Mdn = median; N = number; M = male; F = female; LF PTA = low-frequency pure tone average; PTA = pure tone average.
Data Available for only 10 of the 14 Discontinued HA users.
Table 2.
CI Devices (Implant Type, Processor, and Strategy) Used by Participants.
| Continue HA use (N = 80) |
Discontinued HA use (N = 14) |
|||||||
|---|---|---|---|---|---|---|---|---|
| Processor | N | Strategy | N | Processor | N | Strategy | N | |
| Cochlear | Freedom | 6 | ACE | 54 | Freedom | 2 | ACE | 10 |
| N5 | 34 | N5 | 5 | |||||
| N6 | 14 | N6 | 3 | |||||
| Advanced bionics | Naida Q70 | 11 | CIS | 1 | Naida Q70 | 2 | Optima S | 2 |
| Optima S | 8 | Harmony | 2 | S-Fidelity 120 | 2 | |||
| Optima P | 2 | |||||||
| Harmony | 10 | P-Fidelity 120 | 5 | |||||
| S-Fidelity | 5 | |||||||
| Med-El | Sonnet | 1 | FS4 | 1 | ||||
| Opus 2 | 4 | FSP | 3 | |||||
| FS4-P | 1 | |||||||
Note. CI = cochlear implant; HA = hearing aid; N = number.
Table 3.
Hearing Aids (Manufacturer) and Type of HAs Used by Continuing HA Users.
| N | |
|---|---|
| HA manufacturer | |
| Audibel | 1 |
| Hansaton | 1 |
| Miracle ear | 2 |
| Oticon | 15 |
| Phonak | 37 |
| Resound | 6 |
| Siemens | 3 |
| Starkey | 5 |
| Telex | 1 |
| Unitron | 1 |
| Widex | 8 |
| HA styles | |
| Behind the ear | 55 |
| Receiver in canal | 19 |
| In the ear | 5 |
| Completely in canal | 1 |
Note. HA = hearing aid; N = number.
Data Analysis
Demographic and audiological information extracted from clinic files were analyzed to describe the demographic and audiometric characteristics of the participants.
Speech recognition scores (% correct) were analyzed within groups using the Friedman Repeated Measures Analysis of Variance (RMANOVA) on Ranks, followed by Tukey’s post hoc tests. The Mann–Whitney Rank Sum Test was used for between-group comparisons (of the continuing HA group and the discontinued group) on audiometric characteristics and on measures of speech recognition performance. This nonparametric test that compares the medians of different groups was used because some of the data (e.g., PTA values) were not normally distributed. Note that in the introductory section and later in the discussion section we will also refer to mean values in order to facilitate comparison with previous studies.
Questionnaires were coded to indicate whether the participant was a continuing HA user or had discontinued HA use. The answer to each question was entered into a spreadsheet using numbers assigned to each potential response. The frequency of response to each question (in percent) is described in the results section. For open-ended questions, actual responses were documented.
Results
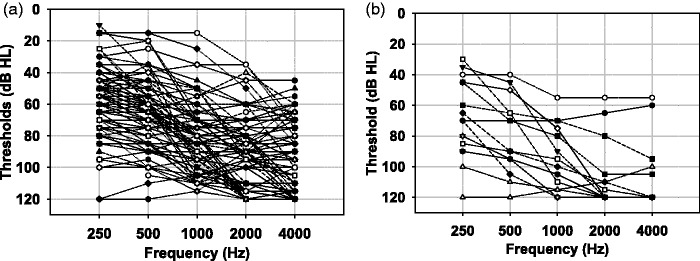
Audiograms for the unimplanted ear of continuing HA users are shown in Figure 1(a) and for those participants who discontinued HA use in Figure 1(b). Note that thresholds of 120 dB were used when no response to the signal was obtained at the limits of the audiometer output. Inspection of the audiograms reveals substantial overlap in the range of audiometric thresholds among participants in the two groups.
Figure 1.
(a) Pure tone audiograms of the unimplanted ear of 80 bimodal patients who continue to use a hearing aid. (b) Pure tone audiograms of the unimplanted ear of 14 patients who discontinued hearing aid use after a period of bimodal experience.
On average, the continuing HA users had more residual hearing than those who discontinued HA use. Median pure tone averages (PTA, average of mean thresholds at 500, 1000, and 2000 Hz) were 81.7 dB HL for the continuing HA group and 99.2 dB HL for the discontinued group. The Mann–Whitney Rank Sum Test revealed that these medians differed significantly (U = 406, p = 0.002). However, the difference in median low-frequency pure tone averages (LF PTA, average of mean thresholds at 250 and 500 Hz) was not statistically significant (p > .05). Median LF PTAs were 61 dB HL for the continuing HA group and 74 dB HL for the discontinued group.
Next, we analyzed CNC word recognition performance by participants to determine the effect of test condition (HA alone, CI alone, and CI + HA). Separate analyses were carried out for the continuing HA users and the discontinued HA users. For the continuing HA group, speech recognition in quiet was poorest with the HA alone and best in the bimodal test condition. Median CNC scores were 24%, 65%, and 72% for the HA alone, CI alone, and CI + HA conditions, respectively. The Friedman RMANOVA on Ranks revealed that test condition was significant, χ2(df = 2) = 79.25, p < .001. The Tukey’s post hoc test revealed significant differences in performance (p < .05) between all three conditions.
For the discontinued HA group, median CNC scores were 8%, 64%, and 64% for the HA alone, CI alone, and CI + HA conditions, respectively. The Friedman RMANOVA on ranks revealed that test condition was significant, χ2(df = 2) = 17.07, p < .001. The Tukey’s post hoc test revealed that CNC scores differed significantly (p < .05) between the HA alone and CI alone condition, and between the HA alone and the CI + HA condition. CI + HA did not differ significantly from the CI alone score.
As seen earlier, median CNC scores with the CI were similar for the continuing HA group and the discontinued HA group. The Mann–Whitney Rank-Sum Test confirmed that median CI alone scores did not differ significantly between the two groups (U = 458.5, p = .283).
Speech recognition performance on CNC words by individual participants as a function of device is shown in Figure 2. Filled circles represent participants who continue HA use and open triangles represent performance by participants who discontinued HA use. Performance with the HA alone and the CI alone is compared in the top panel. Almost all patients who discontinued using the HA show relatively low performance with the HA. All of these participants show significantly higher scores with the CI. Scores obtained with the HA by continuing HA users span the entire range from 0% to 100%. In most cases, performance with the CI is better than with the HA. Some of the participants have similar scores with either device. There are a number of participants with better performance with the HA than with the CI (see data points below the lower confidence interval limits).
Figure 2.
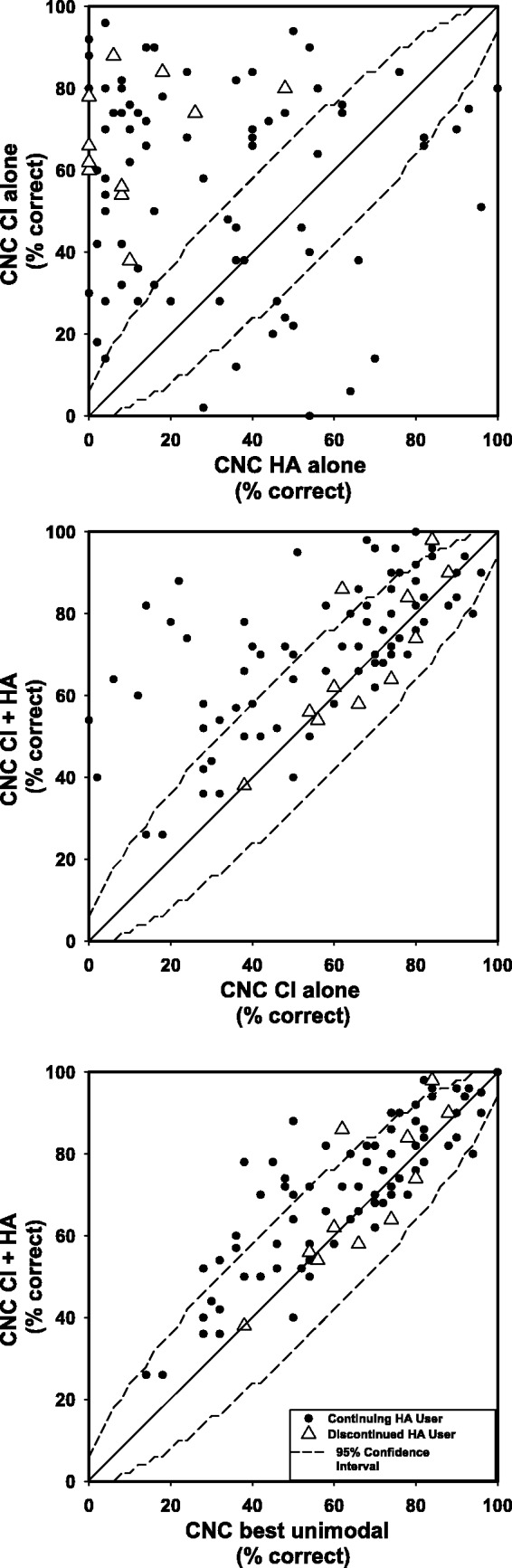
Top panel: Comparison of CNC (consonant-nucleus-consonant) word scores for individual bimodal users tested using the HA alone and the CI alone. The diagonal line represents equivalent performance. The dashed lines represent the upper and lower 95% confidence interval for a single list comparison. Filled circles represent data of continuing hearing aid users. Open triangles represent users who discontinued HA use. Middle panel: Comparison of CNC (consonant-nucleus-consonant) word scores for individual bimodal users tested using the CI alone and the CI + HA. Bottom panel: Comparison of the best unimodal (either CI alone or HA alone) condition score and the bimodal (CI + HA) condition score for individual users on CNC (consonant-nucleus-consonant) words.
In the middle panel of Figure 2, we compare performance with the CI + HA (y-axis) to performance with the CI alone (x-axis). For continuing HA users, the majority of CI + HA scores exceed CI alone scores, with a large number of participants (38%) having bimodal scores significantly higher than CI alone (scores above the 95% confidence interval). In contrast, only 2 of the 11 discontinued HA users (18%) showed significantly higher performance with CI + HA than with CI alone, for the remainder CI + HA scores were not significantly better than with the CI alone.
In this group of unilateral CI users, sometimes the best speech recognition performance is with the HA rather than the CI. So, a more accurate measure of bimodal benefit is to compare bimodal performance with the best unimodal performance. In the bottom panel of Figure 2, we compare CI + HA performance (y-axis) to the best unimodal performance. Bimodal performance is equivalent to or significantly better than the best unimodal performance for all but one continuing HA users. Approximately 20% of the continuing HA users obtained significantly higher bimodal than unimodal CNC scores. While bimodal performance was equivalent to best unimodal performance for the majority of the discontinued HA users (9 of the 11), there were two discontinued users who obtained significant bimodal benefit.
Performance on the AZBio Sentence Test in noise (10 dB SNR) confirmed the benefit of bimodal aiding for the continuing HA users. Median scores were 36%, 53%, and 76% in the HA, CI, and CI + HA conditions, respectively. The Friedman RMANOVA on Ranks revealed that performance differed significantly as a function of test condition, χ2 (df = 2) = 62.55, p < .001. Tukey’s post hoc testing revealed that performance in the CI + HA condition was significantly higher than with either HA or CI alone (p < .05). The difference between scores with the HA alone and CI alone was not significant (p > .05).
A scatterplot of the continuing HA users’ CI alone performance in comparison with HA alone performance on the AZBio Sentence Test (10 dB SNR) is shown in the top panel of Figure 3 (data are not available in the HA alone condition for discontinued users). As can be seen, the majority of the continuing HA users obtain better performance with the CI alone than with the HA alone and a much smaller number obtain similar performance with each device alone. Almost 20% of the participants obtain significantly better scores with the HA than with the CI. As seen in the middle panel of the figure, for all but two participants, performance with CI + HA is either significantly better than (above 95% confidence interval) or equivalent to (within 95% confidence interval) performance with the CI alone. As seen in the bottom panel of the figure, CI + HA performance is better than or equal to the best unimodal performance for all but two participants.
Figure 3.
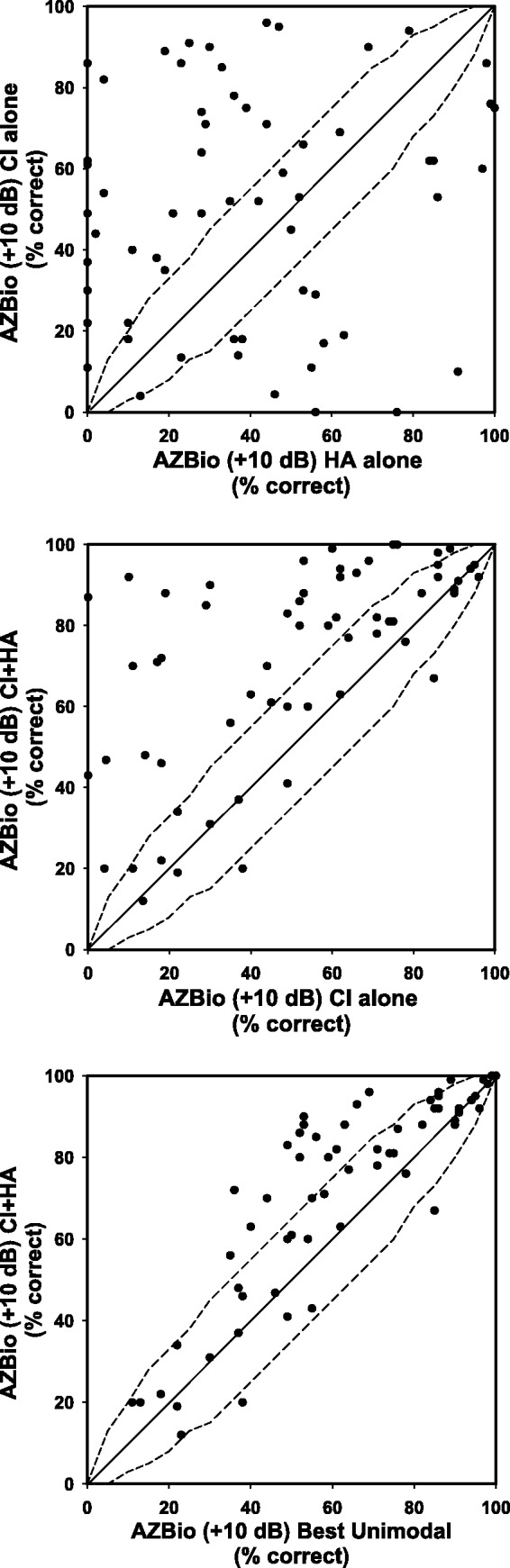
Top panel: Comparison of AZBio sentence scores for individual continuing HA users tested using the HA alone and the CI alone. The diagonal line represents equivalent performance. The dashed lines represent the upper and lower 95% confidence interval for a single list comparison. Middle panel: Comparison of AZBio sentence scores for individual continuing HA users tested using the CI alone and the CI + HA. Bottom panel: Comparison of AZBio sentence scores for individual continuing HA users in the best unimodal (either CI alone or HA alone) condition and the bimodal (CI + HA) condition.
AZBio in noise scores were not available in the HA condition or the bimodal test condition for the discontinued users. However, data were available with the CI for 11 of 14 individuals in the discontinued HA group. The Mann–Whitney Rank-Sum Test was used to compare performance between the HA continued and discontinued groups for CI alone performance. Median scores were 53% for the continuing group and 63% for the discontinued group. This difference was not statistically significant (U = 299.50, p = .218).
Questionnaire Results
The percent of responses to select questions is summarized later. Note that there are 80 continuing HA users and 14 who discontinued. The frequency of responses to each question is listed in table format in Supplementary Material 1.
Questions Answered by All Participants
HA use and perceived benefit (before cochlear implantation)
All participants used a HA in the unimplanted ear prior to implantation. The majority used two HAs before receiving a CI. The majority of the participants (87% continuing, 79% discontinued) reported using their HAs more than 10 h a day before they received a unilateral CI, with the remainder of the continuing participants and all but one in the discontinued group reporting that they used their HA(s) from 5 to 10 h per day.
At the time of implantation, the majority of participants were using current HA technology (HA < 6 years old). Continuing HA users considered their HAs to be more helpful than those who discontinued HA use. In particular, 37% of the continuing HA users and only 14% of those who discontinued HA found the HA to be very helpful.
Decisions made regarding continuing HA use before implantation
All patients at the Cochlear Implant Center are counseled to continue to use the HA with the implant. It appears that a higher percentage of those who continued HA use intended to use the HA after implantation: 86% of the continuing HA users and 64% of those who discontinued reported deciding to continue to use a HA before the implant surgery. The majority of the respondents indicated that their audiologist had encouraged them to try using the HA in conjunction with the CI before or after the CI surgery (81% continuing HA users, 86% of those who discontinued HA use). A small number replied that they had not been encouraged by their audiologist to wear a HA (10% in the continuing HA group, 14% in the discontinued group) and 9% of the continuing participants replied that they did not remember.
Experience With the CI
The majority of both continuing HA users and those who discontinued using the HA felt that they heard better with the CI than with their HAs (86% who continued using a HA, 100% who discontinued). But 5% of the continuing HA users reported that they heard about the same with the CI as with the HA, and 9% felt that they heard worse with the CI than with their HA (consistent with CNC scores shown in top panel of Figure 2).
The majority of participants indicated that they coped with hearing loss much better after they received their CI than before implantation. Whereas before implantation, 40% of the continuing users felt they coped with hearing loss “well much of the time” or “all of the time,” after implantation, the number rose to 86%. After implantation, the number of the continuing HA users indicating that they could cope well only “some of the time” was reduced from 37% preimplant to 13% with the CI.
Those who discontinued HA use also reported coping with hearing loss much better after implantation. Whereas before implantation, only 21% reported that they coped with hearing loss “well much of the time” or “all of the time,” after implantation, the number rose to 92%. After, implantation the number indicating that they could cope well only “some of the time” was reduced from 36% to 0%. The number that reported that they did “not cope well at all” decreased from 43% to 8%.
Patterns of HA/Bimodal Use by Continuing HA Users
The majority of the continuing HA users (75%) indicated that they were using the same HA as they used before they received their CI. Fifty-four percent of those who continued to use a HA reported having adjustments made to their HA in the past year, and the remainder reported that their HA did not need to be adjusted.
Eighty-five percent of the continuing HA users reported using their HA with the implant right away and 13% within 1 to 3 months after implantation. The majority reported that they adapted quickly to using the HA and CI together: 57% reported adapting right away and 29% adapted within 1 to 3 months. A small number indicated that it took a bit longer to adapt to using both devices: 5% within 3 to 6 months and 6% after the first 6 months. A very small number (3%) reported that they had not adapted to using both.
The majority of the group (81%) indicated that they use their HA in conjunction with the CI more than 10 h a day and 17% use their HA 5 to 10 h per day. Only one person reported using the HA for less than 5 h a day.
When asked whether they ever use the HA alone, 54% indicated that they would never wear the HA alone and 44% indicated that they might wear the HA alone “sometimes.” Only two respondents indicated that they often wore the HA alone. Examination of the speech recognition performance of these users revealed rather poor performance with the CI (<10% CNC word score). One of these patients had substantially better performance with the HA and the second patient had slightly better performance with the HA.
In the group of continuing HA users, 41% indicated that they never use only the CI, 53% indicated that they sometimes use only the CI, and 6% (5 patients) indicated that they often wear only the CI. These five were patients with a significantly higher CNC word score with the CI alone than with the HA alone.
Experience of Continuing HA Use Group With Coordination of HA/CI Controls
In response to a question about how they set the volume on the CI and the HA when they wear both, it was clear that bimodal patients use different strategies: 25% reported that they do not change the volume on either the HA or the CI; 21% adjust only the CI volume (no change on HA); 21% keep the same CI volume, but adjust the HA volume; 14% adjust the volume on both HA and CI for different situations (19% have a HA without a volume control).
We were also interested in determining whether those who continued to use a HA perceived the sound as balanced between the CI and the HA. In response to the question asking where participants hear the sound when using the CI and HA together, 32% reported hearing sound in the middle of their head, 36% reported hearing sound closer to the ear with the implant, 10% reported hearing sound closer to the ear with the HA, and 22% reported hearing sound separately in both ears. In response to a question about where sound is louder when using CI and HA, 59% indicated that sound is louder in the CI ear, 16% indicated that sound is louder in the HA ear, and 26% that the level of the sound is similar in both ears.
Both the CI speech processor and the HA can have multiple settings (or programs) in several different memories. It was of interest to determine how bimodal users control these settings of the HA and the CI. Those who change the setting on the HA were in the minority: 15% indicated that they usually change the HA and 5% indicated they manipulated the settings on the HA and the CI. Forty-nine percent indicated that they kept the HA on the same program with or without the CI and 31% indicated that their HA only has one program.
Benefits of Bimodal Hearing for Continuing HA Users
Participants were asked to indicate which device(s) yielded better hearing in quiet, noisy, and reverberant environments, and for listening to music. Results are shown in Table 4. For the majority of participants, using the CI and HA together yielded better hearing in all four conditions. A small number indicated a preference for listening to music with the HA alone.
Table 4.
Device Preference of Continuing HA Users as a Function of Environment or Signal.
| CI | HA | CI + HA | No preference | Total N | |
|---|---|---|---|---|---|
| Quiet | 4% | 2.5% | 91% | 2.5% | 80 |
| Noise | 5% | 3% | 79% | 14% | 79 |
| Reverberation | 3% | 7% | 69% | 21% | 72 |
| Music | 1% | 15% | 68% | 16% | 75 |
Note. CI = cochlear implant; HA = hearing aid; N = number of reponses. Numbers represent the percentage of participants indicating choice of device(s) judged to yield better hearing.
Continuing HA users were asked whether wearing both HA and CI helped in deciding which direction sounds are coming from. A minority indicated that they could never decide on the direction of the sound direction (25%), while others indicated varying levels of help in sound direction identification with the HA: 10% “almost always,” 20% “often,” and 44% “sometimes.”
Postimplant Experience With HAs by the Discontinued HA Group
Recall that five of those who discontinued HA use obtained a second CI. Of the 14 discontinued HA users, four unilateral and two of the bilateral respondents used the HA for more than a year postimplantation, one bilateral CI user had worn the HA for 6 to 12 months, and five unilateral and two of the bilateral respondents used the HA for 1 to 6 months. Four of 13 participants reported that adjustments had been made to the HA during the time period of use.
Patterns of HA Usage by Those Who Discontinued HA Use
Nine of 13 respondents indicated that they had worn the HA everywhere, the others indicated selective use (either at work or at home). Eleven (of 14) indicated that they had worn the HA in both quiet and noisy situations. Two participants indicated they had worn the HA when listening to music.
Perception of Speech When Using HA With CI
Six participants found speech to be less clear when using the HA together with the CI than when listening with the CI alone (three participants report that speech was not clear, three participants reported interference between the CI and the HA). Two participants reported that initially speech was clearer when using the HA with the CI, but that over time they no longer found the HA to be helpful. One participant reported that speech sounded more natural with the CI alone. One participant focused on hearing speech with the HA and reported that he could not understand many words with the HA (alone).
Reasons for Discontinuing HA Use
Reasons given for discontinuing using the HA included lack of helpfulness of the HA (nine), speech was unclear with HA (six), interference between the HA and CI (three), the added expense of using the HA (one), and too much bother to use both devices (one).
Comments by Participants
As part of the questionnaire, participants were offered the opportunity to add comments about their experience using the CI and HA together. See Supplementary Material 2 for a listing of all comments.
The comments of the bimodal users (continuing HA group) revealed their perception of the value of continued HA use. Perceived bimodal benefits included the following: the ability to hear better when using the HA along with the CI, benefits of “bilateral” hearing, improvements in sound quality, and improved quality of life. Comments also included information about their experiences using both devices: the struggles with acclimating to the sound from the CI, the need for continued attention to the HA, and the continuing difficulties experienced (even when using both devices).
Comments by participants who discontinued HA use primarily reflected dissatisfaction with the HA.
Discussion
We obtained information from a relatively large group of participants who continued to use a HA (80) and a much smaller group of participants (14) who discontinued using their HA. A limitation of this study is that participants represent a convenience sample and are not necessarily representative of all unilateral CI users implanted at our center that either continued or discontinued HA use in the contralateral ear. Many of the participants were participating in studies of bimodal hearing, so they may have had extra motivation to continue HA use. The data represent “a snapshot in time.” We realize that those who were continuing HA users at the time that they completed the questionnaire might discontinue using the HA at a later date because they no longer perceive benefit, because of decreases in hearing in the unimplanted ear or because they decide that they might obtain greater assistance from a second CI. Nevertheless, results from the questionnaire provide useful information for counseling patients both before and after implantation.
The 94 unilateral CI recipients who participated in our study displayed a wide range of residual hearing in the unimplanted ear (from mild to profound hearing loss). The PTA of the continuing HA group (mean = 78 dB HL, median = 82 dB HL) is substantially better than the average hearing loss that has been reported in some previous studies of the characteristics of bimodal device users (e.g., Devocht et al., 2015; Farinetti et al., 2015; Fitzpatrick et al., 2009). Inspection of our data reveals that 62 of the 80 continuing group were implanted between February 2010 and February 2015. It is likely that the better hearing in the unimplanted ear of the continuing HA users in the present study reflects less restrictive criteria for allowable residual hearing in the contralateral ear of CI recipients. The mean PTA of the 14 discontinued users was 93 dB HL (Median = 99 dB HL). Seven in the group had profound hearing loss, while the remaining seven participants had more residual hearing. On average, this group has slightly more hearing than the 28 persons who discontinued HA use in the report by Fitzpatrick and Leblanc (2010).
There was considerable overlap in the audiograms of the continuing HA users and those who discontinued using the HA. On average, the continuing HA group had more residual hearing in the mid-frequencies (median PTA for 500, 1000, and 2000 Hz), but had similar low-frequency PTAs (250 and 500 Hz). The data suggest that those with more residual hearing at 1000 and 2000 Hz are more likely to continue using the HA, but for CI recipients with poorer thresholds at those frequencies, it is not possible to determine whether they will continue to use a HA or not. Because of the substantial overlap in the audiograms of the continuing and the discontinued users, we see that the audiogram alone will not predict whether a person will continue HA use.
On average, the continuing HA users obtained better open set speech recognition performance with the HA than those who discontinued using the HA. However, there were large individual differences among participants who continued HA use. CNC scores with the HA ranged from 0 to 100%. As with the audiograms, there was considerable overlap. While 13 of 14 of those who discontinued HA use had CNC scores <30% with the HA, 40 of the 80 continuing HA participants also had CNC scores in this range. Again, the speech recognition score with the HA does not necessarily predict who will continue to use a HA.
The difference in performance with the HA alone and the CI alone may play a factor in the decision whether or not to continue HA use. All 14 of those who discontinued using the HA had significantly higher performance on the CNC test with the CI than with the HA. In contrast, there were some continuing HA users who had similar scores with the HA and with the CI, and a minority with better performance with the HA than the CI.
The clinical measures of speech recognition provided some useful information for individuals for whom it was possible to demonstrate bimodal benefit (significant increases in performance in the bimodal condition from the best unimodal condition). For individual continuing HA participants, bimodal speech recognition in quiet and in noise was either significantly better than or equivalent to performance with the CI alone (see middle panels of Figures 2 and 3) or to best unimodal performance (see bottom panels of Figures 2 and 3). For the majority of those who discontinued HA use, no bimodal benefit was observed; the bimodal score was equivalent to the CI score. In this group, only 2 of the 11 persons with CNC scores in the bimodal condition had significantly better CNC bimodal scores than CI alone scores.
On average, speech recognition performance with the CI was similar for the two groups, both in quiet and in noise. This finding of similarity between the speech recognition outcomes in the CI ear of those who use a HA contralaterally and those who do not has also been reported by Devocht et al. (2015). Audiologists can thus feel comfortable recommending simultaneous use of the CI and the HA immediately after CI activation. Everyday use of the HA postimplantation does not appear to have a negative effect on CI-alone performance.
Among the continuing HA users, there were a number of participants who had asymmetric hearing loss preimplantation. These individuals had severe or profound hearing loss with extremely poor aided speech recognition in one ear, and substantial residual hearing with very good HA performance in the contralateral ear. The fact that these persons pursued implantation shows that they were experiencing difficulty with communicative function in their daily life. The continued use of both devices and the results of the questionnaire indicating that the CI is used in all listening environments are consistent with perceived benefit and lack of interference between the devices for this group. These results are consistent with other studies reporting clinical and functional benefits obtained by unilateral CI patients with substantial residual hearing and good speech recognition performance in the contralateral HA (e.g., Plant, van Hoesel, McDermott, Dawson, & Cowan, 2016).
Questionnaire
The majority of continuing HA users reported that they hear better with the CI than they heard with their HAs before implantation and that they cope much better with their hearing loss since receiving the CI. The majority of those who continued to use the HA reported hearing better in quiet, noisy, and reverberant environments when using both the CI and HA together.
Patterns of HA Use and Attention to the HA by Continuing HA Users
The pattern of adaptation and usage by continuing HA users was similar to that reported by Fitzpatrick et al. (2009). All participants had used a HA in the unimplanted ear before implantation and the majority used the HA more than 10 h/day. Many of these participants (86%) decided to continue to use their HA even before the surgery took place. Most of the bimodal users indicated consistent HA use after surgery (more than 10 h/day), with occasional use of either the CI alone or the HA alone, and that they adapted to using the devices together quickly (immediately or within 3 months of CI activation).
The majority of our participants receive care for their HA from their preimplant HA provider (at a different facility). In many cases, the CI audiologist will notice a drop in the performance with the HA and will recommend that the patient follow-up with their HA audiologist. In other cases, the patient initiates the follow-up care himself. Responses of continuing HA users indicated that many realized the importance (and value) of continued attention to the HA. The majority reported seeing their HA audiologist for follow-up care. Approximately half reported having the HA adjusted after implantation. Information about the nature of the adjustments was not available, since those changes were made elsewhere.
Responses to questions about how users manipulate volume controls on the CI and the HA revealed that some of the participants adjust the volume control of the CI and others adjust the HA. It has been suggested by some that it is important to balance the loudness of the sound from the CI and the HA (e.g., Blamey, Dooley, James, & Parisi, 2000; Ching et al., 2004; Keilmann, Bohnert, Gosepath, & Mann, 2009), although recent research suggests that it may be adequate to set each device for most comfortable listening level (Dorman et al., 2014). It appears that for many of this group of bimodal patients, loudness is not balanced between the CI and the HA. The majority of respondents indicated that sound is heard closer to the ear with the implant and is louder in the ear with the implant. The lack of balance of loudness was not an impediment to continued use of the HA.
The majority of continuing HA users did not change the HA program (in multi-memory HA) or CI program when using both devices. This is not surprising. It is likely that patients would find it confusing to try out different programs and figure out the combination of settings on the HA and the CI that would be appropriate for different listening environments. It is only recently that CI and HA companies have begun to focus on coordinating approaches to signal processing between the CI and the HA (e.g., Veugen, Chalupper, Snik, van Opstal, & Mens, 2016) or on considering how to set the signal processing strategies in the HA to work better with the CI (e.g., Stender, 2016). It remains to be seen whether these approaches will yield significant improvements in bimodal function.
HA Fitting and Expected Outcomes for Bimodal Device Users
It is important to point out that criteria for a “good fit” of the HA may be different for bimodal users than for clients who are dependent only on a HA. In most cases, the HA provides information that is complementary to that from the CI. It may be more important for the audiologist fitting the HA to focus more on providing amplification in the low- and mid-frequency region, and less important to try to provide high-frequency speech information (made available by the CI). More information is becoming available regarding options for fitting the HA and the CI for bimodal patients as results from research studies relevant to bimodal fitting strategies become available (e.g., English, Plant, Maciejczyk, & Cowan, 2016; Fowler, Eggleston, Reavis, McMillan, & Reiss, 2016; Neuman & Svirsky, 2014; Zhang, Dorman, Gifford, & Moore, 2014). The recent move by CI companies to link their CI with specific HAs is also leading to suggested fitting strategies for the CI/HA pair (e.g., Advanced Bionics, 2016; Stender, 2016).
The clinical speech scores of our participants show that even when the CNC scores with the HA alone are very low, the user may obtain improved bimodal speech recognition performance. Therefore, the audiologist should not recommend discontinuing HA use based on performance with the HA alone. But clinical speech scores for individual participants did not always show significant improvement when comparing performance with the CI alone to performance with the CI + HA. For quite a few of our participants, the best unimodal score was quite high on the speech tests and so it was not possible to measure improvements in performance in the bimodal condition. Inclusion of more difficult speech recognition in noise tasks that are more representative of real world listening situations may be helpful in overcoming this problem (e.g., Gifford & Revit, 2010; Neuman, Wroblewski, Hajicek, & Rubinstein, 2012). The audiologist should not necessarily conclude that the HA will not confer functional benefit to the patient when improvement in performance is not seen in the bimodal test condition. The results of the questionnaires revealed that even in absence of improved bimodal speech recognition performance on the clinical speech tests, the continuing HA users report hearing better when using both devices, improved sound quality, improved sound localization, and/or benefit from awareness of sound from the side of the unimplanted ear. These findings are consistent with previous reports (e.g., Ching et al., 2004; Kong et al., 2005; Potts et al., 2009).
Frequency and Patterns of Usage by Those Who Discontinued HA Use
The information obtained from those who discontinued HA use supplements the information obtained by Fitzpatrick and Leblanc (2010). Although those who discontinued HA use are a small fraction of our sample, they provide important information not readily available from previous studies. For example, the majority (18 of 28) of participants in the Fitzpatrick and Leblanc (2010) study who discontinued HA use either did not try using the HA at all or used it for less than 1 week. Five had used their HA for more than 1 month and 4 for less than 1 month. In our sample, six of the participants reported using the HA for more than a year, one used the HA for 6 to 12 months and seven used the HA between 3 and 6 months. The majority indicated that they had used their HA consistently in multiple environments. Therefore, it appears that these participants had given an adequate trial to bimodal usage in order to determine whether or not the HA was beneficial.
It is noteworthy that individuals who discontinued HA reported great difficulty coping with their hearing loss before implantation than those who continued HA use (6/14 reported they did not cope well at all and 5/14 coped well only some of the time). It is also evident that the percentage of discontinued users who had decided to continue using the HA before implantation (64%, 9/14 participants) was lower than for the continuing participants. This may be related to their feeling that the HA was not helping them cope adequately with their listening needs. Most of these participants perceived large changes in their ability to cope after implantation. After implantation, 8/13 reported coping well much of the time and 4/13 reported coping well all of the time. The contrast in ability to function with hearing before and after implantation was less obvious in the reports of the continuing HA users. Those who discontinued HA use reported that using the HA with the implant did not provide better hearing than using the CI by itself. This report is consistent with the poor CNC speech scores among those participants, their significantly higher scores in the CI ear than the HA ear, and with the lack of bimodal benefit in the CI + HA test condition. Other reported reasons for discontinuing the HA were that speech was unclear with the HA, the sound from the HA interfered with the signal from the CI, it was a bother to use both devices, or it was not worth the added expense of the HA.
Conclusions
The preponderance of the evidence in the study suggests that the combined use of a contralateral HA with a CI is often perceived as beneficial. Interference from the HA that would affect performance with the CI seems quite rare. Thus, audiologists should recommend to all patients who are receiving a unilateral CI to continue using their HA in the contralateral ear, at least initially. Patients who chose to continue HA use included those with a very wide range of residual hearing, up to and including some with profound hearing loss. While many continuing HA users in our sample had CNC speech recognition scores higher than 30%, there were substantial numbers with CNC scores <30%. Poor speech recognition performance in the unimplanted ear does not automatically mean that a patient will not appreciate the benefits of bimodal hearing. Neither the audiogram nor the speech recognition performance with the HA alone will predict whether the person receiving a unilateral CI will benefit from using the contralateral HA. Since the questionnaire revealed that most patients adapted quickly to using the HA and the CI together, it makes sense to counsel patients to try using the HA with the CI for at least 3 months and then discuss with the patient their experience with using both devices (frequency of usage, whether or not they hear better when using both devices, and benefits or problems they may experience when using both devices).
It is important to counsel bimodal patients that upkeep of the HA is important. Patients should have periodic evaluations of their performance with their HA in the same manner as they did before being implanted. Patients should also be made aware that their HA may need to be reprogrammed, or that at some point they may need to purchase a new HA in order to take advantage of improved “bimodal” technology. The decision to continue using the HA should be reevaluated at regular intervals to assure that the patient’s hearing needs continue to be satisfied.
Supplementary Material
Acknowledgments
We thank Elizabeth Fitzpatrick for permission to use a modified version of the questionnaires published in Fitzpatrick et al. (2009) and Fitzpatrick and Leblanc (2010). The questions from the two questionnaires were combined and some questions were modified. We are grateful to Keena Seward and Margaret Miller for assistance with data collection.
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by grant R01DC011329 from NIH/NIDCD.
References
- Advanced Bionics (2016) Adaptive Phonak digital bimodal fitting formula: Optimizing hearing for listeners with a cochlear implant and Contralateral hearing aid White Paper, Valencia, CA: Author. [Google Scholar]
- Blamey P. J., Dooley G. J., James C. J., Parisi E. S. (2000) Monaural and binaural loudness measures in cochlear implant users with contralateral residual hearing. Ear and Hearing 21: 6–17. [DOI] [PubMed] [Google Scholar]
- Ching T. Y., Incerti P., Hill M. (2004) Binaural benefits for adults who use hearing aids and cochlear implants in opposite ears. Ear and Hearing 25: 9–21. [DOI] [PubMed] [Google Scholar]
- Crew J. D., Galvin J. J., 3rd, Landsberger D. M., Fu Q. J. (2015) Contributions of electric and acoustic hearing to bimodal speech and music perception. PLoS One 10(3): e0120279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Devocht E. M., George E. L., Janssen A. M. L., Stokroos R. J. (2015) Bimodal hearing aid retention after unilateral cochlear implantation. Audiology and Neurotology 20(6): 383–393. [DOI] [PubMed] [Google Scholar]
- Dorman M. F., Gifford R. H. (2010) Combining acoustic and electric stimulation in the service of speech recognition. International Journal of Audiology 49: 912–919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dorman M. F., Loizou P., Wang S., Zhang T., Spahr A., Loiselle L., Cook S. (2014) Bimodal Cochlear implants: The role of acoustic signal level in determining speech perception benefit. Audiology and Neurotology 19: 234–238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- English R., Plant K., Maciejczyk M., Cowan R. (2016) Fitting recommendations and clinical benefit associated with use of the NAL-NL2 hearing-aid prescription in Nucleus cochlear implant recipients. International Journal of Audiology 55(Suppl. 2): S45–S50. [DOI] [PubMed] [Google Scholar]
- Farinetti A., Roman S., Mancini J., Baumstarck-Barrau K., Meller R., Lavieille J. P., Triglia J. M. (2015) Quality of life in bimodal hearing users (unilateral cochlear implants and contralateral hearing aids). European Archives of Otorhinolaryngology 272: 3209–3215. [DOI] [PubMed] [Google Scholar]
- Fielden C. A., Kitterick P. T. (2016) Contralateral acoustic hearing aid use in adult unilateral cochlear implant recipients: Current provision, practice, and clinical experience in the UK. Cochlear Implants International 17(3): 132–145. [DOI] [PubMed] [Google Scholar]
- Fitzpatrick E. M., Leblanc S. (2010) Exploring the factors influencing discontinued hearing aid use in patients with unilateral cochlear implants. Trends in Amplification 14: 199–210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fitzpatrick E. M., Séguin C., Schramm D., Chenier J., Armstrong S. (2009) Users’ experience of a cochlear implant combined with a hearing aid. International Journal of Audiology 48: 172–182. [DOI] [PubMed] [Google Scholar]
- Flynn M. C., Schmidtke T. (2004) Benefits of bimodal stimulation for adults with a cochlear implant. International congress series, Elsevier 1273: 227–230. [Google Scholar]
- Fowler J. R., Eggleston J. L., Reavis K. M., McMillan G. P., Reiss L. A. (2016) Effects of removing low-frequency electric information on speech perception with bimodal hearing. Journal of Speech, Language, and Hearing Research 59(1): 99–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gifford R. H., Revit L. J. (2010) Speech perception for adult cochlear implant recipients in a realistic background noise: Effectiveness of preprocessing strategies and external options for improving speech recognition in noise. Journal of the American Academy of Audiology 21(7): 441–451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keilmann A. M., Bohnert A. M., Gosepath J., Mann W. J. (2009) Cochlear implant and hearing aid: A new approach to optimizing the fitting in this bimodal situation. European Archives of Oto-Rhino-Laryngology 266: 1879–1884. [DOI] [PubMed] [Google Scholar]
- Kong Y. Y., Stickney G. S., Zeng F. G. (2005) Speech and melody recognition in binaurally combined acoustic and electric hearing. The Journal of the Acoustical Society of America 117(3): 1351–1361. [DOI] [PubMed] [Google Scholar]
- Morera C., Cavalle L., Manrique M., Huarte A., Angel R., Osorio A., Morera-Ballester C. (2012) Contralateral hearing aid use in cochlear implanted patients: Multicenter study of bimodal benefit. Acta Oto-Laryngologica 132(10): 1084–1094. [DOI] [PubMed] [Google Scholar]
- Neuman A. C., Svirsky M. A. (2014) Performance of listeners using a cochlear implant and contralateral hearing aid (bimodal hearing). Ear and Hearing 34: 553–561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neuman A. C., Wroblewski M., Hajicek J., Rubinstein A. (2012) Measuring speech recognition in children with cochlear implants in a virtual classroom. Journal of Speech, Language, and Hearing Research 55(2): 532–540. [DOI] [PubMed] [Google Scholar]
- Offeciers E., Morera C., Müller J., Huarte A., Shallop J., Cavallé L. (2005) International consensus on bilateral cochlear implants and bimodal stimulation. Acta Oto-Laryngologica 125: 918–919. [DOI] [PubMed] [Google Scholar]
- Peterson G. E., Lehiste I. (1962) Revised CNC lists for auditory tests. The Journal of Speech and Hearing Disorders 27: 62–70. [DOI] [PubMed] [Google Scholar]
- Plant K., van Hoesel R., McDermott H., Dawson P., Cowan R. (2016) Influence of contralateral acoustic hearing on adult bimodal outcomes after cochlear implantation. International Journal of Audiology 55: 472–482. [DOI] [PubMed] [Google Scholar]
- Potts L. G., Skinner M. W., Litovsky R. A., Strube M. J., Kuk F. (2009) Recognition and localization of speech by adult cochlear implant recipients wearing a digital hearing aid in the nonimplanted ear (bimodal hearing). Journal of the American Academy of Audiology 20(6): 353–373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scherf F. W., Arnold L. P. (2014) Exploring the clinical approach to the bimodal fitting of hearing aids and cochlear implants: Results of an international survey. Acta Oto-Laryngologica 134: 1151–1157. [DOI] [PubMed] [Google Scholar]
- Siburt H. W., Holmes A. E. (2015) Bimodal programming: A survey of current clinical practice. American Journal of Audiology 24(2): 243–249. [DOI] [PubMed] [Google Scholar]
- Spahr A. J., Dorman M. F., Litvak L. M., Van Wie S., Gifford R. H., Loizou P. C., Cook S. (2012) Development and validation of the AzBio sentence lists. Ear and Hearing 33: 112–117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stender T. (2016) What about the contralateral ear? Bimodal programming considerations. Hearing Review 23(4): 32, Retrieved from http://www.hearingreview.com/news/tech-topic-news/. [Google Scholar]
- Sucher C. M., Mcdermott H. J. (2009) Bimodal stimulation: Benefits for music perception and sound quality. Cochlear Implants International 10(S1): 96–99. [DOI] [PubMed] [Google Scholar]
- Veugen L. C., Chalupper J., Snik A. F., van Opstal A. J., Mens L. H. (2016) Matching automatic gain control across devices in bimodal cochlear implant users. Ear and Hearing 37: 260–270. [DOI] [PubMed] [Google Scholar]
- Yamaguchi C. T., Goffi-Gomez M. V. S. (2013) Prevalence of contralateral hearing aid use in adults with cochlear implants. International Archives of Otorhinolaryngology 17(04): 370–374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang T., Dorman M. F., Gifford R., Moore B. C. (2014) Cochlear dead regions constrain the benefit of combining acoustic stimulation with electric stimulation. Ear and Hearing 35: 410–417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang T., Dorman M. F., Spahr A. J. (2010) Information from the voice fundamental frequency (F0) region accounts for the majority of the benefit when acoustic stimulation is added to electric stimulation. Ear and Hearing 31: 63–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.