ABSTRACT
Walking programs improve health outcomes in adults at risk for cardiovascular disease (CVD), and self-monitoring strategies can improve adherence to such programs. The objective of this study was to determine whether a 6-month Internet-based walking program using Web-enhanced pedometers results in more weight loss than walking programs based on time or simple pedometer step count goals in adults with or at risk for CVD. This was a multisite, randomized controlled trial of 255 male veterans who were ambulatory, insufficiently active, and with body mass index (BMI) ≥28, and who reported CVD risk factors ≥1 risk factors. Participants were randomized to one of three self-monitoring strategies to increase walking: 1) time-based walking goals; 2) simple pedometer-based walking goals; and 3) Web-enhanced pedometer feedback goals with Internet-mediated feedback. All participants also attended five individual weight loss sessions with a dietitian. The main outcome measure was change in weight at 6 months (kg), and the secondary outcomes were change in accelerometer-measured physical activity (min) and change in health-related quality of life at 6 months. The 255 participants had a mean age of 56.3 yr (SD = 10.0), BMI = 36.3 (SD = 5.3), with a mean value of 5.2 (SD = 2.3) medical comorbidities. Dropouts were distributed evenly across the three groups, and 72% of participants completed the program. At 6 months, participants in the Web-enhanced pedometer arm lost significantly more weight (−1.9 kg, 95% CI, −2.7 to −1.1) than those in the time-based group (−0.7 kg, 95% CI, −1.5 to 0.0; P = 0.04) and simple pedometer group (−0.6 kg, 95% CI, −1.4 to 0.2; P = 0.02). In conclusion, Internet-enhanced pedometers result in greater weight loss in veterans than in walking programs using time-based walking goals or simple pedometers.
INTRODUCTION
Walking is a convenient, inexpensive, and safe form of unsupervised physical activity that is recommended for persons with cardiovascular disease (CVD) risk factors (12) and that improves fitness, decreases weight, enhances quality of life, and reduces mortality (29,43,46). Despite the known benefits of walking, many high-risk individuals remain sedentary. Behavioral strategies to enhance physical activity self-monitoring such as logging walking activity and using pedometers to track step counts have been shown to improve health-related outcomes (7,30,35,44).
Self-regulation theory (5,8) suggests that an important reason that motivated individuals fail to adopt healthy behaviors is an inability to accurately self-monitor their behavior. Many people are unable to accurately recall the duration and intensity of walking they have accumulated throughout a given day (14,26). Increased self-awareness of a particular behavior enables people to set more effective short-term, incremental behavioral goals and to reward success (6,9,20,45). Pedometer-based walking programs improve self-monitoring, and when integrated with automated Web-based support, these can provide more detailed feedback and may allow participants to continue to make progress after the intensive phase of a weight loss intervention.
Most pedometer-based studies have used simple devices that only keep a running total of step counts, which therefore require participants to manually log their step counts to track their progress over time. In comparison, Internet-enhanced pedometers offer the advantages of storing time-stamped step count data and uploading to a computer, which reduces participant burden and errors associated with manual logging. Furthermore, enhanced pedometers enable participants to receive more detailed self-monitoring feedback, including information about walking bout duration and intensity that may improve goal attainment compared with goals simply based on time or step counts (39). Enhanced pedometer data and feedback can be integrated into Internet-based physical activity programs where computerized algorithms can provide personalized motivational messages, activity goals, feedback on progress, and access to an online community of walkers (28,34,44).
The Veterans Walk for Health (VWH) study was developed at the request of, and with input from, the Research Council of the Veterans Administration (VA)'s National Advisory Board for Nutrition and Food Services in an effort to address the health problem of obesity in VA patients. Specifically, veterans report disproportionately higher rates of hypertension, dyslipidemia, and diagnosed diabetes than nonveterans, a disparity driven by higher prevalence rates of obesity (17). Although dietary counseling is effective for mitigating some of these risks, combining dietary counseling with lifestyle physical activity is more effective for reducing both CVD risk factors and encouraging modest weight loss than either change in diet or activity by themselves. This study was designed to identify the optimal mode of walking prescription for this at-risk population that could be incorporated into an existing VA dietetics service to enhance weight loss outcomes and improve patient quality of life.
The VWH study is a randomized clinical trial that compared the effects of adding one of three different home-based walking programs to standard medical nutritional counseling offered to male veterans at risk for CVD on weight loss outcomes. The primary objective of this study was to compare the feasibility and preliminary efficacy of a commercially available, Internet-based pedometer walking program with walking programs based on simple time or step count goals in improving weight loss outcomes over a 6-month period. Secondary outcomes evaluated impact of the three strategies on changes in accelerometer-measured physical activity (min) and health-related quality of life (HRQoL). In addition, a process evaluation was conducted to understand contextual site-level factors influencing intervention effectiveness.
METHODS
Design
The VWH study was a multisite randomized controlled trial in which veterans at high risk for CVD received five sessions of dietitian-delivered, one-on-one nutritional counseling for weight loss over 6 months. Participants were randomized to receive one of three walking programs concurrent with and integrated into the counseling sessions.
Arm 1: Time-based walking goals with manual logging of time spent walking (usual care control)
Arm 2: A simple pedometer with manual step count logging and step count walking goals
Arm 3: An uploading pedometer with Internet-mediated step count feedback and goals
We hypothesized that nutritional counseling for weight loss would result in greater improvement in weight loss when augmented with an Internet-mediated pedometer-based walking program than when augmented with walking programs using time-based walking goals or using simple pedometers, manual logging, and step count goals. Secondarily, we hypothesized that daily physical activity levels would increase more for participants with Web-enhanced goals over simple pedometers or time-based goals, and that improved weight and moderate to vigorous physical activity (MVPA) outcomes would be associated with improved physical and mental HRQoL.
Participants
Initially, the trial included six VA sites charged with recruiting 50 participants each, but early in the recruitment phase, one of the sites dropped out (see Appendix, Supplemental Content, Veterans Walk for Health sites, http://links.lww.com/TJACSM/A10). Patients receiving care at one of five participating VA Medical Centers (VAMC) were recruited over 18 months with study advertisements (self-referral) and through VA provider referrals for nutritional counseling. An initial screening visit was scheduled by a study research assistant to discuss eligibility and study enrollment criteria. Eligible individuals were adult male veterans who received medical care from a VA physician at one of the participating VAMCs and who had a body mass index (BMI) of 28 or greater and at least one of the following conditions: diabetes, CAD, hypercholesterolemia, hypertension, or obesity (BMI >30). Eligibility criteria required that participants be able to comfortably walk one block, have interest in starting a walking program, and be insufficiently active at enrollment based on self-report in an adapted Godin Leisure-Time Exercise Questionnaire (18), which ascertained whether a patient performed less than 30 min of moderate-intensity physical activity for ≥5 d·wk−1. Participants also had to obtain written medical clearance from a VA physician and be fluent in English. All interested and eligible participants signed written informed consent documents before study enrollment. After completing the consent process, patients signed a form to obtain medical clearance from their VA primary care physician, completed a baseline survey, and were provided an Actical® accelerometer (Mini Mitter Co., Bend, OR) with instructions to wear the device daily upon waking until bedtime for at least 7 d. At a follow-up visit 1 to 2 wk after enrollment, the research assistant met with the participant and uploaded the Actical® accelerometer data to verify proper recording of data and confirmed medical clearance to start a walking program. Upon completion of these steps, the participant was randomized to a study arm and taken to a dietitian for his/her first of five counseling sessions. Enrolled participants received a remuneration of $10 phone or gas cards for every visit attended and a study T-shirt upon completion of the study.
Safety and Human Subject Protection
In light of the potential risk for a serious adverse event (AE) related to CVD risk factors, extensive safety protocols were implemented to minimize the risk for adverse medical events occurring in response to the walking program. In summary, participants were asked at every visit about AE. Individuals who experienced serious AE were temporarily suspended and referred to their VA doctor. They were allowed to return to the intervention after obtaining written medical reclearance. A detailed description of the safety protocols used and the AE encountered in VWH have been previously published (19). The protocol was approved by the investigational review boards at each of the six participating VAMC. The study protocol is registered at www.ClinicalTrials.gov.
Intervention
Nutritional Counseling
Upon completing the baseline orientation session, all study participants were randomized to receive five sessions of one-on-one, face-to-face nutritional counseling for weight loss delivered by VA usual care dietitians who received additional training to deliver the study interventions. The standardized nutritional counseling was based on a modified version of the medical nutrition therapy (MNT) protocol for weight management published by the American Dietetic Association (1,2). All study arm participants were encouraged to walk at a pace that felt comfortable to them and to report any negative symptoms experienced while walking. Walking goals were set to help participants safely achieve gradual and incremental increases in daily walking over 6 months.
Arm 1—Time-Based Walking Goals
Participants in this active control arm were encouraged to set time-based walking goals. Dietitians used the final 10–15 min of each MNT session to review participant walking logs and to set new walking goals. Participants were encouraged to increase their daily walking goal by 5–10 min after each session.
Arm 2—Simple Pedometer-Based Program with Manual Step Count Logging
Participants in the simple pedometer arm were given a Digiwalker SW 200, a low-cost but accurate device that has been used extensively as a method of measuring physical activity as well as a motivational tool in physical activity interventions (3,4,24,36). Participants were instructed to wear the pedometer all day, every day, throughout the 6-month intervention period and to manually log step counts at the end of each day on a log sheet. Participants reviewed their step count logs with the dietitians, and this information was used to collaboratively set a new step count goal. Participants were encouraged to increase their daily walking target by 10% to 25% after each session.
Arm 3—Internet-Enhanced Pedometer Arm with Automated Step Count Logging and Feedback
Participants in the enhanced pedometer arm were given a SportBrain iStep X, an enhanced pedometer that can store minute-by-minute step count data for about 2 wk. The SportBrain iStepX has been found to be accurate within 3% of step counts recorded on a Digiwalker SW 200 (38). Participants could upload step count data via a USB connection to their home computer and then to the SportBrain.com website online where they could view their progress based on the data they uploaded from home or at a publically available computer at a VA library, along with motivational messages and feedback on the SportBrain.com website (Fig. 1). In addition, participants could set individualized step count goals on the website. These goals were incorporated into graphs and feedback on the individual's personalized feedback Web page. Participants were encouraged to engage in an online community where they could read and post messages about their walking program. At each follow-up visit, the dietitian uploaded the SportBrain data recorded during the week before each session and then reviewed the enhanced pedometer feedback provided by the website to help set new walking goals with the participant. Participants in this arm were encouraged to increase their daily walking target by 10% to 25% after each of the MNT sessions. Finally, home computer ownership was not a requirement for VWH. Study staff worked with participants to identify points of computer access (e.g., at work, child's home, public library) or to make a computer accessible at the VA Patient Library at all sites.
Figure 1.
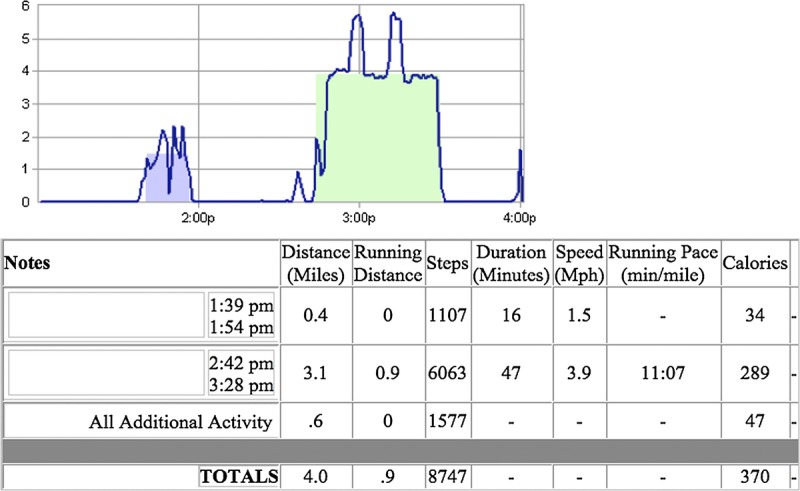
Sample graph and feedback table from the Sportbrain.com website—Sportivity Speed Zoom (mph) (view the whole day).
Nutritional counselors were all registered dietitians. Counselors attended a 2-d training session at the coordinating site before participant recruitment. They received instruction in the study protocol including the nutritional counseling curriculum and coaching strategies related to the various walking goal conditions. During the course of the intervention, dietitians participated in monthly calls with the coordinating center to review the curriculum, discuss difficult cases, and report AE. All study dietitians were required to audio record at least two counseling sessions as a quality assurance step to maintain fidelity to the study protocol. Recordings were reviewed by a study coinvestigator (SF) who provided feedback to dietitians through individual phone supervision or general feedback that was part of the monthly calls with all interventionists.
Nutritional counselors were provided with their own Internet-enhanced pedometer and uploaded their own step counts to become experienced users so that they could assist participants who were experiencing technical problems. In addition, they received basic training in technical issues related to the device and were given resources such as instruction sheets with screen shots to walk through with participants who were experiencing technical problems.
Randomization
Upon receipt of the written medical clearance and completion of the baseline data collection, participants were randomized with block randomization by season and with equal probability to one of three study arms. Baseline data collection occurred before randomization, but patients, dietitians, and study coordinators were not blinded with respect to study arm assignment during the intervention or final assessment.
Assessment of Outcomes
Anthropometry
Height was measured at baseline using a wall-mounted stadiometer and recorded to the nearest 0.1 cm. Participant weight was assessed at baseline and the five MNT sessions. On each occasion, participants were weighed twice to the nearest 0.1 kg on the same study scale with minimal clothing. BMI was calculated for each assessment using the standard formula (kg·m−2).
Objective Physical Activity
Objective assessment of physical activity was conducted at baseline and before MNT sessions at months 3 and 6 using Actical® accelerometers (Mini Mitter Co.), which are small devices that resemble pagers that can be worn on the hip, wrist, or ankle depending on the user's adiposity level. Accelerometers were mailed to participants 10 d before their 3- and 6-month MNT sessions with instructions to wear the unit daily during waking hours for 7 d leading up to their MNT session, at which time, they turned it in to a dietitian. The Actical® is an omnidirectional accelerometer that measures and records movement in detailed frequency counts over time that can be converted into accurate estimations of time engaged in light to moderate physical activity, activity intensity, and energy expenditure (16,21). Objective MVPA was defined as the average number of minutes per day of physical activity recorded by the Actical® of at least moderate intensity. MVPA was operationalized as exceeding a cut point of 2000 frequency counts per minute. Participants were also required to have 600 min of daily wear time, and if they had 60 straight minutes of no counts, the accelerometer was considered not worn. If the data uploaded at a visit contained less than five valid days of data, then these were considered missing.
Baseline and 6-Month Follow-up Surveys
At baseline and 6-month follow-up, participants were also asked to complete measures of potential mediating variables, including HRQoL with the 12-Item Short-Form Health Survey (SF-12 [41]), a 5-item computer background questionnaire, a single-item global health assessment (23), a modified 18-Item Charlson Comorbidity Index, and five questions pertaining to CVD history, risk factors, and medication. Program satisfaction was evaluated at 6 months using the VA's 14-Item Survey of Healthcare Experiences of Patients' Ambulatory Care, and with an additional 12 questions eliciting satisfaction with their walking, nutritional counseling, and Web interface (enhanced pedometer arm only). Intervention adherence was assessed by documenting participant attendance at scheduled study sessions and comparing attainment of physical activity goals in self-report measures with objectively monitored accelerometer assessments at 3 and 6 months. Participants also completed some validated measures at baseline and at 3 and 6 months of self-efficacy for physical activity and physical activity stage of change (25) that were used by dietitians for counseling but which are not reported here.
Sample Size Calculation
The sample size was calculated so it would provide 80% power to detect a 1.4-kg difference in weight loss between pairs of active intervention conditions (e.g., time-based vs simple pedometer) in the planned comparisons with alpha set at 0.05 for a two-tailed test. It is important to note that 1.4 kg represents the difference in weight change between the groups—not the absolute weight change. Based on prior observations, the SD of weight change over a 6-month period was estimated as 3 kg. Power analysis was conducted using Cohen's methods (11) and calculated with PASS2000 software that indicated the need for 82 subjects per group after accounting for attrition. In anticipation of up to 20% attrition, we planned to recruit 103 patients per arm or a total of 300 participants (50 patients per site).
Statistical Analysis
Descriptive statistics stratified by the study arm were used for demographic variables, weight, and accelerometer MVPA. Means and SD were reported for age, number of comorbidities, weight, accelerometer MVPA, days uploaded or logged, and number of visits. Frequencies of race, smoking status, general health status, diabetes, CAD, depression, education, BMI categories, and participant satisfaction were also reported.
Analyses of outcomes were conducted as intent to treat with participants analyzed based on their original program assignment. The analysis was conducted using linear mixed-effects models, which provided an unbiased estimate of adjusted mean outcomes, assuming data were missing at random. The basic model used weight change at visits 1 through 6 as dependent variables, while independent variables consisted of baseline weight, an indicator for program assignment, and an interaction term of time by program assignment. Each site and each participant's data were modeled using a random intercept to allow within-site and within-patient correlation of the repeated measures. We also conducted planned post hoc comparisons between arms. Analyses were conducted using Stata 13.1, and all reported P values and confidence intervals are from adjusted analyses.
Process Evaluation
Near study completion, study staff (LJD) conducted phone interviews of staff involved with the intervention at each site to assess barriers and facilitators encountered when implementing VWH at that site. Interviews were conducted before outcomes data were available to participating sites, and the qualitative researchers were blinded to outcomes during qualitative data collection and analysis. A standardized interview guide was used to conduct interviews based on the Consolidated Framework for Implementation Research (CFIR [13]). This guide assessed factors related to organizational context, attributes of the study intervention, and the process of implementing the interventions. The site investigator, research coordinator, and one randomly selected dietitian out of a pool of two to four dietitians with a high volume of VWH visits at each site were invited to participate. Interviews were transcribed verbatim and qualitatively analyzed (LJD, JCL) using a rigorous analysis approach (15,27). Each analyst independently read each interview and then together summarized each site by inductively identifying themes that emerged from the data. Themes were compared across sites using a cross-case constant comparative method (32) and then mapped to CFIR constructs to construct a matrix with sites in columns and the barriers and facilitators most likely to have influenced implementation of VWH in rows. At this point, the qualitative analysts were shown summative outcomes by site. One site had less than average weight loss and two sites had higher than average weight loss. Barriers and facilitators were compared and contrasted for the low versus high outcome sites.
RESULTS
Participants
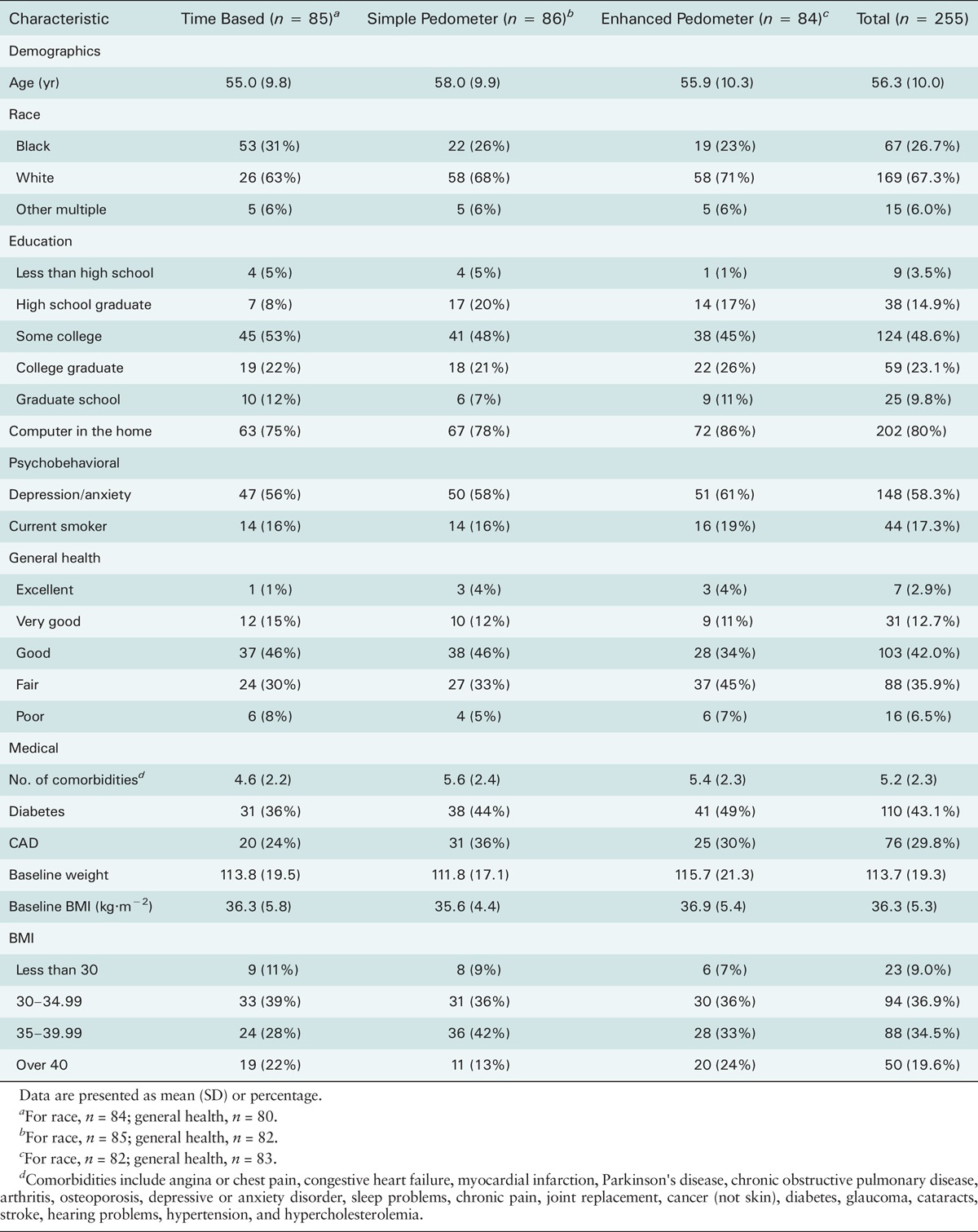
Of 416 veterans screened for participation, 275 (66%) were enrolled in the study (Fig. 2). However, 20 participants dropped out before randomization (61%). Thus, 255 participants were successfully randomized to each study arm: time based (n = 85), simple pedometer (n = 86), and enhanced pedometer (n = 84). At baseline, the sample reported an average of 5.2 comorbid health conditions (SD = 2.3) and an average BMI of 36.3 (SD = 5.3). The time-based arm reported fewer comorbid health conditions (4.6, SD = 2.2, P = 0.01) at baseline than the simple pedometer (5.6 conditions, SD = 2.4) and enhanced pedometer arms (5.4 conditions, SD = 2.3). Between 75% and 86% of participants reported owning a home computer. No other significant differences were found between arms at baseline (Table 1). Among this study cohort, 43% had diabetes, 30% had CAD, and 58% had a diagnosis of depression or anxiety. Dropouts were approximately equal across all three arms, with a mean dropout of 28% during the 6-month intervention. The average number of visits per participant did not differ by arm for the time-based arm (5.3 visits, SD = 1.2), simple pedometer arm (5.2 visits, SD = 1.3), and enhanced pedometer arm (5.3 visits, SD = 1.3) participants.
Figure 2.
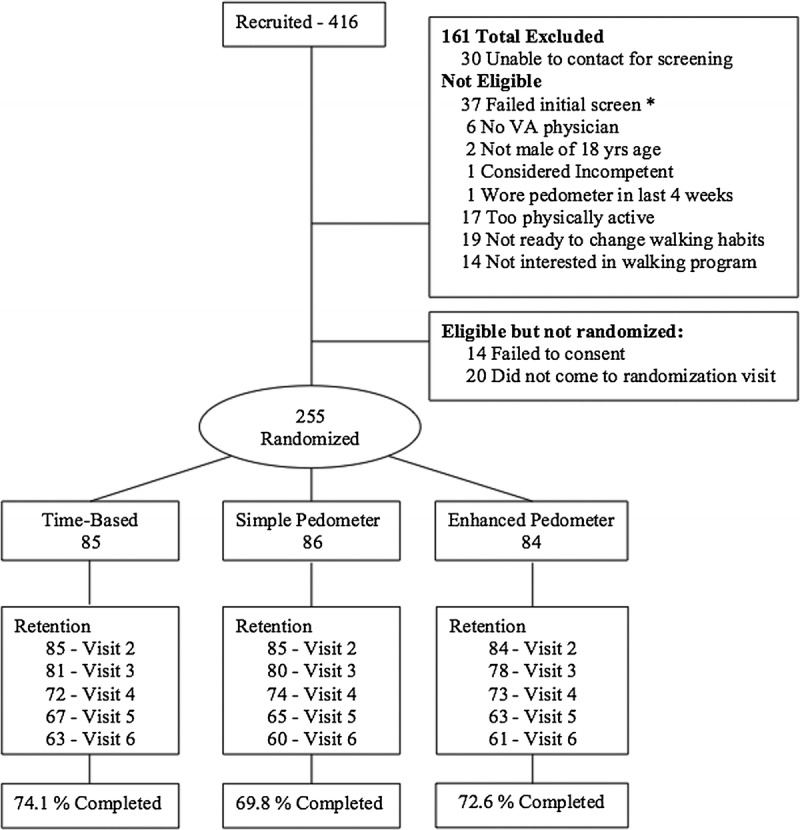
Flow diagram.
TABLE 1.
Baseline Characteristics of Participants by Randomization Group.
Weight Loss
Participants in the enhanced pedometer arm lost significantly more weight at 6 months than those in the time-based walking group (enhanced = −1.9 kg, 95% CI, −2.7 to −1.1, vs time = −0.7 kg, 95% CI, −1.5 to 0.0; P < 0.04) and the simple pedometer group (simple = −0.6 kg, 95% CI, −1.4 to 0.2; P < 0.02). The difference in weight loss between the time-based walking group and the simple pedometer arm was not significant (P = 0.76) (Table 2 and Fig. 3).
TABLE 2.
Baseline Means and Predicted Mean Change in Study Outcomes at 6 Months.
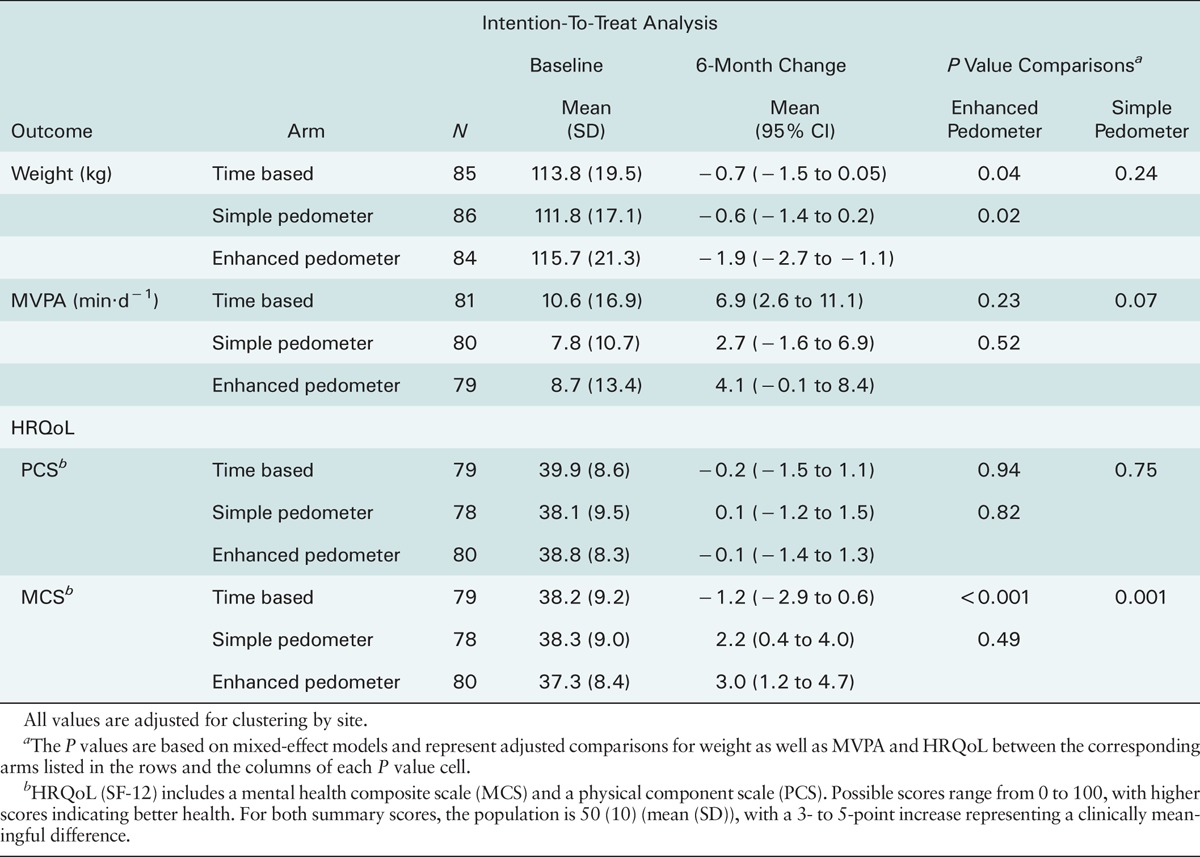
Figure 3.
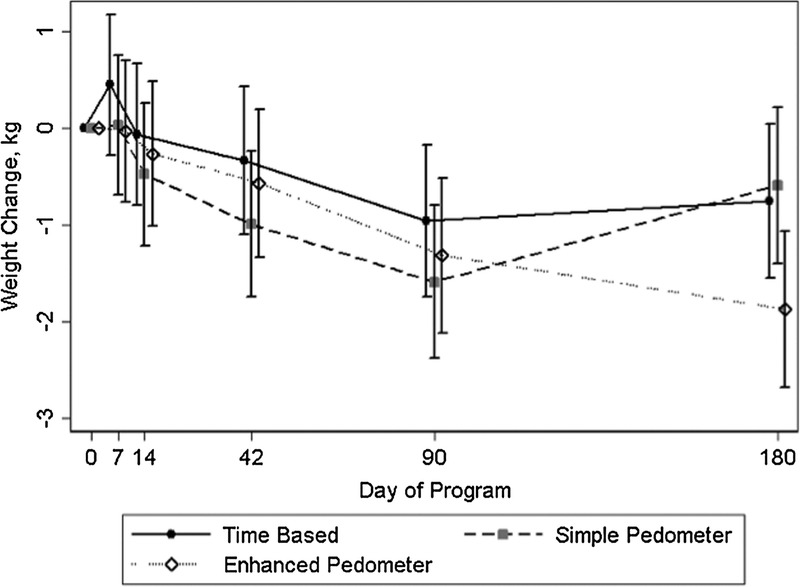
Predicted weight change over 6 months across study arms.
Physical Activity Levels
The time-based arm was the only arm to see a modest but statistically significant increase in average daily minutes of MVPA (P < 0.01). Participants in the enhanced pedometer arm had no difference in MVPA at 6 months compared with those in the time-based walking group (P = 0.23) and the simple pedometer group (P = 0.52). Participants in the time-based pedometer arm had higher levels of MVPA than those in the simple pedometer walking group, but these differences were nonsignificant (P = 0.07) (Table 2).
HRQoL
Individuals in the enhanced pedometer arm increased their score (3.0) on the SF-12 mental health composite scale (MCS) significantly more than those in the time-based arm (−1.2; P < 0.001). The increase in MCS for the enhanced pedometer arm is within the 3- to 5-point increase associated with clinically meaningful change (42). Individuals in the simple pedometer arm also increased their score (2.1; P = 0.001) compared with those in the time-based arm. There were no statistically significant differences between enhanced pedometer and simple pedometer on the SF-12 MCS. There were no differences in change in the physical composite subscore of the SF-12.
Physical Activity Tracking
Over a 6-month period, participants in the enhanced pedometer arm uploaded pedometer step count data on fewer days (67 d (SD = 54)) than minutes or step counts that were manually logged in the time-based (92 d (SD = 64)) and simple pedometer arms (97 d (SD = 64)) (P = 0.01). The majority of participants in the two pedometer arms were comfortable or very comfortable wearing their pedometers (simple pedometer, 95%; enhanced pedometer, 98%), although all participants in the two pedometer arms reported forgetting to wear the pedometer at least sometimes during the intervention period. In the enhanced pedometer arm, 48% of completers reported that viewing graphs of step count data on the website helped a lot with respect to increasing their walking.
Site Differences
There was substantial variation in dropout rates, participant satisfaction, and mean outcomes for weight loss and physical activity across the sites. Based on mean weight loss at 6 months, sites were classified into low performance (n = 1), moderate (n = 3), or high performance (n = 2). Two sites had markedly higher average weight loss with a 10% dropout rate in contrast to one site with markedly less weight loss where over half of participants dropped out (52%). Furthermore, difference in weight loss between arms was more extreme in the sites with highest weight loss. In addition, participant satisfaction with counseling was higher in the two highest weight loss sites; 78% of participants reported that nutritional counseling helped compared with 65% in the site with the lowest average weight loss.
To understand variation in implementation that may help to explain differences in outcomes across sites, 17 interviews were conducted with staff at the study sites. Interviews lasted from 30 to 60 min.
Site with the Lowest Weight Loss
Although participants gave relatively high scores for nutritional counseling, staff described participants as being unmotivated to do what was needed to lose weight and often expressed disappointment with VWH because it required so many visits over a relatively long period (6 months). This site was unique in mentioning participants' challenges with distance, the high cost of gas, very low incomes, and having to juggle multiple jobs. All of these factors may have contributed to their higher dropout from the study. Although a few participants seemed enthusiastic about the enhanced pedometers and potential successful weight loss, staff struggled with getting the software to work for participants at home. As a workaround, they tried but failed to arrange for participants to use a clinic computer to upload their pedometer and access the Internet to see feedback reports in between visits. The site appeared to be beleaguered with “stressed and overworked” primary care providers, most of whom perceived VWH as another program that “will just come and go.” This site also experienced high turnover in dietitians, with the remaining dietitians having to cover for frequent absences.
Sites with the Highest Weight Loss
Dietitians at both sites were integrated into primary care teams. Interviewees talked about supportive primary care providers who already recognized the importance of counseling their patients to lose weight and who willingly referred patients to VWH. Both sites had multiple active referral processes for VWH. Staff at both sites told positive stories about patients who, for example, “had pretty dramatic weight losses … even for the ones that didn't lose very much weight, some of them looked better … like maybe they'd lost flab and gotten more muscle ….” They described many of their participants with the enhanced pedometers as not being “tech savvy” and who also had trouble using their enhanced pedometers. Staff at both sites were successful in setting up a computer workstation, and many of their participants with the enhanced pedometers came in weekly to upload their data and see feedback reports.
AE
There were no significant differences in the occurrence of study-related AE across the three study arms. Only two serious study-related AEs occurred in this high-risk sample. One participant was temporarily suspended with a cardiac arrhythmia. A second participant experienced worsening musculoskeletal pain. Nonserious, study-related AE comprised 9.8% of the 194 symptoms reported by participants over the course of the study—primarily minor musculoskeletal injuries. The descriptive nature of the AE encountered in VWH has been described in greater detail previously (19).
DISCUSSION
In a brief medical weight loss intervention for high CVD risk veterans, using an Internet-enhanced pedometer to track daily step counts resulted in more weight loss compared with using a simple pedometer to manually track step counts or compared with manually tracking time spent in physical activity each day. Results also showed improvements in mental HRQoL that approached clinically meaningful change for both enhanced and simple pedometer arms compared with the time-based arm in a sample with high mental health morbidity. There were no differences in dropout rates across the three arms despite the differences in technical complexity of the programs. This pragmatic trial further demonstrated that Internet-enhanced pedometers can be implemented as a component of an existing clinical nutritional counseling program at geographically dispersed sites with relatively modest training of staff and limited technical infrastructure. These results support the use of Internet-enhanced pedometers to augment existing brief dietary counseling interventions for weight loss and CVD risk reduction.
This trial is unique because it was designed to answer a fundamental question of how different modes of self-monitoring ambulatory activity in a high-risk population enhance clinical outcomes. Although other trials have used simple pedometers (22) or more complex wearable devices to monitor physical activity (37,40), this is a comparativeness research trial with direct comparison of the three modes of walking prescription commonly used in community settings. Notably, this trial was integrated into a standard low-intensity behavioral weight loss program that was designed to be for high CVD risk populations where it was critical for augmented exercise counseling to be simple and efficient. Furthermore, the enhanced pedometer participants benefitted from combining face-to-face counseling with a dietitian with the feedback from their wearable devices that connected to an Internet-based website. Finally, this enhanced pedometer walking strategy also demonstrated real-world feasibility based on the acceptance of patients characterized by low socioeconomic status and by older age and high health morbidity.
The positive results for enhanced pedometers may be the result of theoretical and practical advantages that Internet-enhanced pedometers have over simple pedometer and time-based walking programs. First, compared with simple pedometers that only record total steps accumulated per day, enhanced pedometers collect more detailed information about individual bouts of walking, including start time, stop time, walking speed, and total steps accumulated. The theory of self-regulation suggests that more accurate and detailed self-monitoring may improve behavior change outcomes particularly related to weight loss (5,8). Second, the capability of enhanced pedometers to store and upload objectively recorded data minimizes problems with physical activity self-report including participant logging burden, recall biases, and nonadherence. Logging was found to be a critical component of effective pedometer-based walking programs (7). Third, the enhanced pedometer intervention in this trial can be easily disseminated on a regional or national scale through existing clinical programs because the technical infrastructure does not need to be replicated at each site.
The average weight loss was less than we had hoped even in the most effective arm of the trial. The high average level of medical and psychiatric comorbidity in the target population may help explain why the average overall weight loss in the trial was lower than might have been expected in a program that combined a pedometer-based walking program with dietary counseling. The relatively small improvements seen in average daily minutes of MVPA suggest the necessity to better address barriers to increasing physical activity in older veterans. Changes in MVPA did not explain improvements in weight loss that were consistent with our original hypotheses. We speculate that monitoring physical activity may have had an attentional spillover effect on participants' attention to their dietary behaviors, resulting in better outcomes in proportion to the sophistication of the monitoring tool. A more intensive intervention may have been necessary to achieve clinically significant levels of weight loss. In addition, between-site variations found in the process evaluation suggest that expectations of staff about intervention effectiveness and underlying staffing issues may have reduced the impact at lower performing sites. Nonetheless, these findings underscore the importance of assessing the influence of such contextual, site-level factors that may influence the effectiveness of an intervention in real-world conditions.
We also note that this trial also has a number of unique strengths. First, this was a randomized controlled pragmatic trial that was designed to have a high degree of external validity. The majority of participants in this trial had multiple complex medical conditions and as such would be excluded from most community-based weight loss and physical activity trials. In addition, the decision to evaluate the program at multiple sites was primarily designed to demonstrate ease of dissemination and to allow us to compare implementation experiences across sites in a formative evaluation. By incorporating the program into an existing clinical program rather than delivering it as a stand-alone research intervention, we reinforced the practical and sustainable nature of the intervention. The documentation of AE also underscores that walking programs can be safely implemented with high-risk patient populations (19) to improve not only physical outcomes but also psychological outcomes as documented by the increase in mental composite subscore of the SF-12. Finally, the objective assessment of both weight loss and physical activity using accelerometers in all three arms further supports the validity of the results.
This study is not without limitations. To the extent that a walking program increases cardiorespiratory fitness and lean muscle mass, the average weight loss reported here may underestimate the impact of the intervention on health-related outcomes such as blood pressure, insulin resistance, adiposity, and cardiometabolic risk. However, cardiorespiratory fitness and lean muscle mass were not measured in this study. In recent studies driven by diet change, weight loss and objective MVPA monitoring do not always capture other meaningful health improvements (10,33). The loss of one study site reduced our statistical power by some 50 subjects, but the objective tools to measure outcomes still demonstrated clear differences between arms. Although the design of VWH relied on an early generation of Web-enhanced pedometers that are quite expensive and less user-friendly than current generations, results still provide support for the current generation of remote sensing devices that are significantly cheaper and that provide greater feedback to users. In addition, participants and dietitians were not blinded to their study arm, which may have biased results. We also note at the time of recruitment that the percentage of women veterans using Veterans Health Administration (VHA) facilities was low (approximately 3%). However, women veterans now represent the fastest growing demographics within VHA and the military and should be included in future lifestyle intervention trials. Finally, results from this small study may not generalize beyond the older male sample of veterans recruited from five locations in the nationally integrated VA healthcare system, and further research is recommended with women veterans and nonveteran populations.
CONCLUSION
Results from the VWH trial show that adding an Internet-enhanced pedometer walking program to standard medical nutrition therapy in high CVD risk patients results in greater weight loss than for participants using a simple pedometer or time-based walking program. Although the marginal weight loss was modest, Internet-enhanced pedometers are scalable and low cost, and they have the potential to play a role in optimizing nutritional weight loss programs. Some health experts have observed that individuals who have the most to gain from wearing a remote sensing physical activity device such as those who are older or of lower socioeconomic status (31) are less likely to use such devices because of barriers in cost, usability, and computer literacy. However, the current trial demonstrated the added clinical benefit of providing such technologies to a vulnerable population who exemplify these engagement barriers. Nonetheless, these devices are not a panacea for increasing physical activity without further basic research that develops effective engagement strategies that help high-risk health populations use these devices in a manner that promotes sustained use and integration of physical activity information in a meaningful way that helps the users prevent or manage health risk factors.
Acknowledgments
This study was funded by the Rehabilitation Research and Development Service, Department of Veterans Affairs grant number D3358R. Funding was also provided by Dr. Richardson's career development award from National Heart, Lung, and Blood Institute (K23 HL075098) and Physician Faculty Scholars Program award from the Robert Wood Johnson Foundation (57408). The funding agencies had no role in the study design, data collection, analyses, and interpretation of the findings or decision to submit this manuscript for publication.
This research is dedicated to Dr. David Ronis, an amazing statistician, teacher, and colleague, who passed away before he could see this article published. We acknowledge the invaluable contributions of the following principal investigators and research coordinators at Veterans Administration Medical Centers across the country who made this manuscript possible: Catherine Austin, Margaret Locke (Memphis, TN); Louise Grant (Miami, FL); Debra Colombe, Peggy Turner (Oklahoma City, OK); Kathryn Griver, Karla Martinez (San Diego, CA); Christine Kleckner, Jan Butin (Topeka, KS); and Kathleen Dial, Christine Wilson (Tucson, AZ).
Trial Registration: ClinicalTrials.gov, NCT00123435.
The authors have no conflicts to declare. Results of the present study do not constitute endorsement by the American College of Sports Medicine.
REFERENCES
- 1.American Dietetic Association. Medical Nutrition Therapy across the Continuum of Care: Supplement 1. Paperback Chicago: American Dietetic Association; 1997. unk p. [Google Scholar]
- 2.American Dietetic Association. Position of the American Dietetic Association: integration of medical nutrition therapy and pharmacotherapy. J Am Diet Assoc. 2003;103(10):1363–70. [DOI] [PubMed] [Google Scholar]
- 3.Bassett DR, Jr, Ainsworth BE, Leggett SR, et al. Accuracy of five electronic pedometers for measuring distance walked. Med Sci Sports Exerc. 1996;28(8):1071–7. [DOI] [PubMed] [Google Scholar]
- 4.Bassett DR, Jr, Ainsworth BE, Swartz AM, Strath SJ, O'Brien WL, King GA. Validity of four motion sensors in measuring moderate intensity physical activity. Med Sci Sports Exerc. 2000;32(Suppl 9):S471–80. [DOI] [PubMed] [Google Scholar]
- 5.Boekaerts M, Pintrich PR, Zeidner M. Handbook of Self-Regulation. 1st ed San Diego (CA): Academic Press; 2005. pp. 816. [Google Scholar]
- 6.Boutelle KN, Kirschenbaum DS, Baker RC, Mitchell ME. How can obese weight controllers minimize weight gain during the high risk holiday season? By self-monitoring very consistently. Health Psychol. 1999;18(4):364–8. [DOI] [PubMed] [Google Scholar]
- 7.Bravata DM, Smith-Spangler C, Sundaram V, et al. Using pedometers to increase physical activity and improve health: a systematic review. JAMA. 2007;298(19):2296–304. [DOI] [PubMed] [Google Scholar]
- 8.Cameron LD, Levanthal H. (Eds). The Self-Regulation of Health and Illness Behavior. London: Routledge; 2003. pp. 360. [Google Scholar]
- 9.Carels RA, Darby LA, Rydin S, Douglass OM, Cacciapaglia HM, O'Brien WH. The relationship between self-monitoring, outcome expectancies, difficulties with eating and exercise, and physical activity and weight loss treatment outcomes. Ann Behav Med. 2005;30(3):182–90. [DOI] [PubMed] [Google Scholar]
- 10.Carpenter KM, Lovejoy JC, Lange JM, Hapgood JE, Zbikowski SM. Outcomes and utilization of a low intensity workplace weight loss program. J Obes. 2014;2014:414987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd ed Hillsdale (NJ): Lawrence Erlbaum Associates; 1988. pp. 590. [Google Scholar]
- 12.Coke LA, Fletcher GF. Exercise and the cardiac patient-success is just steps away. J Cardiovasc Nurs. 2010;25(3):238–40. [DOI] [PubMed] [Google Scholar]
- 13.Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci. 2009;4:50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Duncan GE, Sydeman SJ, Perri MG, Limacher MC, Martin AD. Can sedentary adults accurately recall the intensity of their physical activity? Prev Med. 2001;33(1):18–26. [DOI] [PubMed] [Google Scholar]
- 15.Forman J, Damschroder LJ. Qualitative content analysis. In: Jacoby L, Siminoff L, editors. Empirical Research for Bioethics: A Primer. Oxford: Elsevier Publishing; 2008. p. 221. [Google Scholar]
- 16.Frey G, Padilla J, Johnston J, Webb J, Stager J. Impact of engineering design on the relationship between accelerometry activity counts and energy expenditure. Med Sci Sports Exerc. 2006;38(5):S561. [Google Scholar]
- 17.Fryar CD, Herrick K, Afful J, Ogden CL. Cardiovascular disease risk factors among male veterans, U.S., 2009–2012. Am J Prev Med. 2016;50(1):101–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Godin G, Shephard R. Godin Leisure-Time Exercise Questionnaire. Med Sci Sports Exerc. 1997;29(6):36–8. [Google Scholar]
- 19.Goodrich DE, Larkin AR, Lowery JC, Holleman RG, Richardson CR. Adverse events among high-risk participants in a home-based walking study: a descriptive study. Int J Behav Nutr Phys Act. 2007;4:20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hardeman W, Griffin S, Johnston M, Kinmonth AL, Wareham NJ. Interventions to prevent weight gain: a systematic review of psychological models and behaviour change methods. Int J Obes Relat Metab Disord. 2000;24(2):131–43. [DOI] [PubMed] [Google Scholar]
- 21.Heil DP. Predicting activity energy expenditure using the Actical activity monitor. Res Q Exerc Sport. 2006;77(1):64–80. [DOI] [PubMed] [Google Scholar]
- 22.Hultquist CN, Albright C, Thompson DL. Comparison of walking recommendations in previously inactive women. Med Sci Sports Exerc. 2005;37(4):676–83. [DOI] [PubMed] [Google Scholar]
- 23.Idler EL, Benyamini Y. Self-rated health and mortality: a review of twenty-seven community studies. J Health Soc Behav. 1997;38(1):21–37. [PubMed] [Google Scholar]
- 24.Leenders N, Sherman WM, Nagaraja HN. Comparisons of four methods of estimating physical activity in adult women. Med Sci Sports Exerc. 2000;32(7):1320–6. [DOI] [PubMed] [Google Scholar]
- 25.Marcus BH, Bock BC, Pinto BM, Forsyth LH, Roberts MB, Traficante RM. Efficacy of an individualized, motivationally-tailored physical activity intervention. Ann Behav Med. 1998;20(3):174–80. [DOI] [PubMed] [Google Scholar]
- 26.Mathews CE. Use of self-report instruments to assess physical activity. In: Welk GJ, editor. Physical Activity Assessments for Health-Related Research. Champaign: Human Kinetics Publishers, Inc.; 2002. pp. 108–13. [Google Scholar]
- 27.Miles MB, Huberman AM. Qualitative Data Analysis: An Expanded Sourcebook. 2nd ed Thousand Oaks (CA): Sage; 1994. pp. 352. [Google Scholar]
- 28.Moy ML, Janney AW, Nguyen HQ, et al. Use of pedometer and Internet-mediated walking program in patients with chronic obstructive pulmonary disease. J Rehabil Res Dev. 2010;47(5):485–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Murphy MH, Nevill AM, Murtagh EM, Holder RL. The effect of walking on fitness, fatness and resting blood pressure: a meta-analysis of randomised, controlled trials. Prev Med. 2007;44(5):377–85. [DOI] [PubMed] [Google Scholar]
- 30.Ogilvie D, Foster CE, Rothnie H, et al. Interventions to promote walking: systematic review. BMJ. 2007;334(7605):1204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Patel MS, Asch DA, Volpp KG. Wearable devices as facilitators, not drivers, of health behavior change. JAMA. 2015;313(5):459–60. [DOI] [PubMed] [Google Scholar]
- 32.Patton MQ. Qualitative Research and Evaluation Methods. 3rd ed Thousand Oaks (CA): Sage Publications; 2001. pp. 688. [Google Scholar]
- 33.Pierce JP, Natarajan L, Caan BJ, et al. Influence of a diet very high in vegetables, fruit, and fiber and low in fat on prognosis following treatment for breast cancer: the Women's Healthy Eating and Living (WHEL) randomized trial. JAMA. 2007;298(3):289–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Richardson CR, Buis LR, Janney AW, et al. An online community improves adherence in an internet-mediated walking program. Part 1: results of a randomized controlled trial. J Med Internet Res. 2010;12(4):e71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Richardson CR, Newton TL, Abraham JJ, Sen A, Jimbo M, Swartz AM. A meta-analysis of pedometer-based walking interventions and weight loss. Ann Fam Med. 2008;6(1):69–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Schneider PL, Crouter SE, Lukajic O, Bassett DR., Jr Accuracy and reliability of 10 pedometers for measuring steps over a 400-m walk. Med Sci Sports Exerc. 2003;35(10):1779–84. [DOI] [PubMed] [Google Scholar]
- 37.Shuger SL, Barry VW, Sui X, et al. Electronic feedback in a diet- and physical activity-based lifestyle intervention for weight loss: a randomized controlled trial. Int J Behav Nutr Phys Act. 2011;8:41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Swartz AM, Strath SJ, Miller NE, et al. Validity of physical activity monitors in assessing energy expenditure in normal, overweight, and obese adults. Open Sports Sci J. 2009;2:58–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tudor-Locke C, Lutes L. Why do pedometers work? A reflection upon the factors related to successfully increasing physical activity. Sports Med. 2009;39(12):981–93. [DOI] [PubMed] [Google Scholar]
- 40.Turner-McGrievy GM, Beets MW, Moore JB, Kaczynski AT, Barr-Anderson DJ, Tate DF. Comparison of traditional versus mobile app self-monitoring of physical activity and dietary intake among overweight adults participating in an mHealth weight loss program. J Am Med Inform Assoc. 2013;20(3):513–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ware J, Jr, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34(3):220–33. [DOI] [PubMed] [Google Scholar]
- 42.Warkentin LM, Majumdar SR, Johnson JA, et al. Weight loss required by the severely obese to achieve clinically important differences in health-related quality of life: two-year prospective cohort study. BMC Med. 2014;12:175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Williams PT. Reduced diabetic, hypertensive, and cholesterol medication use with walking. Med Sci Sports Exerc. 2008;40(3):433–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wing RR, Crane MM, Thomas JG, Kumar R, Weinberg B. Improving weight loss outcomes of community interventions by incorporating behavioral strategies. Am J Public Health. 2010;100(12):2513–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wing RR, Phelan S. Long-term weight loss maintenance. Am J Clin Nutr. 2005;82(Suppl 1):222S–5. [DOI] [PubMed] [Google Scholar]
- 46.Zheng H, Orsini N, Amin J, Wolk A, Nguyen VT, Ehrlich F. Quantifying the dose–response of walking in reducing coronary heart disease risk: meta-analysis. Eur J Epidemiol. 2009;24(4):181–92. [DOI] [PubMed] [Google Scholar]


