Abstract
Impaired hearing is related to poor health outcomes, including compromised cognitive function, in aging individuals. Hearing loss is the third most common chronic health condition after arthritis and heart disease in older adults and the fourth most detrimental condition related to quality of life in older adults. Only 18% of aging adults who have impactful hearing loss actually use custom-fit amplification. Therefore, the majority of aging individuals entering senior living facilities will have untreated hearing loss. Older adults move to senior communities to maintain or increase their social engagement, to receive care from qualified staff, and to ultimately enhance their quality of life. We know that the majority of individuals over 65 years of age have significant hearing loss, which leaves them with complex listening needs due to low incidence of hearing aid use, group communication situations that are common for social activities, interactive dining environments, and the need for telephone use to connect with loved ones. Busy staff and family members may not be aware of the impact of decreased hearing on quality of life, as well as caregiver burden. HearCARE (Hearing and Communication Assistance for Resident Engagement) is an initiative to provide communication assistance on a day-to-day basis in senior living facilities in a cost-effective manner. This innovative model for delivering audiology services and communication assistance in senior living communities employing communication facilitators who are trained and supervised by an audiologist will be described. Data related to the communication facilitator training, daily activities, interactions with the audiologist, use of devices, and impact on residents, staff, and families will be described.
Keywords: Aging, untreated hearing loss, cognition
Learning Outcomes: As a result of this activity, the participant will be able to (1) list three detrimental effects of untreated hearing loss and; (2) describe a communication facilitator training program.
Impaired hearing is related to poor health outcomes, including compromised cognitive function, in aging individuals. Individuals with untreated hearing loss suffer from depression and social isolation more than the general population.1 2 3 4 Untreated hearing loss is linked to a variety of medical issues including higher mortality in community-dwelling older adults,5 greater hospitalization and general health care use,6 poorer overall health and burden of disease,6 higher odds of falling,7 poorer adherence to treatment recommendations,8 more accidental injury and further medical difficulties,8 more preventable adverse medical events,9 higher total medical expenditures,10 and dissatisfaction with overall quality, accessibility, and receipt of information related to health care.11 Individuals with untreated hearing loss had a 40% greater chance of cognitive decline compared to those with normal hearing and mild hearing loss equated to 7 years of cognitive decline.12 Recently, Lin et al reported that peripheral hearing loss is independently associated with accelerated brain atrophy.13
Hearing loss is the third most common chronic health condition after arthritis and heart disease in older adults and the fourth most detrimental condition related to quality of life in older adults. Mathers reported that untreated hearing loss was the second leading cause (after depression) of years living with disability.14 Treating hearing loss with appropriately fit amplification can improve these outcomes including reducing caregiver burden (e.g., Palmer et al15). Given these data, one would expect aging individuals to pursue amplification, yet only ∼18% of older individuals who need amplification use hearing aids.16 Therefore, the majority of aging individuals entering senior living facilities will have untreated hearing loss. Older adults move to senior communities to maintain or increase their social engagement, to receive care from qualified staff, and to ultimately enhance their quality of life. Specifically, many adult children encourage their parents to seek senior living facilities to increase chances for socialization with others without having to leave the comfort of the facility thereby avoiding barriers related to walking and driving that may prevent socialization.
We know that the majority of individuals over 65 years of age have significant untreated hearing loss, which leaves them with complex listening needs due to low incidence of hearing aid use, group communication situations that are common for social activities, interactive dining environments, and the need for telephone use to connect with loved ones. Busy staff and family members may not be aware of the impact of decreased hearing on quality of life, as well as caregiver burden, or may not have the time or expertise to assist residents with obtaining and using communication solutions for their specific communication challenges.
Senior living facilities include skilled nursing, assisted living, and independent living. Skilled nursing and assisted living provide a higher level of care with skilled nursing providing the highest level of nursing care. Independent living provides services, but not routine nursing care. Approximately one million seniors live in assisted living facilities in the United States, and this number is expected to double by 2030.17 With increasing life expectancy and more years lived with disability, individuals retiring at 65 years of age will be deciding where to spend the next 20 or more years of their lives.18 Although the United States has had a recent economic downturn that would be expected to impact the ability for many seniors to afford the price tag of assisted living, which averages approximately $4,000.00 per month, the assisted living facility industry has withstood the economic downturn better than many other industries. This is, in part, due to the value that assisted living facilities provide seniors and their adult children.19 One would assume that seniors and their adult children would expect that the resident can access all that the facility has to offer, which would include physical and communication access. In reality, there is a focus on physical access—no curbs, automatic doors, elevators, and so on—but little to no systematic focus on communication access in public area and in individual apartments. There appears to be an assumption that if community activities are offered and are physically accessible, all of the residents will be able to participate. This is not an accurate assumption if residents have hearing loss that precludes them from fully participating. This impacts not only the individuals with hearing loss but the other residents as well who may be frustrated when a resident with hearing loss does not interact in the dining room or disrupts group activities when instructions are not heard correctly or when movies and other group listening activities are presented at a level that is uncomfortably loud for some and may not be loud enough for others.
With hearing loss being associated with increased depression, increased falls, and cognitive decline, residents of senior living facilities with untreated hearing loss may be more prone to health status decline and may benefit from on-site communication assistance. It would not be cost-effective to have an audiologist on site daily at an assisted living facility, and an audiologist is not needed for several of the hearing care activities that would be necessary on a day-to-day basis (e.g., hearing aid troubleshooting, assistance with noncustom amplifiers and group amplification systems). Yet, it would be necessary for an audiologist to oversee these activities and to train the individual providing on-site care. HearCARE (Hearing and Communication for Resident Engagement) is a model program developed to evaluate the impact of providing communication assistance on a daily basis to individuals in an assisted living facility. The premise of the program is that an off-site audiologist oversees the activities of a trained communication facilitator (CF) who provides assistance throughout the facility to ensure that all residents are communicating adequately throughout their daily activities whether those occur in public spaces or in their private apartments.
Through generous funding from the Hearst Foundation for the first year of this quality improvement program, HearCARE was implemented at a typical assisted living facility in western Pennsylvania. As part of the larger project, data were collected related to resident communication success and staff and family burden at a facility with the CF in place, at a facility with an audiologist visiting once per month (a common consultative model), and at a facility with no directed hearing/communication care. The larger project is evaluating whether the implementation of a CF who delivers hearing health care and implements communication solutions tailored to the resident and the environment will enhance communication abilities of residents, which in turn will increase social engagement, improve quality of life, and reduce burden on staff and family members as compared with facilities where this model is not implemented. These data will be reported in a separate publication. The purpose of this article is to describe the training program for the CF, the activities of the CF, interactions with the audiologist, use of devices, and impact on residents, staff, and families.
HearCARE
Communication Facilitator Training Program
A training program was developed specifically for the CF. The goal of the training program was to provide an individual with no background in communication, hearing loss, and technology the needed knowledge to be an advocate for communication through strategies and device use in the assisted living facility. This also included interacting with residents, staff, and families. This individual needed to take care of device issues and triage issues that might need to be handled by the audiologist. Fig. 1 shows the content of lectures, discussions, and videos used for the training. Fig. 2 shows the additional hands-on training that the CF and audiologist identified as necessary after the first 2 weeks at the facility. Training became iterative once the CF started in the facility and identified areas that he or she needed more training in to be comfortable. Some of this could be done via e-mail and phone calls and some required onsite visits from the audiologist as the program started. Fig. 3 provides the time devoted to different elements of the training. The section that provides the CF's view of the program highlights the need to be aware that individuals who may pursue this type of employment will likely not have a background in hearing or communication and the trainers need to be cognizant of this. Much of the training will focus on the appreciation of the importance of hearing in successful communication and the need for successful communication to support healthy aging so the CF can promote this view in the facility with residents, staff, and families.
Figure 1.
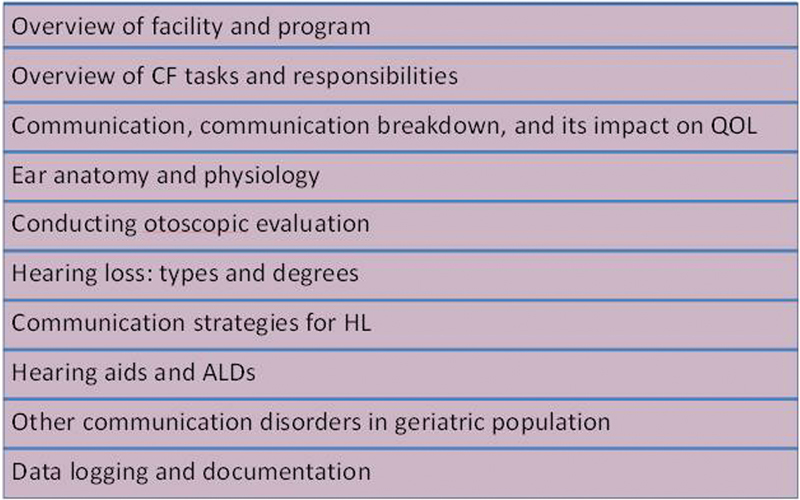
Contents of CF training program. ALD, assistive listening device; CF, communication facilitator; QOL, quality of life.
Figure 2.
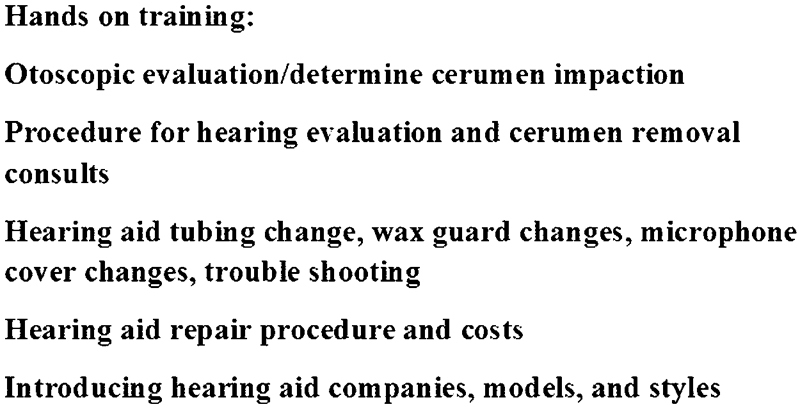
Additional hands-on training that the communication facilitator and audiologist identified as necessary after the first 2 weeks at the facility.
Figure 3.
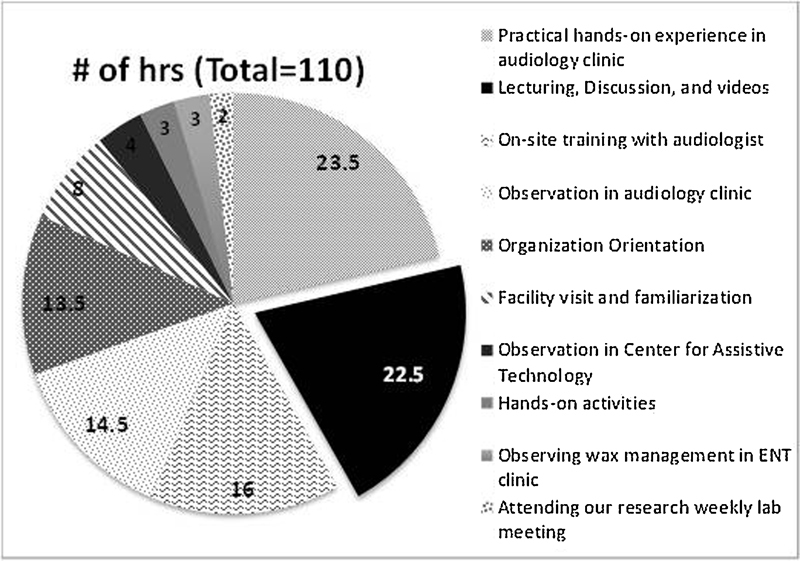
Breakdown of hours devoted to various elements of training. ENT, ear, nose, and throat.
Communication Facilitator Activities
The facility that received the CF had a capacity for 100 residents, although an average of 98 residents resided in the facility during the time period reported in this summary. The average age of the residents was 89. Fig. 4 provides a summary of activities conducted by the CF over a 1-month period. The CF has proven to be a full-time position with activities including setting up assistive listening devices for TV, phone, and group listening; hearing aid troubleshooting, insertion, cleaning and maintenance, and battery changes; facilitating communication interactions in social activities including activity room, bingo, movies, dining; and streamlining referrals for higher-level audiological care when needed.
Figure 4.
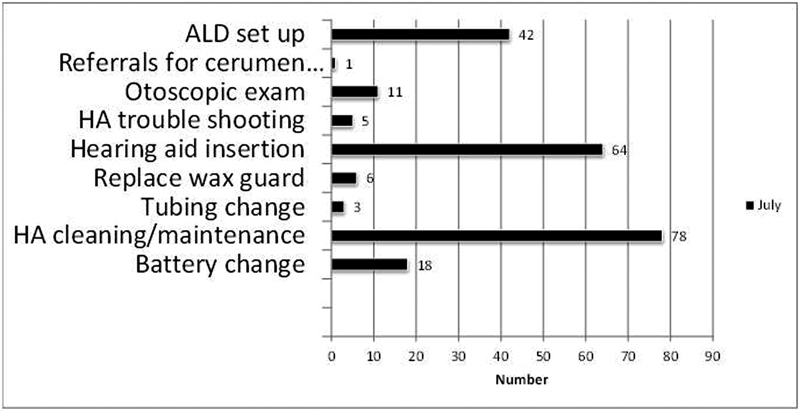
Daily tasks for a 1- month period. ALD, assistive listening device; HA, hearing aid.
Interaction with the Audiologist
It was not clear as this program started how often the audiologist would need to be on site to assist the CF or how many issues could be resolved over the phone or via e-mail. Fig. 5 provides the numbers of phone calls, e-mails, and on site visits that were conducted over a 15-month period. As can be seen in Fig. 5, the majority of questions could be answered via e-mail, with an average of 21 questions posed per month. In the current model, hearing testing and hearing aid fittings are not provided on site. If the model is expanded to include these activities, we would expect the audiologist to be on site more often to perform these activities. One challenge that the project coordinators are currently tackling is the issue of safe cerumen removal on site. Significant occlusion by cerumen is a prominent challenge in this population and impacts hearing and the successful use of devices.
Figure 5.
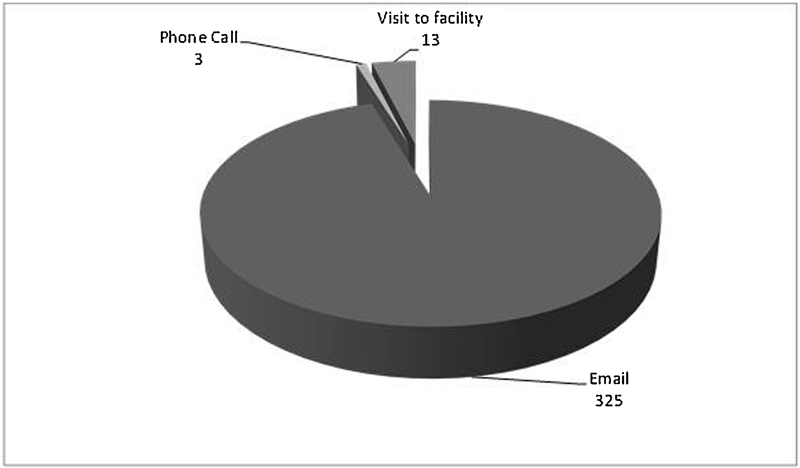
Number of communication contacts between the communication facilitator and the audiologist over a 15-month period.
Devices to Improve Communication
Our goal in implementing devices in the public areas as well as individual apartments included finding devices that were easy for residents and staff to use without extensive instruction. We also wanted to use the same devices across the facility so staff would feel familiar with the devices and would not feel that they might need to learn how to use a different device (e.g., TV or phone) in every apartment. The next section takes the reader through our decision-making process and final choice selection for assistive technology used in the facility. It is likely that several devices could have met our needs based on our described requirements. The information related to specific manufacturers/devices is provided only so the reader can see our final decisions based on what we believe are important considerations considering this population and environment. We focused globally on two areas: group/public activities and individual solutions for one-to-one communication and personal devices used within private apartments for TV, telephone, and alerting. Group devices included solutions for TV/movies and for group activities including bingo, crafts, discussions, and so on. Personal devices included personal sound amplifiers for one-to-one communication and devices to make TV and phone accessible within individual apartments as well as alerting devices. The following descriptions are organized by group versus individual solutions. Fig. 6 illustrates the final solutions chosen for personal listening, and Fig. 7 illustrates the final solutions chosen for the group listening situations.
Figure 6.
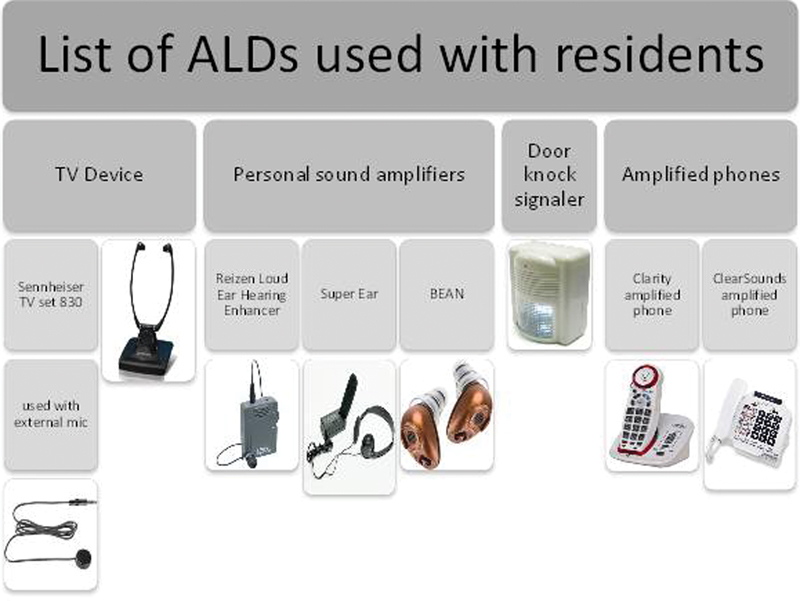
ALDs for personal use. In many cases several devices could be used; devices listed in the figure give the reader an example of devices that met all of the requirements set forth by the authors. ALD, assistive listening device. Sennheiser TV Listening, Sennheiser, Old Lyme, CT; Reizen Loud Ear Hearing Enhancer, Maxi-Aids, Farmingdale, NY; Super Ear, Sonic Technology, Grass Valley, CA; BEAN, Etymotic Research, Elk Grove Village, IL; Clarity Amplified Phone, Clear Sounds, Naperville, IL; ClearSounds Amplified Phone, Naperville, IL.
Figure 7.
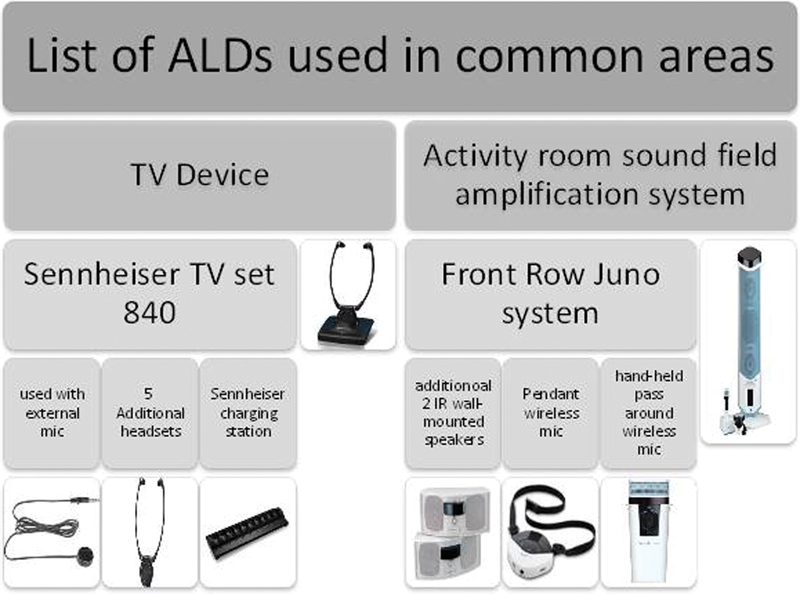
ALDs for group activities. In many cases several devices could be used; devices listed in the figure give the reader an example of devices that met all of the requirements set forth by the authors. ALD, assistive listening device; IR, infrared. Sennheiser TV Set, Sennheiser, Old Lyme, CT; Front Row Juno System, Front Row, Petaluma, CA.
Individual Solutions
TV Devices
When choosing the appropriate TV device set for a senior resident in an assisted living facility, it was our main goal to pick a device that is user-friendly not only to the resident but also to the staff. The staff (in case where there is no communication facilitator on location) will be responsible to hook up and operate the device for the resident. The TV amplifier device comes as a set composed of a transmitter that picks up the TV auditory signal, amplifies it, and transmits it to the listener; and a receiver that receives the amplified signal and directs it to the listener's ear (the headset).
Sound transmitters can be either directly wired (plugged in) to the auditory output of the TV and in this case the transmitter has to be compatible with the TV in terms of technology (analog versus digital) and has to have the appropriate jack. We chose not to use this setup because each resident's TV is different and may or may not have appropriate jacks. This also would require staff to be comfortable plugging in connections, which sometimes can be difficult to locate on wall-mounted televisions. Therefore, we chose an option that has a microphone connected to the transmitter. The microphone is placed near the TV loudspeaker (can be attached to the TV with a Velcro strap). This allowed us to bypass the possible technical barriers that may arise due to the variability of TVs used at the facility or the lack of technical awareness by the residents or facility staff. We chose an infrared transmission because these units were being used in individual apartments and we did not want leakage of an FM signal to neighboring rooms.
The choice of the receiver headset has to be low weight so senior residents can carry it and put it on their ears easily. We wanted a big volume wheel to easily adjust the volume. We chose a receiver that automatically turns on and off when it is put on and removed, which is a great feature to reduce the amount of work the user has to do when using the device. Another feature that is preferable in a TV device for this population is the easy mounting of the headset for charging. We instruct the residents and the staff that if the headset is not on the resident's ears, it should be on the transmitter station (which is connected to the power outlet) for charging.
Personal Amplifiers
Some of the residents had personal hearing aids, and in these cases we supported their use. In other cases, it was our goal to find noncustom personal amplifiers for residents who needed amplification but did not want or were not good candidates for personal hearing aids. We worked with several personal amplifiers and found each had challenges. We should note that noncustom behind-the-ear personal amplifiers were not used and might have been a good option for some of these residents. Based on our trials, the most appropriate personal amplifier for this population that is mobile yet not active and cannot easily manipulate devices was found to be box-style personal amplifier that can be hooked on the collar of a shirt or shirt pocket, rest on a walker tray, or for those less mobile, rest on a table. The noncustom amplifier that we used had the following features.
It is small in size and low weight.
It is easily attached to the resident's clothing.
It has a stable headset that does not slide off the head with head movement. Residents preferred the earbud type for continuous use.
It has a volume wheel that is easy to manipulate with reduced dexterity.
Telephones
The use of amplified phones is frequently needed in senior communities. Residents with good hearing abilities spend a considerable amount of their time talking on the phones with their children, grandchildren, and other loved ones. Residents who do not use the phone report that they cannot understand well on the phone so they quit using it for communication. Amplified phones that were successfully used in the facility had large buttons, had a defined cupped area to place on top of the ear, and most importantly could easily be hung up. The first set of phones that were used were problematic for residents to hang up because the handset continuously came off of the base and the phone line stayed busy. The second set of phones that were used had a wireless handset that had a well-defined headset to place over the ear. The handset could be easily placed on the phone station after hanging up, which ensured the phone line would be available for incoming calls as opposed to being off the hook due to the phone sliding off of the base. The phone also was hearing aid compatible with an enhanced ringer, which helped those with hearing loss to be alerted immediately of incoming calls.
Alerting Devices
There was minimal need to use alerting devices in assisted living facilities due to the dynamics of the facility during the day and night because staff and family members can access the residents' rooms without prior notice from the residents to accommodate the residents' needs. Many residents are not physically capable of moving around their rooms easily and therefore the doors are not locked most of the time. It is, however, respectful to knock on the door prior to entering and if the individual cannot hear the knock, then the warning nature of this effort is lost. A door knock signaler that flashes light upon knocking on the door was provided if residents and/or families requested the device. The door knock signaler chosen was the simplest device found in the market that is battery operated, can be hung on the door, can sense the physical door knocks, and emits flashing LED light in the resident's room.
By state law, an assisted living facility must demonstrate that the residents can alert to the smoke detector. The smoke detector signal in the facility is by design very loud and low frequency. The facility identified two residents who did not alert to the signal during a fire drill, so the Silent Call Fire Alarm (Harris Communications, Inc., Eden Prairie, MN) system was installed with two transmitters to solve this problem. In this way, additional transmitters can be added to the system when needed for new residents who are unable to alert to the regular signal during a fire drill.
Fig. 8 provides data on the number of residents using hearing aids and personal assistive listening devices. This does not capture the number of individuals using the group TV listening enhancement or the sound field system in the activity room. The sound field system impacted all residents, and there were numerous positive comments from staff, family, and residents about communication improvement with the implementation of this system. Comments included identifying individuals participating in activities that they had avoided in the past. The group TV devices also were well received but required the CF or staff member to assist residents in remembering to use the headsets and getting them set up with the equipment to receive the full benefit of the devices.
Figure 8.
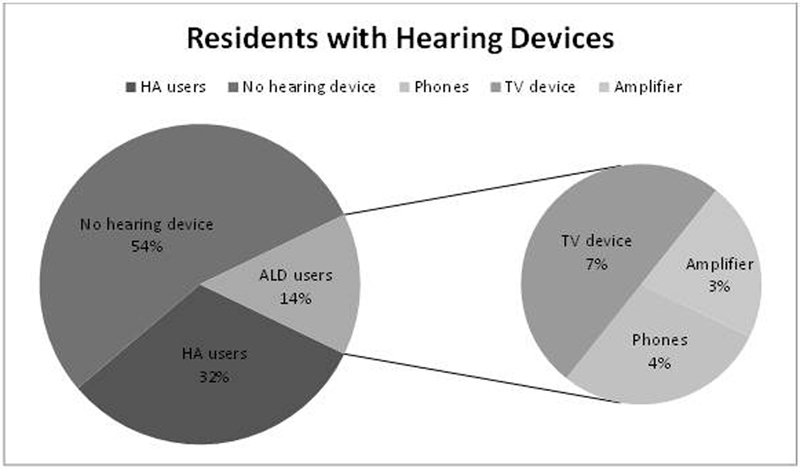
Percentages of residents with hearing aids and assistive devices. ALD, assistive listening device; HA, hearing aid.
During the first 12 months of this service, five residents could not manage personal amplifiers or TV devices, seven individuals did not like using the personal amplifiers or TV devices, and two residents reported that the personal amplifiers did not help them. It is important to remember that these solutions will not work for all residents and some residents simply will not be interested in using technology that is offered. What can be gained in these instances is awareness of such devices and the option that a resident has in attempting to try the device again as their hearing declines or after noticing they are struggling to hear without assistance.
Devices in Common and Public Areas
TV Devices
The common area TV is used for movies and sporting events. The TV uses the same device as individual residents' rooms, because it was familiar to many residents and staff. Because the device was being implemented for multiple users, there were a few important differences:
The transmitter signal was chosen to be radiofrequency as opposed to infrared. Radiofrequency signal has an extended range and is not confined between walls to accommodate larger spaces with possible furniture or wall barriers in the area.
The transmitter is wirelessly connected to multiple receivers so a group of residents can all use independent headsets with sound coming from one transmitter.
A charging station able to accept up to 10 headsets was implemented.
Activity Room Sound Field Amplification System
A sound field system was used in the activity room. The goal of a sound field system is to bathe the room in an equal level of sound regardless of where a listener is sitting. In essence, it puts all listeners near the speaker. Although these systems are called amplification systems, the goal is not to amplify the signal but rather to equalize the level of the signal to all areas of the room. Individuals with personal hearing aids will use their hearing aids and benefit from the sound being delivered at a consistent level throughout the room. Individuals without hearing aids benefit as well because they are not at a disadvantage if they cannot get a seat near the talker. Residents participate in bingo, group discussions, and various arts and crafts activities in this room. This device had to be installed, which makes it different from the other solutions described previously because it required assistance from the company to set up. The sound field system that was implemented in the activity room had the following elements:
A main speaker unit that included all the controls in addition to two additional smaller speakers. All speakers were wall mounted and appropriately distributed around the room to provide full coverage of the amplified signal.
The main speaker is capable of wirelessly connecting to two different microphones, one that is handheld to be passed around among residents or various volunteers during an interactive activity. This allows residents to hear each other much better in these instances. The other microphone is a pendant microphone that is worn around the neck by the activity moderator. The pendant allows this person to be hands free during the activity, which reduces the burden of using a handheld microphone while moderating an activity and moving around the room among residents.
The Unique Challenge of the Dining Room
Dining rooms in senior living facilities are a unique challenge. On the one hand, the staff sees this as a social time and seats groupings of residents to promote socialization and conversation according to their interests and personalities. On the other hand, the majority of individuals have untreated hearing loss and are unable to hear adequately in this noisy environment or are unable to communicate effectively due to their hearing loss. The noise consists of others in the dining room talking, the wait staff, nurses administering medication, and the noise related to the dishes and silverware. A remote microphone that can be worn by a diner will send his or her voice directly to another diner who is wearing hearing aids coupled to the remote microphone (either directly or through to a gateway device and then to the hearing aids). In this case, the solution only works for one person with hearing loss. In reality the majority of the people will have hearing loss, the minority will have personal amplification devices, and even fewer will have hearing aids with remote microphones. If an individual does have this type of communication solution, the wait staff may need to help set it up and that may be problematic. Etymotic Research, Inc (Elk Grove Village, IL) is developing a device that has four microphones and four headsets allowing all four people at a table to hear their dining partners without needing personal amplification (can couple to the ear with an earbud or through a telecoil with a personal hearing aid). Given that assisted living facilities have four tops in the dining room to have smaller groups eating together, this device might be ideal if someone is available to set it up for the listeners. A communication facilitator could help with this if he or she is in the facility during dinner time or the communication facilitator could train the wait staff to assist with this. It would be interesting if the wait staff were not only responsible for serving food but ensuring communication during the meal. It might also help to have residents practice using the devices in small groups in quiet times during the day rather than introducing this type of system in the middle of a meal, which may feel busy for the residents with the other people, noise, ordering food, and so on.
Impact of HearCARE on Residents, Staff, and Families
One of the long-term goals of this quality improvement project is to compare resident, staff, and family members' perceptions of communication improvements and reduction of caregiver burden across a facility implementing the CF model, a facility receiving once per month visits from an audiologist (a common model) and a facility receiving no hearing care. Questionnaires administered to residents and families were used for this purpose. In addition, data reported to the state each month including number of falls, hospital admissions, change in level of care, adverse events, and so on will be compared between facilities. For staff, we collected data through a questionnaire to probe communication involvement of residents by asking staff member's views of the group's hearing problems, communication abilities, use of assistive technology, and participation. These data will be described in a separate report and will assist in analyzing the cost-effectiveness of this program. Fig. 9 provides representative comments from residents and families who benefited from the program. To date, the CF has proven to be a meaningful, full-time position, with residents, staff, and family members appreciating the positive impact of the program.
Figure 9.
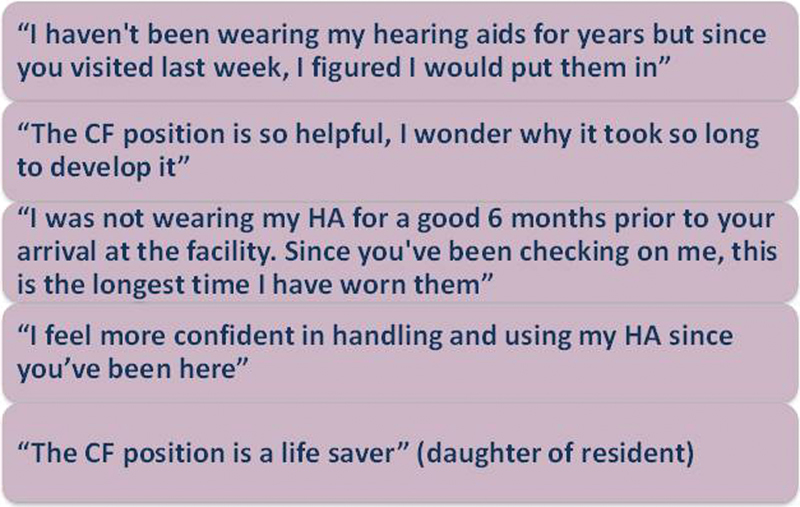
Example feedback from residents and families. CF, communication facilitator; HA, hearing aid.
One of the challenges is deciding how this type of program should be funded. It is increasingly common for senior care facilities to offer à la carte choices of personal care and the hearing services could be added to this. The concern would be that individuals worried about how long their money is going to last might forgo these services (daily or weekly hearing aid check, and so on). Another model might include a level of hearing-related services in the monthly payment the individual is already providing with the rationale that facilities would not charge extra to make sure the facility was physically accessible and should not charge extra to make sure the facility and activities are communication accessible. A hybrid model might also be attractive where some services are considered part of accessibility and other services and/or devices would be paid for by residents or their families.
The Communication Facilitator's Perspective
This section is written from the perspective of the communication facilitator. These are her thoughts related to the position, which help audiologists understand the many things related to communication, assistive devices, and hearing aids that we may take for granted. This is a reminder that individuals who are not trained in hearing do not implicitly understand the importance of hearing to successful aging, which is why training is an essential aspect of the success of the CF position.
As a communication facilitator, duties at the senior living facility vary from simple tasks like replacing a wax guard to more difficult tasks like troubleshooting a nonfunctioning hearing aid. Daily activities are tasks that the communication facilitator will do for the residents of the facility to prevent blockages in hearing aids, hearing aid loss and damage, and failure to use hearing aid(s). Duties also include creating a general awareness and appreciation for custom hearing devices if they are appropriate for a particular resident. The CF will have a list of residents who need to be visited daily to ensure his or her hearing aid is functioning and inserted correctly at all times of the day. These tasks include cleaning hearing aid vents, tubing, domes, receiver area, microphones, sanitizing the hearing aid body, checking for proper hearing aid placement in ear, encouraging and reminding residents to insert hearing aids, keeping track of hearing aid location when not in use, changing wax guards, checking in on assistive listening device function and use, and performing listening checks on hearing aids. In addition, the CF will evaluate communication success in individual apartments and make recommendations related to TV, phone, and alerting devices. The CF also will participate in group activities making sure that the staff and residents know how to use the noncustom group hearing devices. These also all require ongoing upkeep and instruction with the staff.
Not all problems that arise will be something simple for the CF to fix. Some hearing aids may require more time than others to restore to proper functioning or some may need to be sent out for repair. The CF will need a level of discernment in these scenarios to sort out the issue and know how to handle it appropriately. The hearing aid may not be functioning because there is a block in the ear hook, or the tubing needs to be changed, in which case the CF is trained to restore the hearing aid to proper functioning. In other cases, the CF will have had tried all the troubleshooting techniques and the hearing aid is still not functioning correctly. In this instance, the CF will know that the hearing aid needs to be sent out for repair. The CF will need to contact the family to see if they want our group to send out the repair or if they would like to take the hearing aid to the original dispenser. The CF will then take the appropriate steps to ensure this process will be completed for the family and the resident. This also includes receiving payment for any repair charges.
CF training is key to the position's success. The training included 110 hours total of lecturing/discussion, orientation, supervised time out in the field and observation, and hands-on experience in the audiology clinic. The lecture time is imperative for the CF to learn about the structures and functions and disorders of the ear, what happens to the ear as a result of hearing loss, and how to help those with hearing loss. During training the CF will be introduced to hearing aids, how they work, how they are cleaned, and how to troubleshoot hearing aids when aids are not functioning. The knowledge gained during fieldwork and actual experiences with the residents' hearing aids, hearing loss, and general communication problems will help the CF to understand all aspects of communication and patient care.
It is important that the CF understands the importance of hearing loss in relation to a person's quality of life and delivers communication services at all times. Part of the CF's position is to create a general awareness about assistive listening devices through regular maintenance and utilization of the devices, but also by being a resource of information for staff, family, and residents for communication strategies and personalized solutions.
As someone with no former audiology background, I was intrigued by how much hearing affects communication. Now that I am trained, this sounds ridiculous because I understand the impact of hearing loss but for those outside audiology, the impact of hearing loss on quality of life and health care outcomes will not be obvious. When I thought of communication, I thought of the words exchanged and how they are interpreted but did not give much thought to how a person is hearing those words. As someone who was not affiliated with audiology, it was amazing to learn that hearing is absolutely imperative to how one communicates. I assumed that a person with hearing loss is able to read lips or make do, but I did not think that people with hearing loss would not participate or avoid activities because of the hearing loss.
I also was surprised to learn how sensitive hearing aids are and how difficult it is for the older individuals to keep hearing aids functioning at all times when there is no one there to remind and assist them. Limited dexterity, mobility, and memory keeps many of the residents from being able to perform battery changes, maintain and insert devices, and even know when hearing aids are working or not. These challenges make it nearly impossible for the hearing aids to be functioning on a consistent basis. I never knew that such small fixes like changing the batteries and wax guards, brushing the mics, and cleaning any blockages within hearing aids could make such an impact on the way the hearing aids perform. This position helped me see just how much older individuals and staff working with them struggle to communicate and participate in activities if there is not someone in the facility specifically charged with making sure everyone can communicate through the use of devices and strategies.
Conclusions and Future Directions
The CF model may be a cost-effective way to extend audiology-based solutions for enhancing hearing and communication for residents in residential settings. Data from the quality improvement project indicate that:
CFs can be trained by audiologists in less than a month.
CFs can significantly reduce the burden of traveling to the audiology clinic for simple hearing aid repairs for residents and family members.
CFs can increase hearing aid use and assistive listening technology use.
CFs can increase awareness of residents, staff, and families of the importance of successful communication for health aging.
CF training and activities need to be overseen by an audiologist who can be available by e-mail and phone with infrequent facility visits.
Further data collection and analysis are needed to evaluate possible reimbursement methods to make this service sustainable. This includes analysis of possible cost savings to the facility if reduction in unwanted outcomes (e.g., falls, hospitalization, increased medications, increased level of care) can be demonstrated with the use of CFs.
Acknowledgment
The Hearst Foundation generously funded the first year of the HearCARE quality improvement project. Jenifer Fruit was instrumental in designing this project.
References
- 1.Chuan-Ming L. et al. Hearing impairment associated with depression in US adults, NHANES 2005–2010. Otolaryngol Head Neck Surg. 2014;140(4):293–302. doi: 10.1001/jamaoto.2014.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jones E M, White A J. Mental health and acquired hearing impairment: a review. Br J Audiol. 1990;24(1):3–9. doi: 10.3109/03005369009077837. [DOI] [PubMed] [Google Scholar]
- 3.Garnefski N, Kraaij V. Cognitive coping and goal adjustment are associated with symptoms of depression and anxiety in people with acquired hearing loss. Int J Audiol. 2012;51(7):545–550. doi: 10.3109/14992027.2012.675628. [DOI] [PubMed] [Google Scholar]
- 4.Mick P, Kawachi I, Lin F R. The association between hearing loss and social isolation in older adults. Otolaryngol Head Neck Surg. 2014;150(3):378–384. doi: 10.1177/0194599813518021. [DOI] [PubMed] [Google Scholar]
- 5.Genther D J, Betz J, Pratt S. et al. Association of hearing impairment and mortality in older adults. J Gerontol A Biol Sci Med Sci. 2015;70(1):85–90. doi: 10.1093/gerona/glu094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Genther D J, Frick K D, Chen D, Betz J, Lin F R. Association of hearing loss with hospitalization and burden of disease in older adults. JAMA. 2013;309(22):2322–2324. doi: 10.1001/jama.2013.5912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lin F R, Ferrucci L. Hearing loss and falls among older adults in the United States. Arch Intern Med. 2012;172(4):369–371. doi: 10.1001/archinternmed.2011.728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lawthers A G, Pransky G S, Peterson L E, Himmelstein J H. Rethinking quality in the context of persons with disability. Int J Qual Health Care. 2003;15(4):287–299. doi: 10.1093/intqhc/mzg048. [DOI] [PubMed] [Google Scholar]
- 9.Bartlett G, Blais R, Tamblyn R, Clermont R J, MacGibbon B. Impact of patient communication problems on the risk of preventable adverse events in acute care settings. CMAJ. 2008;178(12):1555–1562. doi: 10.1503/cmaj.070690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Foley D M, Frick K D, Lin F R. Association between hearing loss and healthcare expenditures in older adults. J Am Geriatr Soc. 2014;62(6):1188–1189. doi: 10.1111/jgs.12864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hoffman J M, Yorkston K M, Shumway-Cook A, Ciol M A, Dudgeon B J, Chan L. Effect of communication disability on satisfaction with health care: a survey of Medicare beneficiaries. Am J Speech Lang Pathol. 2005;14(3):221–228. doi: 10.1044/1058-0360(2005/022). [DOI] [PubMed] [Google Scholar]
- 12.Lin F R, Yaffe K, Xia J. et al. Hearing loss and cognitive decline in older adults. JAMA Intern Med. 2013;173(4):293–299. doi: 10.1001/jamainternmed.2013.1868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lin F R, Ferrucci L, An Y. et al. Association of hearing impairment with brain volume changes in older adults. Neuroimage. 2014;90:84–92. doi: 10.1016/j.neuroimage.2013.12.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mathers C, Geneva, Switzerland: World Health Organization; 2003. Global Burden of Hearing Loss in the Year 2000. [Google Scholar]
- 15.Palmer C V, Adams S W, Bourgeois M, Durrant J, Rossi M. Reduction in caregiver-identified problem behaviors in patients with Alzheimer disease post-hearing-aid fitting. J Speech Lang Hear Res. 1999;42(2):312–328. doi: 10.1044/jslhr.4202.312. [DOI] [PubMed] [Google Scholar]
- 16.Chien W, Lin F R. Prevalence of hearing aid use among older adults in the United States. Arch Intern Med. 2012;172(3):292–293. doi: 10.1001/archinternmed.2011.1408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Retirement communities in the US. May 2009. IBISWorld, Santa Monica, CA. University of Texas at San Antonio. John Peace Library, San Antonio, TX. June 10, 2009, Available at: http://www.ibisworld.com. Accessed April 24, 2017
- 18.American Association of Retirement Communities. Attracting retirees as an economic development strategy: looking into the future. Economic Development Quarterly. 1995;9(4):372–382. [Google Scholar]
- 19.Senior living executives optimistic about future. PR Newswire University of Texas at San Antonio, John Peace Library; San Antonio, TX, June 9, 2009. Available at: prnewswire.com/news-releases/senior-living-executives-optomistic-about-future-61795297.html. Accessed April 24, 2017 [Google Scholar]


