Abstract
The management of frontal sinus fractures has evolved in the endoscopic era. The development of functional endoscopic sinus surgery (FESS) has been incorporated into management algorithms proposed by otolaryngologists, but the extent of its influence on plastic surgeons and oral and maxillofacial surgeons is heretofore unknown. A cross-sectional survey was performed to assess the practice pattern variations in frontal sinus fracture management across multiple surgical disciplines. A total of 298 surveys were reviewed. 33.5% were facial plastic surgeons with otolaryngology training, 25.8% general otolaryngologists, 25.5% plastic surgeons, and 15.1% oral and maxillofacial surgeons. 74.8% of respondents practiced in an academic setting. 61.7% felt endoscopic sinus surgery changed their management of frontal sinus fractures. 91.8% of respondents favored observation for uncomplicated, nondisplaced frontal sinus outflow tract fractures. 36.4% favored observation and 35.9% favored endoscopic sinus surgery for uncomplicated, displaced frontal sinus outflow tract fractures. For complicated, displaced frontal sinus outflow tract fractures, obliteration was more frequently favored by plastic surgeons and oral and maxillofacial surgeons than those with otolaryngology training. The utility of FESS in managing frontal sinus fractures appears to be recognized across multiple surgical disciplines.
Keywords: frontal sinus fracture, endoscopic sinus surgery, otolaryngology, plastic surgery, oral and maxillofacial surgery, survey
The frontal bone is stronger than any other facial bone, requiring 3.6 to 7.1 kN of force to cause a fracture.1 These fractures are most commonly due to high impact, craniomaxillofacial (CMF) injuries such as motor vehicle accidents, assaults, and industrial accidents.2 Due to improved safety mechanics in automobiles and laws requiring seat belt use, the incidence of frontal sinus fractures has diminished.2 Overall, 5 to 15% of all facial fractures may involve the frontal sinus with 33 to 70% of these patients presenting with intracranial injuries.3 4 5 6 7
Injuries to the frontal sinus are categorized by location and type with fracture patterns classified as displaced versus nondisplaced or comminuted versus noncomminuted. Thin-cut (1.0–1.5 mm) axial computed tomographic (CT) scan with sagittal and coronal reformats is the preferred radiologic modality to define the extent of injury to the frontal sinus.8 Fractures can involve the anterior table (AT), posterior table (PT), and/or the frontal sinus outflow tract (FSOT). Each subsite carries its own indications for repair. The goals in treating anterior and posterior table (APT) fracture are to prevent intracranial complications and restore cosmesis while rehabilitating the sinus to its baseline function. Injuries to the FSOT are managed to avoid the long-term sequelae secondary to obstruction. Traditional surgical approaches required obliteration or cranialization in cases of complicated PT fractures or those involving the FSOT.
Multiple surgical specialties are involved in caring for frontal sinus fractures, reflected in the various available treatment algorithms.3 5 6 Otolaryngologists have proposed novel algorithms to incorporate advances in radiologic imaging and surgical techniques.9 10 11 12 Functional endoscopic sinus surgery (FESS) offers an alternative to frontal sinus obliteration and cranialization to manage the initial injury and potential long-term complications of frontal sinus fractures, including meningitis, cerebrospinal fluid (CSF) leak, mucoceles, and osteomyelitis.12 13 14 Outpatient endoscopic exams can corroborate radiologic findings to improve surveillance when electing to treat FSOT fractures conservatively. Endoscopic surgical interventions can involve extended endoscopic frontal sinusotomy (Draf type II) or endoscopic modified Lothrop procedures (Draf type III) to address the long-term complications of FSOT fractures, including chronic frontal sinusitis, mucoceles, or mucopyoceles. Balloon dilation sinuplasty is a novel and minimally invasive method for treating sinus outflow obstruction.15 16 In cases of difficult revision frontal sinus surgeries, a technique using a combination of balloon dilation and powered instruments has been reported to perform extended endoscopic frontal sinusotomies.17 Hueman and Eller reported successful reduction of an AT fracture involving the FSOT using balloon sinuplasty,18 but the utility of treating frontal sinus obstruction secondary to trauma with balloon dilation has not yet been thoroughly explored. Additionally, endoscopic transnasal approaches can be used to reduce APT fractures.19 20 Despite the advancement of FESS in the endoscopic era, the extent of its influence in the management principles of those caring for CMF trauma is not clearly known. Nevertheless, as FESS is practiced solely by otolaryngologists, we hypothesize that its utility is recognized more commonly by those with background in otolaryngology than those with plastic surgery or oral and maxillofacial surgery training. This survey was created to collect quantitative data on the practice patterns of physicians treating frontal sinus fractures and to analyze the practice differences among various surgical disciplines.
Materials and Methods
This study was approved as an exempt study by the IRB. A survey was created to query patterns in managing FSOT fractures among various surgical specialties. The survey eliminated scenarios wherein there exists a widely accepted practice pattern: isolated AT fractures with cosmetic defects or PT fractures with intracranial complications. Demographic data were gathered to assess the respondents' surgical training, practice setting, region of practice, access to a rhinologist, and number of years in practice. Respondents were asked whether FESS changed their management of FSOT fractures.
In April 2015, an e-mail containing the survey (Fig. 1) was sent to the members of the American Academy of Facial Plastics and Reconstructive Surgery (AAFPRS), Society of University Otolaryngologists (SUO), American Society of Maxillofacial Surgeons (ASMS), and AO Craniomaxillofacial (AOCMF). The goal was to gather responses from facial plastic surgeons with training in otolaryngology (FPRS), general otolaryngologists (OHNS), plastic surgeons (PS), and oral and maxillofacial surgeons (OMFS), given their role as primary managers of CMF traumas. The members of the American Rhinologic Society were not included as they are not involved in the initial evaluation of patients with frontal sinus fractures. Participation was voluntary, and the participants' willingness to complete the questionnaire was their consent. Two follow-up e-mails were sent in 3-week intervals as a reminder in accordance with the Dillman Total Design Survey Method.21 Compensation was not provided.
Fig. 1.
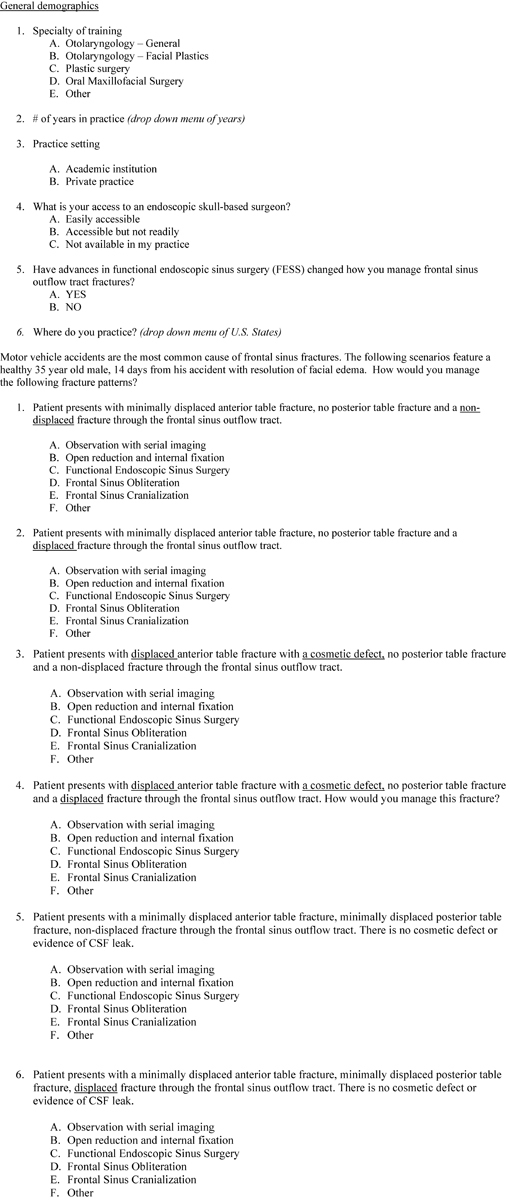
Survey distributed to the members of SUO, American Academy of Facial Plastics and Reconstructive Surgery (AAFPRS), American Society of Maxillofacial Surgeons (ASMS), and AO Craniomaxillofacial (AOCMF) via e-mail.
Clinical scenarios were selected to assess how concomitant AT and PT fractures may influence the management of FSOT fractures. Statistical analysis was unable to be performed due to the lack of variability in the survey results. Instead, descriptive statistics were utilized to present the study findings. The scenarios surveyed are listed below:
Scenario 1: Isolated, nondisplaced FSOT fracture.
Scenario 2: Isolated, displaced FSOT fracture.
Scenario 3: Nondisplaced FSOT fracture with displaced AT fracture causing cosmetic defect.
Scenario 4: Displaced FSOT fracture with displaced AT fracture causing cosmetic defect.
Scenario 5: Nondisplaced FSOT fracture with uncomplicated APT fractures.
Scenario 6: Displaced fracture FSOT with uncomplicated APT fractures.
Study data were collected and managed using Research Electronic Data Capture (REDCap) tools, which is a secure, web-based application designed to support data capture for research studies through (1) an intuitive interface for validated data entry; (2) audit trails for tracking data manipulation and export procedures; (3) automated export procedures for seamless data downloads to common statistical packages; and (4) procedures for importing data from external sources.22
Results
The survey was distributed to 2,892 members (438 SUO members, 1,100 AAFPRS members, 946 AOCMF members, and 408 ASMS members). The response rate was 10.5% (304/2,892) and 298 completed surveys were included for review. The regional distribution of respondents is depicted in Fig. 2. The general demographic of the study cohort is outlined in Table 1. The number of years in clinical practice did not influence whether respondents felt FESS changed their management principles, as 36.5% (58/159) of those with 15 or less years of practice and 40.3% (56/139) of those with more than 16 years of practice responded that FESS did not alter their practice patterns. Similar percentage of OMFS (68.9% [31/45]) and PS (77.6% [59/76]) responded that FESS did not influence their management of frontal sinus fractures.
Fig. 2.
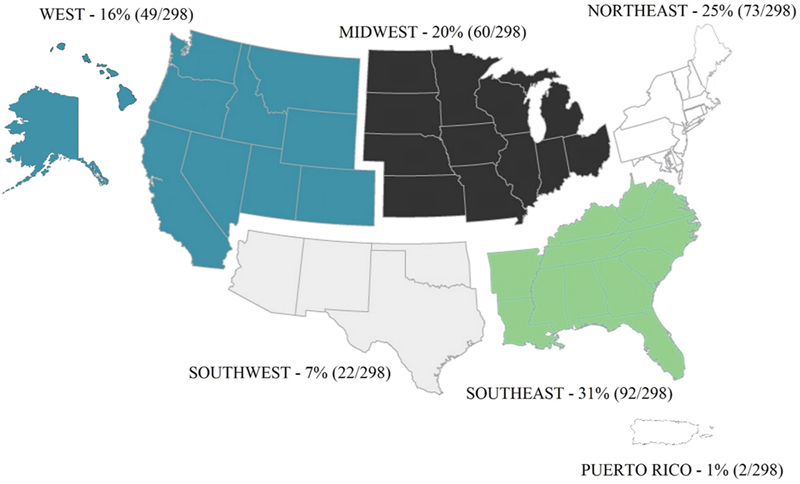
Regional groupings of all survey respondents within the United States.
Table 1. Study demographics.
| Surgical specialty | |
|---|---|
| General otolaryngologist | 25.8% (77/298) |
| Facial plastic surgeons | 33.5% (100/298) |
| Plastic surgeons | 25.5% (76/298) |
| Oral and maxillofacial surgeons | 15.1% (45/298) |
| Average number of years in practice | 15.9 (1–40 y) |
| Practice setting | |
| Academic practice | 74.8% (223/298) |
| Private practice | 25.2% (75/298) |
| Access to rhinologist | |
| Easily accessible | 71.8% (214/298) |
| Accessible not but readily | 16.1% (48/298) |
| Not available in my practice | 12.1% (36/298) |
| Has FESS changed your management of FSOT fractures? | |
| Yes | 61.7% (184/298) |
| No | 38.2% (114/298) |
Abbreviations: FESS, functional endoscopic sinus surgery; FSOT, frontal sinus outflow tract.
Most respondents (94.6% [282/298]) endorsed observation for isolated, nondisplaced FSOT fracture (Fig. 3a). This was true regardless of specialty, with 97.7% (173/177) of those with otolaryngology training and 90.1% (109/121) of PS or OMFS endorsing observation. Ten respondents endorsed other management principles that were not listed in our survey.
Fig. 3.
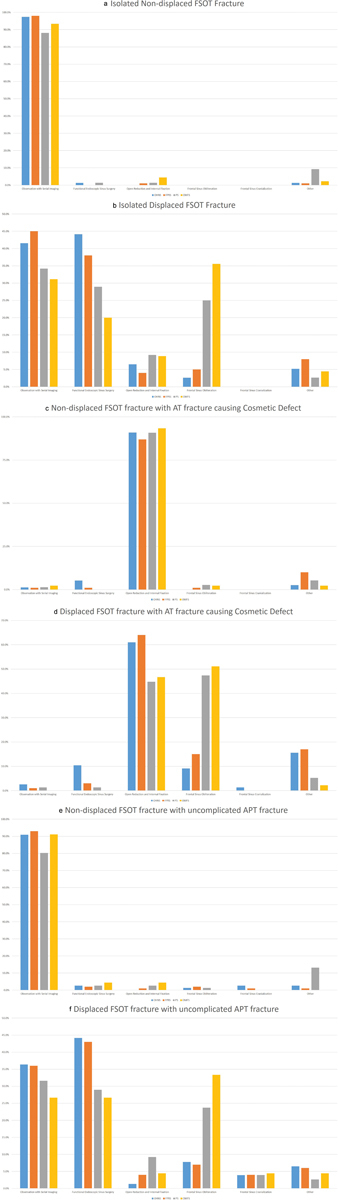
(a–f) Distribution of survey results per surgical specialty. Percentages represent number of selected answers per surgical specialty/total number of respondents per surgical specialty.
Observation was most frequently selected (39.3%, 117/298) in managing isolated, displaced FSOT fractures (Fig. 3b). FESS was the second most frequently selected treatment (34.6%, 103/298). Otolaryngologists were split between observation (43.5% [77/177]) and FESS (40.7% [72/177]). PS and OMFS favored serial observation (33.1% [40/121]) over FESS (25.6% [31/121]). Only 14.1% (42/298) of respondents believed that obliteration was warranted for displaced FSOT fractures. Obliteration was preferred by PS (45.2%, 19/42) and OMFS (38.1%, 16/42) more frequently than OHNS (4.8%, 2/42) or FPRS (11.9%, 5/42). Open reduction internal fixation (ORIF) was supported by 6.7% (20/298) of respondents and other unlisted management strategies supported by 5.4% (16/298) of respondents.
Almost all respondents (89.9% [268/298]) supported ORIF for treatment of nondisplaced FSOT fractures with a displaced AT fracture causing cosmetic deformity (Fig. 3c). This was supported by 88.7% (157/177) of respondents with training in otolaryngology compared with 91.7% (111/121) of PS or OMFS. Other management principles were endorsed by 17 respondents. FESS (1.7%, 5/298), observation (1.3%, 4/298), and obliteration (1.3%, 4/298) were all infrequently selected.
ORIF was most frequently selected (166/298, 55.7%) for displaced FSOT fractures with a displaced AT fracture causing cosmetic deformity (Fig. 3d). Obliteration was supported by 27.2% (81/298) of respondents, and preferred by PS (44.4%, 36/81) and OMFS (28.4%, 23/81) more frequently than by OHNS (8.6%, 7/81) or FPRS (18.5%, 15/81). Other management principles were selected by 11.4% (34/298) of respondents, followed by FESS (4.0%, 12/298), observation (1.3%, 4/298), and cranialization (0.3%, 1/298).
Almost all physicians (88.9% [265/298]) supported observation when a nondisplaced FSOT fracture was present with an uncomplicated APT fracture (Fig. 3e). Sixty-one percent (163/265) of these respondents had training in otolaryngology, while 38.5% (102/265) were PS or OMFS. Thirteen respondents supported other treatment protocols. FESS (2.7%, 8/298), ORIF (1.7%, 5/298), obliteration (1.3%, 4/298), and cranialization (1.0%, 3/298) were infrequently selected.
FESS was endorsed by 37.3% (111/298) of respondents when displaced FSOT fractures were present with an uncomplicated APT fracture (Fig. 3f). More respondents had training in otolaryngology (69.4% [77/111]) than PS and OMFS combined (30.6% [34/111]). Observation was selected by 33.6% (100/298) of respondents following a similar distribution: Sixty-four percent (64/100) had otolaryngology training, whereas 36% (36/100) had PS or OMFS training. Obliteration was selected by 15.4% (46/298) of respondents, and was preferred by PS (39.1%, 18/46) and OMFS (32.6%, 15/46) more frequently than by OHNS (13.0%, 6/46) or FPRS (15.2%, 7/46). Other procedures (5.0%, 15/298), ORIF (4.7%, 14/298), and cranialization (4.0%, 12/298) were not favored for this clinical scenario.
Discussion
Management principles of frontal sinus fractures have evolved over time. Today, there are multiple surgical subspecialties involved in the management of craniomaxillofacial (CMF) injuries, including OMFS, PS, FPRS, and OHNS. Although there are surgical principles agreed upon by all specialties, some treatment paradigms continue to be debated. In 1973, Newman and Travis espoused the use of osteoplastic frontal sinusotomy with fat obliteration for managing FSOT injuries.23 They also suggested that unilateral injuries be treated by removing the intersinus septum and reconstructing the injured FSOT.23 Gruss proposed in 1986 that bony injuries to the FSOT be repaired with rigid fixation to restore its function.24 Subsequently in 1992, Rohrich and Hollier endorsed a progressive treatment algorithm based on the degree and location of the displaced bone, and the presence of a CSF leak.5 Injuries involving the FSOT were recommended for obliteration with autologous bone grafts. Gonty et al supported obliteration techniques with fat, muscle, or bone for FSOT fractures in 1999.3 A survey published in 1992 by Thaller and Kawamoto demonstrated that the management of FSOT injuries appeared to be inconsistent among PS.25
Complications incurred by patients following frontal sinus fractures are significant. The risk for mucocele formation is high in patients treated with obliteration or cranialization.6 26 27 This is especially true in trauma due to soft tissue and bony injuries. Successful obliteration or cranialization is difficult to achieve in this scenario due to compromised vascularity or difficult access secondary to comminuted or displaced fracture segments.6 12 Fat graft obliteration in a devascularized frontal sinus can develop graft resorption or necrosis, creating an incomplete obliteration that is prone to complications.28 Due to these difficulties, surgeons have long desired an alternative means for treatment.
Surgical options for frontal sinusitis include frontal sinusotomy or extended endoscopic approaches. Although routine FESS and extended endoscopic approaches to the frontal sinus risk subsequent FSOT stenosis and mucocele formation, they have been successfully applied to the management of frontal sinus fractures to potentially avoid obliteration or cranialization.12 Two adaptions for the timing of endoscopic surgery to address the FSOT have been described. Smith et al reported expectant observation of the FSOT with serial CT scans and endoscopic exams following ORIF of displaced AT segments at the time of injury.12 Extended frontal sinusotomies were required in two of five patients who developed subsequent FSOT obstruction during the observation that were refractory to medical management. Emara et al described a method for simultaneous debridement of lacerated mucosa and bony spicules at the FSOT during the time of open repair involving the AT or the nasoorbitoethmoid complex.29 Excellent results were reported with 13 of 17 patients demonstrating complete restoration of frontal sinus function and 4 patients with mild mucosal thickening on CT without evidence of sinusitis at a mean follow-up of 20 months. Despite these reports and newly proposed algorithms, it is important to note that there is no consensus among otolaryngologists on the timing and extent of endoscopic surgeries required in the management of FSOT fractures.
Advances in radiologic technique are critical in determining the need for operative intervention or conservative management of frontal sinus fractures. Rodriguez et al reported that FSOT obstruction is the most common predictor of complications following frontal sinus fractures and can be identified radiographically by the following criteria: (1) frontal sinus floor fracture, (2) fracture of the medial aspect of the AT, and (3) FSOT obstruction.30 These criteria were correlated with intraoperative findings by Yakirevitch et al in a retrospective review, and determined that an increasing number of radiographic criteria present was predictive of intraoperative evidence of FSOT obstruction.31 The treatment algorithm proposed by Rodriguez et al30 based on these criteria endorses observation when the FSOT is patent, and for treatment with obliteration or cranialization when FSOT obstruction is present at the time of injury. This was again supported by a retrospective review by Stanwix et al, endorsing that radiologic obstruction of the FSOT is pivotal in surgical planning,32 and the aforementioned criteria for identifying FSOT obstruction must be appropriately evaluated by the surgeon at the time of injury.
In addition to preoperative planning, radiographic scans can be used to complement observation strategies by complementing the endoscopic exam. Although this is useful for primary observation, it may be difficult when monitoring an obliterated frontal sinus. The obliteration precludes endoscopic assessment of the frontal sinus beyond the area of obliteration and the endoscopic findings may not correlate with clinical symptoms. Surveillance with radiologic imaging can be problematic, as CT and MRI may provide variable and inconclusive results.33 34 Alternatively, endoscopic transnasal approaches have been deployed to address complicated fractures to the APT to minimize intracranial complications and address cosmetic defects.15 Despite the introduction of FESS into the treatment algorithm managing frontal sinus fractures, the extent of its influence on those with and without otolaryngology training is unknown. This survey seeks to provide an update on current practice patterns among all surgical specialties involved in managing frontal sinus fractures.
Our survey demonstrates the role of FESS in managing frontal sinus fractures which is primarily recognized by those with training in otolaryngology. This is not surprising given the diversity in training among the surgical specialties. As OMFS and PS have limited exposure to FESS during residency, the extent of its influence on the management principles of frontal sinus injuries is limited for these specialists. In contrast to previously published surveys on OMFS and PS, our data demonstrate an acknowledgment among these specialists that FSOT injuries do not always require obliteration or cranialization.21 35
Surgical expertise and knowledge of the anatomy are necessary in performing frontal sinusotomies, as the dissection of the FSOT can be challenging due to its variable anatomy and the need for angled endoscopes and instruments. We hypothesized that recent graduates are more likely to rely on FESS, given their increased likelihood for exposure during training. However, the number of years in clinical practice did not appear to influence the respondents in determining whether FESS changed their management principles, independent of their specialty.
Our results suggest that CMF surgeons believe nondisplaced fractures of the FSOT do not warrant repair. Observation was suggested for an isolated or uncomplicated, nondisplaced fracture through the FSOT (clinical scenarios 1 and 5). The survey response to clinical scenario 3 also reinforces this trend, as ORIF was most often selected to treat the AT fracture independently, rather than with obliteration in the event of a nondisplaced FSOT fracture. These results suggest that observation, if appropriately selected, is agreed upon to be reliable by all surgical specialties. Although only 61.7% of all respondents felt that FESS changed their management principles, there was an overwhelming support for observation in managing nondisplaced FSOT fractures. This can be attributed to improvements in radiologic imaging, or may also represent a trend toward conservative measures, as long-term results of obliteration and cranialization become even more apparent. Among otolaryngologists, proficiency in nasal endoscopy can provide corroborative data in addition to radiologic studies in selecting observation as the primary mode of treatment in this patient population.
Observation was most frequently selected for isolated, displaced fractures of the FSOT or displaced FSOT fracture with uncomplicated APT fractures. FESS was the second most frequently selected treatment method in the aforementioned clinical scenarios. These responses echo previous findings that conservative measures are pursued in appropriately selected cases. Results also suggest that FESS has a primary role in managing displaced FSOT fractures, as the likelihood of FSOT stenosis with mucocele formation is high. All surgical subspecialties queried in our survey acknowledged the utility of FESS in these scenarios, demonstrating a significant shift in practice pattern compared with prior surveys, when FESS was not readily available.21 35 Another practice pattern that emerged in these scenarios was that OMFS and PS were more likely to perform obliterations than OHNS or FPRS. This finding suggests that there is a subset of OMFS and PS that are unfamiliar with FESS, or feel that improved outcomes can be achieved with obliteration. It is also possible that these practitioners may not have access to a rhinologist to perform surveillance exams or surgical interventions when required. When a displaced FSOT fracture was present with an AT fracture requiring repair, obliteration was preferred by OMFS and PS, followed by ORIF. For those with background training in otolaryngology, ORIF was the preferred treatment method followed by an otherwise unlisted procedure. This discrepancy highlights the reliance by OMFS and PS on traditionally proposed treatment methods, a disparity that may be due to variance in surgical training. Additionally, this may be attributed to their extensive experience with the vagaries of endoscopy and willingness to avoid repetitive endoscopic surveillance procedures. Although not evaluated in this study, the greater ease in performing endoscopic rescue procedures utilizing balloon sinuplasties in those who fail traditional treatments may also play a role in the pragmatic perception of FESS in the treatment algorithm of frontal sinus fractures.
There are several limitations to our study. There is an inherent sampling bias, as it is likely that only those proficient in managing frontal sinus fractures responded to the survey. This may explain the low response rate, contributing to the decreased validity of our results. Though if this assumption is true, it is the expertise of the respondents who provide this service that establishes current opinions on standard of care. We recognize that the introduction of sampling error could not be avoided when surveying large professional societies. There is also a selection bias, as the societies selected for participation contain a disproportionately large number of otolaryngologists. The opinions presented in our study also favor the thoughts of those in academic practice, although one must also consider that the severity of traumas necessary to produce frontal sinus fractures will likely result in care being provided at a tertiary care center with an academic association. The clinical scenarios in our survey are closed-ended to limit answer variability, but these can be subject to misinterpretations. This may result in inaccurate responses and limit this survey's ability to capture the current climate of frontal sinus fracture management.
Despite these limitations, the comments from surgical specialists collected in this survey recognize that there has been a paradigm shift toward the utilization of high-resolution CT and endoscopes to perform primary and rescue operations for frontal sinus fractures. Our findings demonstrate the need for objective data points that are reflective of these opinions and would benefit from a multi-institutional study, given the low frequency of frontal sinus fractures. Prospective studies can also be performed to provide comparative data against the currently available retrospective data to assess if the benefits of endoscopic management of frontal sinus fractures are clinically significant.
Conclusion
A surgical team with experience in both open CMF and endoscopic techniques is needed to achieve excellent results for patients presenting with frontal sinus fractures. Our cross-sectional survey among multiple specialties demonstrates an evolution in the practice patterns of frontal sinus fracture management compared with previously published surveys. Observation is espoused by all specialties for nondisplaced fractures of the FSOT. Management of displaced fractures through the FSOT is dependent on the presence of concomitant injuries. Conservative measures with observation or FESS are suggested by all specialties for displaced FSOT fracture. Obliteration is favored by PS and OMFS when displaced FSOT fractures are present with AT fractures requiring surgical repair. ORIF is favored by those with training in otolaryngology. The advent of FESS appears to influence the decision tree in managing fractures to the frontal sinus across all surgical specialties. These findings would benefit from objective data to corroborate the current opinions noted in our survey.
References
- 1.Nahum A M. The biomechanics of maxillofacial trauma. Clin Plast Surg. 1975;2(1):59–64. [PubMed] [Google Scholar]
- 2.Strong E B, Pahlavan N, Saito D. Frontal sinus fractures: a 28-year retrospective review. Otolaryngol Head Neck Surg. 2006;135(5):774–779. doi: 10.1016/j.otohns.2006.03.043. [DOI] [PubMed] [Google Scholar]
- 3.Gonty A A Marciani R D Adornato D C Management of frontal sinus fractures: a review of 33 cases J Oral Maxillofac Surg 1999574372–379., discussion 380–381 [DOI] [PubMed] [Google Scholar]
- 4.Olson E M, Wright D L, Hoffman H T, Hoyt D B, Tien R D. Frontal sinus fractures: evaluation of CT scans in 132 patients. AJNR Am J Neuroradiol. 1992;13(3):897–902. [PMC free article] [PubMed] [Google Scholar]
- 5.Rohrich R J, Hollier L H. Management of frontal sinus fractures. Changing concepts. Clin Plast Surg. 1992;19(1):219–232. [PubMed] [Google Scholar]
- 6.Wallis A Donald P J Frontal sinus fractures: a review of 72 cases Laryngoscope 198898; (6, Pt 1):593–598. [DOI] [PubMed] [Google Scholar]
- 7.Weber S C, Cohn A M. Fracture of the frontal sinus in children. Arch Otolaryngol. 1977;103(4):241–244. doi: 10.1001/archotol.1977.00780210097014. [DOI] [PubMed] [Google Scholar]
- 8.Jain S A, Manchio J V, Weinzweig J. Role of the sagittal view of computed tomography in evaluation of the nasofrontal ducts in frontal sinus fractures. J Craniofac Surg. 2010;21(6):1670–1673. doi: 10.1097/SCS.0b013e3181f3c5f1. [DOI] [PubMed] [Google Scholar]
- 9.Guy W M, Brissett A E. Contemporary management of traumatic fractures of the frontal sinus. Otolaryngol Clin North Am. 2013;46(5):733–748. doi: 10.1016/j.otc.2013.07.005. [DOI] [PubMed] [Google Scholar]
- 10.Kellman R, Goyal P. Managing the frontal sinus in the endoscopic age: has the endoscope changed the algorithm? Craniomaxillofac Trauma Reconstr. 2014;7(3):203–212. doi: 10.1055/s-0034-1371773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pawar S S, Rhee J S. Frontal sinus and naso-orbital-ethmoid fractures. JAMA Facial Plast Surg. 2014;16(4):284–289. doi: 10.1001/jamafacial.2014.14. [DOI] [PubMed] [Google Scholar]
- 12.Smith T L, Han J K, Loehrl T A, Rhee J S. Endoscopic management of the frontal recess in frontal sinus fractures: a shift in the paradigm? Laryngoscope. 2002;112(5):784–790. doi: 10.1097/00005537-200205000-00004. [DOI] [PubMed] [Google Scholar]
- 13.Chaaban M R, Conger B, Riley K O, Woodworth B A. Transnasal endoscopic repair of posterior table fractures. Otolaryngol Head Neck Surg. 2012;147(6):1142–1147. doi: 10.1177/0194599812462547. [DOI] [PubMed] [Google Scholar]
- 14.Yoo M H, Kim J S, Song H M, Lee B J, Jang Y J. Endoscopic transnasal reduction of an anterior table frontal sinus fracture: technical note. Int J Oral Maxillofac Surg. 2008;37(6):573–575. doi: 10.1016/j.ijom.2008.03.010. [DOI] [PubMed] [Google Scholar]
- 15.Gould J, Alexander I, Tomkin E, Brodner D. In-office, multisinus balloon dilation: 1-Year outcomes from a prospective, multicenter, open label trial. Am J Rhinol Allergy. 2014;28(2):156–163. doi: 10.2500/ajra.2014.28.4043. [DOI] [PubMed] [Google Scholar]
- 16.Chandra R K, Kern R C, Cutler J L, Welch K C, Russell P T. REMODEL larger cohort with long-term outcomes and meta-analysis of standalone balloon dilation studies. Laryngoscope. 2016;126(1):44–50. doi: 10.1002/lary.25507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bhandarkar N D, Smith T L. Revision frontal sinusotomy using stepwise balloon dilation and powered instrumentation. Laryngoscope. 2010;120(10):2015–2017. doi: 10.1002/lary.21110. [DOI] [PubMed] [Google Scholar]
- 18.Hueman K, Eller R. Reduction of anterior frontal sinus fracture involving the frontal outflow tract using balloon sinuplasty. Otolaryngol Head Neck Surg. 2008;139(1):170–171. doi: 10.1016/j.otohns.2008.02.003. [DOI] [PubMed] [Google Scholar]
- 19.Egemen O, Özkaya Ö, Aksan T, Bingöl D, Akan M. Endoscopic repair of isolated anterior table frontal sinus fractures without fixation. J Craniofac Surg. 2013;24(4):1357–1360. doi: 10.1097/SCS.0b013e3182902518. [DOI] [PubMed] [Google Scholar]
- 20.Bhavana K, Kumar R, Keshri A, Aggarwal S. Minimally invasive technique for repairing CSF leaks due to defects of posterior table of frontal sinus. J Neurol Surg B Skull Base. 2014;75(3):183–186. doi: 10.1055/s-0033-1363503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hoddinott S N, Bass M J. The Dillman total design survey method. Can Fam Physician. 1986;32:2366–2368. [PMC free article] [PubMed] [Google Scholar]
- 22.Harris P A, Taylor R, Thielke R, Payne J, Gonzalez N, Conde J G. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Newman M H, Travis L W. Frontal sinus fractures. Laryngoscope. 1973;83(8):1281–1292. doi: 10.1288/00005537-197308000-00012. [DOI] [PubMed] [Google Scholar]
- 24.Gruss J S. Complex nasoethmoid-orbital and midfacial fractures: role of craniofacial surgical techniques and immediate bone grafting. Ann Plast Surg. 1986;17(5):377–390. doi: 10.1097/00000637-198611000-00005. [DOI] [PubMed] [Google Scholar]
- 25.Thaller S R, Kawamoto H K. Care of maxillofacial injuries: survey of plastic surgeons. Plast Reconstr Surg. 1992;90(4):562–567. doi: 10.1097/00006534-199210000-00003. [DOI] [PubMed] [Google Scholar]
- 26.Donald P J. The tenacity of the frontal sinus mucosa. Otolaryngol Head Neck Surg (1979) 1979;87(5):557–566. doi: 10.1177/019459987908700502. [DOI] [PubMed] [Google Scholar]
- 27.Hybels R L, Weimert T A. Evaluation of frontal sinus fractures. Arch Otolaryngol. 1979;105(5):275–276. doi: 10.1001/archotol.1979.00790170045012. [DOI] [PubMed] [Google Scholar]
- 28.Donald P J, Ettin M. The safety of frontal sinus fat obliteration when sinus walls are missing. Laryngoscope. 1986;96(2):190–193. doi: 10.1288/00005537-198602000-00011. [DOI] [PubMed] [Google Scholar]
- 29.Emara T A, Elnashar I S, Omara T A, Basha W M, Anany A M. Frontal sinus fractures with suspected outflow tract obstruction: a new approach for sinus preservation. J Craniomaxillofac Surg. 2015;43(1):1–6. doi: 10.1016/j.jcms.2014.09.013. [DOI] [PubMed] [Google Scholar]
- 30.Rodriguez E D, Stanwix M G, Nam A J. et al. Twenty-six-year experience treating frontal sinus fractures: a novel algorithm based on anatomical fracture pattern and failure of conventional techniques. Plast Reconstr Surg. 2008;122(6):1850–1866. doi: 10.1097/PRS.0b013e31818d58ba. [DOI] [PubMed] [Google Scholar]
- 31.Yakirevitch A, Bedrin L, Alon E E, Yoffe T, Wolf M, Yahalom R. Relation between preoperative computed tomographic criteria of injury to the nasofrontal outflow tract and operative findings in fractures of the frontal sinus. Br J Oral Maxillofac Surg. 2013;51(8):799–802. doi: 10.1016/j.bjoms.2013.06.001. [DOI] [PubMed] [Google Scholar]
- 32.Stanwix M G, Nam A J, Manson P N, Mirvis S, Rodriguez E D. Critical computed tomographic diagnostic criteria for frontal sinus fractures. J Oral Maxillofac Surg. 2010;68(11):2714–2722. doi: 10.1016/j.joms.2010.05.019. [DOI] [PubMed] [Google Scholar]
- 33.Loevner L A, Yousem D M, Lanza D C, Kennedy D W, Goldberg A N. MR evaluation of frontal sinus osteoplastic flaps with autogenous fat grafts. AJNR Am J Neuroradiol. 1995;16(8):1721–1726. [PMC free article] [PubMed] [Google Scholar]
- 34.Seiden A M, Stankiewicz J A. Frontal sinus surgery: the state of the art. Am J Otolaryngol. 1998;19(3):183–193. doi: 10.1016/s0196-0709(98)90086-2. [DOI] [PubMed] [Google Scholar]
- 35.Laskin D M, Best A M. Current trends in the treatment of maxillofacial injuries in the United States. J Oral Maxillofac Surg. 1988;46(7):595–602. doi: 10.1016/0278-2391(88)90151-6. [DOI] [PubMed] [Google Scholar]


