Abstract
Objectives
Practicing antimicrobial stewardship in nursing homes faces many challenges, particularly in non-academic settings. We sought to identify features of community nursing home environments that are associated with lower rates of overall antibiotic use.
Design
In this pilot study, we used an explanatory sequential design that incorporated comparative feedback about antibiotic use to inform a discussion about antimicrobial stewardship practices among community nursing homes.
Measurements
For the quantitative phase, we measured the number of antibiotic prescriptions, length of therapy and days of therapy/1000 days of care at 6 nursing homes. For the qualitative phase, we conducted semi-structured interviews with healthcare workers in leadership positions at 5 community nursing homes. Transcripts from the recorded interviews were assessed using emergent thematic analysis. For the triangulation phase, we evaluated themes from the semi-structured interviews in the context of each NHs antibiotic use.
Results
The number of antibiotic prescriptions ranged from 172 to 1244, with 50% to 83% written for ≤ 7 days. All nursing homes reported a similar proportion of fluoroquinolone use (27–32% days of therapy). Triangulation yielded 6 themes for which the environment at each facility ranged from less to more supportive antimicrobial stewardship: practice patterns, external influences, infection control, leadership, communication and facility culture. All nursing homes reported pressure from well-intentioned family members to prescribe antibiotics. Nursing homes with shorter lengths of therapy and lower overall antibiotic use were consonant with an environment more supportive of antimicrobial stewardship.
Conclusion
Our findings suggest several features of nursing homes that are supportive of antimicrobial stewardship: practice patterns grounded in established diagnostic criteria, proactive infection control and prevention, open communication and interconnectedness among staff.
Keywords: nursing home, infectious diseases, antimicrobial stewardship, semi-structured interview, fluoroquinolones
Introduction
Only a limited number of studies describe successful antimicrobial stewardship in nursing homes (NHs) [1,2], usually in government or academic settings [3,4]. Little is known about antimicrobial use patterns in community NHs and how that use corresponds with current engagement in antimicrobial stewardship practices. We hypothesized that NHs with more judicious antibiotic use would have an environment more favorable towards antimicrobial stewardship compared to NHs with less judicious antibiotic use. To test this hypothesis, we conducted a pilot study using a mixed methods approach to explore the qualitative views of NH leadership about antimicrobial stewardship in the context of quantitative data that compared antibiotic use among the NHs.
Methods
Study design
We used an explanatory sequential design, beginning with a quantitative phase measuring NH antibiotic use, followed by a qualitative phase comprised of semi-structured interviews of NH leadership that included comparative feedback about antibiotic use. The final component was a triangulation phase that evaluated themes from the semi-structured interviews within the context of each NH’s antibiotic use [7]. For the purposes of testing the feasibility of this approach, the intended sample size for this pilot study was 4 NHs with 2 people from each NH participating in the semi-structured interviews. The Institutional Review Board (IRB) at the corresponding author’s institution approved the research protocol.
NHs were recruited via the Association for Professionals in Infection Control and Epidemiology (APIC) member list-serve as well as personal contacts with individual facilities. The NHs that agreed to participate supplied their antibiotic prescriptions and census data for 2013. We obtained additional NH characteristics from CMS’s Nursing Home Compare [5].
Antibiotic Prescriptions
Each NH supplied prescription data obtained through their pharmaceutical vendor in a unique, unstructured format. After cleaning and transforming the data into a standard and consistent dataset, we determined the number of prescriptions and length of therapy for systemic antibiotics. Antibiotics were grouped based on their pharmacological class or subclass. The major classes were penicillins, β-lactam/ β-lactam inhibitor combinations, first-generation cephalosporins, second- or later- generation cephalosporins, fluoroquinolones, macrolides, metronidazole, tetracyclines, nitrofurantoin, and sulfamethoxazole and/or trimethoprim. The oral and intravenous forms of the glycopeptide, vancomycin, have clinically distinct indications and were thus considered separately. Census data from each facility permitted calculations of days of therapy per 1000 resident days of care (DOT/1000 DOC).
Comparative Feedback & Semi-Structured Interviews
Each session began with a pre-interview followed by the semi-structured interview. The pre-interview, grounded in the cognitive interview approach, familiarized participants with all the survey components and primed them to respond with feelings [6]. The semi-structured interviews asked participants to respond to de-identified tables and figures comparing antibiotic use among 6 participating NHs (Supplementary Text S1). The participants only knew the identity of their facility. The interviewer (RJ), who was not blinded, used an appreciative inquiry approach [7] to ask participants pre-determined open-ended questions and to immediately follow up on new ideas that emerged within the dynamic of the interview.
Thematic Framework Analysis and Triangulation
Interviews were analyzed using a thematic framework approach designed to identify emergent themes [8]. Briefly, two raters independently coded and grouped the interview content and then collaboratively charted their findings (RC, MM). Discrepancies were discussed and the framework revised until there was a shared understanding of theme definitions and inter-rater agreement. For triangulation, we developed an informational matrix to assess the responses from each emergent qualitative theme within the context of the quantitative antibiotic prescription data, including the number of antibiotic prescriptions, length of therapy and overall rate of antibiotic use (DOT/1000 DOC) (RC, RJ) [9,10].
Results
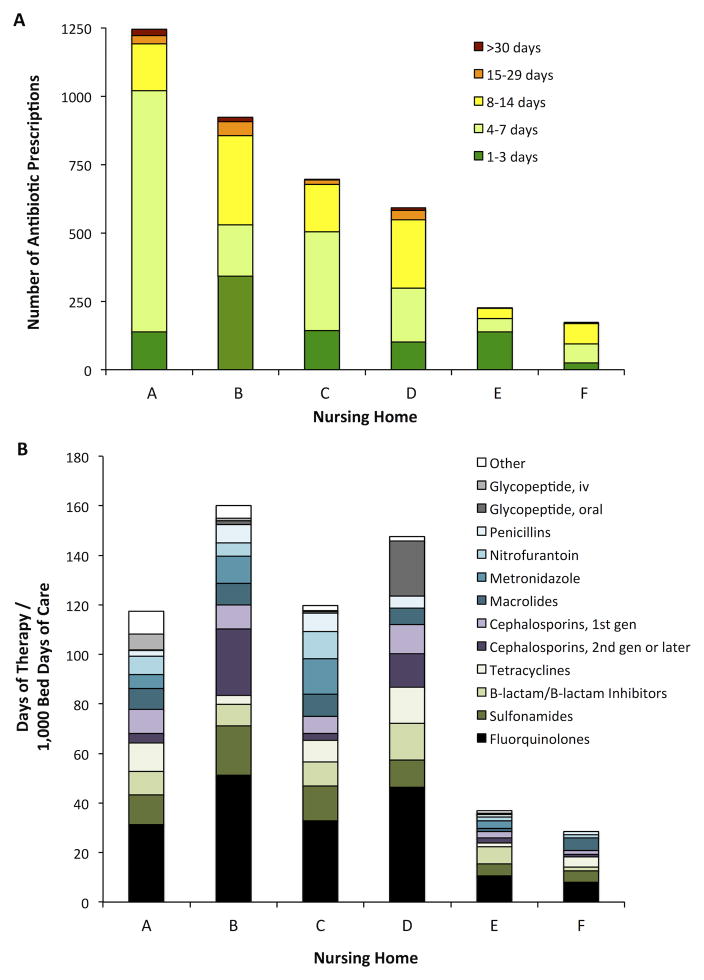
Among the 8 NHs that expressed interest in participating, 6 provided antibiotic prescription data (Supplementary Table S1). Figure 1 shows the total number of antibiotic prescriptions, categorized by length of therapy, and rates of antibiotic use at each NH. The majority of the antibiotic prescriptions were for 7 or fewer days. Fluoroquinolones were the most frequently administered antibiotic, ranging from 27–32% of DOT/1000 DOC.
Figure 1.
Antibiotic use at 6 community nursing homes in 2013. A. Total number of antibiotic prescriptions, stratified by length of therapy. B. Rates of antibiotic use, grouped by pharmacological class. Antibiotics grouped as Other include the following classes (or agents): aminoglycosides, monobactam (aztreonam), carbapenems, lipopeptide (daptomycin), macrocyclic (fidaxomycin), fosfomycin, and rifamycins. B-lactam is beta-lactam; gen is generation; iv is intravenous.
For the qualitative phase, at least 1 staff member from each facility participated in a semi-structured interview (Supplementary Text S1), with the exception of NH A. The participants’ comments portrayed their NHs along a spectrum of less to more supportive of antimicrobial stewardship principles. The interviews revealed 6 themes describing antimicrobial stewardship in NHs (Table 1 and Supplementary Table S2).
Table 1.
Illustrative Quotations from Semi-Structured Interviews of Nursing Home Leadership
| Theme | Illustrative Quotationsa | |
|---|---|---|
| Less Supportive of Antimicrobial Stewardship | More Supportive of Antimicrobial Stewardship | |
| Practice Patterns | ||
| “I wonder if it’s just a knee jerk response anytime someone says this resident’s more confused today and they just automatically start antibiotics for a UTI. I’m not sure that we’re always treating appropriately.” (NH B) | “We went to the McGeer criteria, hung them up everywhere in the nursing station, so the nurses weren’t calling about inappropriate things, especially the UTIs. That made a huge drop in our UTIs.” (NH E) | |
| External Influences | ||
| “It’s very frustrating. I’ll send someone…to the emergency department for chest pains. They get a diagnosis of UTI. I think it feeds the family problem because every time they go to the ED…the ED says they’re diagnosed with a UTI.” (NH F) | “I’ve seen eventually the family builds trust in the physicians here” (NH F) | |
| Infection Control | ||
| “I’m not happy going and making my rounds in this facility that has all these germs running around and they don’t seem to be trying to track it or see who’s developing it or trying to contain it in any way. They haven’t isolated people. They do put C. diff patients in their own room. They didn’t do that up until the last year. (NH D) | “We are kind of strict with isolation. The state isn’t always very happy with it, but once someone is coughing and has a fever, they don’t leave their room. When the flu season starts, we’re very strict on visiting and that, not to visit when you’re sick.” (NH F) | |
| Leadership | ||
| “One thing I’d like to do is take the McGeer criteria and say these are the things that you should be looking for if someone has an infection [but] it always seems like there’s something else [the staff] needs to be learning before that.” (NH B) | “We do at least 1 to 2 [training sessions] a month on all different topics for the STNAs. If we have something unusual develop, we will in-service the staff. If we bring something into the building that the staff isn’t familiar with, we in-service the staff on that as well.” (NH F). | |
| Communication | ||
| “We have a little document that the nurse’s aide can write on and give to the nurse and also give to the manager. They don’t always use that.” (NH B) | “We talk a lot about [patient care]. There’s actually communication on what’s happening with this resident and what else could we possibly do.” (NH E). | |
| Facility Culture | ||
| “Are we doing what’s best for our patients or are we just following orders because somebody said this is what you need to do?” (NH C) | “Our regular doctors are great. Sometimes the on-call doctors, just because they don’t know the residents and they don’t know the staff, it’s not that good relationship. But the doctors that we have here, the nurses aren’t afraid to talk to them.” (NH E) | |
UTI, urinary tract infection; ED, emergency department; STNA, state tested nursing assistant.
Theme 1: Practice Patterns
We defined practice patterns as responses to changes in a resident’s clinical status, including decisions about ordering diagnostic tests and medical treatments such as antibiotics. Practice patterns less supportive of antibiotic stewardship included: little use of established criteria to order diagnostic studies or to start antibiotics (NHs B, C, D); starting antibiotics based on a urinalysis or urine culture rather than on symptoms (NH D); no trial of watchful waiting or hydration in residents with non-specific symptoms (NH B); no post-prescription reassessment based on culture results or response to treatment (NHs B, E); a greater likelihood to prescribe antibiotics for cultures growing multi-drug resistant organisms (NH C); and use of antibiotics for months to prophylax or suppress urinary tract infections (NH D).
Practice patterns more supportive of antibiotic stewardship took the form of those applicable to NHs and to general practice. NH-specific practice patterns included education of nurses leading to practice changes (NH C), nurse- or pharmacist-initiated review of antibiotic prescriptions for >30 days (NH C), having only NH-experienced providers take call (NH E), awareness of NH medical providers’ residents and their expectations for care (NH F), and established communication between the NH and the hospital, such as a shared electronic medical record and a collegial relationship among providers (NH E). Generalized practice patterns included: using established criteria to assess for symptoms of infection (NH E) [11,12], responding to non-specific symptoms with supportive measures such as hydration or cough syrup (NHs B, D), writing shorter antibiotic courses (NHs C, E), incorporating the results of diagnostic tests to adjust antibiotics (NHs D, F) and offering feedback to providers about their antibiotic use (NH C).
Theme 2: External Influences
We defined external influences as factors and people outside of the NH that directly affect residents’ care. Described by NHs B–F, pressure from family members to prescribe antibiotics was the most notable external influence. Participants from NH F indicated that specialists and emergency department physicians also faced pressure from family members. Participants from NHs C, E and F indicated that their NH staff could, at times, influence family members to avoid unnecessary antibiotics. A specific example given by NH F was teaching families that a negative urinalysis ruled out infection.
Theme 3: Infection Control & Prevention
We defined infection control and prevention as systematic efforts by the NH to minimize transmission of pathogens among residents and NH staff. Infection control and prevention strategies less supportive of antimicrobial stewardship included lack of routine surveillance practices to monitor rates of healthcare-acquired infections (NHs C, D), and, as described by interview participants, slow responses to viral outbreaks (NH D) and lack of experience and education about fundamental infection control practices (NHs B, D).
Infection control and prevention strategies more supportive of antimicrobial stewardship involved proactive approaches, including protocols for initiating and removing contact precautions (NHs C, F) and active surveillance for multiple drug resistant organisms (MDROs) and Clostridium difficile (NHs D, E, F). NH F reported placing their residents in isolation as soon as they suspected C. difficile infection rather than waiting for a laboratory result. NH F also developed a protocol such that residents under contact precautions received physical and occupational therapy at the end of the day, permitting a thorough disinfection of shared equipment. NH E stressed resident hand-hygiene and restricted visitors during both influenza season and a norovirus outbreak to minimize the risk of visitors becoming sick.
Theme 4: Leadership
We considered leadership as the priority given to and the dedication of resources for activities supportive of antimicrobial stewardship. Most of these activities centered on providing resources to support infection control and prevention. Leadership less supportive of antimicrobial stewardship provided the minimum federally mandated education for staff (i.e., upon hire and annually) and did not set institutional expectations for standards of care regarding hand hygiene or documentation of changes in clinical status (NHs B, D). Participants reported that leadership at NHs B and D did not support development of protocols to use during outbreaks of infection, largely due to other needs perceived as higher priority. Leadership more supportive of antimicrobial stewardship promoted frequent education for nurses and nurse aides (NHs E, F), using monthly in-service sessions to review important topics like hand washing (NHs E, F) as well as addressing new concerns (NHs D, E, F). Additionally, leadership at NHs E and F stressed the importance of staff longevity and reducing aide turnover as a way to maintain an institutional culture supportive of antimicrobial stewardship.
Theme 5: Communication
We characterized communication as defined, tangible means to share and receive information between and among nursing home staff. Communication less supportive of antimicrobial stewardship relied upon clinical notes to convey information among staff. Among NHs B, C and D, use of forms, including handwritten notes and templates within an electronic medical record, led to breakdowns and gaps in communication. Additionally, the absence of feedback to staff about facility measures such as antibiotic use (NH C and D), infection rates or changes in policies pertaining to infection control (NHs D and F) did not support antimicrobial stewardship. Participants who described communication more supportive of antimicrobial stewardship highlighted scheduled interdisciplinary meetings. The frequency varied, from monthly (NH B) to daily reports (NHs D, E and F) to discuss residents and develop plans to address symptoms as a means to forestall initiating antibiotics. Furthermore, communication was multi-modal, involving forms, phone calls, faxes, email and texting when providers were not available in person (NHs E and F).
Theme 6: Facility Culture
We characterized facility culture as interconnectedness among providers, nurses, nurse aids, family members and other staff. Facility cultures less supportive of antimicrobial stewardship suggested a staff hierarchy characterized by a lack of rapport among personnel at different seniority levels, perpetuated by a desire to avoid conflict. At NHs B, C and D, participants reported considerable apprehension among nurses to question physicians and nurse practitioners. At NH D, this apprehension sometimes manifested as nurses reluctant to educate families about potentially inappropriate antibiotic use, most commonly for asymptomatic bacteriuria. Facility cultures more supportive of antimicrobial stewardship revealed a less hierarchal organizational structure among different disciplines (NHs E and F), characterized by a strong voice for nurses to share their views about resident care and providers who are receptive to discussion. This extended to providers and nurses providing consistent information to family members about risks associated with antibiotics.
Discussion
Our pilot study used comparative feedback, an effective means to improve healthcare practice [13,14], to inform a qualitative assessment of barriers and facilitators to antimicrobial stewardship perceived by NH staff members. Comparative feedback about antibiotic use combined with thematic analysis was an important and, to our knowledge, novel component of our pilot study. Our findings suggest that NHs with lower rates of antibiotic use have a different culture than NHs with higher rates of antibiotic use. Features of NHs that appear supportive of antimicrobial stewardship include practice patterns grounded in established diagnostic criteria, proactive infection control, communication among team members and interconnectedness among staff.
In Table 2, we intercalate our findings with 5 indicators of nursing homes ready for change [15], categorized into philosophy of care or task-oriented [16]. These echo the Centers for Disease Control and Prevention’s (CDC’s) Core Elements for Antibiotic Stewardship in Nursing Homes [17]. Task-oriented activities, such as recording the attendance and frequency of in-service training about signs and symptoms of infection or determining rates of antibiotics prescribed for infections that do not meet the Loeb minimum criteria [12], lend themselves to quantitative measures and are likely to lead to positive outcomes [16]. Such activities may support the efforts of NHs to demonstrate their compliance with antimicrobial stewardship principles in the Conditions of Participation recently announced by the Centers for Medicare and Medicaid Services (CMS) [18].
Table 2.
Activities at Nursing Homes Supportive of Antimicrobial Stewardship
| Category | Indicatorsa | Activities |
|---|---|---|
| Philosophy of Care | ||
| Leadership engagement and commitment | ||
|
||
| Ownership and sense of responsibility by all staff | ||
|
||
| Task Oriented | ||
| Ongoing education activities for all staff | ||
|
||
| Regularly share process measures with all staff | ||
|
||
| Compare outcomes to that of other NHsb | ||
|
||
As detailed in reference [15].
While comparative feedback about antibiotic use is not yet feasible for most NHs, the CDC’s National Healthcare Safety Network has a long-term care component to help assess progress towards national healthcare-associated infection goals.
A meta-synthesis of qualitative studies reported that external pressure from family members contributes to increased antibiotic prescriptions [19]. Our study expands upon these findings in two ways. First, the interview participants reported that outside providers, including specialists and emergency room providers, may prescribe antibiotics for NH residents in the absence of signs and symptoms suggestive of infection or give in to pressure to treat from well-intentioned family members. These actions may impede NHs’ attempts to avoid antibiotic prescriptions for non-specific criteria, like confusion or cloudy or foul-smelling urine [20,21]. Second, NHs with lower rates of antimicrobial use detailed their often successful and united efforts among nursing and providers to educate family members about asymptomatic bacteriuria.
All of the interview participants introduced the topic of infection control and prevention as an aspect of antimicrobial stewardship [22]. NHs with lower rates of antimicrobial use reported using surveillance criteria to monitor their rates of infection and to improve care. Compared to NHs with higher rates of antimicrobial use, in which the discussion of infection prevention and control efforts focused on regulatory concerns, NHs more supportive of antimicrobial stewardship communicated a proactive approach balanced with a concern for maintaining a home-like environment [23].
Furthermore, the themes of communication, facility culture and leadership presented here expand upon previous findings that nurses strongly influence antibiotic prescribing and infection management [19]. Fleming et al. noted that the quality of the communication between nurses and physicians may affect the quality of residents’ care [19]. We found that NHs with a more hierarchical culture, in which nurses avoided conflict, had higher rates of antibiotic use compared to NHs that encouraged routine communication among a multi-disciplinary team.
Our study has several limitations. First, the sample size is small, with antibiotic data from 6 NHs and 11 interview participants from the clinical leadership of 5 NHs. The constraint of a small number of participants and narrow spectrum of roles may limit generalizability of our findings. Second, the participating NHs varied in size, location and population. Although dissimilar in some respects, the NHs were all community-based and did not have academic affiliates. The in-depth examination of the interview participants’ portrayal of their NHs allowed detection of emergent themes common to the 5 participating facilities. Third, the NHs provided antibiotic data using different formats. Most of the prescription data did not include indications for the antibiotics, precluding interpretations about the appropriate selection, indication and dosage of agents. Furthermore, the data did not permit identification of consecutive antibiotic prescriptions for the same individual. This may have led to an inconsistent underestimation of length of therapy among the NHs.
Despite these limitations, the outcomes suggest specific features of NHs that favor antimicrobial stewardship. The emergent themes merit further exploration as they may suggest targets for interventions to augment antimicrobial stewardship practices at NHs. Finally, comparative feedback using objective quantitative data about antibiotic use among NHs has the potential to validate ongoing antimicrobial stewardship efforts and to identify NHs in need of improvement.
Supplementary Material
Supplementary Table S1: Nursing Home Characteristics
Supplementary Table S2: Additional Illustrative Quotations from Semi-Structured Interviews of Nursing Home Leadership
Supplementary Text S1: Semi-structured Interview Materials
Acknowledgments
Funding Sources: Veterans Affairs healthcare system and the National Institutes of Health
The authors gratefully acknowledge the staff of the participating skilled nursing facilities as well as Steven J. Schweon for assistance with contacting nursing homes. This work was supported in part by funds from the Geriatric Research Education and Clinical Centers (GRECC) in Veterans Integrated Service Network (VISN) 10 (RLPJ) and from the National Institutes of Health (NIH), through the Clinical and Translational Science Collaborative of Cleveland (UL1TR000439) from the National Center for Advancing Translational Sciences (NCATS) component of the NIH and NIH Roadmap for Medical Research (RLPJ). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. RLPJ gratefully acknowledges the T. Franklin Williams Scholarship with funding provided by Atlantic Philanthropies, Inc.; the John A. Hartford Foundation, the Association of Specialty Professors, the Infectious Diseases Society of America and the National Foundation for Infectious Diseases.
Footnotes
Author Contributions: RLPJ designed the research study. RLPJ and RRC obtained, cleaned and analyzed the data. RLPJ and RRC developed and conducted the semi-structured interviews. RRC, RLPJ, and MM analyzed the semi-structured interviews. All authors contributed to drafting and editing the manuscript.
Sponsor’s Role: None
Conflict of Interest: All authors report no conflicts of interest. RLPJ has grant support from Pfizer.
References
- 1.Nicolle LE. Antimicrobial stewardship in long term care facilities: what is effective? Antimicrobial Resistance and Infection Control. 2014;3:6. doi: 10.1186/2047-2994-3-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Crnich CJ, Jump R, Trautner B, Sloane PD, Mody L. Optimizing Antibiotic Stewardship in Nursing Homes: A Narrative Review and Recommendations for Improvement. Drugs Aging. 2015;32:699–716. doi: 10.1007/s40266-015-0292-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jump RLP, Olds DM, Seifi N, et al. Effective Antimicrobial Stewardship in a Long-Term Care Facility through an Infectious Disease Consultation Service: Keeping a LID on Antibiotic Use. Infect Control Hosp Epidemiol. 2012;33:1185–1192. doi: 10.1086/668429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zimmerman S, Sloane PD, Bertrand R, et al. Successfully reducing antibiotic prescribing in nursing homes. J Am Geriatr Soc. 2014;62:907–912. doi: 10.1111/jgs.12784. [DOI] [PubMed] [Google Scholar]
- 5.Medicare.gov. [Accessed 27 June 2014];Nursing Home Compare. Available at: https://www.medicare.gov/nursinghomecompare/search.html.
- 6.Willis G. Cognitive Interviewing. 2455 Teller Road, Thousand Oaks California 91320 United States of America: SAGE Publications, Inc; 2005. [Accessed 20 October 2016]. Available at: http://methods.sagepub.com/book/cognitive-interviewing. [Google Scholar]
- 7.Bushe G. Advances in Appreciative Inquiry as an Organization Development Intervention. Organizational Development Journal. 1995;13:14–22. [Google Scholar]
- 8.Ritchie Jane, Spencer Liz. The qualitative researcher’s companion. SAGE Publications; 2002. Qualitative data analysis for applied policy research; pp. 305–29. Available at: https://us.sagepub.com/en-us/nam/the-qualitative-researchers-companion/book7103#contents. [Google Scholar]
- 9.Boland MR, Rusanov A, So Y, et al. From expert-derived user needs to user-perceived ease of use and usefulness: a two-phase mixed-methods evaluation framework. J Biomed Inform. 2014;52:141–150. doi: 10.1016/j.jbi.2013.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mertens DM, Hesse-Biber S. Triangulation and Mixed Methods Research Provocative Positions. Journal of Mixed Methods Research. 2012;6:75–79. [Google Scholar]
- 11.Stone ND, Ashraf MS, Calder J, et al. Surveillance definitions of infections in long-term care facilities: revisiting the McGeer criteria. Infect Control Hosp Epidemiol. 2012;33:965–977. doi: 10.1086/667743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Loeb M, Bentley DW, Bradley S, et al. Development of minimum criteria for the initiation of antibiotics in residents of long-term-care facilities: results of a consensus conference. Infect Control Hosp Epidemiol. 2001;22:120–124. doi: 10.1086/501875. [DOI] [PubMed] [Google Scholar]
- 13.Ivers N, Jamtvedt G, Flottorp S, et al. Audit and feedback: effects on professional practice and healthcare outcomes. Cochrane Database Syst Rev. 2012;6:CD000259. doi: 10.1002/14651858.CD000259.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Meeker D, Linder JA, Fox CR, et al. Effect of behavioral interventions on inappropriate antibiotic prescribing among primary care practices: A randomized clinical trial. JAMA. 2016;315:562–570. doi: 10.1001/jama.2016.0275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rantz MJ, Zwygart-Stauffacher M, Flesner M, et al. Challenges of Using Quality Improvement Methods in Nursing Homes that ‘Need Improvement’. Journal of the American Medical Directors Association. 2012;13:732–738. doi: 10.1016/j.jamda.2012.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Low L-F, Fletcher J, Goodenough B, et al. A Systematic Review of Interventions to Change Staff Care Practices in Order to Improve Resident Outcomes in Nursing Homes. PLOS ONE. 2015;10:e0140711. doi: 10.1371/journal.pone.0140711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nursing Homes and Assisted Living (LTC) CDC; [Accessed 25 June 2016]. The Core Elements of Antibiotic Stewardship for Nursing Homes. Available at: http://www.cdc.gov/longtermcare/prevention/antibiotic-stewardship.html. [Google Scholar]
- 18.Federal Register. [Accessed 31 August 2016];Medicare and Medicaid Programs; Conditions of Participation: Immunization Standards for Hospitals, Long-Term Care Facilities, and Home Health Agencies. Available at: https://www.federalregister.gov/articles/2002/10/02/02-25096/medicare-and-medicaid-programs-conditions-of-participation-immunization-standards-for-hospitals. [PubMed]
- 19.Fleming A, Bradley C, Cullinan S, Byrne S. Antibiotic Prescribing in Long-Term Care Facilities: A Meta-synthesis of Qualitative Research. Drugs Aging. 2015;32:295–303. doi: 10.1007/s40266-015-0252-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nicolle LE, Bradley S, Colgan R, Rice JC, Schaeffer A, Hooton TM. Infectious Diseases Society of America Guidelines for the Diagnosis and Treatment of Asymptomatic Bacteriuria in Adults. Clinical Infectious Diseases. 2005;40:643–654. doi: 10.1086/427507. [DOI] [PubMed] [Google Scholar]
- 21.Nace DA, Drinka PJ, Crnich CJ. Clinical uncertainties in the approach to long term care residents with possible urinary tract infection. J Am Med Dir Assoc. 2014;15:133–139. doi: 10.1016/j.jamda.2013.11.009. [DOI] [PubMed] [Google Scholar]
- 22.Lim CJ, Kwong M, Stuart RL, et al. Antimicrobial stewardship in residential aged care facilities: need and readiness assessment. BMC Infectious Diseases. 2014;14:410. doi: 10.1186/1471-2334-14-410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mody L, Bradley SF, Huang SS. Keeping the ‘home’ in nursing home: Implications for infection prevention. JAMA Intern Med. 2013;173:853–854. doi: 10.1001/jamainternmed.2013.330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Long-term Care Facilities. NHSN | CDC; [Accessed 17 July 2016]. Available at: http://www.cdc.gov/nhsn/LTC/index.html. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Table S1: Nursing Home Characteristics
Supplementary Table S2: Additional Illustrative Quotations from Semi-Structured Interviews of Nursing Home Leadership
Supplementary Text S1: Semi-structured Interview Materials