Abstract
Background
State policies pertaining to health care provider reporting of perinatal substance use have implications for provider screening and referral behavior, patients’ care-seeking and access to prenatal substance use disorder treatment, and pregnancy and birth outcomes.
Objectives
To characterize specific provisions enacted in state statutes pertaining to mandates that health care providers report perinatal substance use, and to determine the proportion of births occurring in states with such laws.
Methods
We conducted a systematic content analysis of statutes in all U.S. states that mentioned reporting by health care providers of substance use by pregnant women or infants exposed to substances in utero; inter-rater reliability was high. We calculated the number of states, and proportion of U.S. births occurring in states, with processes for mandatory reporting of perinatal substance use to authorities, and substance use disorder treatment provision for individuals who are reported.
Results
Twenty states (corresponding to 31% of births) had laws requiring health care providers to report perinatal substance use to child protective authorities, and four states (18% of births) had laws requiring reporting only when a health care provider believed the substance use was associated with child maltreatment. About half of states (13) with any reporting law had a provision promoting substance use disorder treatment in the perinatal period.
Conclusions
Findings inform the ongoing debate about how health policies may be used to reduce the population burden of perinatal substance use.
INTRODUCTION
Perinatal substance use poses significant risks for pregnancy, delivery, and infant health outcomes, both through biological and behavioral pathways (Behnke, Smith, Committee on Substance Abuse, & Committee on Fetus and Newborn, 2013; Smith et al., 2006). Five percent of U.S. pregnant women self-report use of any illicit substance in the prior 30 days (Substance Abuse and Mental Health Services Administration, 2014). The recent opioid epidemic in the United States has disproportionately affected women of reproductive age with a corresponding increase in the rate of neonatal abstinence syndrome (Centers for Disease Control and Prevention, 2013; Patrick et al., 2012). As such, the question of how governmental action can protect infants from adverse effects of exposure to substance use in the perinatal period has re-emerged on the national agenda.
One response to the problem of perinatal substance use has been the enactment of state laws that require health care providers to report pregnant women who use substances, or infants affected by substance use, to child protective agencies. A federal law known as the Child Abuse Prevention and Treatment Act (CAPTA) requires that, as a condition to receive federal grants for programs to prevent child abuse and neglect, state governments have policies and procedures to require health care providers to report to child protection agencies any cases of child abuse or neglect (Young NK, 2009). CAPTA contains a provision that requires states to have:
“policies and procedures (including appropriate referrals to child protection service systems and for other appropriate services) to address the needs of infants born with and identified as being affected by substance abuse or withdrawal symptoms resulting from prenatal drug exposure, or a Fetal Alcohol Spectrum Disorder, including a requirement that health care providers involved in the delivery or care of such infants notify the child protective services system of the occurrence of such condition in such infants.”
There are conflicting views on whether mandatory reporting policies constitute sound public health policy. Policies promoting substance use disorder treatment and offering long-term social services have been associated with improved outcomes (Lester, Andreozzi, & Appiah, 2004; MacMahon, 1997). However, there is also evidence that policies perceived as punitive by patients and providers discourage prenatal care and substance use disorder treatment (American College of Obstetricians and Gynecologists Committee on Ethics, 2015; Angelotta, Weiss, Angelotta, & Friedman, 2016; Roberts & Nuru-Jeter, 2012).
State laws pertaining to perinatal substance use, and interjurisdictional variation in such laws, are important for several reasons. First, specific provisions in state laws may have a significant influence on provider screening and referral behavior, patients’ care-seeking and access to perinatal substance use disorder treatment, and obstetric and neonatal outcomes (Roberts & Pies, 2011). Second, the U.S. opioid epidemic has opened a window of opportunity for stakeholders seeking to amend or improve health policies pertaining to perinatal substance use. Third, characterization of specific provisions of state laws are necessary for future evaluation of the effects of such policies on substance use disorder treatment or health outcomes. However, little prior research has investigated how state laws address health care provider reporting of perinatal substance use. The objectives of the present study were to characterize specific provisions enacted in state law pertaining to mandates that health care providers report perinatal substance use, and to determine the proportion of births occurring in states with such laws.
METHODS
We conducted a systematic content analysis of statutes in all 50 states and the District of Columbia (hereafter referred to as a state) pertaining to the reporting of perinatal substance use to child protective agencies. The Guttmacher Institute publishes annual reports on state policies that consider substance use during pregnancy to be child abuse, whether states require reporting or testing of prenatal substance use, and what substance use disorder treatment programs are available to states (Guttmacher Institute, 2015). Because we are interested in health policies that have direct implications on health care provided to pregnant and postpartum women with substance use disorders, our study is focused more narrowly on state statutes that require health care providers to report either pregnant women who use substances, or fetuses or infants who are suspected of being exposed to substances.
The LexisNexis database, a searchable repository of law, was used to identify relevant state statutes. To identify additional and newer relevant state statutes, we conducted full-text searches using the following search terms: “pregnancy or pregnant or prenatal or perinatal or infant or neonate” and “controlled substance or drug or abuse” and “health care”. We identified a total of 467 individual provisions, and excluded those that contained our search terms but were not relevant to our study. We excluded the following types of laws as beyond the scope of our study: laws making the production or sale of illicit substances in the presence of children a criminal offense; laws defining parental substance use as child abuse absent a reference to substance use in the perinatal period or in utero exposure; laws pertaining to benefit packages under public health care programs; laws relative to the administration of public health programs or departments; and other laws that contained the search terms but were unrelated to health care reporting provisions. To ensure our search included all relevant statutes, we cross-referenced a document published by the Administration for Children and Families that lists state statutes relating to parental drug use and child abuse (Administration for Children and Families, 2016). A compilation, by state, of excerpts of the text of statutes included in the present study is available online (https://perinatalpolicyresearch.wordpress.com/).
Coding instrument development
We used summative content analysis methods to develop a coding instrument to analyze the content of the public health agency websites (Hsieh & Shannon, 2005). Two authors (MJ, CH) read a small number of the state statutes and met to discuss themes that emerged across multiple states. The study team met and developed a 15-item coding instrument that included codes to capture specific provisions of state laws requiring that health care providers report perinatal substance use. We pilot-tested the coding instrument in a sample of statutes (n=8) for clarity of the codes. After pilot-testing of the instrument was complete, two authors (MJ, CH) coded all content, meeting weekly to adjudicate any coding discrepancies. A third coder then independently coded the statutes to assess reliability of the instrument. To measure inter-rater reliability, we used prevalence- and bias-adjusted Kappa statistics, which provide a measure of inter-rate reliability that is adjusted to assess reliability for binary items where “yes” and “no” values are not evenly distributed (Byrt, Bishop, & Carlin, 1993). Inter-rater reliability was substantial, with prevalence- and bias-adjusted ĸ ranging from 0.56 to 1.00 and mean κ=0.75. (Table 1 in the Supplemental Material shows raw agreement and prevalence- and bias-adjusted κ for each specific item.)
Measures
We first determined whether states had laws requiring health care providers to report perinatal substance use to child protective agencies; whether states had laws requiring reporting of perinatal substance use only when a health care provider believed the substance use was associated with child maltreatment; or whether states did not have a specific law about health care provider reporting of perinatal substance use. (States without a specific law are still required under federal law to have policies or procedures in place to address needs of infants exposed to substances in utero; although these policies might not be enacted by statute or codified in regulations.) Among states that had a specific law pertaining to health care provider reporting of perinatal substance use, we identified the following specific characteristics: whether health care providers are required to report pregnant women, infants, or both; whether toxicology testing or other criteria are required to trigger report; and whether the law makes an exemption for medically indicated substances (e.g., buprenorphine).
Second, the instrument identified consequences of perinatal substance use reporting for health care providers and patients. Among states that had a statute pertaining to health care provider reporting of perinatal substance use, we assessed whether the law grants immunity from civil suits to health care providers who, in good faith, made erroneous reports, and whether the statute includes any penalty for not making required reports. We characterized whether the statute specifies that being reported to child protective agency for perinatal substance use cannot be used to criminally prosecute women, or, conversely, whether the law specifies that substance use in pregnancy is a criminal act.
Third, our instrument identified whether state statutes with mandatory reporting include any provisions related to substance use disorder treatment. We measured whether a statute includes provisions that patients be referred to treatment or if there was funding for a treatment program. Among states with treatment provisions, we assessed whether the treatment is required to be appropriate to the perinatal period and whether provisions were included to help women access treatment. We also measured whether there are punitive measures (involuntary commitment or loss of custody) if women refused or did not complete substance use disorder treatment programs.
Analysis
We present frequencies of states with each specific provision that we identified. To determine the proportion of U.S. births that occur in states with different types of laws pertaining to health care provider reporting of perinatal substance use, we assigned each state a count of births published in U.S. Vital Statistics reports for 2013, the latest year for which data are available (Martin JA, 2015). Proportions were then calculated by dividing the number of births in states with specific policies by the number of U.S. births in all states.
RESULTS
We identified current statutes pertaining to health care provider reporting of perinatal substance use in 24 states. We grouped states into three mutually exclusive categories of the type of law: mandatory reporting statute, reporting only with child maltreatment, and no specific law (Figure 1). Mandatory reporting laws were classified as those that required health care providers to report perinatal substance use to child protective agencies (n=20 states). Statutes requiring reporting only with child maltreatment were classified as those that required health care providers to report perinatal substance use only when such substance use indicated or was associated with child maltreatment (n=4 states). We did not identify specific statutes pertaining to the reporting of perinatal substance use to child protective agencies in the remaining 27 states.
Figure 1. State laws pertaining to health care provider reporting of perinatal substance use.
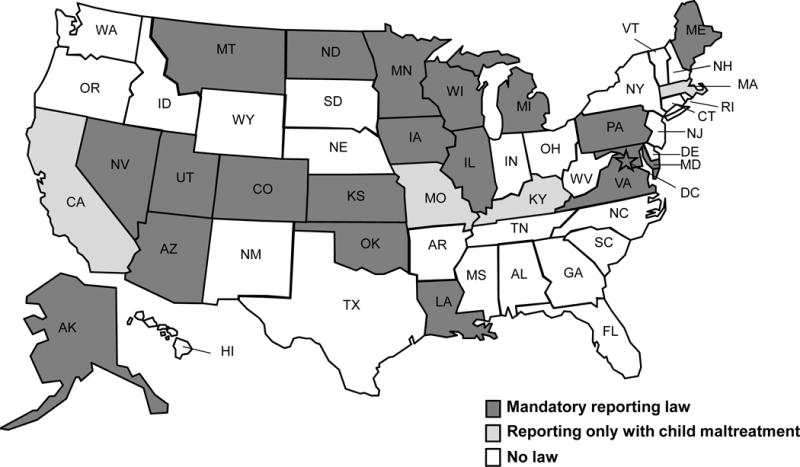
Based on analysis of state statutes in effect through 2015. Arkansas has a law defining in utero substance exposure as neglect but does not have specific provisions related to health care provider reporting of perinatal substance use. Hawaii enacted a mandatory reporting law in 2004 and repealed the law in 2010. South Carolina requires mandatory reporting only when more than one infant born to the same woman have been exposed to substances. Tennessee law criminalizes substance use in pregnancy but does not have specific provisions relating to reporting to child protective agencies.
An estimated 31% of births occur in states with mandatory reporting laws, and an estimated additional 18% of births occur in states requiring reporting only with child maltreatment. Table 1 shows the frequency of specific policies of state reporting laws, with the corresponding percentages of births occurring in states with such policies.
Table 1.
Characteristics of state laws pertaining to health care provider reporting perinatal substance use
| Mandatory reporting law (20 states; 31% of births) | Reporting only with child maltreatment (4 states; 18% of births) | |||
|---|---|---|---|---|
|
| ||||
| No. Statesa | % of birthsb | No. Statesa | % of birthsb | |
| Reporting Policy | ||||
| Pregnant woman is reported | 6 | 11 | 1 | 1 |
| Infant is reported | 19 | 30 | 4 | 17 |
| Toxicology screening is a consideration | 13 | 23 | 3 | 16 |
| Other criteria trigger a report | 17 | 24 | 3 | 5 |
| Treatment exemption for health care providersc | 5 | 8 | 1 | 2 |
| Consequences of Reporting | ||||
| Report cannot be used in criminal prosecution | 2 | 2 | 2 | 3 |
| Liability exemption for health care providersd | 11 | 19 | 2 | 4 |
| Legal penalty for provider’s failure to report | 9 | 18 | 2 | 3 |
| Substance Use Disorder Treatment | ||||
| Any policy promoting treatment in the perinatal period | 11 | 15 | 2 | 14 |
| Specifies that treatment be appropriate for perinatal period | 5 | 9 | 1 | 13 |
| Requires a public agency to support women in obtaining treatment | 5 | 9 | 2 | 14 |
| Allows involuntary commitment related to prenatal substance use | 2 | 3 | 0 | 0 |
| Allows loss of custody related to prenatal substance usee | 3 | 7 | 1 | 1 |
Excludes a mandatory reporting law that was in place in Hawaii from 2006–2010. Excludes South Carolina, which has limited reporting only in certain cases. Excludes Tennessee, which does not have a mandatory reporting law but has a law making substance use in pregnancy a criminal act.
Percentage of births subject to specific laws calculated by dividing state-specific counts of births by the count of all U.S. births, using national vital statistics births data for 2014
Exempts health care providers from reporting perinatal substance use if they are providing healthcare to a substance-using patient
These policies generally specify that health care providers are exempt from civil liability for making false reports if reports are made in good faith
Permit loss of custody of children if women refuse treatment or fail to complete treatment
Reporting Policies
Among the 20 states with a mandatory reporting law, most (19) require health care providers to report infants to child protective agencies, although 6 states require that pregnant women with substance use be reported (7 require reporting of both infants and pregnant women). Thirteen states specify that toxicology results are a trigger for reporting, and 17 states specify, in addition to or separately from toxicology screening, other criteria that would trigger a report, such as physician knowledge of substance use or clinical symptoms in neonates.
Consequences of Reporting
In total, 4 states’ statutes (corresponding to 5% of births) specify that reports of perinatal substance use could not be used as evidence in a criminal prosecution of a woman. Twelve state statutes (corresponding to 22% of births) specify that health care providers who report perinatal substance use to child protective agencies in good faith could not be held legally responsible for false reports. Statutes in 11 states (21% of births) specify a penalty for health care providers’ failure to report known perinatal substance use; typically, it is considered to be a misdemeanor (i.e., a lesser offense).
Substance use Disorder Treatment
The provision of treatment for women who are involved with a report is required in about half of states with reporting laws. Among states with a mandatory reporting law, 11 have statutes that include policies promoting treatment in the perinatal period; among states requiring reporting only with child maltreatment, only 2 have policies promoting treatment. Typical treatment policies require that women be referred to substance use disorder treatment providers. Fewer state statutes specified that such treatment be appropriate for prenatal or postpartum women (5 states with mandatory reporting laws and 1 state with reporting only for child maltreatment). Two states have statutes allowing pregnant women to be involuntarily committed if they refuse or fail substance use disorder treatment; and 4 states have statutes allowing child protective agencies to remove those children of women who refuse or fail substance use disorder treatment.
Time trends in state laws
Figure 2 shows the number of states with mandatory reporting laws or laws requiring reporting only with child maltreatment from 1972 to 2015. The first statutes were enacted in 1973. The number of states with mandatory reporting statutes increased sharply after 2003, after enactment of the federal law requiring states to have policies and procedures protecting infants exposed to substances in utero.
Figure 2. Frequency of states with perinatal substance use reporting laws, 1972–2015.
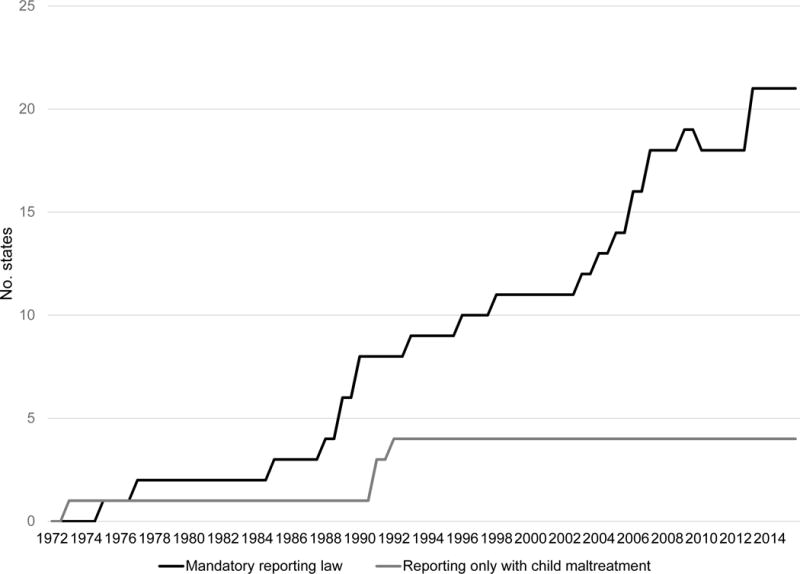
The first such law was enacted in 1973. States were considered to have a specific law if it was in effect at any time during the calendar year. Hawaii enacted a mandatory reporting law in 2004 and repealed the law in 2010.
DISCUSSION
In this national study, we found that approximately half of all U.S. births occur in states with statues mandating that health care providers report perinatal substance use to child welfare authorities. The majority of these births occur in states with statutes requiring mandatory reporting of all cases, while some births occur in states with laws requiring reporting of perinatal substance use only when a health care provider believed the substance use was associated with child maltreatment. While statutes generally required reporting of any substance use, the provision of substance use disorder treatment to women who are the subject of reports was not universally specified in state statutes. Some states have laws imposing punitive measures (involuntary commitment or loss of custody) for refusing or failing to complete substance use disorder treatment. This is the first study, to our knowledge, to characterize specific provisions of these state laws using a reliable instrument.
These findings contribute to the ongoing discussion about how to improve care for substance using pregnant women and neonates, particularly in the midst of the opioid epidemic (Krans & Patrick, 2016). A recent report from an expert Centers for Disease Control and Prevention advisory panel recommends universal screening for substance use at the first prenatal visit, and risk stratification with brief interventions or more intensive specialty care as warranted (Wright et al., 2016). While desirable from a public health perspective, universal screening in the context of punitive state laws poses ethical and moral dilemmas for health care providers. State laws allowing for involuntary commitment for treatment or custody loss solely because of prenatal substance use violate the principles of patient autonomy and beneficence (American College of Obstetricians and Gynecologists Committee on Ethics, 2015). Punitive measures may discourage women from seeking care or disclosing substance use to their health care providers (Chang et al., 2015; Roberts & Pies, 2011).
Our study also raises questions about whether the intent of state reporting statutes is to ensure women receive substance use disorder treatment or to impose punitive measures. Recent, emotional news media coverage of neonatal abstinence syndrome suggested that state laws are not effectively protecting infants who are exposed to opioids in utero (Wilson D, 2015). In response, federal lawmakers have suggested that states should be held more accountable for compliance with CAPTA, which requires states to have policies and procedures in place to meet the needs of substance-exposed infants, as well as to develop plans to ensure infants’ safety and well-being (U.S. House of Representatives Committee on Education and the Workforce, 2016). Such procedures should include access to quality substance use disorder treatment for pregnant and postpartum women, along with other supportive services. However, the fact that only about half of state reporting laws have provisions to facilitate referral or access to substance use disorder treatment for women reported to child protective agencies is concerning. The dearth of policy attention to substance use disorder treatment during the perinatal period is reflected in recent data showing that fewer than 20% of substance use disorder treatment facilities nationally provide specialized care for pregnant or postpartum women, and estimates of unmet need for substance use disorder treatment range from 81% to 95% of women (Terplan, Longinaker, & Appel, 2015). Lack of access to substance use disorder treatment is likely to be amplified in states that have not expanded Medicaid eligibility to all low-income adults. Notably, the recently enacted federal Comprehensive Addiction and Recovery Act of 2016 requires treatment for families and caregivers of infants affected by substance use, and requires states to monitor the provision of such treatment.
Limitations
This study has limitations. First, our analysis included only state statutes to define state laws; therefore, our results should be interpreted only as reflecting state policies that are passed by the legislatures and enacted into law. Regulations promulgated by executive branch agencies and judicial scrutiny that examines perinatal substance use law may define how state statutes are to be interpreted, but our study does not include such provisions. Second, federal law requires states to have policies to address the needs of infants exposed to substances in utero in order to receive certain federal grants, and our results should not be used to determine whether states are in compliance with federal law. Rather, our objective was to characterize specific reporting provisions that affect health care providers, and by extension, their patients. Third, other relevant levels of policy, such as local governmental ordinances or hospital-specific policies, were not included in our analysis, so we are unable to determine within-state variation in perinatal substance use reporting policies that may be present. Fourth, the presence of state statutes requiring health care providers to report perinatal substance use may or may not drive reporting or treatment patterns. Our study is unable to measure the extent to which health care providers are aware of their states’ reporting requirements, or how reporting requirements are monitored or enforced.
Implications for Practice and Policy
The present study has implications for practice, suggesting that health care providers and women with substance use face an array of different statutory requirements depending on their state. Even in states with mandatory reporting of perinatal substance use, there may be room for clinical discretion in who is reported, and when. These considerations may directly affect patient-provider interactions both during prenatal care and during the neonatal period. Notably, prior research has suggested that pregnant women with substance use consider substance use testing and reporting to child protective agencies to be punitive, rather than potentially helpful, procedures (Roberts & Nuru-Jeter, 2010).
Findings also have implications for policy makers seeking to reduce morbidity and mortality associated with substance use. It is not clear that simply enforcing current law is the optimal approach to reduce the burden of perinatal substance use. Our findings suggest that such an approach could lead to large geographic inequities, for example, in women’s exposure to punitive legal consequences such as involuntary commitment for substance use disorder treatment or loss of custody because of substance use. There are also well-documented racial disparities in reporting to child protective agencies (Osterling, D’Andrade, & Austin, 2008) that appear to persist even when hospitals adopt reporting protocols (Roberts, Zahnd, Sufrin, & Armstrong, 2015). Additionally, there is typically fragmentation between medical and social services agencies’ approaches to perinatal substance use (Substance Abuse and Mental Health Services Administration, 2016). Moreover, surprisingly little is known about the availability and effectiveness of interventions provided to families by child protective agencies after a woman or infant has been reported for perinatal substance use. One descriptive study suggests benefits of medical and financial services (McCann et al., 2010). More research is required to elucidate how different state statutes and regulations affect access to substance use disorder treatment in pregnancy and maternal and infant outcomes. Subsequent state and federal law should be developed based on such evidence. One example of the translation of evidence to policy might be the federal law requiring insurance parity in coverage of physical and behavioral health treatments, which was enacted after a wealth of research was conducted on state-specific parity laws (Barry, Huskamp, & Goldman, 2010).
Conclusion
An estimated 49% of U.S. births occur in states with laws requiring health care providers to report pregnant women with substance use or infants exposed to substances in utero, and there is significant variation in specific provisions of reporting laws. Among states that have mandatory reporting laws, the provision of substance use disorder treatment in the perinatal period is not universally specified in law. Findings inform the ongoing debate about how state or federal policies may be used to reduce the population burden of substance use in the perinatal period.
Supplementary Material
Acknowledgments
We thank Alex Carter, BS, and Wyatt Koma for valuable research assistance.
Funding/Support: This research was supported by the Building Interdisciplinary Research Careers in Women’s Health (BIRCWH) Program (K12 HD043441). The funder had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest Disclosures: None of the authors have any conflict of interest to disclose.
References
- Administration for Children and Families. Parental Drug Use as Child Abuse. 2016 Retrieved from https://www.childwelfare.gov/topics/systemwide/laws-policies/statutes/drugexposed/
- American College of Obstetricians and Gynecologists Committee on Ethics. Committee opinion no. 633: Alcohol abuse and other substance use disorders: ethical issues in obstetric and gynecologic practice. Obstet Gynecol. 2015;125(6):1529–1537. doi: 10.1097/01.AOG.0000466371.86393.9b. [DOI] [PubMed] [Google Scholar]
- Angelotta C, Weiss CJ, Angelotta JW, Friedman RA. A Moral or Medical Problem? The Relationship between Legal Penalties and Treatment Practices for Opioid Use Disorders in Pregnant Women. Womens Health Issues. 2016;26(6):595–601. doi: 10.1016/j.whi.2016.09.002. [DOI] [PubMed] [Google Scholar]
- Barry CL, Huskamp HA, Goldman HH. A political history of federal mental health and addiction insurance parity. Milbank Q. 2010;88(3):404–433. doi: 10.1111/j.1468-0009.2010.00605.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Behnke M, Smith VC, Committee on Substance Abuse, & Committee on Fetus and Newborn Prenatal substance abuse: short- and long-term effects on the exposed fetus. Pediatrics. 2013;131(3):e1009–1024. doi: 10.1542/peds.2012-3931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Byrt T, Bishop J, Carlin JB. Bias, prevalence and kappa. J Clin Epidemiol. 1993;46(5):423–429. doi: 10.1016/0895-4356(93)90018-v. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Vital signs: overdoses of prescription opioid pain relievers and other drugs among women–United States, 1999–2010. MMWR Morb Mortal Wkly Rep. 2013;62(26):537–542. [PMC free article] [PubMed] [Google Scholar]
- Chang JC, Holland CL, Tarr JA, Rubio D, Rodriguez KL, Kraemer KL, Arnold RM. Perinatal Illicit Drug and Marijuana Use: An Observational Study Examining Prevalence, Screening, and Disclosure. Am J Health Promot. 2015 doi: 10.4278/ajhp.141215-QUAL-625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guttmacher Institute. Substance Abuse During Pregnancy. 2015 Retrieved from New York, NY; : http://www.guttmacher.org/statecenter/spibs/spib_SADP.pdf.
- Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–1288. doi: 10.1177/1049732305276687. [DOI] [PubMed] [Google Scholar]
- Krans EE, Patrick SW. Opioid Use Disorder in Pregnancy: Health Policy and Practice in the Midst of an Epidemic. Obstet Gynecol. 2016;128(1):4–10. doi: 10.1097/AOG.0000000000001446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lester BM, Andreozzi L, Appiah L. Substance use during pregnancy: time for policy to catch up with research. Harm Reduct J. 2004;1(1):5. doi: 10.1186/1477-7517-1-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacMahon JR. Perinatal substance abuse: the impact of reporting infants to child protective services. Pediatrics. 1997;100(5):E1. doi: 10.1542/peds.100.5.e1. [DOI] [PubMed] [Google Scholar]
- Martin JAHB, Osterman MJK, Curtin SC, Matthews TJ. Births: Final data for 2013. 2015 Retrieved from Hyattsville, MD: [PubMed] [Google Scholar]
- McCann KJ, Twomey JE, Caldwell D, Soave R, Fontaine LA, Lester BM. Services used by perinatal substance-users with child welfare involvement: a descriptive study. Harm Reduct J. 2010;7:19. doi: 10.1186/1477-7517-7-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osterling KL, D’Andrade A, Austin MJ. Understanding and addressing racial/ethnic disproportionality in the front end of the child welfare system. J Evid Based Soc Work. 2008;5(1–2):9–30. doi: 10.1300/J394v05n01_02. [DOI] [PubMed] [Google Scholar]
- Patrick SW, Schumacher RE, Benneyworth BD, Krans EE, McAllister JM, Davis MM. Neonatal abstinence syndrome and associated health care expenditures: United States, 2000–2009. JAMA. 2012;307(18):1934–1940. doi: 10.1001/jama.2012.3951. [DOI] [PubMed] [Google Scholar]
- Roberts SC, Nuru-Jeter A. Women’s perspectives on screening for alcohol and drug use in prenatal care. Womens Health Issues. 2010;20(3):193–200. doi: 10.1016/j.whi.2010.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts SC, Nuru-Jeter A. Universal screening for alcohol and drug use and racial disparities in child protective services reporting. J Behav Health Serv Res. 2012;39(1):3–16. doi: 10.1007/s11414-011-9247-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts SC, Pies C. Complex calculations: how drug use during pregnancy becomes a barrier to prenatal care. Matern Child Health J. 2011;15(3):333–341. doi: 10.1007/s10995-010-0594-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts SC, Zahnd E, Sufrin C, Armstrong MA. Does adopting a prenatal substance use protocol reduce racial disparities in CPS reporting related to maternal drug use? A California case study. J Perinatol. 2015;35(2):146–150. doi: 10.1038/jp.2014.168. [DOI] [PubMed] [Google Scholar]
- Smith LM, LaGasse LL, Derauf C, Grant P, Shah R, Arria A, Lester BM. The infant development, environment, and lifestyle study: effects of prenatal methamphetamine exposure, polydrug exposure, and poverty on intrauterine growth. Pediatrics. 2006;118(3):1149–1156. doi: 10.1542/peds.2005-2564. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results from the 2013 National Survey on Drug Use and Health: Summary of National Findings. 2014 Retrieved from Rockville, MD. [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. A collaborative approach to the treatment of pregnant women with opioid use disoders: Practice and policy considerations for child welfare, collaborating meidcal, and service providers. 2016 Retrieved from https://ncsacw.samhsa.gov/files/Collaborative_Approach_508.pdf.
- Terplan M, Longinaker N, Appel L. Women-Centered Drug Treatment Services and Need in the United States, 2002–2009. Am J Public Health. 2015;105(11):e50–54. doi: 10.2105/AJPH.2015.302821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. House of Representatives Committee on Education and the Workforce. Committee conducts overwight of child abuse prevention policies. 2016 Retrieved from http://edworkforce.house.gov/news/documentsingle.aspx?DocumentID=400097.
- Wilson DSJ (Producer) Newborns die after being sent home with mothers struggling to kick drug addictions. Reuters. 2016 Jul 11; 2015. Retrieved from http://www.reuters.com/investigates/special-report/baby-opioids/
- Wright TE, Terplan M, Ondersma SJ, Boyce C, Yonkers K, Chang G, Creanga AA. The role of screening, brief intervention, and referral to treatment in the perinatal period. Am J Obstet Gynecol. 2016 doi: 10.1016/j.ajog.2016.06.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young NKGS, Otero C, Deniis K, Chang R, Early K, Amatetti S. Substance-Exposed Infants: State Responses to the Problem. 2009 Retrieved from Rockville, MD; : https://www.ncsacw.samhsa.gov/files/Substance-Exposed-Infants.pdf.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


