Abstract
Purpose of review
This review provides historical background on trauma care in the USA and summarizes contemporary trauma-related health policy issues. It is a primer for orthopedic surgeons who want to promote improvements in research, delivery, and cost reduction in trauma care.
Recent findings
As of 2010, funding for trauma research accounted for only 0.02% of all National Institutes of Health research funding. This is disproportionate to the societal burden of traumatic injury, which is the leading cause of death and disability among people aged 1 to 46 years in the USA. The diagnosis-related group model of hospital reimbursement penalizes level-I trauma centers, which typically treat the most severely injured patients. Treatment of traumatic injury at level-I and level-II trauma centers is associated with lower rates of major complications and death compared with treatment at non-trauma centers. Patient proximity to trauma centers has been positively correlated with survival after traumatic injury. Inadequate funding has been cited as a reason for recent closures of trauma centers.
Summary
Orthopedic surgeons have a responsibility to engage in efforts to improve the quality, accessibility, and affordability of trauma care. This can be done by advocating for greater funding for trauma research; choosing the most cost-effective, patient-appropriate orthopedic implants; supporting the implementation of a national trauma system; leading high-quality research of trauma patient outcomes; and advocating for greater accessibility to level-I trauma centers for underserved populations.
Keywords: Disability, Healthcare policy, Injury burden, Orthopedic trauma, Outcome measures
Introduction
In the USA, traumatic injury is the leading cause of death and disability among people aged 1 to 46 years and the fourth leading cause of death overall [1]. By 2020, it is estimated that injuries related to automobile collisions will represent the third largest disease burden globally on the basis of disability-adjusted life-years [2]. In the current healthcare environment, which is changing rapidly, it is important that orthopedic surgeons be familiar with changing healthcare policy, which will uniquely affect not only us as trauma care providers but also the patients we treat. Additionally, as leaders of improvement, it is imperative that we take action and emphasize public advocacy based on data and objective analysis.
Background
Historically, systematic trauma care was associated with armed national conflict and focused on preventing death in the seriously injured; most surgeries consisted of amputations and treatment of soft tissue injuries [3]. The expansion of urban populations, increase in urban violence, a growing population, and the building of more highways result in an increase in the number of trauma patients who need care. Additionally, trauma care has evolved with surgical management directed at achieving optimal functional injury recovery, rather than the previous mainstay of life-saving amputations. With these new goals, as the number of trauma patients being treated grows, so does the cost of treating them [4].
To understand the issues around trauma care policy, one must first understand that trauma centers can exist as single facilities or as part of larger, regional systems that involve coordination of emergency medical services, allocation of assets, and control of patient flow and resources. It is in our interest as a society and a healthcare community to ensure that an infrastructure exists that allows us to care appropriately for injured patients today and into the future. This infrastructure requires skilled and knowledgeable trauma surgeons and care teams, as well as appropriate equipment, communication, collaboration, rehabilitation, and research.
Efforts to balance the need for high-quality, accessible trauma care and the costs required to provide it began in the 1960s, but progress has not been straightforward. Healthcare reform has focused on three core concepts: increasing accessibility, decreasing costs, and implementing mandatory data submission for outcomes-based research. These goals have not changed since the introduction of the concept of a trauma system.
Despite efforts to reach these goals, the number of trauma centers has decreased, reducing access to trauma care and increasing mortality rates in the rural populations that are most affected by these closures. It is important for us as trauma care providers to educate ourselves about healthcare policy decisions currently under debate, as well as those on the horizon. Additionally, we must advocate for our patients while continually evaluating and optimizing the quality of care we provide.
Accessibility
Before the establishment of the Clinical Shock Trauma Research Unit in Baltimore in 1961, there was no organized effort to deliver trauma care to civilians in the USA. As urban areas began to experience increased violence, trauma patients were recognized as a population lacking adequate care. In 1966, the National Academy of Science’s National Research Council released a report entitled Accidental Death and Disability: The Neglected Disease of Modern Society [5]. This report was the impetus for the National Traffic and Motor Vehicle Safety Act of 1966 [6], which provided the first federal financial support for emergency medical services. Professional organizations were established to address the deficiencies in trauma care that led to this “neglected disease.” They established requirements for hospitals to be “qualified” to provide care to the injured, eventually producing the system on which the current American College of Surgeons’ trauma level classification was built [7].
A second report entitled Injury in America: A Continuing Public Health Problem [8] was published in 1985 and served as another catalyst for federal funding of trauma research and care. The report prompted the Trauma Care Systems Planning and Development Act of 1990 [9] and the federally funded Center for Injury Control (now the Injury Control Research Centers, funded by the Centers for Disease Control and Prevention). These centers fund research in all three phases of injury control: prevention, acute care, and rehabilitation. Early research supported the importance of accessibility of trauma care for improved patient outcomes [10]. One study found that being located more than 60 min away from a level-I trauma center was associated with significantly higher odds of dying [11]. Despite this evidence, a recent report of access to acute trauma care in the USA found that nearly 30 million Americans, or 11.7% of the US population in 2010, live more than an hour away from a level-I or level-II trauma center [12••]. The authors found that living far from a trauma center was associated with being uninsured, having low income, and living in a rural area.
As the number of US trauma centers decreases, there has been a concomitant increase in patient mortality rates. A 2014 study of California trauma centers found that trauma patients whose drive time was an average of 47 min to the nearest trauma center had 21% higher odds of inpatient death than patients whose average drive time was 34 min [13•]. This is an important finding considering that in 2007, 69 million Americans had to travel farther to the closest trauma center than they did in 2001 [14].
Accountability
To determine whether the changes implemented after The Accidental Death and Disability report had resulted in improved outcomes for injured patients, Glance, et al. [15] analyzed the outcomes of trauma patients admitted to level-I or level-II trauma centers in Pennsylvania between 2000 and 2009. They found a 30% decline in the adjusted odds ratio for mortality between 2000 to 2001 versus 2008 to 2009; mortality rates were 7.2% (of 32,533 admissions) in 2001 and 5.7% (of 51,223 admissions) in 2009. When stratified by injury severity, declines were 40 to 50%. A similar analysis of level-I trauma centers was conducted in Canada, finding a trend (non-significant) toward lower odds of dying among trauma patients treated at level-I trauma centers compared with those treated at uncategorized hospitals [11]. Analysis of the trauma care delivered between 1996 and 2008 at the R Adams Cowley Shock Trauma Center in Baltimore indicated a significantly higher survival rate after severe trauma compared with predicted probability of survival [16]. Similar survival results were found in Florida and Illinois [17].
To complement assessments of individual trauma centers or trauma systems, a multi-state comparison of mortality rates in ACS-verified level-I trauma centers versus non-trauma centers was conducted [4]; they reported a significantly lower risk of death from trauma when care was provided at a trauma center versus a non-trauma center. The authors argued for continued efforts to establish accessible regional trauma centers. They concluded that establishment of trauma centers (i.e., single hospitals) and systems (i.e., networks of hospitals, emergency medical services, and traffic/triage controls) saved lives.
Trauma survivors often undergo multiple-staged surgeries and frequently experience complications. The Hospital Readmissions Reduction Program was introduced in 2012 to reduce the number of “avoidable readmissions” by focusing on quality of care. This system is intended to hold treating surgeons and hospitals accountable for the quality of care delivered to patients as measured by “avoidable” readmissions. If a hospital is deemed to have a higher-than-expected 30-day readmission rate, it is penalized with a reduction of Medicare payments for all patients [18]. However, “avoidable readmission” is not yet objectively defined, with poor interobserver reliability specifically regarding which readmissions are preventable [19]. A systematic review was conducted to identify the proportion of avoidable readmissions and how “avoidability” is defined [20]; from 34 studies, they found avoidable readmission rates ranging from 5 to 79%. Most studies used a single reviewer to determine whether readmissions were avoidable on the basis of subjective criteria; three studies used combinations of administrative diagnostic codes. Factors shown to be the drivers of variability in 30-day readmissions are related to community resources, patient population, and other variables that are difficult or impossible to change [17]. The centers at higher risk of penalty from preventable readmissions are the “safety net” hospitals (i.e., those that provide care to a high proportion of low-income, uninsured, and Medicaid patients), potentially widening the disparity in medical care available to minority populations [21].
Affordability
Although government efforts were aimed initially at increasing access to healthcare, the development of Medicare and Medicaid programs in 1965 shifted focus toward containing costs with the establishment of health maintenance organizations (HMOs) in 1973 and the introduction of diagnosis-related groups (DRGs) in 1982. Shortly thereafter, federal funding for emergency medical services fell sharply with the Omnibus Budget Reconciliation Act of 1981 [22]. Medicare adjusted hospital reimbursements to increase funding for centers more likely to treat trauma patients who were uninsured or underinsured or who had more comorbidities, as well as to hospitals associated with medical education through the case-mix index, the disproportionate share hospital program, outlier payments, and indirect medical education payments. However, these adjustments dwindled after experiencing a series of cuts [23].
Without system-wide financial support for the care of underinsured trauma patients, trauma centers began closing, creating accessibility challenges. Thirty percent of trauma centers in the USA closed between 1999 and 2005 [13•]. Initially, reasons for the closures were unclear; however, analyses found evidence that insufficient funding was a frequent cause [23]. Hospitals were at higher risk of closure if they had a negative profit margin compared to hospitals without a negative profit margin or if they received below-average Medicare reimbursement compared to hospitals that received at least the average Medicare reimbursement [23]. Compared with hospitals serving a small proportion of racial and ethnic minorities, those serving a high proportion of minorities were at greater risk of closure [23].
The variable most strongly associated with closure was a high concentration of patients insured by HMOs [23]. Medicaid managed care (an HMO) represents 60% of the Medicaid population. The rates of injury in the Medicaid population challenge the economic viability of trauma centers as the proportion of patients insured by HMOs increases.
Before implementing cost reduction measures, it is important to determine the largest sources of costs. Using samples from the Medicare Provider Analysis and Review dataset from 1992 to 2010, areas of the greatest spending, as well as the greatest spending growth in the acute phase, post-acute phase, and recovery phase (30 to 365 days after the index event) in the treatment of heart attack, congestive heart failure, and hip fracture were identified [24]. Spending increased in all three phases between 1994 and 2009, and spending for post-acute services grew the fastest for all three diagnoses. In the treatment of hip fractures, post-acute spending represented 73% of growth in expenditures. Although there was a significant increase in spending during the recovery phase after hip fractures, the authors did not identify an associated improvement in the 1-year survival rate in these patients. In fact, there was an increase in the risk-adjusted 1-year mortality rate for patients with hip fractures, from 23% in 1994 to 27% in 2002. Between 2002 and 2009, the rate declined to 24% from 27% but remained higher than the rate of 23% in 1994. The authors found a 13% increase in the 1-year mortality rate when adjusted for age, race, and sex [24].
In addition to reimbursements, one of the most notable opportunities for cost reduction in orthopedic trauma systems lies in the cost of implants. In the first year after implementing matrix pricing at their hospital, one group reported savings of nearly US$780,000, or 49%, for intramedullary nails alone [25•]. The matrix pricing model establishes one price for a particular procedure with a standard construct. For example, an intramedullary nail construct for a femur fracture could include the guide pin, intramedullary nail, ball-tipped guide wire, lag screw, two distal interlock screws, reamers, and drill bits for a set price. A formal notice of this pricing is sent to vendors, and those willing to accept the mandated pricing are allowed to supply products to the hospital.
DRG reimbursement model
The U.S. Health Care Financing Administration introduced DRGs into the reimbursement system in 1982. In this model, diagnoses are categorized into groups according to the estimated hospital resources required to treat them, resulting in fixed, pre-determined lump-sum reimbursements. If the cost of care exceeds the reimbursement amount, the hospital incurs a deficit. If the cost of care is less than the reimbursement amount, the hospital earns a profit. The incentive for hospitals to reduce costs is inherent in the model. The DRG classification, however, does not consider heterogeneity within diagnostic groups; namely, injury severity and comorbidities. These factors can substantially affect the resources required for appropriate treatment. Within this lump-sum model, trauma centers are at a disadvantage in two ways. First, trauma centers are obligated to treat patients and to seek reimbursement retroactively, unlike providers of elective surgery who obtain insurance preauthorization. Second, the most severely injured patients are typically transported to level-I trauma centers, whereas less severely injured patients within the same DRG are often transported to non-ACS-verified acute care hospitals. Although both types of patient may have similar diagnoses, the cost of treatment is positively correlated with injury severity, potentially penalizing the trauma center and rewarding the non-acute care facility.
Reflections and future endeavors
Traumatic injury accounted for the largest percentage of life-years lost in 2014—more than cancer or heart disease [1]. Studies of single trauma centers or cities that have implemented formal trauma systems have found reductions of up to 50% in the rates of major complications and death when stratified by injury severity [4, 11, 15, 17]. Despite this, funding for trauma research remains far below that for conditions causing less morbidity and death, while the costs associated with fatal and non-fatal trauma continue to increase [26]. In 2013, the costs associated with fatal and non-fatal injuries were US$214 billion and more than US$457 billion, respectively [26]. National Institutes of Health research funding for trauma is far lower than that for cancer and heart disease. Currently, many orthopedic trauma studies are underpowered and arguably unfit to guide the administration or evaluation of orthopedic trauma care [27]. More than 50 years after the National Research Council described injury as the most important health issue facing our nation and identified the dearth of long-term funding for trauma research as “the most significant obstacle at present,”(p33) trauma research funding remains grossly incommensurate with its associated healthcare burden (Fig. 1), receiving only 0.02% of National Institutes of Health research funding [28••]. Had a National Institute of Trauma been established after the National Research Council recommendations, trauma might not be the leading cause of death in those younger than 46 years, and the costs associated with those deaths may not have reached US$214 billion in 2015 [28••]. Implementation of a national trauma system that integrates prevention, acute care, research, performance improvement, and education with the goals of decreasing the death and disability associated with trauma is long overdue.
Fig. 1.
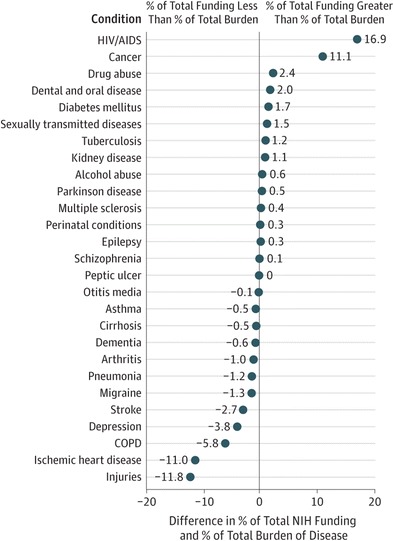
Estimates of National Institutes of Health (NIH) funding for various research, condition, and disease categories showing that trauma research is underfunded compared with other conditions on the basis of disease burden. COPD chronic obstructive pulmonary disease. (Reprinted with permission from Catherine A. Richards, PhD, MPH)
In June 2016, the National Academies of Sciences, Engineering, and Medicine (NASEM) released the report entitled A National Trauma Care System: Integrating Military and Civilian Trauma Systems to Achieve Zero Preventable Deaths After Injury [29], with 11 recommendations to reach the goal. The Coalition for National Trauma Research (CNTR) publicly supported this report in their position statement released in August 2016, which emphasized recommendations 7 and 8:
Recommendation 7. “To strengthen trauma research and ensure that the resources available for this research are commensurate with the importance of injury and the potential for improvement in patient outcomes, the White House should issue an executive order mandating the establishment of a National Trauma Research Action Plan (NTRAP) requiring a resourced, coordinated, joint approach to trauma care research across the U.S. Department of Defense (DoD), the U.S. Department of Health and Human Services, the U.S. Department of Transportation, the U.S. Department of Veterans Affairs and others”(p26–27) [30••].
-
Recommendation 8. “To accelerate progress toward the aim of zero preventable deaths after injury and minimizing disability, regulatory agencies should revise research regulations and reduce misinterpretation of the regulations through policy statements (guidance documents)”(p227) [30••].
Armed with these NASEM recommendations in addition to the valuable research experience of the organization, the CNTR “stands ready to lead to the national injury research initiative”(p818) [29].
As orthopedic surgeons, we can be agents of the change needed in trauma care. While the NASEM report emphasizes the elimination of preventable deaths, the burden of disability is more heavily dependent on the outcomes of extremity trauma, managed by orthopedic surgeons and their multi-disciplinary teams. Research into orthopedic trauma outcomes is burgeoning through organizations such as the Major Extremity Trauma Research Consortium (METRC). To achieve recommendations 7 and 8 from the NASEM report, a national trauma research action plan requires full participation by the orthopedic trauma community. Currently, METRC is the largest consortium of large academic orthopedic trauma centers and is supported by more than US$60 million in U.S. Department of Defense funding [31••]. This consortium has highlighted best practices in prospective data collection.
Another important area where we can make a difference in cost containment is implant choice. Most orthopedic surgeons do not know the costs of the implants they use [32]. By familiarizing ourselves with less expensive and non-inferior implant options, we can become active participants in hospital cost-reduction efforts without compromising patient care. Groups of surgeons can negotiate with vendors to establish pricing systems to reduce the costs of implants. Partnership strategies such as matrix pricing and sole-source contracting have been successful [25•]. Awareness and engagement in the pricing systems best occurs in partnership between physicians and administration.
Conclusions
Trauma remains a leading and yet underfunded epidemic in the USA. It is important for orthopedic surgeons to understand the burden of traumatic injury on society, the historic lack of action in response to the epidemic of traumatic injury, and the need for a unified and systematic approach to address this long-standing health crisis. We have a responsibility to engage in efforts to improve the systems-based care of trauma patients and to reduce the disability and death resulting from injury. To this end, we recommend the following actionable items to improve national trauma care and patient outcomes:
Support implementation of a national trauma system as recommended in the NASEM report
Advocate for greater NIH funding for trauma research through a national trauma research action plan
Become familiar with costs and efficacy of orthopedic implants and choose accordingly.
Lead high-quality outcomes research with larger samples of orthopedic trauma patients
Advocate for greater accessibility to level-I trauma care for underserved populations
Despite the current turbulence in the healthcare industry, opportunities exist to initiate many policy-driven improvements, and orthopedic surgeons are well-positioned to be leaders of reform.
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflicts of interest.
Human and animal rights
This article does not contain any studies with human or animal subjects performed by any of the authors.
Funding statement
The authors did not receive any funding or grants in support of their research for or preparation of this work.
Footnotes
This article is part of the Topical Collection on Orthopaedic Health Policy
References
Papers of particular interest, published recently, have been highlighted as: •Of importance, ••Of major importance
- 1.United States Department of Health and Human Services. Health, United States, 2015: with special feature on racial and ethnic health disparities. Available at https://www.cdc.gov/nchs/data/hus/hus15.pdf#019. Accessed 1 March 2017.
- 2.Murray CJL, Lopez AD. The global burden of disease: a comprehensive assessment of mortality and disability from diseases, injuries, and risk factors in 1990 and projected to 2020. Boston, MA: Harvard School of Public Health on behalf of the World Health Organization and the World Bank; 1996. [Google Scholar]
- 3.Trunkey DD. History and development of trauma care in the United States. Clin Orthop. 2000;374:36–46. doi: 10.1097/00003086-200005000-00005. [DOI] [PubMed] [Google Scholar]
- 4.MacKenzie EJ, Rivara FP, Jurkovich GJ, Nathens AB, Frey KP, Egleston BL, et al. A national evaluation of the effect of trauma-center care on mortality. N Engl J Med. 2006;354(4):366–378. doi: 10.1056/NEJMsa052049. [DOI] [PubMed] [Google Scholar]
- 5.National Academy of Sciences and National Research Council Committee on Trauma, National Academy of Sciences and National Research Council Committee on Shock . Accidental death and disability: the neglected disease of modern society. Washington (DC): National Academies Press (US) Copyright (c) National Academy of Sciences; 1966. [Google Scholar]
- 6.National Traffic and Motor Vehicle Safety Act. Pub. L. 89–563, § 1, 80 Stat. 718. 1966
- 7.Mitchell PM, Thakore R, Obremskey A, Sethi MK. Orthopaedic trauma and the evolution of healthcare policy in America. J Orthop Trauma. 2014;28(Suppl 10):S2–S4. doi: 10.1097/BOT.0000000000000214. [DOI] [PubMed] [Google Scholar]
- 8.Institute of Medicine (US), National Research Council (US) Committee on Trauma Research . Injury in America: a continuing public health problem. 1. Washington DC: National Academy Press; 1985. [PubMed] [Google Scholar]
- 9.Trauma Care Systems Planning and Development Act HR 1602, 101st Leg. 1990.
- 10.Buchmueller TC, Jacobson M, Wold C. How far to the hospital? The effect of hospital closures on access to care. J Health Econ. 2006;25(4):740–761. doi: 10.1016/j.jhealeco.2005.10.006. [DOI] [PubMed] [Google Scholar]
- 11.Sampalis JS, Lavoie A, Williams JI, Mulder DS, Kalina M. Impact of on-site care, prehospital time, and level of in-hospital care on survival in severely injured patients. J Trauma. 1993;34(2):252–261. doi: 10.1097/00005373-199302000-00014. [DOI] [PubMed] [Google Scholar]
- 12.Carr BG, Bowman AJ, Wolff CS, Mullen MT, Holena DN, Branas CC, et al. Disparities in access to trauma care in the United States: a population-based analysis. Injury. 2017;48(2):332–338. doi: 10.1016/j.injury.2017.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hsia RY, Srebotnjak T, Maselli J, Crandall M, Mcculloch C, Kellermann AL. The association of trauma center closures with increased inpatient mortality for injured patients. J Trauma Acute Care Surg. 2014;76(4):1048–1054. doi: 10.1097/TA.0000000000000166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hsia RY, Shen YC. Rising closures of hospital trauma centers disproportionately burden vulnerable populations. Health Affairs (Project Hope). 2011;30(10):1912–1920. doi: 10.1377/hlthaff.2011.0510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Glance LG, Osler TM, Mukamel DB, Dick AW. Outcomes of adult trauma patients admitted to trauma centers in Pennsylvania, 2000–2009. Archives of Surgery (Chicago, Ill : 1960) 2012;147(8):732–737. doi: 10.1001/archsurg.2012.1138. [DOI] [PubMed] [Google Scholar]
- 16.Dutton RP, Stansbury LG, Leone S, Kramer E, Hess JR, Scalea TM. Trauma mortality in mature trauma systems: are we doing better? An analysis of trauma mortality patterns, 1997–2008. J Trauma. 2010;69(3):620–626. doi: 10.1097/TA.0b013e3181bbfe2a. [DOI] [PubMed] [Google Scholar]
- 17.Mullins RJ. A historical perspective of trauma system development in the United States. J Trauma. 1999;47(3 Suppl):S8–14. doi: 10.1097/00005373-199909001-00004. [DOI] [PubMed] [Google Scholar]
- 18.American Hospital Association. TrendWatch: Rethinking the hospital readmissions reduction program. Available at http://www.aha.org/research/reports/tw/15mar-tw-readmissions.pdf. Accessed 7 March 2016.
- 19.Benbassat J, Taragin M. Hospital readmissions as a measure of quality of health care: advantages and limitations. Arch Intern Med. 2000;160(8):1074–1081. doi: 10.1001/archinte.160.8.1074. [DOI] [PubMed] [Google Scholar]
- 20.van Walraven C, Bennett C, Jennings A, Austin PC, Forster AJ. Proportion of hospital readmissions deemed avoidable: a systematic review. CMAJ. 2011;183(7):E391–E402. doi: 10.1503/cmaj.101860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Joynt KE, Jha AK. Characteristics of hospitals receiving penalties under the hospital readmissions reduction program. JAMA. 2013;309(4):342–343. doi: 10.1001/jama.2012.94856. [DOI] [PubMed] [Google Scholar]
- 22.Congress.gov. H.R.3982 - Omnibus Budget Reconciliation Act of 1981. Available at https://www.congress.gov/bill/97th-congress/house-bill/3982. Accessed 7 March 2017.
- 23.Shen YC, Hsia RY, Kuzma K. Understanding the risk factors of trauma center closures: do financial pressure and community characteristics matter? Med Care. 2009;47(9):968–978. doi: 10.1097/MLR.0b013e31819c9415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chandra A, Dalton MA, Holmes J. Large increases in spending on postacute care in Medicare point to the potential for cost savings in these settings. Health Affairs (Project Hope). 2013;32(5):864–872. doi: 10.1377/hlthaff.2012.1262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Althausen PL, Lapham J, Mead L. Financial impact of dual vendor, matrix pricing, and sole-source contracting on implant costs. J Orthop Trauma. 2016;30(Suppl 5):S37–Ss9. doi: 10.1097/BOT.0000000000000719. [DOI] [PubMed] [Google Scholar]
- 26.Centers for Disease Control and Prevention. Cost of injuries and violence in the United States. Available at https://www.cdc.gov/injury/wisqars/overview/cost_of_injury.html. Accessed 7 March 2017.
- 27.Lochner HV, Bhandari M, Tornetta P., 3rd Type-II error rates (beta errors) of randomized trials in orthopaedic trauma. J Bone Joint Surg Am. 2001;83-a(11):1650–1655. doi: 10.2106/00004623-200111000-00005. [DOI] [PubMed] [Google Scholar]
- 28.Davis KA, Fabian TC, Cioffi WG. The toll of death and disability from traumatic injury in the United States—the “neglected disease” of modern society, still neglected after 50 years. JAMA Surg. 2016 doi: 10.1001/jamasurg.2016.4625. [DOI] [PubMed] [Google Scholar]
- 29.Jenkins DH, Cioffi WG, Cocanour CS, Davis KA, Fabian TC, Jurkovich GJ, et al. Position statement of the Coalition for National Trauma Research on the National Academies of Sciences, Engineering and Medicine report, a National Trauma Care System: integrating military and civilian trauma systems to achieve zero preventable deaths after injury. J Trauma Acute Care Surg. 2016;81(5):816–818. doi: 10.1097/TA.0000000000001218. [DOI] [PubMed] [Google Scholar]
- 30.Berwick DM, Downey AS, Cornett E, National Academies of Sciences Engineering and Medicine (U.S.), Committee on Military Trauma Care’s Learning Health System and Its Translation to the Civilian Sector, National Academies of Sciences Engineering and Medicine (U.S.) et al. A national trauma care system: integrating military and civilian trauma systems to achieve zero preventable deaths after injury. Washington, DC: National Academies Press; 2016. [PubMed] [Google Scholar]
- 31.Major Extremity Trauma Research Consortium (METRC) Building a clinical research network in trauma orthopaedics: the Major Extremity Trauma Research Consortium (METRC) J Orthop Trauma. 2016;30(7):353–361. doi: 10.1097/BOT.0000000000000549. [DOI] [PubMed] [Google Scholar]
- 32.Okike K, O'Toole RV, Pollak AN, Bishop JA, McAndrew CM, Mehta S, et al. Survey finds few orthopedic surgeons know the costs of the devices they implant. Health Affairs (Project Hope) 2014;33(1):103–109. doi: 10.1377/hlthaff.2013.0453. [DOI] [PMC free article] [PubMed] [Google Scholar]


