Abstract
Background
Various osteotomies have been introduced to treat osteonecrosis of the femoral head. The purpose of this study was to compare surgical parameters, postoperative limb length discrepancy, and minimum 5-year clinical and radiological results between transtrochanteric curved varus osteotomy (TCVO) and transtrochanteric rotational osteotomy (TRO) for osteonecrosis of the femoral head.
Methods
From 2004 to 2009, 103 consecutive TROs (97 patients) followed by 72 consecutive TCVOs (64 patients) were performed for the treatment of osteonecrosis of the femoral head. Of these, 85 patients (91 hips) in the TRO group and 58 patients (65 hips) in the TCVO group completed minimum 5-year clinical and radiological follow-up. The Kaplan-Meier product-limit method was used to estimate survival.
Results
The TCVO group had shorter operation time (p < 0.05) and less estimated blood loss (p = 0.026). Postoperative collapse developed in 26 hips (28.6%) in the TRO group and 7 hips (10.8%) in the TCVO group (p = 0.007). Osteophyte formation was observed in 34 hips (37.4%) in the TRO group and 13 hips (20%) in the TCVO group (p = 0.020). Fifteen hips (16.5%) in the TRO group and 7 hips (10.8%) in the TCVO group underwent conversion total hip arthroplasty (THA). The survival rate at 9 years with radiographic collapse as the endpoint was 68.7% (95% confidence interval [CI], 58.1% to 79.3%) in the TRO group, and 84.7% (95% CI, 71.5% to 97.9%) in the TCVO group. With conversion to THA as the endpoint, the survival rate was 82.2% (95% CI, 73.1% to 91.3%) in the TRO group and 89.2% (95% CI, 81.7% to 96.7%) in the TCVO group.
Conclusions
The comparison indicates that TCVO was better than TRO in terms of surgical parameters including operation time and estimated blood loss while the 9-year survival rates were similar.
Keywords: Femur head, Osteonecrosis, Transtrochanteric rotational osteotomy, Transtrochanteric curved varus osteotomy
Osteonecrosis is the most frequent disease of the hip that can lead to total hip arthroplasty (THA) in young adults.1,2) In young patients, THA using conventional polyethylene has been associated with excessive wear and osteolysis and unacceptably high failure rates.3,4) THAs using contemporary bearings are known to have lower rates of failure.5,6,7) However, most reports were based on mid-term followups and only a few studies reported long-term results.8) In the meantime, several osteotomies have been introduced as alternatives to THA for young patients.1,2,9)
Transtrochanteric curved varus osteotomy (TCVO) was devised by Nishio and Sugioka10) in 1971. In this technique, a curved osteotomy is made between the greater and the lesser trochanters and the femoral head is rotated into varus to move the necrotic portion of the femoral head from the weight-bearing region to a non-weight-bearing medial region. This osteotomy can reduce complications of conventional varus wedge osteotomy, such as elevation of the greater trochanter, nonunion of the osteotomy site, and limb length discrepancy (LLD).9,11,12) Saito et al.13) reported a 100% success rate in 4 cases of osteonecrosis of the femoral head, and the rate of satisfactory outcomes ranged from 90% to 97.3% in other studies.11,14,15)
Transtrochanteric rotational osteotomy (TRO) was introduced by Sugioka16) in 1978. It also moves the necrotic portion from the weight-bearing region to a non-weight-bearing region. However, in this procedure, the greater trochanter is osteotomized and the joint capsule is circumferentially incised. The reported success rates of this technique range from 17% to 100%.17,18,19)
However, studies thus far have not compared these two well-known osteotomies. Until 2006, we had performed TRO in patients who met our predefined selection criteria. However, collapse of the femoral head and osteoarthritis of the hip developed in some patients after the osteotomy.19) Therefore, we have performed TCVO since 2007. In this study, we compared surgical parameters, postoperative LLD and minimum 5-year clinical and radiological results between the two osteotomies in young patients.
METHODS
Patient Selection
The subjects of this study were 97 consecutive patients (103 hips) who underwent TRO from 2004 to 2006 and 64 consecutive patients (72 hips) who underwent TCVO from 2007 to 2009. All osteotomies were done at one institution by a single senior surgeon. The design and protocol of this retrospective study were approved by the Seoul National University Bundang Hospital Institutional Review Board, which waived informed consent (No. B-1412-280-113).
The diagnosis of osteonecrosis was based on findings on radiographs and magnetic resonance imaging (MRI) scans. The selection criteria for the osteotomies were (1) Ficat stage IIB (a crescentic subchondral line and segmental flattening of the femoral head) or stage III (a sequestrum, a break in the articular cartilage from one end of the affected area to the other, and a normal joint space);20,21) (2) age younger than 55 years; (3) a painful hip; and (4) a hip with an adequate area of viable bone as seen on MRI scans, which was expected to occupy more than 50% of the articular surface below the acetabular dome after osteotomy.
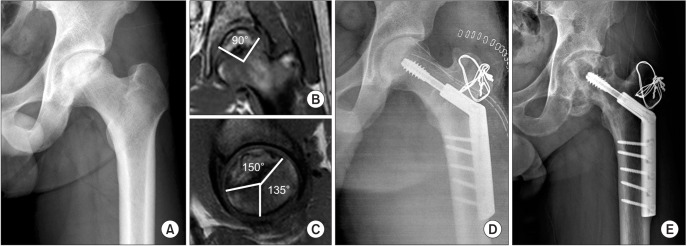
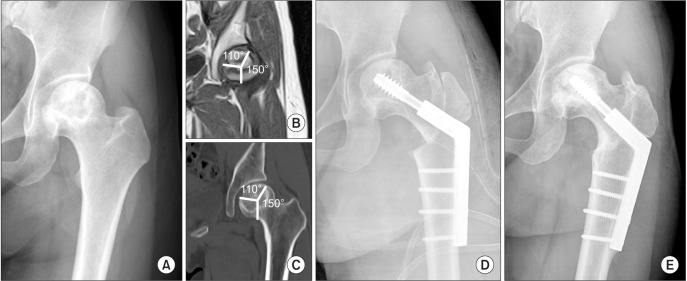
The criterion of adequate viable bone for TRO was an arc of > 120° between the central vertical line of the femoral head and the posterior margin of the necrotic portion on the mid-sagittal MRI scan (Fig. 1).18) The criterion for TCVO was an arc of > 150° between the central vertical line of the femoral head and the lateral margin of the necrotic portion on the mid-coronal MRI scan (Fig. 2).
Fig. 1. A 35-year-old man had osteonecrosis in the left femoral head. (A) Preoperative anteroposterior hip radiograph. (B and C) The combined necrotic angle was 240°. (B) The angle of the necrotic area in the mid-coronal image was 90°. (C) The angle of the necrotic area in the mid-sagittal image was 150°. The angle between the central vertical line of the femoral head and the posterior margin of the necrotic portion was 135°. (D) Immediate postoperative anteroposterior hip radiograph after transtrochanteric rotational osteotomy. (E) Follow-up radiograph taken 6 years after the operation showing osteophyte formation around the femoral head.
Fig. 2. A 28-year-old woman had osteonecrosis in the left femoral head. (A) Preoperative anteroposterior hip radiograph. (B and C) The angle of the necrotic area in the mid-coronal images of computed tomography and magnetic resonance imaging was 110°. The angle between the central vertical line of the femoral head and the lateral margin of the necrotic portion was 150°. (D) Immediate postoperative anteroposterior hip radiograph after curved intertrochanteric varus osteotomy. (E) Follow-up radiograph taken 6 years after the operation showing no progressing collapse or osteophyte formation around the femoral head.
The extent of osteonecrosis was measured on preoperative MRI scans using the combined necrotic angle. Briefly, the angle of the necrotic portion on the mid-coronal image (A) and the angle of the necrotic portion on the mid-sagittal image (B) were measured, and the combined necrotic angle was calculated as the sum of A and B (Fig. 1B and C).
Demographic Data
Of the 97 patients (103 hips) who were operated with TRO, 12 patients (12 hips) were lost to follow-up before 5 years after the osteotomy. The remaining 85 patients (91 hips), who were followed for a minimum of 5 years or until conversion THA, were included in the final analysis. There were 72 men (78 hips) and 13 women (13 hips). The mean age of the patients at the time of osteotomy was 33.8 years (range, 16 to 54 years) and the mean body mass index was 24.1 kg/m2 (range, 17.2 to 34.1 kg/m2). The cause of osteonecrosis was idiopathic in 36 hips (34 patients), alcohol-associated in 32 hips (29 patients), steroidinduced in 15 hips (14 patients), posttraumatic in 7 hips (7 patients), and systemic lupus erythematosus (SLE) in 1 hip (1 patient). The preoperative Ficat stage was IIB in 37 hips and III in 54 hips. The combined necrotic angle was 218.0° ± 12.0° (range, 195° to 260°). The preoperative Merle d'Aubigne and Postel hip score22) ranged from 9 to 17 points (mean, 14.9 points). The mean follow-up period was 7.7 years (range, 5 to 11 years).
Of the 64 patients (72 hips) who were operated with TCVO, 6 patients (7 hips) were lost to follow-up before 5 years after the osteotomy. The remaining 58 patients (65 hips), who were followed for a minimum of 5 years or until conversion THA, were included in the final analysis. There were 33 men (37 hips) and 25 women (28 hips). The mean age of the patients at the time of osteotomy was 31.8 years (range, 18 to 52 years) and the mean body mass index was 23.5 kg/m2 (range, 17.7 to 38.8 kg/m2). The cause of osteonecrosis was idiopathic in 32 hips (29 patients), alcohol-associated in 9 hips (8 patients), steroid-induced in 21 hips (18 patients), posttraumatic in 2 hips (2 patients) and SLE in 1 hip (1 patient). The preoperative Ficat stage was IIB in 19 hips and III in 46 hips. The combined necrotic angle was 219.7° ± 24.9° (range, 180° to 280°). The preoperative Merle d'Aubigne and Postel hip score ranged from 13 to 18 points (mean, 14.7 points). The mean follow-up period was 6.5 years (range, 5 to 9.5 years)
The gender distribution, causes of osteonecrosis and follow-up durations were different between the 2 groups. However, there were no significant differences regarding age (p = 0.155), the stage of osteonecrosis (p = 0.142), body mass index (p = 0.312), and combined necrotic angle (p = 0.262) (Table 1).
Table 1. Patient Demographics.
| Variable | TRO (n = 91) | TCVO (n = 65) | p-value |
|---|---|---|---|
| Sex (male:female) (hip) | 78:13 | 37:28 | < 0.001 |
| Age (yr) | 33.8 ± 8.4 | 31.8 ± 8.2 | 0.155 |
| Body mass index (kg/m2) | 24.1 ± 3.3 | 23.5 ± 3.7 | 0.312 |
| Causes of ONFH | 0.012 | ||
| Idiopathic | 36 | 32 | |
| Alcohol | 32 | 9 | |
| Steroid | 15 | 21 | |
| Posttraumatic | 7 | 2 | |
| SLE | 1 | 1 | |
| Ficat stage | 0.142 | ||
| IIB | 37 | 19 | |
| III | 54 | 46 | |
| Combined necrotic angle (°) | 218.0 ± 12.0 | 219.7 ± 24.9 | 0.262 |
| Follow-up duration (yr) | 7.7 ± 2.1 | 6.5 ± 1.2 | < 0.001 |
Values are presented as mean ± standard deviation or number.
TRO: transtrochanteric rotational osteotomy, TCVO: transtrochanteric curved varus osteotomy, ONFH: osteonecrosis of femoral head, SLE: systemic lupus erythematosus.
Operative Technique and Postoperative Care
All operations were done by a single surgeon. TROs were performed using a modified Sugioka technique19) and TCVOs using a technique by Nishio and Sugioka.10)
The osteotomy site was fixed with use of a 120° compression hip screw (Solco, Seoul, Korea). Postoperative care consisted of the use of crutches with protected weight-bearing until there was radiographic evidence of osseous union of the osteotomy site usually for 3 months.
Follow-up Evaluations
All of the patients underwent a bone scan within 1 week postoperatively to assess the viability of the femoral head.23) Routine follow-up visits were scheduled for 6 weeks, 3, 6, 9 and 12 months after surgery and every 6 months thereafter. Postoperative radiographic and clinical evaluations were performed at a minimum of 5 years in the 143 patients (85 TRO patients and 58 TCVO patients).
Clinical evaluations were done using Merle d'Aubigne and Postel hip score,22) which allots up to 6 points for pain, mobility, and gait each. A score of 17 or 18 points was recorded as an excellent result; 15 or 16 points, as a good result; 13 or 14 points, as a fair result; and < 12 points, as a poor result. If the score was < 12 or the patient had a THA, the result was considered as a clinical failure.
Radiographic evaluation included determination of whether there was postoperative collapse of the newly established weight-bearing area of the femoral head, osteophyte formation around the femoral head, or osteoarthritic change of the hip. The radiographic evaluation was done by two independent observers who did not participate in the operations (CHP, YKL). The 6-week anteroposterior and cross-table lateral radiographs were considered to be the baseline studies for radiographic comparison. Collapse was defined as subsidence of the articular surface exceeding 2 mm as compared with the contour on the baseline radiograph.18) Osteophyte formation was defined as spurs > 3 mm around the femoral head as compared with the contour on the baseline radiograph.24) Joint space narrowing was defined as a width of joint space < 2 mm at the narrowest portion.25)
To evaluate LLD, we measured the distance between the inter-teardrop line and the lower margin of the lesser trochanter.26) Then, we evaluated whether the difference in distance between the operated limb and the contralateral limb was more than 2 cm.
We compared the surgical parameters, including the operation time, estimated blood loss (EBL) and requirement of transfusion between TRO patients and TCVO patients. We also compared perioperative complications, LLD, postoperative collapse, postoperative osteoarthritis, the final hip score and survivorship between both groups.
Statistical Analysis
Qualitative data were compared with the chi-squared test or Fisher exact test, and quantitative data were compared with the Student t-test or the Mann-Whitney U-test, depending on the distribution of the data. All reported p-values were two sided, and p < 0.05 was used to determine statistical significance. We calculated the time from the index osteotomy to conversion to a THA. And, Kaplan-Meier survival analysis was performed with use of 2 endpoints; radiological failures such as secondary collapse on the newly established weight bearing portion or degenerative change and conversion to THA. The analysis was performed with use of IBM SPSS ver. 22.0 (IBM Co., Armonk, NY, USA).
RESULTS
Postoperative Scintigraphy
All hips in both groups showed adequate perfusion of the proximal segment on the postoperative bone scan.
Intraoperative Parameters
The TCVO group had shorter operation time (p < 0.001) and less estimated blood loss (p = 0.026) than the TRO group (Table 2). However, the mean amount of transfusion was not different in both groups (p = 0.678).
Table 2. Comparison of Variables between the TRO and TCVO Groups.
| Variable | TRO | TCVO | p-value |
|---|---|---|---|
| Operation time (min) | 168.5 ± 29.3 | 149.1 ± 23.5 | < 0.001 |
| Estimated blood loss (mL) | 540.2 ± 275.3 | 390.0 ± 361.9 | 0.026 |
| Transfusion (mL) | 213.3 ± 158.3 | 208.3 ± 147.3 | 0.678 |
| Secondary collapse | 26 | 7 | 0.007 |
| Osteophyte formation | 34 | 13 | 0.020 |
| Joint space narrowing | 11 | 6 | 0.572 |
| No. of conversion to THA | 15 | 7 | 0.312 |
| LLD > 2 (cm) | 4 | 0 | 0.141 |
| Merle d'Aubigne and Postel hip score | |||
| Preoperative | 14.9 ± 1.5 | 14.7 ± 1.1 | 0.449 |
| Final follow-up | 17.4 ± 0.8 | 17.1 ± 0.9 | 0.523 |
| Complication | 0.361 | ||
| Infection | 1 | 0 | |
| Nonunion | 2 | 1 | |
| Metal failure | 5 | 1 | |
| Periprosthetic fracture | 1 | 1 |
Values are presented as mean ± standard deviation or number.
TRO: transtrochanteric rotational osteotomy, TCVO: transtrochanteric curved varus osteotomy, THA: total hip arthroplasty, LLD: limb length discrepancy.
Secondary Collapse and Osteoarthritic Change
Secondary collapse of the femoral head developed in 26 hips (28.6%) in the TRO group and 7 hips (10.8%) in the TCVO group (p = 0.007). Osteophyte formation was observed in 34 hips (37.4%) in the TRO group and 13 hips (20%) in the TCVO group (p = 0.020). Joint space narrowing developed in 11 hips (12.1%) in the TRO group and 6 hips (9.2%) in the TCVO group (p = 0.572).
Complications
A deep infection developed in 1 hip of the TRO group at 13 months after the osteotomy. It was successfully treated with removal of the compression hip screw, debridement, and administration of antibiotics. Nonunion of the greater trochanter occurred in 2 hips of the TRO group. All of these hips were asymptomatic and required no additional intervention. Nonunion of the osteotomy site occurred in 1 hip of the TCVO group, which was treated with a conversion THA at 15 months after the osteotomy. Periprosthetic fracture at the tip of the plate occurred in 1 hip of the TRO group and 1 hip of the TCVO group. These fractures were treated with open reduction and fixation with a longer plate and osteosynthesis was obtained in all of them (Table 2).
Conversion to THA
Fifteen collapsed hips of the TRO group were converted to a THA due to intractable pain. In the TCVO group, 6 hips were converted to a THA due to collapse and intractable pain and 1 hip due to nonunion of the osteotomy site.
Leg Length Discrepancy
The mean LLD was 8.3 mm (range, 2 to 26 mm) in the TRO group and 4.3 mm (range, 1 to 17 mm) in the TCVO group (p = 0.083). In the TRO group, the operated leg was shortened by 10 to 20 mm in 23 patients (25.3%) and by > 20 mm in 4 patients (4.4%).
Clinical Results
In the TRO group, 31 patients (36.5%) had a limp, which was mild in 26 and moderate in 5. In the TCVO group, 10 patients (17.2%) had a limp, which was mild in 3 and moderate in 7.
In the TRO group, the final Merle d'Aubigne and Postel hip score was 17.4 ± 0.8 (range, 15 to 18). Seventy-three of the 85 patients (85.9%) had excellent or good hip scores without conversion to THA at the latest follow-up.
In the TCVO group, the final hip score was 17.1 ± 0.9 (range, 15 to 18). Fifty of the 58 patients (86.2%) had excellent or good hip scores without conversion to THA at the latest follow-up (Table 2).
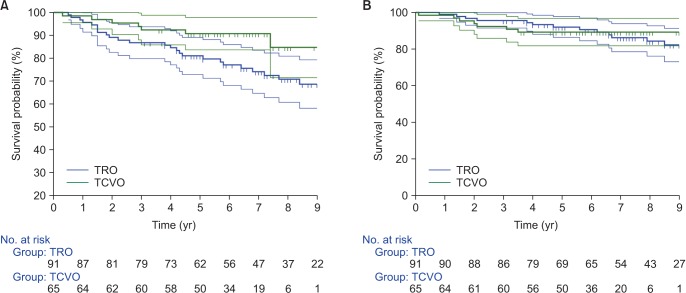
Survivorship
Kaplan-Meier survivorship analysis with collapse on the radiographs as the endpoint, revealed a cumulative survival rate of 68.7% (95% confidence interval [CI], 58.1% to 79.3%) in the TRO group, and 84.7% (95% CI, 71.5% to 97.9%) in the TCVO group at 9 years (p = 0.064) (Fig. 3A). With a conversion to THA as the endpoint, the survival rate was 82.2% (95% CI, 73.1% to 91.3%) in the TRO group and 89.2% (95% CI, 81.7% to 96.7%) in the TCVO group at 9 years (p = 0.246) (Fig. 3B).
Fig. 3. Survival curves with collapse on the radiograph as the endpoint (A) and conversion to total hip arthroplasty as the endpoint (B). TRO: transtrochanteric rotational osteotomy, TCVO: transtrochanteric curved varus osteotomy.
DISCUSSION
To date, 3 studies have reported the results of TCVO: the success rate was more than 90% in these studies. In contrast, the success rates of TRO are inconsistent: successful results have been reported by Japanese and Korean surgeons18,27,28,29) whereas such favorable results have not been obtained by surgeons in Western countries.30) The inconsistency in the results of TRO may be related to differences in the selection criteria of patients, ethnic difference especially in body mass index, preoperative stage of the necrosis, the extent of necrosis, the surgical technique, the method of fixation, and/or the postoperative management.19) However, there was no comparison study of these 2 osteotomies. Our study indicates that TCVO compared to TRO has advantages in radiological outcomes, such as the lower incidence of osteophyte formation and collapse of the femoral head. However, the 9-year survival rate was comparable between the 2 procedures when radiographic collapse and conversion to THA was used as the endpoint.
Osteophyte formation has been known to cause impingement of the hip joint and subsequent osteoarthritis.28,31) In our study, osteophyte formation was observed in 34 hips (37%) in the TRO group and 7 of them showed joint space narrowing. However, osteophyte formation was observed in 13 hips (20%) in the TCVO group and no case among them showed joint space narrowing. In TCVO, the head segment is simply rotated into varus in the coronal plane. However, in TRO, the segment is rotated anteriorly in the sagittal plane as well as into varus in the coronal plane. The mechanical simplicity and avoidance of capsulotomy of TCVO seem to result in a low incidence of osteophyte formation and joint space narrowing.
LLD is a serious problem after osteotomies of the proximal femur. In 1965, Merle D'Aubigne et al.1) reported good results with varus wedge osteotomy for the treatment of osteonecrosis of the femoral head. Since then, several studies have reported successful results with this technique.9,12) It is a less invasive and less technically demanding surgical approach as compared with TRO. However, several complications, such as elevation or lateral displacement of the greater trochanter and LLD, occurred following varus wedge osteotomy.9,11,12) TCVO was designed to minimize these complications. In previous studies, the mean discrepancy following TCVO ranged from 12.5 mm to 13.0 mm.11,14) In our study, although the mean postoperative LLD was not significantly different between the groups, 4 patients in the TRO group showed their operated legs were shortened by > 20 mm at the latest follow-up.
This study has several limitations. First, our study included a small cohort of TCVO group compared to the TRO group, which might have negatively affected statistical power. Second, our study was not a randomized clinical trial. It is a so called “before and after study,” in which values obtained before TCVO were compared with those taken afterwards. This design is prone to bias because of failure to control for potential confounding variables. However, all osteotomies were done by a single high-volume surgeon who had specialized in hip surgery since 1992. Except for gender distribution and the causes of osteonecrosis, there were no significant differences between the groups in terms of age, the stage of osteonecrosis, body mass index, and the extent of disease measured by combined necrotic angle. All 161 patients had adequate viable bone in the femoral head on both mid-sagittal and midcoronal MRI scans to meet the selection criteria for TRO and TCVO. In addition, our results of TCVO were consistent with those of the previous studies on this osteotomy (Table 3).11,14,15,17,18,19,27,28,29,30,31,32)
Table 3. Clinical Results of Osteotomy for Osteonecrosis of the Femoral Head in Published Studies.
| Study (year) | Type | No. of patients (hips) | Follow-up duration (yr) | Mean age (yr) | Success rate (%) |
|---|---|---|---|---|---|
| Jacobs et al. (1989)32) | TRO | 22 (22) | 5.3 | 35 | 73 |
| Sugioka et al. (1992)27) | TRO | 229 (295) | 3–16 | - | 78 |
| Sugano et al. (1992)31) | TRO | 40 (41) | 6.3 | 36 | 56 |
| Dean and Cabanela (1993)17) | TRO | 17 (18) | 5 | 35 | 17 |
| Miyanishi et al. (2000)29) | TRO | (125) | 13.5 | - | 78 |
| Koo et al. (2001)18) | TRO | 17 (17) | 4.5 | 30 | 100 |
| Hisatome et al. (2004)28) | TRO | 21 (25) | 6.4 | 38 | 80 |
| Rijnen et al. (2005)30) | TRO | 22 (26) | 8.7 | 31.5 | 27 |
| Ha et al. (2010)19) | TRO | 105 (113) | 4.3 | 34 | 63 |
| Sakano et al. (2004)14) | TCVO | 20 (20) | 4 | 38 | 90 |
| Ikemura et al. (2007)11) | TCVO | 36 (42) | 5.9 | 34 | 97.3 |
| Zhao et al. (2010)15) | TCVO | 62 (73) | 12.4 | 33.3 | 91.8 |
| Current study | TCVO | 58 (65) | 6.7 | 31.8 | 88.3 |
| TRO | 85 (91) | 8.2 | 33 | 80.6 |
TRO: transtrochanteric rotational osteotomy, TCVO: transtrochanteric curved varus osteotomy.
Since 2007, we have exclusively used TCVO for the treatment of osteonecrosis of the femoral head in patients aged less than 40 years. Based on the results of our study, we recommend TCVO as a joint preserving osteotomy in young patients.
Footnotes
CONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported.
References
- 1.Merle D'Aubigne R, Postel M, Mazabraud A, Massias P, Gueguen J, France P. Idiopathic necrosis of the femoral head in adults. J Bone Joint Surg Br. 1965;47(4):612–633. [PubMed] [Google Scholar]
- 2.Kerboul M, Thomine J, Postel M, Merle d'Aubigne R. The conservative surgical treatment of idiopathic aseptic necrosis of the femoral head. J Bone Joint Surg Br. 1974;56(2):291–296. [PubMed] [Google Scholar]
- 3.Katz RL, Bourne RB, Rorabeck CH, McGee H. Total hip arthroplasty in patients with avascular necrosis of the hip: follow-up observations on cementless and cemented operations. Clin Orthop Relat Res. 1992;(281):145–151. [PubMed] [Google Scholar]
- 4.Kim YH, Oh JH, Oh SH. Cementless total hip arthroplasty in patients with osteonecrosis of the femoral head. Clin Orthop Relat Res. 1995;(320):73–84. [PubMed] [Google Scholar]
- 5.Daniel J, Pynsent PB, McMinn DJ. Metal-on-metal resurfacing of the hip in patients under the age of 55 years with osteoarthritis. J Bone Joint Surg Br. 2004;86(2):177–184. doi: 10.1302/0301-620x.86b2.14600. [DOI] [PubMed] [Google Scholar]
- 6.Lee YK, Ha YC, Yoo JJ, Koo KH, Yoon KS, Kim HJ. Alumina-on-alumina total hip arthroplasty: a concise follow-up, at a minimum of ten years, of a previous report. J Bone Joint Surg Am. 2010;92(8):1715–1719. doi: 10.2106/JBJS.I.01019. [DOI] [PubMed] [Google Scholar]
- 7.Hwang KT, Kim YH, Kim YS, Choi IY. Cementless total hip arthroplasty with a metal-on-metal bearing in patients younger than 50 years. J Arthroplasty. 2011;26(8):1481–1487. doi: 10.1016/j.arth.2011.02.020. [DOI] [PubMed] [Google Scholar]
- 8.Kang BJ, Ha YC, Ham DW, Hwang SC, Lee YK, Koo KH. Third-generation alumina-on-alumina total hip arthroplasty: 14 to 16-year follow-up study. J Arthroplasty. 2015;30(3):411–415. doi: 10.1016/j.arth.2014.09.020. [DOI] [PubMed] [Google Scholar]
- 9.Mont MA, Fairbank AC, Krackow KA, Hungerford DS. Corrective osteotomy for osteonecrosis of the femoral head. J Bone Joint Surg Am. 1996;78(7):1032–1038. doi: 10.2106/00004623-199607000-00007. [DOI] [PubMed] [Google Scholar]
- 10.Nishio A, Sugioka Y. A new technique of the varus oste-otomy at the upper end of the femur. Orthop Traumatol. 1971;20(3):381–386. [Google Scholar]
- 11.Ikemura S, Yamamoto T, Jingushi S, Nakashima Y, Mawatari T, Iwamoto Y. Leg-length discrepancy after transtrochanteric curved varus osteotomy for osteonecrosis of the femoral head. J Bone Joint Surg Br. 2007;89(6):725–729. doi: 10.1302/0301-620X.89B6.18499. [DOI] [PubMed] [Google Scholar]
- 12.Ito H, Kaneda K, Matsuno T. Osteonecrosis of the femoral head: simple varus intertrochanteric osteotomy. J Bone Joint Surg Br. 1999;81(6):969–974. doi: 10.1302/0301-620x.81b6.10037. [DOI] [PubMed] [Google Scholar]
- 13.Saito S, Ohzono K, Ono K. Joint-preserving operations for idiopathic avascular necrosis of the femoral head: results of core decompression, grafting and osteotomy. J Bone Joint Surg Br. 1988;70(1):78–84. doi: 10.1302/0301-620X.70B1.3276703. [DOI] [PubMed] [Google Scholar]
- 14.Sakano S, Hasegawa Y, Torii Y, Kawasaki M, Ishiguro N. Curved intertrochanteric varus osteotomy for osteonecrosis of the femoral head. J Bone Joint Surg Br. 2004;86(3):359–365. doi: 10.1302/0301-620x.86b3.14383. [DOI] [PubMed] [Google Scholar]
- 15.Zhao G, Yamamoto T, Ikemura S, et al. Radiological outcome analysis of transtrochanteric curved varus osteotomy for osteonecrosis of the femoral head at a mean follow-up of 12.4 years. J Bone Joint Surg Br. 2010;92(6):781–786. doi: 10.1302/0301-620X.92B6.23621. [DOI] [PubMed] [Google Scholar]
- 16.Sugioka Y. Transtrochanteric anterior rotational osteotomy of the femoral head in the treatment of osteonecrosis affecting the hip: a new osteotomy operation. Clin Orthop Relat Res. 1978;(130):191–201. [PubMed] [Google Scholar]
- 17.Dean MT, Cabanela ME. Transtrochanteric anterior rotational osteotomy for avascular necrosis of the femoral head: long-term results. J Bone Joint Surg Br. 1993;75(4):597–601. doi: 10.1302/0301-620X.75B4.8331115. [DOI] [PubMed] [Google Scholar]
- 18.Koo KH, Song HR, Yang JW, Yang P, Kim JR, Kim YM. Trochanteric rotational osteotomy for osteonecrosis of the femoral head. J Bone Joint Surg Br. 2001;83(1):83–89. doi: 10.1302/0301-620x.83b1.10914. [DOI] [PubMed] [Google Scholar]
- 19.Ha YC, Kim HJ, Kim SY, Kim KC, Lee YK, Koo KH. Effects of age and body mass index on the results of transtrochanteric rotational osteotomy for femoral head osteonecrosis. J Bone Joint Surg Am. 2010;92(2):314–321. doi: 10.2106/JBJS.H.01020. [DOI] [PubMed] [Google Scholar]
- 20.Ficat RP. Idiopathic bone necrosis of the femoral head: early diagnosis and treatment. J Bone Joint Surg Br. 1985;67(1):3–9. doi: 10.1302/0301-620X.67B1.3155745. [DOI] [PubMed] [Google Scholar]
- 21.Smith SW, Meyer RA, Connor PM, Smith SE, Hanley EN., Jr Interobserver reliability and intraobserver reproducibility of the modified Ficat classification system of osteonecrosis of the femoral head. J Bone Joint Surg Am. 1996;78(11):1702–1706. doi: 10.2106/00004623-199611000-00010. [DOI] [PubMed] [Google Scholar]
- 22.D'Aubigne RM, Postel M. Functional results of hip arthroplasty with acrylic prosthesis. J Bone Joint Surg Am. 1954;36(3):451–475. [PubMed] [Google Scholar]
- 23.Lausten GS, Hesse B, Thygesen V, Fogh J. Prediction of late complications of femoral neck fractures by scintigraphy. Int Orthop. 1992;16(3):260–264. doi: 10.1007/BF00182707. [DOI] [PubMed] [Google Scholar]
- 24.Swezey RL, Bjarnason DM. Inhibition of secondary osteophyte formation in rheumatoid arthritis. Rheumatol Rehabil. 1976;15(1):10–16. doi: 10.1093/rheumatology/15.1.10. [DOI] [PubMed] [Google Scholar]
- 25.Jacobsen S, Sonne-Holm S, Soballe K, Gebuhr P, Lund B. The relationship of hip joint space to self reported hip pain: a survey of 4.151 subjects of the Copenhagen City Heart Study: the Osteoarthritis Substudy. Osteoarthritis Cartilage. 2004;12(9):692–697. doi: 10.1016/j.joca.2004.05.010. [DOI] [PubMed] [Google Scholar]
- 26.Woolson ST, Hartford JM, Sawyer A. Results of a method of leg-length equalization for patients undergoing primary total hip replacement. J Arthroplasty. 1999;14(2):159–164. doi: 10.1016/s0883-5403(99)90119-5. [DOI] [PubMed] [Google Scholar]
- 27.Sugioka Y, Hotokebuchi T, Tsutsui H. Transtrochanteric anterior rotational osteotomy for idiopathic and steroid-induced necrosis of the femoral head: indications and longterm results. Clin Orthop Relat Res. 1992;(277):111–120. [PubMed] [Google Scholar]
- 28.Hisatome T, Yasunaga Y, Takahashi K, Ochi M. Progressive collapse of transposed necrotic area after transtrochanteric rotational osteotomy for osteonecrosis of the femoral head induces osteoarthritic change: mid-term results of transtrochanteric rotational osteotomy for osteonecrosis of the femoral head. Arch Orthop Trauma Surg. 2004;124(2):77–81. doi: 10.1007/s00402-003-0610-0. [DOI] [PubMed] [Google Scholar]
- 29.Miyanishi K, Noguchi Y, Yamamoto T, et al. Prediction of the outcome of transtrochanteric rotational osteotomy for osteonecrosis of the femoral head. J Bone Joint Surg Br. 2000;82(4):512–516. doi: 10.1302/0301-620x.82b4.10065. [DOI] [PubMed] [Google Scholar]
- 30.Rijnen WH, Gardeniers JW, Westrek BL, Buma P, Schreurs BW. Sugioka's osteotomy for femoral-head necrosis in young Caucasians. Int Orthop. 2005;29(3):140–144. doi: 10.1007/s00264-005-0639-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sugano N, Takaoka K, Ohzono K, Matsui M, Saito M, Saito S. Rotational osteotomy for non-traumatic avascular necrosis of the femoral head. J Bone Joint Surg Br. 1992;74(5):734–739. doi: 10.1302/0301-620X.74B5.1527125. [DOI] [PubMed] [Google Scholar]
- 32.Jacobs MA, Hungerford DS, Krackow KA. Intertrochanteric osteotomy for avascular necrosis of the femoral head. J Bone Joint Surg Br. 1989;71(2):200–204. doi: 10.1302/0301-620X.71B2.2925735. [DOI] [PubMed] [Google Scholar]