Abstract
Heart failure is appropriately described as an epidemic, with 1–2% of health care expenditure being directed at its management. In England, the National Institute for Health and Care Excellence (NICE) has issued guidance on the best practice for the diagnosis and treatment of acute and chronic heart failure. Echocardiography is key to the diagnosis of the underlying cardiac abnormalities, and access to this (with our without biochemical testing using natriuretic peptides) is key to high-quality and speedy diagnosis. New models of care aim to speed up access to echocardiography, but a shortage of technically trained staff remains a limiting factor in improving standards of care. The NHS audits the quality of care and outcome for patients admitted to hospital with heart failure, and this continues to show wide variation in practice, particularly, where patients are not reviewed by the local heart failure multidisciplinary team. Recently, the All Party Parliamentary Group on Cardiac Disease issued 10 suggestions for improvement in care for patients with heart failure – access to echocardiography being one of the key suggestions. Time will tell as to whether this support from law makers will assist in the implementation of NICE-recommended standards of care consistently across the country.
Keywords: heart failure, echocardiography, diagnosis, guidelines
Introduction
An epidemic attacks or affects many persons simultaneously in a community – and according to that definition, heart failure is indeed a present day epidemic. Recent estimates suggest that there are 26 million patients worldwide with heart failure (1) and more than half a million people living with this syndrome in the United Kingdom alone (2). From the health care system perspective, the burden is large: 1–2% of the NHS budget is estimated to be spent on heart failure, with 60–70% related to the costs of hospitalisation (3).
The epidemiology
Epidemiological studies of new cases of heart failure in the United Kingdom have helped to clarify some of the key features of this syndrome. In the 1990s, the average age at first diagnosis was around 76 years, and the incidence was always higher in men than that in women, presumably related to the earlier onset of coronary artery disease in men (4). The risk increases steeply with age in both sexes and reaches as high as 1.5% per annum in men over the age of 85 years. In those aged below 75 years, coronary artery disease accounts for more than 50% of cases, and more than 20% have a dilated cardiomyopathy as the underlying cardiac abnormality – presumably many of these cases are familial (5). Valve disease accounted for just over 10% of new cases in the 1990s, but this is likely to be increasing as our population ages, and senile aortic stenosis becomes increasingly common.
Echocardiography is key to the diagnosis of heart failure – being the most readily available and economic manner of imaging the heart and gathering key information about its structure and function.
NHS audit data
We are fortunate in the United Kingdom to have a national audit of patients discharged from hospital with a diagnosis of heart failure. In the most recently available data, from 2014/15, 56,915 cases from England and Wales were included in the audit, representing just under 80% of all heart failure admissions (6). Echocardiography was performed in around 90% of these cases, with the use higher in those patients admitted to a cardiac ward (around 50% of patients) than those admitted to a more general or non-cardiac ward. In addition to non-cardiologists not using echocardiography as much as cardiologists (perhaps because their access is more restricted or because they do not realise how useful it can be), non-cardiologists are less likely to use all of the disease-modifying drugs for heart failure: ACE inhibitors, beta-blockers and mineralocorticoid receptor antagonists. Thankfully, heart failure specialist nurses reach an additional 20% of all patients, so that currently in England and Wales, around 80% of patients admitted to a National Health Service (NHS) hospital with heart failure are seen by either a cardiologist or a specialist nurse.
The echocardiographic data collected in the national audit are not detailed, but it shows that 70% have obvious LV systolic dysfunction. Valve disease is very common (over 30% of cases), but isolated diastolic dysfunction is only recorded for around 10% of cases.
The strategic context
It is clear that we are facing serious challenges in delivering world class care to all patients with heart failure. The National Health Service’s current strategy, as outlined in The Five Year Forward View (7), is to move care closer to patient’s homes, to use technology to support better care and a better experience of that care and to support primary care in taking up a lot of the work that is currently done in hospital. This is a challenging time financially in which to enact such changes.
Guidelines and Quality Standards from NICE
Thankfully, the National Institute for Health and Care Excellence (NICE) has issued clear guidance to the NHS in England as to what good care looks like for both chronic and acute (hospitalised) heart failure. It has also issued Quality Standards so that health care services, commissioners, patients and the public can judge the quality of care using a small number of carefully chosen metrics.
NICE issued guidance on chronic heart failure in 2003 and updated this in 2010 (8) (and is currently updating this again). For acute heart failure, it issued its first guidance in 2014 (9). The relevant Quality Standards were issued in 2011 for chronic heart failure (updated in 2016) (10) and in 2015, for acute heart failure (11).
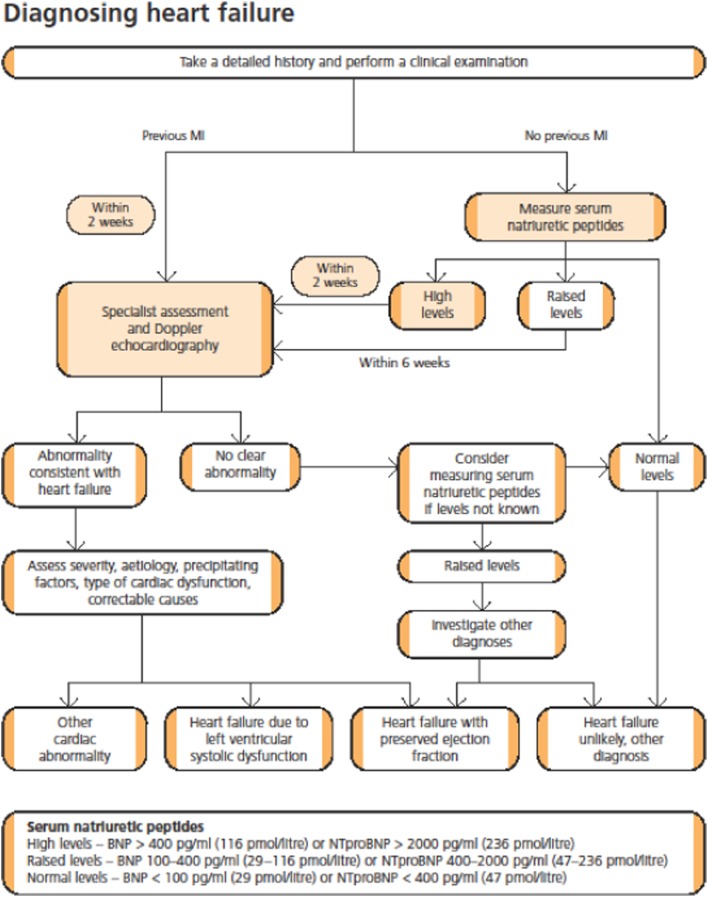
For chronic heart failure, people with suspected heart failure should have an echocardiogram AND specialist assessment. This confirms the key role of echocardiography in the diagnostic work-up of heart failure. If the patient has had a previous myocardial infarction or has a very high level of serum natriuretic peptides, then the echocardiogram and assessment need to be delivered within 2 weeks (Fig. 1) (8). Only some English hospitals can reach this benchmark currently. NICE does not stipulate the location of the imaging – leaving this up to local services to determine whether community- or hospital-based facilities are the more appropriate.
Figure 1.
Algorithm summarising the recommendations for the diagnosis of heart failure (8). Reproduced from National Guideline Centre (2010) chronic heart failure: the management of chronic heart failure in adults in primary and secondary care, Clinical Guideline 108, Published by the National Guidelines Centre at The Royal College of Physicians, 11 St Andrews Place, Regent’s Park, London, NW11 4LE. Copyright 2010 NGC. Reproduced by permission.
For acute heart failure – when the patient’s symptoms are so severe they require to be hospitalised – new cases should have a measurement of natriuretic peptide in the emergency room or acute admissions unit, and if this elevated and heart failure is suspected, then an echocardiogram would be performed within 48 h of admission (irrespective of whether it is the weekend or not). Also, such patients should have input from the specialist heart failure team within 24 h of admission. In practice, this means a cardiology or specialist nurse consultation as part of the post-admission ward round or process.
Another very challenging Quality Standard is that all patients discharged from hospital with a diagnosis of heart failure should have a follow-up clinical assessment by a member of the community- or hospital-based specialist heart failure team within 2 weeks of discharge. This is in recognition of the high risk of readmission or death during the first few weeks. My own work suggests that currently, even in the youngest age groups with least co-morbidity, only 70% receive such follow-up and the average wait for this is 6 weeks (12).
The challenges to delivery of good care
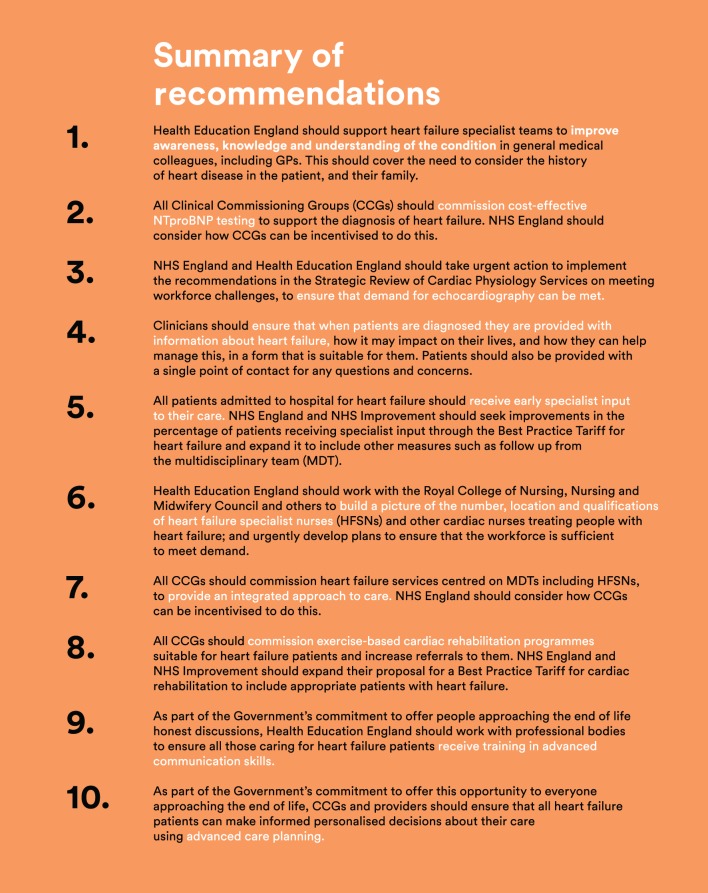
The challenges are clear. Recent qualitative work has confirmed that major issues remain regarding access to diagnostic tests in primary and secondary care, with huge variability from one part of the country to another (13). The All Party Parliamentary Group on Heart Disease (under the chairmanship of Stuart Andrew, MP for Pudsey, Horsey and Aireborough) has issued a report entitled ‘Focus on heart failure’ in response to evidence from an alliance of heart failure stakeholders (including health care professionals, the British Society for Heart Failure, the British Society of Echocardiography, patients and carers and the health care industry) (14). It makes 10 recommendations to improve care and to transform lives for those with heart failure. These are shown in Fig. 2.
Figure 2.
All Party Parliamentary Group on Heart Disease Focus on Heart Failure. Summary of recommendations (14). Reproduced by kind permission of the British Heart Foundation. Copyright 2016 British Heart Foundation.
In its submission, the Alliance for Heart Failure made several key points regarding echocardiography:
Echocardiography is a key test to support the diagnosis of heart failure and the national audit reports that is performed in 95% of hospitalised patients, although in many cases, this is unlikely to be performed within the recommended 48 h of admission.
NICE recommends the use of natriuretic peptides and the patient’s history to identify which patients should be referred by general practitioners for echocardiography and a specialist assessment and how rapidly. Access to natriuretic peptide testing is variable across England, and this hinders patient referral.
The NHS does not collate data nationally to confirm whether patients are being seen in accordance within the standards set by NICE (for either acute or chronic heart failure).
A postcode lottery in available clinical expertise affects the level and quality of treatment for patients with heart failure.
There is an acute shortage of echocardiographers in the United Kingdom – with only 44 individuals trained in the last year, with severe delays for many patients waiting for an echocardiogram.
Such a dearth of imaging expertise is threatening the delivery of good heart failure care across the United Kingdom. In its 2015 report, the British Cardiovascular Society and the Society for Cardiological Science and Technology recommended that models of delivery for cardiac physiology services are redesigned to improve clinical quality, affordability, patient experience and sustainability, including providing services in the community closer to where patients live and providing urgent and emergency treatment as soon as it is needed to return patients to health (15). Additionally, the report highlighted the need for urgent action to address the ‘considerable shortfall’ in the current cardiac physiology workforce, which is inadequate to meet current demand and with marked variations in access to cardiac physiology investigations and significant waiting lists in some areas. Without a strategic plan locally and nationally, it is likely that these shortages will increasingly affect service quality and timeliness as time goes on.
Conclusion
Heart failure is an epidemic that is upon us. It is clear what good care looks like, and when this is delivered, patients and their families can experience good results. Echocardiography is one of the key investigations to underpin a diagnosis of heart failure and to ensure the correct management plan is put into place. However, the current manpower issues for echocardiography are a major hurdle that must be overcome if the NHS can deliver the quality of care that NICE, health care professionals and patients demand.
Footnote
This review is based on the National BSE Invited Lecture, presented by Prof Martin R Cowie at the 2016 BSE Annual Clinical and Scientific Meeting, November 2016, London, UK.
Disclaimer
Prof Cowie is a Non-Executive Director of the National Institute for Health and Care Excellence, but the opinions expressed in this article are his own, and should not be taken to represent the official position of NICE.
Declaration of interest
The author declares that there is no conflict of interest that could be perceived as prejudicing the impartiality of this review. Prof Cowie has received consultancy fees from Roche Diagnostics.
Funding
This work did not receive any specific grant from any funding agency in the public, commercial, or not-for-profit sector.
References
- 1.Ambrosy AP, Fonarow GC, Butler J, Chioncel O, Greene SJ, Vaduganathan M, Nodari S, Lam CS, Sato N, Shah AN, et al. 2014. The global health and economic burden of hospitalizations for heart failure. Lessons learned from hospitalized heart failure registries. Journal of the American College of Cardiology 63 1123–1133. ( 10.1016/j.jacc.2013.11.053) [DOI] [PubMed] [Google Scholar]
- 2.Townsend N, Bhatnagar P, Wilkins E, Wickramasinghe K, Rayner M. 2015. Cardiovascular disease statistics. London: British Heart Foundation; (available at: https://www.bhf.org.uk/publications/statistics/cvd-stats-2015). Accessed on 20 November 2016 [Google Scholar]
- 3.Braunschweig F, Cowie MR, Auricchio A. 2011. What are the costs of heart failure? Europace 13 (Supplement 2) ii13–ii17. ( 10.1093/europace/eur081) [DOI] [PubMed] [Google Scholar]
- 4.Cowie MR, Wood DA, Coats AJ. 1999. Incidence and aetiology of heart failure: a population-based study. European Heart Journal 20 421–428. ( 10.1053/euhj.1998.1280) [DOI] [PubMed] [Google Scholar]
- 5.Fox KF, Cowie MR, Wood DA, Coats AJ, Gibbs JS, Underwood SR, Turner RM, Poole-Wilson PA, Davies SW, Sutton GC. 2001. Coronary artery disease as the cause of incident heart failure in the population. European Heart Journal 22 228–236. ( 10.1053/euhj.2000.2289) [DOI] [PubMed] [Google Scholar]
- 6.National Heart Failure Audit 2014/15. National Institute for Cardiovascular Outcomes Research (NICOR), Institute of Cardiovascular Science, University College London. (available at: https://www.ucl.ac.uk/nicor/audits/heartfailure/documents/annualreports/annual_report_2014_15_v2). Accessed on 20 November 2016. [Google Scholar]
- 7.NHS Five Year Forward View. NHS England, October 2014. (available at: https://www.england.nhs.uk/wp-content/uploads/2014/10/5yfv-web.pdf). Accessed on 20 November 2016.
- 8.National Clinical Guideline Centre 2010 Chronic heart failure: the management of chronic heart failure in adults in primary and secondary care. London, UK: National Clinical Guideline Centre; (available at: https://www.nice.org.uk/guidance/cg108/evidence/full-guideline-136060525). Accessed on 20 November 2016. [Google Scholar]
- 9.Acute heart failure: diagnosis and management (CG187). (available at https://www.nice.org.uk/guidance/cg187). Accessed on 20 November 2016.
- 10.Quality Standards for Chronic Heart Failure (QS9). (available at: https://www.nice.org.uk/guidance/qs9). Accessed on 20 November 2016.
- 11.Quality Standards for Acute Heart Failure (QS103). (available at: https://www.nice.org.uk/guidance/qs103). Accessed on 20 November 2016.
- 12.Bottle A, Goudie R, Bell D, Aylin P, Cowie MR. 2016. Use of hospital services by age and comorbidity after an index heart failure admission in England; an observational study. BMJ Open 6 e010669( 10.1136/bmjopen-2015-010669) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hancock HC, Close H, Fuat A, Murphy JJ, Hungin AP, Mason JM. 2014. Barriers to accurate diagnosis and effective management of heart failure have not changed in the past 10 years; a qualitative study and national survey. BMJ Open 4 e003866 ( 10.1136/bmjopen-2013-003866) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.All Party Parliamentary Group on Heart Disease 2016 Focus on heart failure: 10 recommendations to improve care and transform lives, September 2016. (available at: https://www.bhf.org.uk/-/media/files/campaigning/appg-on-heart-disease-focus-on-heart-failure-report.pdf). Accessed on 20 November 2016.
- 15.British Cardiovascular Society and Society for Cardiological Science and Technology 2015 Strategic review of cardiac physiological services in England: Final Report, May 2015. (available at: http://www.bcs.com/documents/SRCPS_Final_Report_12052015_2.pdf). Accessed on 20 November 2016.



 This work is licensed under a
This work is licensed under a