Dear Editor
Frontal fibrosing alopecia (FFA) is considered a variant of lichen planopilaris affecting mainly postmenopausal women. A progressive frontal or frontotemporal symmetric band of alopecia is the usual presentation, with eyebrows being commonly involved [1]. Currently, several authors consider FFA as a generalized skin condition, and many features other than hair loss have been associated with the disease, including facial papules [2]. Facial papules as a sign of facial vellus hair follicle involvement in FFA was first recognized by Abbas et al. [3] in 2007 and was later confirmed by Donati et al. [4].
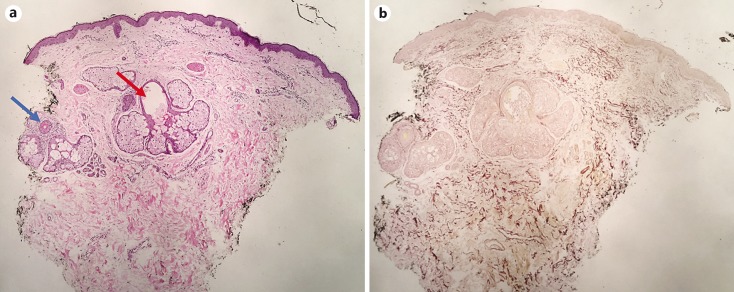
In a current ongoing study, our group observed that histopathological features of facial papules might not be limited to perifollicular inflammation. Our findings include variable vellus hair follicle involvement, elastic fiber involvement, and preserved sebaceous glands (Fig. 1) (unpublished data). Due to the effects of oral isotretinoin over sebaceous glands and previous studies reporting a possible role on the therapeutic regimen of FFA [5,6], we opted to use this drug in the treatment of 3 patients with FFA with prominent facial papules.
Fig. 1.
a Vertical section of a punch biopsy from a facial papule of Patient 1, revealing preserved sebaceous glands with a dilated duct (red arrow). Involvement of vellus hair by a mild lymphocytic inflammatory infiltrate can also be noted (blue arrow). HE. ×10. Colors refer to the online version only. b Orcein staining demonstrating a mild reduction and fragmentation of elastic fibers in the reticular dermis surrounding the sebaceous unit.
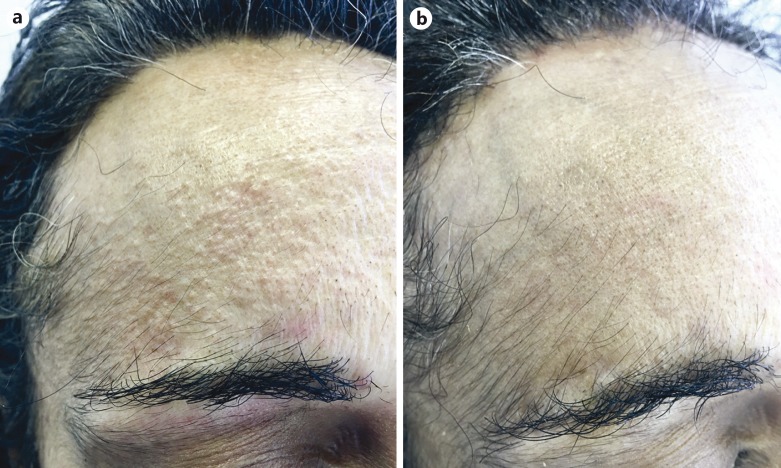
All patients were female, biopsy-confirmed cases of FFA, with the age range 49–53 years. Clinical information, concurrent, and previous treatments are presented in Table 1. All patients were started on the dosage of 20 mg/day of oral isotretinoin for the first month, which was then titrated to 0.5 mg/kg/day for the following 2 months (40 mg/day in all 3 patients). The patients were seen monthly for isotretinoin laboratory monitoring and, at the end of the third month, on a visit scheduled to evaluate FFA treatment efficacy. At the end of the first month, a remarkable improvement was noted, with a reduction in the number and size of facial papules. Patients reported perceiving that by the second week of treatment, the aspect of their facial skin had already considerably improved. At the end of the third month, facial papules had completely disappeared or were considered minimal (Fig. 2). The patients did not show a significant progression of FFA, and all reported decreased pruritus. However, signs of disease activity were still present over the hairline in all 3 patients, namely perifollicular erythema and scaling. Isotretinoin was then discontinued and hydroxychloroquine 400 mg/day was introduced.
Table 1.
Clinical information, previous and concurrent treatments
| Patient | Age, years | Gender | Postmenopausal | Previous treatments | Concurrent treatments (besides oral isotretinoin) |
|---|---|---|---|---|---|
| 1 | 49 | F | No | None | Finasteride 5 mg/day Tacrolimus 0.3% lotion (eyebrows and hairline) Triamcinolone injections eyebrows and hairline) |
| 2 | 49 | F | Yes | Doxycycline 100 mg/day Tacrolimus 0.1% (face) Triamcinolone injections (eyebrows and hairline) |
Finasteride 5 mg/day Clobetasol 0.05% gel (hairline) |
| 3 | 53 | F | Yes | None | Finasteride 5 mg/day Tacrolimus 0.3% lotion (eyebrows and hairline) |
Fig. 2.
Clinical picture of Patient 1 before (a) and after 3 months (b) of treatment with oral isotretinoin.
Facial papules are a characteristic feature of FFA, being present in 14% of the patients, according to a large multicenter study [7]. They may be discrete and even go unnoticed but can be a source of distress in patients with severe presentation. To date, there are no effective treatments described for facial papules in FFA. According to our histopathological findings (unpublished data), we speculate that perifollicular inflammation is not alone responsible for facial papule formation. Possibly, other factors involving elastic fibers and sebaceous glands contribute to perifollicular architecture derangement and the formation of papules. The dramatic response observed after isotretinoin therapy may corroborate this idea. We believe that the improvement of facial papules was due, at least in part, to sebaceous gland atrophy, a well-known effect of the drug [6]. Although it is not possible to exclude any role of concurrent systemic and topical treatments, the temporal relation between the introduction of oral isotretinoin and the disappearance of the lesions is remarkable. In addition, we have never observed such a response in our practice in FFA patients using other treatments and we are unaware of studies reporting similar results. Persistence of inflammatory signs over the hairline after 3 months might represent drug failure to control scalp disease or too short follow-up.
In conclusion, our observation offers a possibility of treatment for facial papules in FFA patients. Further studies with a greater number of patients are necessary to confirm our observations and to better evaluate dosage and treatment duration. Long-term follow-up is also necessary, considering that isotretinoin-induced sebaceous gland atrophy is not permanent.
Statement of Ethics
All patients have given their consent for their details to be described in this paper.
Disclosure Statement
The authors have no conflicts of interest to disclose.
References
- 1.Pirmez R, Duque-Estrada B, Donati A, Campos-do-Carmo G, Valente NS, Romiti R, Sodré CT, Tosti A. Clinical and dermoscopic features of lichen planus pigmentosus in 37 patients with frontal fibrosing alopecia. Br J Dermatol. 2016;175:1387–1390. doi: 10.1111/bjd.14722. [DOI] [PubMed] [Google Scholar]
- 2.Pirmez R, Donati A, Valente NS, et al. Glabellar red dots in frontal fibrosing alopecia: a further clinical sign of vellus follicle involvement. Br J Dermatol. 2014;170:745–746. doi: 10.1111/bjd.12683. [DOI] [PubMed] [Google Scholar]
- 3.Abbas O, Chedraoui A, Ghosn S. Frontal fibrosing alopecia presenting with components of Piccardi-Lassueur-Graham-Little syndrome. J Am Acad Dermatol. 2007;57:S15–S18. doi: 10.1016/j.jaad.2006.11.010. [DOI] [PubMed] [Google Scholar]
- 4.Donati A, Molina L, Doche I, et al. Facial papules in frontal fibrosing alopecia: evidence of vellus follicle involvement. Arch Dermatol. 2011;147:1424–1427. doi: 10.1001/archdermatol.2011.321. [DOI] [PubMed] [Google Scholar]
- 5.Tan KT, Messenger AG. Frontal fibrosing alopecia: clinical presentations and prognosis. Br J Dermatol. 2009;160:75–79. doi: 10.1111/j.1365-2133.2008.08861.x. [DOI] [PubMed] [Google Scholar]
- 6.Rademaker M. Isotretinoin: dose, duration and relapse. What does 30 years of usage tell us? Australas J Dermatol. 2013;54:157–162. doi: 10.1111/j.1440-0960.2012.00947.x. [DOI] [PubMed] [Google Scholar]
- 7.Vañó-Galván S, Molina-Ruiz AM, Serrano-Falcón C, et al. Frontal fibrosing alopecia: a multicenter review of 355 patients. J Am Acad Dermatol. 2014;70:670–678. doi: 10.1016/j.jaad.2013.12.003. [DOI] [PubMed] [Google Scholar]