Abstract
Nail dermoscopy was initially used only in the assessment of nail pigmentation, but now it is widely utilized for the evaluation of many nail disorders. In daily practice, dermoscopy may confirm clinical diagnoses and guides in the management of nail diseases and treatments, permitting a better visualization of symptoms. Dry dermoscopy is required for evaluation of the nail plate surface, while gel as an interface is necessary for assessment of nail pigmentation and onycholysis, as well as for the evaluation of the distal nail margin. In this review, we describe the dermoscopic features of the most important nail disorders, looking at the different areas of the nail. Dermatoscopic changes that usually accompany specific nail diseases are also reviewed.
Keywords: Dermoscopy, Onychoscopy, Onycholysis, Splinter hemorrhages, Capillary alterations, Subungual hyperkeratosis, Melanonychia, Nail tumor, Hyponychium
Introduction
Nail dermoscopy has initially been used for the assessment of nail pigmentation, but its utilization has expanded for the diagnosis of all nail disorders; it became a routine diagnostic instrument, as its reveals helpful information. Dermoscopy can be applied to all visible parts of the nail unit, and even the nail matrix can be studied, in conjunction with intraoperative methods.
With dermoscopy (onychoscopy), many nail signs can be magnified and combined with clinical examination to reach a diagnosis. The nail is visible as a whole only at ×10 magnification, but observation can be improved with magnifications ranging from ×20 to ×70, moving the lens back and forth and transversally. In most cases, nail dermoscopy only permits a better visualization of symptoms already evident to the naked eye [1].
Onychoscopy can be performed dry or with ultrasound gel. The most important rule is to use dry dermoscopy to study the nail plate surface and to apply gel as an interface when the evaluation includes nail pigmentation, onycholysis, and the distal nail margin. Gel is necessary also for looking at the skin of the periungual folds and hyponychium.
Onychoscopy of the Nail Folds
Proximal Nail Fold Capillary Alterations
Nail fold capillaroscopy is a valid technique used to study patients with connective tissue diseases, even if nowadays dermoscopy has replaced it thanks to its better manageability [2]. Dermoscopic observation of the nail fold capillaries is usually made on the fourth or the third finger, avoiding the thumb, whose skin has a lower transparency. Specific capillary abnormalities include 3 diagnostic patterns: (1) a normal pattern, (2) scleroderma, and (3) a nonspecific pattern. The normal capillaroscopy pattern evidences normal skin transparency, a hairpin-shaped morphology of the capillaries, morphological/structural homogeneity, 10–12 capillaries/mm, 1 dermal papilla, a diameter of the capillary branches <20 mm, and lack of morphological atypia. The scleroderma pattern is characterized by giant capillaries, microhemorrhages, capillary loss, the presence of avascular areas, and angiogenesis [3]. Capillary alterations may sometimes precede the symptoms of a connective tissue disease. Capillaroscopy can also be used to monitor response to therapy.
Systemic Sclerosis
Capillaroscopy is considered the best predictable value for disease development, and it has been observed to precede symptoms by many years [4]. Microangiopathy and decreased peripheral blood perfusion explain the dermoscopic pattern of systemic sclerosis.
There are 3 different scleroderma patterns in systemic sclerosis: (1) early (with a limited number of giant capillaries and rarely microhemorrhages), (2) active (with numerous giant capillaries, frequent microhemorrhages, and a moderate reduction in capillary density), and (3) late (with marked loss of capillaries and evidence of extensive avascular areas, as well as with ramified or bushy neoangiogenesis) [4].
Dermatomyositis
The typical alterations visible with capillaroscopy are present in 75% of patients with dermatomyositis and can involve several digits. Capillaroscopy shows the scleroderma pattern, characterized by giant capillaries, microhemorrhages, and a complete change of the microvascular architecture. The most typical alteration is a tortuous and arborescent aspect of the capillaries (Fig. 1) [5]. The Raynaud phenomenon is frequently associated with capillary changes. Capillaroscopic features may help to evaluate disease activity.
Fig. 1.

Capillaroscopy in dermatomyositis: giant capillaries with arborescent appearance and microhemorrhages. Magnification, ×50.
Systemic Lupus Erythematosus
In systemic lupus erythematosus patients, capillaroscopic alterations have a lower specificity, and they are characterized by tortuous loops – sometimes with a serpiginous appearance, stretched loops, and an odd shape – and greater visibility of the subpapillary venous plexus, which has an increased diameter (Fig. 2) [6].
Fig. 2.

Capillaroscopy in systemic lupus erythematosus: tortuous, oddly shaped loops with serpiginous appearance. Magnification, ×20.
Masses in the Proximal and Lateral Nail Folds
Pyogenic Granuloma
Pyogenic granuloma is a benign vascular disease that frequently occurs in the periungual tissues, and more rarely in the nail bed. Its etiology includes trauma, ingrowing nails, drugs, peripheral nerve injury, and inflammatory diseases [7]. It clinically appears as a bleeding vascular nodule.
The principal onychoscopic aspect of a pyogenic granuloma is the vascular pattern, characterized by red discoloration with a milky-red veil and a regular pattern of the vessels (Fig. 3). Due to magnification and bleaching, vessels appear as dots at low magnification and as regular lines at higher enlargement. The color is red, darker at the center of the lesion and paler at the periphery. Necrotic areas, brown in color, can be present.
Fig. 3.

Dermoscopy of pyogenic granuloma: reddish mass with irregular vessels and white central area. Magnification, ×10.
In our experience, dermoscopy is not diagnostic for pyogenic granuloma of the nail. While the location of pyogenic granulomas in the lateral and proximal nail folds is helpful for diagnosis, masses located in the nail bed should be differentiated from malignant tumors, such as squamous cell carcinoma and melanoma. In these cases, a differential diagnosis requires pathology, as onychoscopy does not give specific clues.
Warts
Even if a diagnosis of warts is essentially clinical, nail dermoscopy can be used to magnify small periungual warts not evident to the naked eye. Dry dermoscopy typically shows well-demarcated hyperkeratotic and rough lesions with regular micropapules, as well as a collarette and small black dots, which correspond to the dilated capillaries of the papillary dermis (Fig. 4). The most important differential diagnosis is from Bowen disease (in situ squamous cell carcinoma), which clinically appears as a periungual or subungual verrucous plaque, typically associated with lateral onycholysis and a band of melanonychia in the adjacent nail plate [8].
Fig. 4.

Dry dermoscopy of periungual warts: hyperkeratotic and rough lesion with small black dots. Magnification, ×10.
Dorsal Pterygium
Dorsal pterygium is the result of irreversible damage to part of the nail matrix and may be a consequence of inflammatory diseases that destroy part of the nail matrix – most commonly nail lichen planus, but also bullous diseases – or may follow surgical or accidental traumas. The destruction of part of the matrix allows adhesion of the skin of the dorsum of the digit to the nail bed, with formation of a V-shaped extension of the proximal nail fold that splits the nail plate in 2 parts. Dermoscopy of the dorsal pterygium shows that it is formed by skin and continues with the skin of the proximal nail fold (Fig. 5). The color is pink-red with elongated capillaries in early lesions, while is white in longstanding lesions, due to fibrosis.
Fig. 5.

Dry dermoscopy easily enhances visualization of the longitudinal fissures of the nail plate due to lichen planus with partial anonychia and dorsal pterygium. Magnification, ×10.
Alterations of the Nail Plate
Surface
Alterations of the nail plate reflect damage to the proximal nail matrix, which can be mild or severe. Dry dermoscopy is necessary.
Trachyonychia
Trachyonychia or “20-nail dystrophy” is a benign disease where the nails appear rough, as if sandpapered in a longitudinal direction. It can be idiopathic or caused by inflammatory disorders that involve the proximal matrix, such as alopecia areata, psoriasis, or lichen planus. On onychoscopy, the nail plate shows multiple fine and superficial longitudinal fissures covered by thin scales (Fig. 6). In the “shiny” variety of trachyonychia, the nail shows superficial ridging and a myriad of small geometrical pits.
Fig. 6.

Dry dermoscopy enhances visualization of the typical surface nail plate alterations with recent trachyonychia in the proximal nail plate. Magnification, ×10.
Longitudinal Fissuring and Distal Splitting
When occurring in several/all nails, these are the typical signs of nail matrix lichen planus: the nails are thinned and show longitudinal ridging and fissuring with distal splitting. Dermoscopy shows multiple deep longitudinal fissures reaching the distal part of the nail as well as partial absence of the nail plate.
Onychoscopy is not diagnostic for nail lichen planus; instead, a nail biopsy is recommended to confirm the diagnosis. Dermoscopy is useful for the follow-up of nail lichen planus, as it allows observation of the proximal nail plate, where lichen planus emerges from the nail fold; it shows the regrowing nail plate and permits evaluating the response to therapy at an early stage.
Pitting
Pits are small punctate depressions of the nail plate surface that result from defective keratinization of the foci of cells of the proximal nail matrix. Pitting is commonly seen in fingernails in patients with nail psoriasis and in those with alopecia areata. Punctate nail plate depressions vary in size and distribution in the 2 diseases. Visible with dry dermoscopy, the pits of psoriasis appear large, deep, and irregular in shape, size, and distribution and are often covered by large scales (Fig. 7). Onycholysis with salmon borders is often associated with it. The pits of alopecia areata are regular, superficial, and homogeneously distributed along geometrical lines (“geometrical pitting”).
Fig. 7.

Dry dermoscopy of nail psoriasis with irregular pitting. Magnification, ×20.
Nail Fragility
This condition is very common and typically affects the fingernails of adult women. The nail plate is fragile, with typical surface alterations well visible by dry dermoscopy. There are 3 different types of nail fragility that show different aspects on onychoscopy. The first and most common form is lamellar onychoschizia, where dermoscopy reveals horizontal splitting of several layers of the distal plate with irregular edges (Fig. 8). In the second type, onychorrhexis, dermoscopy shows multiple longitudinal fissures of the distal edge. In the third form, keratin degranulation, dermoscopy shows small regular scales firmly attached to the distal part of the nail plate (Fig. 9).
Fig. 8.

Lamellar onychoschizia of a fingernail: the distal portion of the nail plate peels off in layers, and horizontal and vertical breakages are easily visible with dry dermoscopy. Magnification, ×20.
Fig. 9.

Dry dermoscopy shows thin fissures on the nail plate and opaqueness of the white spots of nail fragility due to superficial degranulation of the nail plate from chemicals. Magnification, ×20.
A differential diagnosis from white superficial onychomycosis is possible due to the regular aspect of the scales, in contrast with white onychomycosis, where the spots are irregularly distributed along the nail. A differential diagnosis from true leukonychia is easy with apposition of gel to the nail plate, which, in the case of nail fragility, induces the disappearance of the scales.
Nail plate dermoscopy can also be used to monitor response to treatment for nail fragility [9].
Color
Alterations in nail color can be due to deposition of a pigment on the nail plate (exogenous pigmentation), due to pigmentation of the nail bed, or due to production of pigment from the nail matrix. With dermoscopy, a differential diagnosis is possible in most of the cases.
Leukonychia
Dermoscopy permits close observation of leukonychia and allows distinguishing true leukonychia from apparent leukonychia and pseudoleukonychia. In true leukonychia, the pigmentation is localized within the nail plate and results from altered keratinization of the distal nail matrix, whereas in apparent leukonychia the discoloration originates in the nail bed and in pseudoleukonychia it has an external origin.
True leukonychia may be punctate, transverse, or, rarely, total, and it is secondary to repetitive traumas with production of white bands/spots that move distally with nail growth (Fig. 10) [10]. Dermoscopy shows 1 or more white dots or transverse bands inside the plate, with a normally smooth and transparent nail plate surface. In transverse leukonychia, the white lines run parallel to the proximal nail fold and the space separating each transverse band indicates the intervals between traumas. Application of gel does not change the white appearance.
Fig. 10.

Dermoscopy with gel shows white bands within the nail plate in transverse leukonychia of the right toenail. Magnification, ×20.
Proximal subungual onychomycosis produces a white discoloration below the nail plate in the lunula, while the remaining nail plate is normal (Fig. 11). In white superficial onychomycosis, dermoscopy shows a nail plate with several small white-to-yellow opaque and friable patches. Dermoscopy shows single or multiple opaque white irregular spots of the nail plate surface (Fig. 12).
Fig. 11.

The white area in the lunula of a proximal subungual onychomycosis is well visible by dermoscopy. Magnification, ×20.
Fig. 12.

Dermoscopy shows a nail plate with several small white, opaque, and friable patches in white superficial onychomycosis. Magnification, ×20.
Leukonychia can also be longitudinal with multiple or single bands. Multiple bands alternating with red bands are typical of Darier and Hailey-Hailey disease, while a single band of longitudinal leukonychia can be a possible presentation of onychopapilloma [11].
Green Discoloration
A green discoloration of the nail plate associated with onycholysis or chronic paronychia can be caused by Pseudomonas aeruginosa infection, where the bacterium colonizes the subungual space or the dorsal nail plate, producing the yellow-green pigment pyocyanin [12]. Onychoscopy shows the yellow-green discoloration and its localization. In green nails due to chronic paronychia, the green color is adherent to the nail surface in close proximity with the proximal nail fold, which is edematous and without cuticle. The discoloration involves the lateral nail and is more evident proximally; it does not have a longitudinal shape and is associated with an irregular nail plate surface. Scraping the nail plate with a curette removes the pigment.
In green nails due to onycholysis, dermoscopy permits observing the border of the subungual pigmentation, where the color typically fades into pale green at the margin of the detachment (Fig. 13). After clipping away the detached nail plate, a pale green-yellow pigmentation is evident at the bottom of the nail plate and on the nail bed.
Fig. 13.

Dermoscopy shows a bright green color that fades to yellow in case of onycholysis. Note the border of the subungual pigmentation, where the color typically fades into pale green at the margin of detachment. Magnification, ×10.
Differential diagnosis includes chemical exposure to solutions containing pyocyanin or pyoverdine [13]; the clinical history is suggestive, and the presence of paronychia and onycholysis as well.
Erythronychia
The term “erythronychia” describes a red nail discoloration that can have a round or irregular shape or present as a longitudinal band originating from the lunula and running along the nail until the distal nail plate. The corresponding nail plate may be normal or present longitudinal fissures and a distal subungual mass. Several benign tumors may be responsible for it.
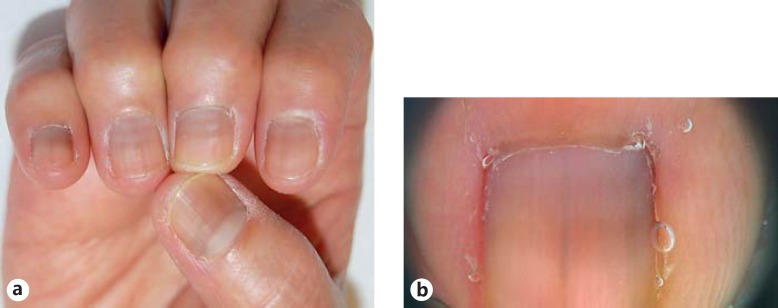
Onychopapilloma. Onychopapilloma is a benign neoplasm that arises from the distal matrix/proximal nail bed, inducing a band of longitudinal erythronychia. Onychoscopy shows a longitudinal red band, starting from the lunula and reaching to the distal margin, often associated with splinter hemorrhages (Fig. 14). The distal nail plate may show a fissure and a subungual filiform hyperkeratotic mass. An evident subungual mass with onycholysis can be a sign of onychopapilloma of a bigger size. Removal of the detached nail plate reveals hyponychial hyperkeratosis [14]. Tosti et al. [11] performed a retrospective study analyzing the clinical, dermoscopic, and pathologic features of 47 patients with onychopapilloma. They observed that, dermoscopically, the distal edge showed a keratotic subungual mass in correspondence to the streak in all cases, and that splinter hemorrhages could be the only onychoscopic sign. Dermoscopy permits a differential diagnosis from onychomatricoma, of which the honeycomb aspect of the distal part of the nail plate is diagnostic.
Fig. 14.
Dermoscopy of onychopapilloma presenting as a longitudinal red band associated with splinter hemorrhages. Magnification, ×10.
Glomus Tumor. Glomus tumor is a painful benign nail tumor occurring most commonly in the subungual area of the first and second fingernails. The classic triad of symptoms includes intense paroxysmal pain, pinpoint tenderness, and cold sensitivity [15]. Glomus tumor is usually not visible clinically, due to its small dimensions, or it may appear as an erythematous marking suggestive of vascular abnormalities. Dermoscopy with gel can be very useful to obtain better visualization of the mass; the tumor appears as a deep red-purple discolored area with blurred borders (Fig. 15), or as a band of longitudinal erythronychia that does not usually reach the distal margin [16]. The intensity of the red color contrasts with the pale pink color of the surrounding nail bed and with the white color of the lunula [17]. Moreover, dermoscopy could indicate the site of the tumor, because the more distal within the nail bed the tumor is, the more diffuse the erythronychia and the less pronounced the integrity of the nail plate. In cases of a bigger mass, onycholysis could be present, as well as nail plate thinning and fissuring due to matrix compression. Nail plate dermoscopy can show the presence of vascular structures, too, evident as small red ramified vessels. A new tool for the diagnosis of glomus tumor is the “pink glow” sign visible on UV light, where a pinkish glow suggests the vascular nature of the tumor [18]. Intraoperative onychoscopy of the nail matrix and bed after nail plate removal aids in tumor localization and in visualization of the vascular pattern of the lesion, which appears as ramified telangiectasis over a blue background [19]. This method helps in the delimitation of surgical margins. Nail bed onychoscopy may also show residual macroscopic tumor foci [16].
Fig. 15.

Dermoscopy of a glomus tumor with a deep red-purple subungual mass. Magnification, ×20.
Darier Disease. In Darier disease, nail dermoscopy shows alternance of red and white streaks that may be associated with nail plate thinning (Fig. 16). Splinter hemorrhages may be visible, associated with distal notches on the nail plate.
Fig. 16.

Dry dermoscopy of the third fingernail of a left hand with alternance of multiple and parallel red and white bands in Darier disease. Magnification, ×10.
Yellow Discoloration
A yellowish discoloration of the nail plate evident on dermoscopy can be seen in 2 different conditions: onychomycosis and nail psoriasis. In nail discoloration with onycholysis, subungual hyperkeratosis is the most important clinical sign of distal subungual onychomycosis. Dermoscopy shows white-yellow longitudinal striae in the onycholytic nail plate (Fig. 17), and the overall appearance of the affected nail plate with bands of fading colors resembles the aurora borealis (aurora borealis pattern) [20]. In dermatophytoma, there is a subungual accumulation of hyphae and scales that dermoscopically appears as a round-shaped yellow-orange patch in the mid nail bed, connected by a thin narrow channel to the distal edge of the nail plate (Fig. 18) [21].
Fig. 17.

Dermoscopic aspect of distal subungual onycholysis, which is yellow-whitish in color due to the colony's formation and corresponds to a pattern of longitudinal striae. Magnification, ×10.
Fig. 18.

Dermoscopy of dermatophytoma: subungual accumulation of dermatophytes and scales, presenting as a round yellow-orange subungual area, connected by a thin band to the distal edge of the nail plate. Magnification, ×10.
Nail psoriasis typically causes the “oil drop sign” or salmon patch, which appears as a circular translucent yellow-red area of discoloration in the middle of the nail or surrounding onycholysis.
Another cause of yellowish nail discoloration forming a longitudinal band can be onychomatricoma; however, in this tumor, longitudinal striae due to the tunnels of the digitations of the tumor and splinter hemorrhages are usually evident with dermoscopy, and observation of the distal thickened edge is diagnostic.
Red-Brown-Black Discoloration
Splinter Hemorrhages. These correspond to hemorrhages of blood capillaries of the nail bed which run longitudinally along the rows of the dermal papillae and clinically appear as 1 or more longitudinal red-to-brown striae, deep red in color and a few millimeters in length and located in the distal nail. Splinter hemorrhages are frequently due to trauma, but they may also be seen in nail psoriasis or onychomycosis, or they may be associated with nail tumor, i.e., onychopapilloma. Dermoscopy with gel enhances visualization of the longitudinal orientation of the red lines and allows observation of nail bed capillary dilations that precede rupture.
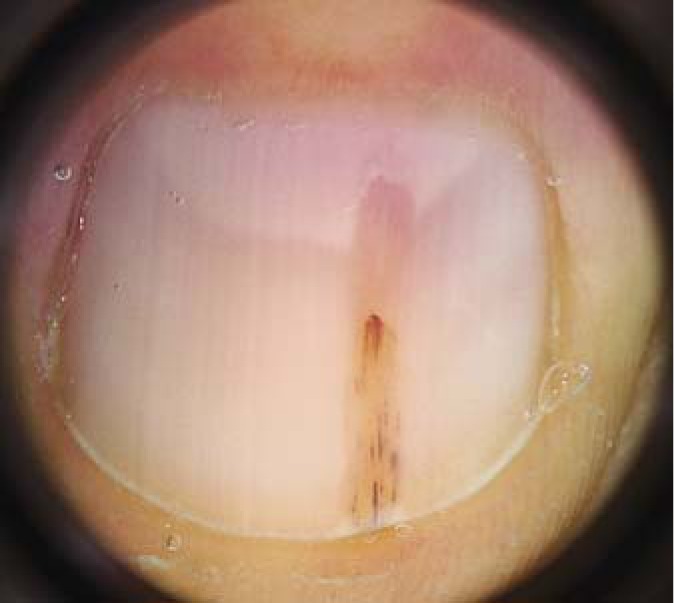
Subungual Hematoma. Subungual hematoma is the most common cause of brown-black nail pigmentation. Acute hematomas are very easy to diagnose, as the clinical history of a trauma explains the origin of the pigmentation. Chronic hematomas, on the other hand, are caused by repeated microtraumas that the patient is not aware of. In these cases, the patient or the practitioner notices a brown-black nail pigmentation of a toenail that should be differentiated from melanotic pigmentation, i.e., from nail melanoma. This is not always easy with the naked eye, since hematomas do not necessarily have a round shape but may be longitudinal or may involve the whole nail. The most important role of nail dermoscopy is that of allowing recognition of subungual hematoma, differentiating it from the frightening disease of longitudinal melanonychia [22]. Dermoscopy better defines the round shape of the hematoma and its homogeneous pigmentation, without the longitudinal lines that characterize melanonychia. The color of a hematoma depends on the time since the occurrence of the trauma. A recent hematoma is located deep under the plate and appears red-purple to black in color, with round margins at the proximal edge and with a streaked and filamentous distal end (Fig. 19) [23]. One or several red-black small round spots representing smaller blood extravasations may be present around. The new term “pseudopod” refers to the distal end of a nail hemorrhage [24]. Older lesions are more superficial, located in the ventral nail plate, roundish, red-brown in color, and often surrounded by multiple small blood globules of paler color or splinter hemorrhage globules (Fig. 19b).
Fig. 19.
Dermoscopy of a recent hematoma (a), presenting as a red-to-black discoloration of the fingernail and proximal fading of the red color, and of a late stage of the same subungual hematoma (b), presenting with a darker color. Magnification, ×10.
Melanonychia. The term melanonychia describes a black-brown pigmentation of the nail due to the presence of melanin within the nail plate. Usually, it appears as a longitudinal band that starts from the proximal margin extending to the distal margin of the nail, following the growth of the nail, or it involves the whole nail plate (total melanonychia). Melanonychia can occur because of melanocytic activation or because of melanocytic proliferation due to benign or malignant causes. Three steps are needed in the evaluation of melanonychia: (1) establishing whether the pigment is melanin or not; (2) determining whether the development of melanonychia is due to activation or proliferation of matrix melanocytes; and (3) assessing whether there is proliferation in order to determine whether the disease is benign or malignant [23].
(1) Dermoscopy is very useful for the first step. Generally, melanotic pigmentation is brown-black, and within the nail plate and the aspect is a longitudinal band, whereas exogenous pigmentation includes different substances that adhere to the nail plate and it does not usually have a longitudinal appearance. As already mentioned, common causes of amelanotic pigmentation are subungual hematoma, fungal melanonychia, and Pseudomonas infection.
(2) Help is provided by the number of digits that are involved: if more than 1 digit is affected, the first thought should be melanocytic activation, such as in drug-induced melanonychia, which appears with a gray background of the band with thin grayish regular and parallel lines (Fig. 20a, b).
Fig. 20.
a Clinical picture of multiple nails affected by melanonychia due to drugs. b Dermoscopy of melanocytic activation, with a gray background of the band and thin grayish regular and parallel lines. b Magnification, ×20.
(3) When melanonychia involves only 1 digit, a proliferative process has to be considered, and this poses the diagnostic dilemma over whether it has a benign or a malignant origin. The aspect of the band can be very different: the color can be more or less pronounced and homogeneous; the borders can be well defined or less sharp; and its width can range from a few millimeters to the entire nail plate. The corresponding nail plate can show some changes or be completely normal. Finally, a brown-black periungual pigmentation (Hutchinson sign) may be present. The first aspect to consider in case of longitudinal melanonychia due to proliferation is the age of the patient. Nail matrix nevi are typically seen in childhood, and they may be congenital or acquired. Nail melanoma in children is extremely rare [25,26,27]. Clinical and dermoscopic parameters used in adults are not valid for children [28]. Nail matrix nevi may be present at birth or may occur with age, more frequently in the thumb. Dermoscopic patterns that suggest a nevus are the presence of a brown background with longitudinal brown-to-black regular and parallel lines with regular spacing and thickness and, more important in children, black dots due to pigment accumulation in the nail plate (Fig. 21). These dots are black in color, with a regular size and shape (less than 0.1 mm), irregularly distributed along the lines, and sometime form a shallow pit at the periphery. At other times, it is possible to find them within the pigmented lines, often interrupting the lines. In most young patients, the dots will disappear over time. The authors explained the presence of dots as an accumulation of melanin derived from a cluster of nevus cells that migrate upward from the dermoepidermal junction. Fading of melanonychia accompanies the disappearance of the dots. These dots are then a sign of regression of a nevus and not a warning sign of a melanoma [29]. Dermoscopic patterns that may suggest a melanoma in children are the rapid evolution of a brown background with longitudinal brown-to-black lines with an irregular color, spacing, and thickness and ending abruptly. However, these features can also be seen in longitudinal melanonychia in children, and their specificity in youth is very low [30].
Fig. 21.

Dermoscopic pattern of a nevus in a 3-year-old child with the presence of a brown background with longitudinal brown-to-black irregular and parallel lines with irregular spacing and thickness. Magnification, ×20.
In adulthood, the use of dermoscopy in the evaluation of nail pigmentation began in 2007, when dermoscopic criteria suggestive of benign and malignant nail melanocyte lesions were proposed [31], but it was later shown that the technique is not always reliable in the management of pigmented nail lesions [32]. The clinical ABCDEF rule for nail pigmentation [33] should always be applied with dermoscopy [22] for diagnostic accuracy. Dermoscopic features suggestive of nail melanoma include a brown-to-black background of the band, with longitudinal lines irregular in their thickness, spacing, color, or parallelism (Fig. 22) [31]. However, this rule is not always reliable, as it is possible to find lines that are irregular in width or color also in benign lesions [31,34]. The conditions in which dermoscopy is not performable are thickened nails, blurred borders of the lesions, and a totally black nail plate [34]. A recent study [35] demonstrated a strong association between clinical and dermoscopic findings in nail band pigmentation, helping to distinguish whether a band is benign or malignant. The authors identify 3 important dermoscopic patterns that could help in this distinction: (1) the width of the band, involving more than two-thirds of the nail plate in melanoma; (2) the presence of a gray-to-black color; and (3) the presence of nail dystrophy, which increases the risk of detecting a nail melanoma 3 times. Dermoscopy of the hyponychium and periungual tissues permits discovering the micro-Hutchinson sign, a periungual pigmentation seen with a dermoscope but not with the naked eye that corresponds to the initial radial growth of melanoma into adjacent tissue. The micro-Hutchinson sign could be associated with a band of melanonychia or with amelanotic melanoma, characterized by the lack of melanin pigment. The clinical features of this type of melanoma are absence of the nail plate and nail dystrophy with nail bed hyperkeratosis or ulceration. The reliability of dermoscopy in the diagnosis of melanoma is particularly high in the presence of the micro-Hutchinson sign. Dermoscopy may be used to look at the pattern of pigmentation of the nail matrix [36], for which it has a high sensitivity and specificity. With an intraoperative method, a Brazilian group identified 4 dermoscopic patterns: (1) a regular gray pattern, typical of hypermelanosis; (2) a regular brown pattern, typical of benign melanocytic hyperplasia; (3) a regular brown pattern with globules or blotches, typical of melanocytic nevi; and (4) an irregular pattern, typical of melanoma. The use of an intraoperative procedure permitted selecting the best site for performing a biopsy [37]. The gold standard for a definitive diagnosis of nail pigmentation is histopathology [38,39].
Fig. 22.

High magnification of the dermoscopic features of nail melanoma, with a brown-to-black background of the band and longitudinal lines irregular in thickness, spacing, color, and parallelism. Magnification, ×20.
Fungal Melanonychia. One cause of black coloring of the nail is fungal melanonychia, caused by Trichophyton rubrum melanoid or by other non-dermatophyte fungi. Dermoscopy of fungal melanonychia reveals a brown or black irregular band associated with thick subungual hyperkeratosis with yellow and brown scales (Fig. 23) [40,41]. Additional dermoscopic features of fungal melanonychia include: multicolored pigmentation (yellow, brown, gray, black, or red), matt black pigmentation (lines, disrupted black linear pigmentation, or homogeneous areas), black pigment aggregates (seen as coarse granules and/or pigment clumps), and pigmentation that is wider at the distal than at the proximal edge, called the “black reverse triangle” [40,42].
Fig. 23.

Dermoscopy of fungal melanonychia with yellow streaks associated with homogeneous pigmentation and brown-black discoloration with irregular accumulation of black pigment and scales under the nail plate. Magnification, ×10.
Alterations of Nail Plate/Nail Bed Attachment (Onycholysis)
Onycholysis is described as detachment of the nail plate from the nail bed. It is not specific to any diseases, but it is frequently associated with the most frequent nail diseases, together with other dermoscopic signs. Due to the new space between the nail plate and the nail bed, air passes underneath, so the color of the nail plate changes from pink to white. Other pigments can spread under the nail plate, coloring it green (such as in Pseudomonas infection), yellow (such as in onychomycosis), or red (if hemosiderin deposition has occurred). Traumatic onycholysis, nail psoriasis, and onychomycosis are the principal diseases causing onycholysis in the toenails; dermoscopic observation of the proximal margin of the onycholytic area helps in the differential diagnosis.
Traumatic onycholysis is very common in the great toenails, and it is usually bilateral and symmetrical. With dermoscopy, the line of detachment of the plate from the bed appears linear, regular, and smooth and is surrounded by a normally pale pink bed, without hyperkeratosis (Fig. 24) [21]. The subungual space is usually whitish to yellow, and splinter hemorrhages can be present due to traumas.
Fig. 24.

Dermoscopy of the linear and regular margin of an onycholytic area due to traumatic onycholysis. Magnification, ×10.
In nail psoriasis, onycholysis is characterized by an erythematous border surrounding the distal edge of the detachment, by signs of nail bed inflammation, which on dermoscopy appear bright yellow, and by a slightly dented margin of the detachment (Fig. 25).
Fig. 25.

Dermoscopy of nail psoriasis with onycholysis presenting a slightly dented margin of the onycholytic area surrounded by a yellow-orange band and splinter hemorrhages and irregular pitting. Magnification, ×10.
In distal subungual onychomycosis, the detachment runs along the horny layer of the nail bed, which is thicker in the longitudinal furrows between the dermal creases; this explains the ragged border of the onycholysis with a jagged edge and sharp structures, directed to the proximal fold, named “spikes” [20].
Subungual Hyperkeratosis
Subungual hyperkeratosis is characterized by the accumulation of scales under the nail plate, which is detached and uplifted. It can be localized or diffuse over the whole width of the nail. It results from excessive proliferation of nail bed/hyponychium keratinocytes. Diffuse subungual hyperkeratosis is typically seen in psoriasis and distal subungual onychomycosis. A large study described a new pattern of subungual hyperkeratosis discovered in distal subungual onychomycosis, i.e., a “ruin appearance” of subungual hyperkeratosis on dermoscopy that corresponds to a fungal presence [43].
Alteration of the Distal Edge of the Nail
Dermoscopy of the free distal margin of the nail can allow diagnoses of some nail lesions. It allows distinguishing between nail thickening due to subungual hyperkeratosis and nail thickening due to thickening of the nail plate. In melanonychia, dermoscopy of the free edge of the distal nail plate helps to distinguish whether the pigment is produced by the proximal or the distal nail matrix. If the pigment is in the upper part of the free edge, the origin of the pigment is in the proximal nail matrix, whereas if the pigment is in the lower part of the free edge, the origin is in the distal nail matrix [44]. In onychopapilloma, the distal margin often shows a subungual filiform mass, while in onychomatricoma a characteristic aspect of the nail plate showing multiple holes is diagnostic (Fig. 26). These honeycomb holes correspond to longitudinal hollows that contain the digitations of the tumor within the nail plate. Other typical dermoscopic findings of this tumor include a yellowish discoloration with longitudinal striae due to the tunnels of the digitations of the tumor and splinter hemorrhages [45].
Fig. 26.

Typical dermoscopic aspect of onychomatricoma in the frontal view, with a honeycomb pattern. Magnification, ×10.
Dermoscopy of the Hyponychium
Dermoscopy of the hyponychium at high magnification is widely utilized to confirm the diagnosis of nail psoriasis, where it shows typical irregularly distributed, dilated, tortuous, and glomerulus-shaped capillaries [46]. Capillary density is positively correlated with disease severity and response to treatment. Hyponychium capillaries are better visualized with ×40 or higher magnifications, but they can also be seen with a handheld dermatoscope, through which they look like regular red dots [23].
Dermoscopy of the hyponychium and periungual tissue permits to evaluate the Hutchinson sign, due to the radial growth phase of nail melanoma into the adjacent tissue, characterized by its polychromia and asymmetry. Dermoscopy has a crucial role in finding the micro-Hutchinson sign, a periungual pigmentation seen with the dermoscope but not with the naked eye (Fig. 27).
Fig. 27.

Dermoscopy of periungual tissue with the micro-Hutchinson sign and longitudinal lines irregular in thickness, spacing, color, and parallelism in a melanoma. Magnification, ×20.
Conclusions
Nowadays, onychoscopy is used routinely, as it provides important information, providing specific criteria for the dermoscopic assessment of nail diseases. In collagen disorders, dermoscopy of the capillaries of the proximal nail fold is useful for the assessment of vascular injury and evaluation of therapeutic effects. Distinctive dermoscopic signs that are exclusive to distal subungual onychomycosis and to traumatic onycholysis have also been described and allow a differential diagnosis from psoriasis. Several nail tumors, such as onychopapilloma and onychomatricoma, are now easily diagnosed with dermoscopy.
Disclosure Statement
The authors declare no conflict of interest.
References
- 1.Piraccini BM, Bruni F, Starace M. Dermoscopy of non-skin cancer nail disorders. Dermatol Ther. 2012;25:594–602. doi: 10.1111/j.1529-8019.2012.01521.x. [DOI] [PubMed] [Google Scholar]
- 2.Hasegawa M. Dermoscopy findings of nail fold capillaries in connective tissue disease. J Dermatol. 2011;38:66–70. doi: 10.1111/j.1346-8138.2010.01092.x. [DOI] [PubMed] [Google Scholar]
- 3.Cutolo M, Sulli A, Secchi ME, Oliveri M, Pizzorni C. The contribution of capillaroscopy to the differential diagnosis of connective autoimmune diseases. Best Pract Res Clin Rheumatol. 2007;21:1093–1108. doi: 10.1016/j.berh.2007.10.001. [DOI] [PubMed] [Google Scholar]
- 4.Pizzorni C, Sulli A, Smith V, Lladó A, Paolino S, Cutolo M, Ruaro B. Capillaroscopy in 2016: new perspectives in systemic sclerosis. Acta Rheumatol Port. 2016;41:8–14. [PubMed] [Google Scholar]
- 5.Shenavandeh S, Zarei Nezhad M. Association of nailfold capillary changes with disease activity, clinical and laboratory findings in patients with dermatomyositis. Med J Islam Repub Iran. 2015;29:233. [PMC free article] [PubMed] [Google Scholar]
- 6.Lambova SN, Müller-Ladner U. Capillaroscopic pattern in systemic lupus erythematosus and undifferentiated connective tissue disease: what we still have to learn? Rheumatol Int. 2013;33:689–695. doi: 10.1007/s00296-012-2434-0. [DOI] [PubMed] [Google Scholar]
- 7.Piraccini BM, Bellavista S, Misciali C, Tosti A, de Berker D, Richert B. Periungual and subungual pyogenic granuloma. Br J Dermatol. 2010;163:941–953. doi: 10.1111/j.1365-2133.2010.09906.x. [DOI] [PubMed] [Google Scholar]
- 8.Perruchoud DL, Varonier C, Haneke E, Hunger RE, Beltraminelli H, Borradori L, Ehnis Pérez A. Bowen disease of the nail unit: a retrospective study of 12 cases and their association with human papillomaviruses. J Eur Acad Dermatol Venereol. 2016;30:1503–1506. doi: 10.1111/jdv.13654. [DOI] [PubMed] [Google Scholar]
- 9.Rigopoulos D, Ralph D. Management of simple brittle nails. Dermatol Ther. 2012;25:596–573. doi: 10.1111/j.1529-8019.2012.01518.x. [DOI] [PubMed] [Google Scholar]
- 10.Baran R, Perrin C. Transverse leukonychia of toenails due to repeated microtrauma. Br J Dermatol. 1995;133:267–269. doi: 10.1111/j.1365-2133.1995.tb02627.x. [DOI] [PubMed] [Google Scholar]
- 11.Tosti A, Schneider SL, Ramirez-Quizon MN, Zaiac M, Miteva M. Clinical, dermoscopic, and pathologic features of onychopapilloma: a review of 47 cases. J Am Acad Dermatol. 2016;74:521–526. doi: 10.1016/j.jaad.2015.08.053. [DOI] [PubMed] [Google Scholar]
- 12.Chiriac A, Brzezinski P, Foia L, Marincu I. Chloronychia: green nail syndrome caused by Pseudomonas aeruginosa in elderly persons. Clin Interv Aging. 2015;10:265–267. doi: 10.2147/CIA.S75525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Leung LK, Harding J. A chemical mixer with dark-green nails. BMJ Case Rep. 2015;2015:bcr2014209203. doi: 10.1136/bcr-2014-209203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Perrin C. Tumors of the nail unit. A review. Part I: acquired localized longitudinal melanonychia and erythronychia. Am J Dermatopathol. 2013;35:621–636. doi: 10.1097/DAD.0b013e31826b74b8. [DOI] [PubMed] [Google Scholar]
- 15.Kallis P, Miteva M, Patel T, Zaiac M, Tosti A. Onychomatricoma with concomitant subungual glomus tumor. Skin Appendage Disord. 2015;1:14–17. doi: 10.1159/000371582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Maehara Lde S, Ohe EM, Enokihara MY, Michalany NS, Yamada S, Hirata SH. Diagnosis of glomus tumor by nail bed and matrix dermoscopy. An Bras Dermatol. 2010;85:236–238. doi: 10.1590/s0365-05962010000200018. [DOI] [PubMed] [Google Scholar]
- 17.de Berker D. Erythronychia. Dermatol Ther. 2012;25:603–611. doi: 10.1111/j.1529-8019.2012.01525.x. [DOI] [PubMed] [Google Scholar]
- 18.Thatte SS, Chikhalkar SB, Khopkar US. “Pink glow”: a new sign for the diagnosis of glomus tumor on ultraviolet light dermoscopy. Indian Dermatol Online J. 2015;6(suppl 1):S21–S23. doi: 10.4103/2229-5178.171041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rai AK. Role of intraoperative dermoscopy in excision of nail unit glomus tumor. Indian Dermatol Online J. 2016;7:448–450. doi: 10.4103/2229-5178.190488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Piraccini BM, Balestri R, Starace M, Rech G. Nail digital dermoscopy (onychoscopy) in the diagnosis of onychomycosis. J Eur Acad Dermatol Venereol. 2013;27:509–513. doi: 10.1111/j.1468-3083.2011.04323.x. [DOI] [PubMed] [Google Scholar]
- 21.Jesús-Silva MA, Fernández-Martínez R, Roldán-Marín R, Arenas R. Dermoscopic patterns in patients with a clinical diagnosis of onychomycosis – result of a prospective study including data of potassium hydroxide (KHO) and culture examination. Dermatol Pract Concept. 2015;5:39–44. doi: 10.5826/dpc.0502a05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ronger S, Touzet S, Ligeron C, Balme B, Viallard AM, Barrut D, Colin C, Thomas L. Dermoscopic examination of nail pigmentation. Arch Dermatol. 2002;138:1327–1333. doi: 10.1001/archderm.138.10.1327. [DOI] [PubMed] [Google Scholar]
- 23.Lencastre A, Lamas A, Sá D, Tosti A. Onychoscopy. Clin Dermatol. 2013;31:587–593. doi: 10.1016/j.clindermatol.2013.06.016. [DOI] [PubMed] [Google Scholar]
- 24.Haas N, Henz BM. Pitfall in pigmentation: pseudopods in the nail plate. Dermatol Surg. 2002;28:966–967. doi: 10.1046/j.1524-4725.2002.02063.x. [DOI] [PubMed] [Google Scholar]
- 25.Murata Y, Kumano K. Dots and lines: a dermoscopic sign of regression of longitudinal melanonychia in children. Cutis. 2012;90:293–296. 301. [PubMed] [Google Scholar]
- 26.Lyall D. Malignant melanoma in infancy. JAMA. 1967;202:1153. [Google Scholar]
- 27.Uchiyama M, Minemura K. Two cases of malignant melanoma in young persons. Nippon Hifuka Gakkai Zasshi. 1979;89:668. [Google Scholar]
- 28.Chu DH, Rubin AI. Diagnosis and management of nail disorders in children. Pedriatr Clin North Am. 2014;61:293–308. doi: 10.1016/j.pcl.2013.11.005. [DOI] [PubMed] [Google Scholar]
- 29.Kikuchi I, Inoue S, Sakaguchi E, Ono T. Regressing nevoid nail melanosis in childhood. Dermatology. 1993;186:88–93. doi: 10.1159/000247314. [DOI] [PubMed] [Google Scholar]
- 30.Iorizzo M, Tosti A, Di Chiacchio N, Hirata SH, Misciali C, Michalany N, Domiguez J, Toussaint S. Nail melanoma in children: differential diagnosis and management. Dermatol Surg. 2008;34:974–978. doi: 10.1111/j.1524-4725.2008.34191.x. [DOI] [PubMed] [Google Scholar]
- 31.Thomas L, Dalle S. Dermoscopy provides useful information for the management of melanonychia striata. Dermatol Ther. 2007;20:3–10. doi: 10.1111/j.1529-8019.2007.00106.x. [DOI] [PubMed] [Google Scholar]
- 32.Di Chiacchio ND, Farias DC, Piraccini BM, Hirata SH, Richert B, Zaiac M, Daniel R, Fanti PA, Andre J, Ruben BS, Fleckman P, Rich P, Haneke E, Chang P, Cherit JD, Scher R, Tosti A. Consensus on melanonychia nail plate dermoscopy. An Bras Dermatol. 2013;88:309–313. doi: 10.1590/S0365-05962013000200029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Levit EK, Kagen MH, Scher RK, Grossman M, Altman E. The ABC rule for clinical detection of subungual melanoma. J Am Acad Dermatol. 2000;42(pt 1):269–274. doi: 10.1016/S0190-9622(00)90137-3. [DOI] [PubMed] [Google Scholar]
- 34.Piraccini BM, Dika E, Fanti PA. Tips for diagnosis and treatment of nail pigmentation with practical algorithm. Dermatol Clin. 2015;33:185–195. doi: 10.1016/j.det.2014.12.002. [DOI] [PubMed] [Google Scholar]
- 35.Benati E, Ribero S, Longo C, Piana S, Puig S, Carrera C, Cicero F, Kittler H, Deinlein T, Zalaudek I, Stolz W, Scope A, Pellacani G, Moscarella E, Piraccini BM, Starace M, Argenziano G. Clinical and dermoscopic clues to differentiate pigmented nail bands: an International Dermoscopy Society study. J Eur Acad Dermatol Venereol. 2016 doi: 10.1111/jdv.13991. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 36.Hirata SH, Yamada S, Enokihara MY, Di Chiacchio N, de Almeida FA, Enokihara MM, Michalany NS, Zaiac M, Tosti A. Patterns of nail matrix and nail bed of longitudinal melanonychia by intraoperative dermatoscopy. J Am Acad Dermatol. 2011;65:297–303. doi: 10.1016/j.jaad.2010.06.009. [DOI] [PubMed] [Google Scholar]
- 37.Hirata SH, Yamada S, Almeida FA, Enokihara MY, Rosa IP, Enokihara MM, Michalany NS. Dermoscopic examination of the nail bed and matrix. Int J Dermatol. 2006;45:28–30. doi: 10.1111/j.1365-4632.2004.02335.x. [DOI] [PubMed] [Google Scholar]
- 38.Ackerman AB. Malignant melanoma in situ: the flat, curable stage of malignant melanoma. Pathology. 1985;17:298–300. doi: 10.3109/00313028509063771. [DOI] [PubMed] [Google Scholar]
- 39.Ruben BS. Pigmented lesions of the nail unit: clinical and histopathologic features. Semin Cutan Med Surg. 2010;29:148–158. doi: 10.1016/j.sder.2010.06.008. [DOI] [PubMed] [Google Scholar]
- 40.Wang YJ, Sun PL. Fungal melanonychia caused by Trichophyton rubrum and the value of dermoscopy. Cutis. 2014;94:E5–E6. [PubMed] [Google Scholar]
- 41.Braun RP, Baran R, Le Gal FA, Dalle S, Ronger S, Pandolfi R, Gaide O, French LE, Laugier P, Saurat JH, Marghoob AA, Thomas L. Diagnosis and management of nail pigmentation. J Am Acad Dermatol. 2007;56:835–847. doi: 10.1016/j.jaad.2006.12.021. [DOI] [PubMed] [Google Scholar]
- 42.Kilinc Karaarslan I, Acar A, Aytimur D, Akalin T, Ozdemir F. Dermoscopic features in fungal melanonychia. Clin Exp Dermatol. 2015;40:271–278. doi: 10.1111/ced.12552. [DOI] [PubMed] [Google Scholar]
- 43.De Crignis G, Valgas N, Rezende P, Leverone A, Nakamura R. Dermatoscopy of onychomycosis. Int J Dermatol. 2014;53:e97–e99. doi: 10.1111/ijd.12104. [DOI] [PubMed] [Google Scholar]
- 44.Braun R, Baran R, Saurat JH, Thomas L. Surgical Pearl: Dermatoscopy of the free edge of the nail to determine the level of the nail plate pigmentation and the location of its probable origin in the proximal or distal nail matrix. J Am Acad Dermatol. 2006;55:512–513. doi: 10.1016/j.jaad.2005.09.032. [DOI] [PubMed] [Google Scholar]
- 45.Lesort C, Debarbieux S, Duru G, Dalle S, Poulhalon N, Thomas L. Dermoscopic features of onychomatricoma: a study of 34 cases. Dermatology. 2015;231:177–183. doi: 10.1159/000431315. [DOI] [PubMed] [Google Scholar]
- 46.Iorizzo M, Dahdah M, Vincenzi C, Tosti A. Videodermoscopy of the hyponychium in nail bed psoriasis. J Am Acad Dermatol. 2008;58:714–715. doi: 10.1016/j.jaad.2007.11.026. [DOI] [PubMed] [Google Scholar]