Abstract
Objective
Pediatric traumatic brain injuries (TBIs) adversely affect long-term functional and social outcomes. Limited research suggests children with TBI are more likely to be victimized by peers than noninjured children. Deficits in social information processing (SIP), cognitive ability, and executive functioning (EF) may contribute to increased victimization risk. This study examined rates of peer victimization/bullying in children with early TBI compared with children with orthopedic injuries (OIs) and the role of processing speed, executive function (EF), and SIP as mediators of the association of TBI and peer victimization.
Method
Children ages 10 to 14 years who sustained a complicated mild/moderate or severe TBI (N = 58) or OI (N = 72) during early childhood (ages 3–7 yr) and their parents participated in a longitudinal prospective follow-up 6.8 years postinjury. SIP, EF and processing speed, and peer victimization were assessed.
Results
Parents of children with severe TBI reported greater rates of peer victimization than parents of children with OIs. Children with severe TBI demonstrated greater EF deficits than children with complicated mild/moderate TBI or OI and poorer processing speed than children with OI. No significant indirect relationships were found between groups and any outcome variables to indicate mediation.
Conclusion
Based on parent report, children with severe TBI have higher risk of peer victimization than those with less severe injuries. In addition, children with severe TBI have more impaired EF and cognitive ability than counterparts with less severe TBI. Further research is needed to explore predictors of long-term victimization after early TBI to create interventions aimed at providing social, emotional, and behavioral skill building for victimized youth.
Index terms: executive function, peer victimization, bullying, social information processing, traumatic brain injury
Pediatric traumatic brain injury (TBI) is a significant public health concern given its potential to adversely affect long-term functioning and alter developmental trajectories through adolescence and into adulthood.1 Negative sequelae of pediatric TBI include impairments in social, emotional, behavioral, and cognitive functioning.2–5
Traumatic brain injury has been shown to adversely affect social adjustment and peer relationships.6,7 A recent study showed that children with severe TBI were rated higher by classmates in peer rejection and victimization than children with orthopedic injuries (OIs), especially if they did not have a reciprocal friend in their classroom.6 Children with severe TBI also have fewer friends.8 These studies included students who were middle school aged, a peak time for victimization and transition-related difficulties.9,10
The association between TBI and peer victimization is poorly understood but may reflect deficits in social information processing (SIP) and cognition. SIP—the encoding, storage, processing, and retrieval of information pertaining to social interaction and situations—has been shown to be adversely affected by TBI.6,7,11 Post-TBI deficits include poor social problem solving characterized by more frequent aggressive or ineffective solutions and impaired social skills relative to noninjured children.12 Children with TBI also display deficits in social cognition and language pragmatics.6,13 The literature indicates that children with deficits in social cognition and a poor understanding of emotions and social relationships are at greatest risk for peer victimization. More broadly, SIP has been linked to children’s social adjustment, aggression, and conduct problems.7,11,14
Crick and Dodge’s14 model of SIP provides a useful framework for examining children’s ability to understand and respond to social information. Assertive SIP is predicted to lead to more socially adaptive behavior, whereas aggressive or passive SIP is predicted to lead to socially maladaptive behavior.14 Children with TBI may exhibit deficits in SIP that increase the likelihood that they will engage in or elicit problematic social behavior. For instance, children with aggressive attribution biases may attribute malicious intent in ambiguous situations, and they may engage in subsequent aggression against peers they view as threatening. Thus, deficits in SIP may be a key mediator of the association between TBI and victimization. Limited evidence suggests that deficits in SIP after TBI correspond to injury severity and peer victimization.7 Specifically, children with TBI have SIP deficits (e.g., theory of mind) that negatively affect their ability to form friendships and obtain peer acceptance, and these SIP deficits make them vulnerable to peer victimization. Consistent with this hypothesis, one previous study found that better theory of mind predicted less victimization after childhood TBI.7
Impaired cognitive ability, processing speed, and executive functioning skills may also lead to victimization. One study examined the association between executive functions, social behavior, and peer acceptance for children with TBI and found that victimization is a significant mediator of the relation between executive function and peer acceptance.15 Factors that contribute to the appearance of being different from others are also associated with an increased likelihood of peer victimization. However, the role of similar mechanisms in peer victimization after pediatric TBI has not been examined.
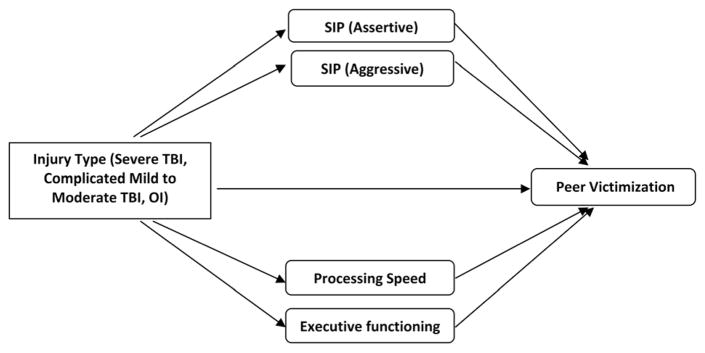
As illustrated in Figure 1 and building on the work of Yeates et al.,11 we propose a framework in which SIP and cognitive abilities mediate the association of TBI with peer victimization. Guided by the framework, the current investigation examined whether deficits in processing speed, executive functioning, and SIP after early childhood TBI may place children at long-term risk for peer victimization. Specifically, we explored whether peer victimization associated with TBI is mediated by impairments in processing speed, executive functioning, and SIP. We hypothesized higher levels of self- and parent-report of victimization among children with TBI relative to those with OI. In addition, we hypothesized that greater injury severity would be associated with poorer processing speed, executive functioning, and SIP after TBI. We also hypothesized that impaired processing speed and executive functioning, and SIP styles (Assertive and Aggressive), after TBI would help to account for differences in victimization.
Figure 1.
Model of mediators and outcomes for children with TBI. Based on Yeates et al.11 model of social information processing (SIP) and traumatic brain injury (TBI), we propose a similar framework such that SIP and cognitive abilities mediate the association of TBI with peer victimization.
METHOD
Participants
Participants were drawn from a middle school-aged cohort of children who were originally recruited as part of a prospective, concurrent cohort longitudinal study of outcomes of early childhood traumatic brain injuries (TBI). Children who sustained TBI or orthopedic injury (OI) between 3 and 6 years, 11 months of age were recruited within the initial 3 months postinjury, and outcomes were assessed at 6, 12, and 18 months and again at an average 3.5 and 6.7 years after injury. Children were recruited from inpatient admissions between 2003 and 2006 at 3 Ohio children’s hospitals and 1 Ohio general hospital, all of which have Level 1 trauma centers. Children with OI were included as a comparison group to control for pre-injury factors like to give rise to injury, as well as the experience of hospitalization for a traumatic injury.
General eligibility criteria for the initial study included evidence of a traumatic injury (TBI or OI) between ages 3 and 6 years, 11 months that required overnight hospitalization. Eligible participants also had to have English as the primary language spoken at the home. Children who sustained nonblunt head trauma (e.g., drowning and stroke) were excluded. In addition, exclusionary criteria for both groups included history of autism, intellectual disability, or a neurological disorder before injury and documentation in either the medical record or in a parent interview indicating child abuse as the cause of the injury. Consistent with previous investigations, severe TBI was defined by a Glasgow Coma Scale (GCS16) score of 8 or less at any point after injury, moderate TBI by a GCS score of 9 to 12, and complicated mild TBI by a GCS score of 13 to 15 accompanied by evidence of brain insult on neuroimaging. In view of similarity in outcomes of complicated mild and moderate TBI,17 these 2 groups were combined for analysis. Eligibility criteria for the OI group included a documented bone fracture in an area of the body other than the head and the absence of any evidence of loss of consciousness or other findings suggesting the presence of a brain injury. A total of 221 children (46% TBI, 58% male, and 72% white) were enrolled in the original study. More detailed enrollment criteria for the initial study is described by Wade et al.18 Participants in this study were those who completed the extended follow-up 5 to 8 years (average 6.7 yr after injury) after early childhood injury. Of the 217 participants eligible for the follow-up assessment, 146 participants (66% of the original cohort) were enrolled. Sixteen participants were excluded from analysis because of either having a mild TBI (N = 12) or not completing the follow-up assessment (N = 4). The sample included 130 children between ages 10 and 14 years and their caregiver(s). This study examined outcomes collected at the final follow-up, which was conducted between 2010 and 2015.
Procedure
The Institutional Review Boards at each participating study site approved the study. Informed consent and assent were obtained from the primary caregivers and children, respectively, before data collection. Families completed a packet of questionnaires that included measures of peer victimization and emotional and behavioral problems, and children completed assessments of their social information processing (SIP), cognitive abilities (e.g., processing speed), executive functioning, and ratings of victimization, as described under measures.
Measures
Outcome Measures
Peer victimization was measured using the Schwartz Report of Victimization,19 a 9-item questionnaire with items rated on a 7-point Likert scale (1 = Never or almost never happens to me, 7 = Happens to me almost every day). The Schwartz Victimization Scale is available in child self-report and parent-report versions and measures the frequency of verbal (e.g., teasing and name calling), physical (e.g., pushing and hitting), and relational (e.g., gossiping and excluding) types of victimization. We examined the total score of both self- and parent reports of peer victimization. Researchers caution against using self-reports of victimization alone because children may be unaware of their victimization, especially relational forms of victimization (e.g., gossip). Internal consistency estimates, as measured by Cronbach’s alpha, were excellent for both child self-report (α = .93) and parent report (α = .95) versions. The total peer victimization score was log transformed before analysis to reduce skewness in the distribution and create a more normally distributed measure.
Mediating Measures
The Dodge SIP Self-Report Stories20 provides composite measures of 3 attributional styles of SIP: Assertive, Passive, and Aggressive. Each of the SIP composites consists of the total of responses from 6 stories. Each story is followed by 14 questions designed to elicit attributional style. Thirteen of the 14 questions were rated on a 5-point Likert scale (1 = Yes, definitely, 5 = No, definitely not). For example, participants were asked to rate why they thought the classmate in the scenario behaved the way he/she did (i.e., was the classmate trying to be mean? Did the classmate just really want a turn?), how angry they would feel if the scenario happened to them, how likely they would be to get back at the classmate, how likely they would be to get along with the classmate, and how likely they would do or say certain things within the context of the scenario (i.e., how likely would you say “I was here first and have waited a long time. You can have a turn right after me”). The Aggressive composite included hostile attribution, whether the situation would evoke anger, if there was an aggressive goal orientation, the likelihood there would be an aggressive response, and instrumental and interpersonal value attributed to the aggressive response. The Passive composite also included the hostile attribution but included the following items: whether the situation evoked sadness, if there was a passive goal orientation, the likelihood that there would be a passive response, and if the instrumental and interpersonal value was nonassertive. The Assertive composite included a nonhostile attribution, an assertive/prosocial goal orientation, the likelihood that there would be a prosocial response, and the instrumental and interpersonal value attributed to an assertive/prosocial response.20 Internal consistency estimates, as measured by Cronbach’s alpha, were excellent for Aggressive SIP (α = .85) and Assertive SIP (α = .83) but too low for Passive SIP (α = .37) to merit inclusion in analysis. Thus, we examined Assertive and Aggressive attributional styles as possible mediators of the relationship between TBI and victimization.
The age-based, scaled score of the Walk/Don’t Walk (WDW) subtest of the Test of Everyday Attention for Children (TEA-Ch21) provided a measure of sustained attention and inhibitory control. The active maintenance of attention across the WDW task is a strong determinant of response suppression abilities.21 On the WDW sub-test, participants are presented a sheet depicting 20 paths, each comprising 14 squares containing footprints. Participants are instructed to listen to an audio tape and use a dry erase marker to “walk” along the path marking the footprints on “go” tones but leaving the footprints unmarked on “don’t go” tones. The published test–retest reliability for the WDW subtest is .73.21
The Processing Speed Index (PSI) composite score from the Wechsler Intelligence Scale for Children-Fourth Edition (WISC-IV22) was used to assess psychomotor speed and coordination, short-term visual memory, attention, and cognitive flexibility. The PSI consists of the Coding and Symbol Search subtests. The Coding subtest asks the child to copy symbols paired with numbers, with higher scores reflecting greater speed and accuracy of performance, whereas the Symbol Search is a timed subtest requiring visual scanning of geometric symbols to determine whether they match the target symbol. WISC-IV subtests have good validity and reliability and are normed for children ages 6 to 16.22
Statistical Analysis
Analysis of covariance was used to examine differences between the severe TBI, complicated mild/moderate TBI, and OI groups on Schwartz Child Victimization—self-report, Schwarz Child Victimization—parent report, SIP assertive scale, SIP aggressive scale, TEA-Ch—Walk/Don’t Walk scale, and WISC—PSI. Covariates in the models included age, time since injury, sex, race (dichotomized as white/nonwhite), parental education, and average neighborhood income based on census tract data. An alpha level of p < .05 was considered statistically significant. Multiple comparisons were controlled for using a Bonferroni correction, and these adjusted probabilities are reported in the tables.
Associations between the outcome measures and other variables in the models were initially computed using Pearson’s correlations coefficients for 2 continuous variables and point biserial correlations for the correlations between a continuous variable and a dichotomous variable. To avoid multicollinearity, we examined the variance inflation factor, and no covariates exceeded the maximum value of 5.23 Multivariable analyses were then conducted to examine the mediation models. A macro developed by Preacher and Hayes was used to examine mediation. This macro calculates the multiple indirect effects simultaneously by calculating the total effect of the predictor and the specific indirect effects of the predictor through the mediator variables. Bootstrap confidence intervals (CIs) were calculated to determine significance. If the CIs do not cross 0.00, then the effect is considered significant. Significant covariates were included in the models. All data were analyzed using SAS v9.2 and the Preacher and Hayes Process Macro.24
RESULTS
Sample Characteristics
As summarized in Table 1, mean age at injury was approximately 5 years (range 3–7 yr) and mean time since injury was nearly 7 years (range 5–11 yr). Glasgow Coma Scale (GCS) scores ranged from 3 to 15 (M = 10.8, SD = 4.8) in the traumatic brain injury (TBI) group. The 2 TBI groups differed significantly on GCS scores, with a higher mean score for the complicated mild/moderate TBI group (13.4, SD = 1.1) than for the severe TBI group (M = 4.0, SD = 1.9) (t = −15.21, p < .001). The groups did not differ significantly on any of the demographic variables. Participants did not differ significantly from nonparticipants with respect to injury type (TBI vs orthopedic injury [OI]), sex, ethnicity/race, socioeconomic status, or child intelligence quotient at baseline.
Table 1.
Sample Characteristics: Overall and by Injury Group
| Overall | Group
|
T/Z Score (pa)
|
|||||
|---|---|---|---|---|---|---|---|
| OI | Complicated Mild/Moderate TBI | Severe TBI | Severe TBI vs CMild/Mod | Severe TBI vs OI | CMild/Mod TBI vs OI | ||
| N (%) | 130 | 72 (55.4) | 42 (32.3) | 16 (12.3) | |||
| Current age | |||||||
| Mean | 11.9 | 11.9 | 12.0 | 12.2 | .51 | .81 | .49 |
| SD | 1.1 | 1.1 | 1.1 | 1.5 | 1.00 | 1.00 | 1.00 |
| Years since injury at baseline | |||||||
| Mean | 6.8 | 6.8 | 6.8 | 7.1 | .97 | 1.19 | −.02 |
| SD | 1.1 | 1.0 | 1.1 | 1.3 | 1.00 | .93 | 1.00 |
| Sex (% male) | 56.2% | 52.8% | 59.5% | 62.5% | .21 (1.00) | .70 (1.00) | .70 (1.00) |
| Race (% white) | 74.6% | 76.4% | 76.2% | 62.5% | 1.03 (.90) | 1.13 (.77) | 0.02 (1.00) |
| Income | |||||||
| Mean | $64,447 | $68,080 | $68,121 | $54,708 | −1.83 | −1.94 | .008 |
| SD | 25,189 | 24,575 | 26,739 | 21,816 | .21 | .17 | 1.00 |
| Primary caregiver has a college education | |||||||
| Mean | 2.92 | 3.03 | 2.88 | 2.56 | −.95 | −1.48 | −0.66 |
| SD | .16 | .13 | .17 | .28 | 1.00 | .42 | 1.00 |
All probabilities have been adjusted for multiple comparisons using the Bonferroni correction.
CMild/Mod, complicated mild to moderate TBI; OI, orthopedic injury; TBI, traumatic brain injury.
Injury Group Differences on Outcomes and Mediators
The results of group comparisons are summarized in Table 2. No significant group difference was found on the self-reported Schwarz Child Victimization scores (df = 2, 125, F = 2.23, p = .112). However, the groups differed significantly on parent ratings for the Schwartz Child Victimization total (df = 2,125, F = 7.92, p = .0006). Post hoc tests indicated that parents of children with severe TBI reported significantly higher levels of victimization than parents of children with OI.
Table 2.
Group Differences in Victimization, Behavior Problems, SIP, and Cognitive/Executive Functioning
| Group
|
T-Score (pa)
|
|||||
|---|---|---|---|---|---|---|
| OI | Complicated Mild/Mod TBI | Severe TBI | Severe TBI vs CMild/Mod | Severe TBI vs OI | CMild/Mod TBI vs OI | |
| Outcomes | ||||||
| Schwartz Child Victimization: self-reportb | ||||||
| Mean | 0.50 | 0.68 | 0.76 | 0.54 | 1.70 | 1.64 |
| SD | 0.51 | 0.57 | 0.66 | 1.00 | .28 | .31 |
| Schwartz Child Victimization: parent-reportb | ||||||
| Mean | 0.43 | 0.65 | 0.92 | 1.94 | 3.72 | 2.33 |
| SD | 0.44 | 0.52 | 0.55 | .17 | .00 | .06 |
| Mediators | ||||||
| SIP (assertive) | ||||||
| Mean | 3.63 | 3.56 | 3.78 | 1.36 | 1.01 | −0.64 |
| SD | 0.42 | 0.70 | 0.36 | .53 | .95 | 1.00 |
| SIP (aggressive), mean (SD) | ||||||
| Mean | 2.54 | 2.65 | 2.77 | 0.64 | 1.34 | 0.95 |
| SD | 0.59 | 0.64 | 0.69 | 1.00 | .55 | 1.00 |
| TEA-Ch: WDW, mean (SD) | ||||||
| Mean | 7.94 | 8.07 | 4.40 | −3.49 | −3.57 | 0.19 |
| SD | 3.40 | 3.86 | 2.74 | .00 | .00 | 1.00 |
| WISC-IV: PSI, mean (SD) | ||||||
| Mean | 99.12 | 95.93 | 86.75 | −2.15 | −3.10 | −1.15 |
| SD | 13.39 | 15.02 | 17.85 | .10 | .01 | .76 |
All probabilities have been adjusted for multiple comparisons using the Bonferroni correction.
Group differences were assessed using natural log transformation.
Scores were transformed using a natural log transformation before analysis. CMild/Mod, complicated mild to moderate TBI; OI, orthopedic injury; PSI, processing speed index composite score; SIP, social information processing composite score; TBI, traumatic brain injury; TEA-Ch, Test of Everyday Attention in Children age-based scaled score; WDW, Walk Don’t Walk; WISC-IV, Wechsler Intelligence Scale for Children-Fourth Edition.
The correlation between parent report and child report of victimization was strong for the severe TBI group (r = .70) and moderate for the complicated mild/moderate TBI group (r = .55). Significantly, more parents of children with severe TBI (37%) and complicated mild/moderate TBI (15%) reported peer victimization, defined by verbal, physical, and relational forms of peer victimization than did parents of children with an OI (8.6%). In addition, 33% of children with severe TBI and 24.4% of children with complicated mild/moderate TBI reported peer victimization compared with 14.1% of children with OI; however, these proportions were not significantly different across groups.
The groups did not differ significantly for either assertive (df = 2, 124, F = 0.93, p = .3958) or aggressive (df = 2, 124, F = 0.00, p = .9968) social information processing (SIP) style. The groups did differ, however, on the Test of Everyday Attention for Children (TEA-Ch) Walk/Don’t Walk (WDW) scaled score (df = 2, 125, F = 7.01, p = .001) and the Wechsler Intelligence Scale for Children-Fourth Edition (WISC-IV) Processing Speed Index (PSI) composite (df = 2, 127, F = 4.86, p = .009). On the TEA-Ch WDW test, the severe TBI group had significantly lower scores than both the complicated mild/moderate TBI and OI groups. For the WISC-IV PSI, the severe TBI group had significantly lower scores than OI group.
Correlations Among Victimization, SIP, and Executive Functioning
Table 3 shows the correlations among outcome variables and mediators and covariates. The TEA-Ch WDW had a significant low to moderate inverse correlation with parent-reported victimization (r = −.19), and the WISC-IV PSI showed a significant low to moderate inverse correlation with parent-reported victimization (r = −.23). Highest education attainment for primary caregiver was significantly negatively correlated with both outcomes: r = −.23 and −.17 for child- and parent-reported victimization, respectively.
Table 3.
Correlations Between Outcomes, Mediators, and Covariates
| Schwartz Child Victimization
|
||
|---|---|---|
| Child Self-Report | Parent Report | |
| Outcomes | ||
| Schwartz: child self-report | 1.00 | |
| Schwartz: parent-report | .57*** | 1.00 |
| Mediators | ||
| SIP (assertive) | −.12 | .01 |
| SIP (aggressive) | .22* | .26** |
| TEA-Ch WDW | −.03 | −.19* |
| WISC PSI | −.13 | −.23** |
| Covariates | ||
| Sex (1 = male) | .05 | .17 |
| Current age | .17 | .19* |
| Time since injury | .16 | .20* |
| Child is white (1 = white) | .05 | −.04 |
| Income | −.17 | −.25** |
| Highest educational attainment level of primary caregiver | .23** | .17* |
p < .05;
p < .01;
p < .001.
PSI, processing speed index composite score; SIP, social information processing composite score; WDW, Walk Don’t Walk; WISC, Wechsler Intelligence Scale for Children.
Does SIP or Executive Functioning Mediate the Relation Between Injury Severity and Outcomes?
With all 4 mediators in the model, no significant indirect relationships were found between groups and any of the outcomes (Table 4). Direct group effects were significant for parent-reported victimization but not on self-reported victimization.
Table 4.
Mediation Models Comparing TBI Groups to OI Group (Self-Report and Parent Report)
| Effect | SE | t | P | LLCI | ULCI | |
|---|---|---|---|---|---|---|
| Schwartz Child Victimization: self-report | ||||||
| Total effect of CMild/Mod | 0.1846 | 0.1069 | 1.7274 | .0866 | −0.027 | 0.3961 |
| Direct effect of CMild/Mod | 0.1475 | 0.1074 | 1.3734 | .1722 | −0.0652 | 0.3602 |
| Total indirect | 0.0371 | 0.0388 | −0.0252 | 0.1331 | ||
| Indirect effect through: | ||||||
| SIP (assertive) | 0.0082 | 0.0177 | −0.014 | 0.0619 | ||
| SIP (aggressive) | 0.0197 | 0.0233 | −0.0094 | 0.0914 | ||
| TEA-Ch WSW | 0.0015 | 0.0125 | −0.0165 | 0.0404 | ||
| WISC PSI | 0.0077 | 0.0198 | −0.0138 | 0.073 | ||
| Total effect of severe | 0.2396 | 0.1591 | 1.5059 | .1347 | −0.0754 | 0.5545 |
| Direct effect of severe | 0.2233 | 0.1711 | 1.3049 | .1945 | −0.1156 | 0.5621 |
| Total indirect | 0.0163 | 0.0909 | −0.1621 | 0.2018 | ||
| Indirect effect through: | ||||||
| SIP (assertive) | −0.0148 | 0.0218 | −0.093 | 0.0079 | ||
| SIP (aggressive) | 0.0379 | 0.0449 | −0.0119 | 0.1788 | ||
| TEA-Ch WDW | −0.0289 | 0.0591 | −0.1428 | 0.0917 | ||
| WISC PSI | 0.0222 | 0.0471 | −0.0529 | 0.1432 | ||
| Model statistics | R-sq = 0.03 | MSE = 0.2952 | F = 2.11 | df1 = 2 | df2 = 122 | p = .1256 |
| Schwartz Child Victimization: parent-report | ||||||
| Total effect of CMild/Mod | 0.2049 | 0.0954 | 2.1481 | .0338 | 0.016 | 0.3938 |
| Direct effect of CMild/Mod | 0.1957 | 0.0957 | 2.0451 | .0432 | 0.0061 | 0.3853 |
| Total indirect | 0.0092 | 0.0306 | −0.0424 | 0.0838 | ||
| Indirect effect through: | ||||||
| SIP (assertive) | −0.0036 | 0.012 | −0.0484 | 0.0085 | ||
| SIP (aggressive) | 0.0076 | 0.0165 | −0.016 | 0.0557 | ||
| TEA-Ch WDW | −0.002 | 0.0139 | −0.0473 | 0.016 | ||
| WISC PSI | 0.0071 | 0.0163 | −0.0083 | 0.0672 | ||
| Total effect of severe | 0.4241 | 0.1418 | 2.9898 | .0034 | 0.1432 | 0.7049 |
| Direct effect of severe | 0.3302 | 0.1524 | 2.1669 | .0323 | 0.0283 | 0.6321 |
| Total indirect | 0.0939 | 0.0735 | −0.0441 | 0.2447 | ||
| Indirect effect through: | ||||||
| SIP (assertive) | 0.0085 | 0.0171 | −0.0108 | 0.0689 | ||
| SIP (aggressive) | 0.0145 | 0.0298 | −0.0195 | 0.1141 | ||
| TEA-Ch WDW | 0.045 | 0.0521 | −0.0533 | 0.1543 | ||
| WISC PSI | 0.026 | 0.0391 | −0.0319 | 0.1297 | ||
| Model statistics | R-sq = 0.14 | MSE = 0.2287 | F = 3.7916 | df1 = 5 | df2 = 117 | p = .0032 |
CMild/Mod, Complicated Mild to Moderate TBI; PSI, processing speed index composite score; SIP, social information processing composite score; TEA-Ch, Test of Everyday Attention for Children; WDW, Walk Don’t Walk; WISC, Wechsler Intelligence Scale for Children; SE, Standard Error; t, t Score; P, Probability Value; LLCI, Lower Limit Confidence Interval (95th Percentile); ULCI, Upper Limit Confidence Interval (95th Percentile).
DISCUSSION
This article examined whether children with traumatic brain injury (TBI) have an increased risk of peer victimization, and whether the effects of TBI on these outcomes were mediated by processing speed, executive function, or social information processing (SIP). Our findings were partially in accord with hypotheses. Although we failed to find significant group differences in child-reported victimization, we found evidence of significantly greater parent-reported victimization after severe TBI. These differences are noteworthy given that these ratings were obtained nearly 7 years after injury. The findings suggest that children with severe TBI experience greater victimization than children with injuries not involving the brain many years after their initial injury.
Having a severe TBI increased a child’s likelihood of being victimized. This is consistent with findings from a previous study showing that school-aged children with severe TBI had higher ratings of peer victimization.6 Correlational analyses suggested a correspondence between child and parent-reports of victimization. However, the moderate differences in child and parent-reports of victimization support the use of multiinformant methods for assessing victimization,25 as different information sources provide unique information. More specifically, in the severe TBI group, parents reported more frequent peer victimization than did the children themselves. This finding is consistent with other studies showing that more symptoms are reported by parent and teacher report than child self-report.26 However, in this study, parents in the complicated mild/moderate TBI and orthopedic injury groups reported less frequent peer victimization than did their children. The lower child-reported rates of victimization among children with severe TBI may be partly attributable to varying levels of social self-awareness among children with TBI, particularly regarding their awareness of peer rejection/victimization. Also, for some children with severe TBI, the lower rates of self-reported peer victimization could be due to minimization or normalization of victimization. The addition of peer and teacher reports of victimization would provide helpful information regarding the nature and extent of classroom victimization.
Surprisingly, no differences in SIP styles were found as a function of injury severity, and SIP was not a mediator of the association between injury severity and victimization. Deficits in SIP were expected to be a negative consequence of TBI because research suggests that TBI contributes to impairments in various aspects of social cognition, including SIP.6 Our failure to find support for differences in SIP after TBI has several potential explanations. First, the Dodge SIP measure was designed to predict conduct disorder/aggression and may not capture alterations in SIP that are most common after TBI. Although youth with TBI may not misread aggressive intent, they may have difficulty accurately perceiving and responding to nonliteral, pragmatic communication and understanding the intentionality of statements.7,11,13 Using a social cognition measure that is developed to assess TBI-related issues may be more sensitive to long-term alterations in SIP. Future studies should examine whether other measures of SIP may tap into differences in the ability to read and respond to social cues for TBI and control groups. Although aggressive SIP was not more common after TBI and did not mediate the effects of TBI on victimization, aggressive SIP was significantly correlated with the Schwartz Report of Victimization child (p = .01) and parent questionnaires (p = .004). These findings suggest that Crick and Dodge’s model is useful for understanding the underpinnings of victimization in children more broadly but that the Dodge vignettes may not be sensitive to the types of SIP deficits that arise after TBI.
Parent reports of victimization were significantly correlated with executive functioning as measured by the Test of Everyday Attention for Children Walk/Don’t Walk task and processing speed as measured by the Wechsler Intelligence Scale for Children: Processing Speed Index composite; however, these neurocognitive variables did not mediate the association between TBI and victimization. Laboratory-based measures of executive function are often poor predictors of behavior in everyday settings,27 and thus test scores may not be sensitive to the neuro-cognitive and behavioral challenges that children with TBI experience in their classroom and peer interactions. Youth who sustain a TBI are especially likely to exhibit aggression, impulsivity, and hyperactivity,28,29 which may contribute to difficulties with social interactions. Children with difficulties in self-regulation may struggle with appropriate social interactions, which in turn contribute to peer rejection and victimization. One study found that executive functioning is predictive of peer victimization in youth with TBI.15 Thus, results may depend on the specific measures used (parent vs peer report of victimization, single vs composite measures of executive functioning) and the timing of assessment. Also, future studies should examine behavioral/observational measures of emotional and behavioral regulation as potential determinants of victimization.
Although the association between primary caregiver’s highest education attained and victimization were not a major focus of this study, correlation analyses of parental education and victimization indicated that children of parents with less education were more likely to be victimized by peers according to both child and parent-reports of victimization. This finding is compelling and consistent with a previous study showing that social outcomes in children with TBI are exacerbated by low family socioeconomic status (SES), poorer family functioning, and limited family resources.4 These findings suggest that factors related to family SES, family functioning, and access to resources are important to examine in future studies as they may be predictive of youth social behaviors and peer acceptance after TBI.
Clinically, these findings highlight the importance of screening for victimization in youth, who have sustained a TBI, peers, and their parents because youth themselves may minimize or be less aware of peer victimization. Pediatricians in primary care clinics and those embedded in subspecialty clinics (e.g., neurology) should conduct brief assessments of victimization (i.e., 9-item Schwartz Report of Victimization) for patients with TBI who may be at risk for peer victimization and supplement this information with parent report of victimization. In this regard, pediatricians may serve as “gate-keepers” and help connect youth who are identified as experiencing victimization or at risk of victimization with mental health services. In addition, pediatricians who work in interdisciplinary settings with psychologists, psychiatrists, and licensed clinical social workers/therapists could potentially consult with their mental health colleagues and conduct “warm handoffs” so that identified patients are provided with psychoeducation, brief intervention, mental health referrals, and resources.
Findings from this study should be considered in the context of its limitations. These include a small sample of children with severe TBI that limited statistical power and potential biases from attrition over the nearly 7 years since injury. As noted above, reliance on the Dodge stories as our sole measure SIP may have limited our ability to detect group differences on this dimension. Similarly, use of parent- and self-reports of victimization could be augmented by teacher or peer reports in future studies to provide a more comprehensive understanding of peer victimization after early TBI.
Despite these limitations, the current findings contribute to the limited existing literature by suggesting that TBI in early childhood is associated with parent reports of higher levels of peer victimization many years after the injury. The fact that these differences were apparent approximately 7 years postinjury provides compelling evidence that peer victimization remains a serious concern for children who sustained an early childhood TBI. Future studies should examine behavioral control/regulation in everyday settings as a mediator of outcomes. Future studies should also examine whether family SES (parental income, education, and occupation), cultural factors, and access to resources (schools and mental health care) are related to socioemotional outcomes in children with TBI.
Moreover, children who are victimized may also experience externalizing problems, consistent with findings that peer group victimization significantly predicted behavioral problems (i.e., externalizing difficulties and attention dysregulation) both concurrently and prospectively.30 Also, adolescents who exhibit higher levels of externalizing problems may stand out in the peer group, thereby increasing susceptibility to peers victimization. The association between victimization and behavioral problems after TBI warrants further investigation. In addition, future research is needed to better understand how various cognitive, behavioral, and SIP deficits mediate the association between TBI and elevated rates of peer victimization.
In conclusion, our findings suggest that youth with TBI are more vulnerable to victimization many years after injury and indicate that the need to evaluate for possible victimization during outpatient visits. The current results also underscore the need to identify factors that contribute to victimization in this population and reasons for discrepancies between parent and child report. Given that TBI is related to various negative outcomes, greater emphasis should be placed on understanding risk and protective factors related to long-term outcomes to create effective preventive interventions. These findings could shed light on interventions aimed at providing social, emotional, and behavioral skill building for youth with TBI who are at risk for peer victimization.
Footnotes
Disclosure: The authors declare no conflict of interest. The research reported here was supported by Grant R01 HD42729 from the National Institute of Child Health and Human Development, in part by U.S. Public Health Service National Institutes of Health Grant M01 RR 08084, and by Trauma Research grants from the State of Ohio Emergency Medical Services. The project described was also supported by the National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant 8 UL1 TR000077-04.
References
- 1.Anderson V, Brown S, Newitt H, et al. Educational, vocational, psychosocial, and quality-of-life outcomes for adult survivors of childhood traumatic brain injury. J Head Trauma Rehabil. 2009;24:303–312. doi: 10.1097/HTR.0b013e3181ada830. [DOI] [PubMed] [Google Scholar]
- 2.Catroppa C, Anderson VA, Morse SA, et al. Outcome and predictors of functional recovery 5 years following pediatric traumatic brain injury (TBI) J Pediatr Psychol. 2008;33:707–718. doi: 10.1093/jpepsy/jsn006. [DOI] [PubMed] [Google Scholar]
- 3.Wade SL, Gerry Taylor H, Yeates KO, et al. Long-term parental and family adaptation following pediatric brain injury. J Pediatr Psychol. 2006;31:1072–1083. doi: 10.1093/jpepsy/jsj077. [DOI] [PubMed] [Google Scholar]
- 4.Yeates KO, Swift E, Taylor HG, et al. Short- and long-term social outcomes following pediatric traumatic brain injury. J Int Neuropsychol Soc. 2004;10:412–426. doi: 10.1017/S1355617704103093. [DOI] [PubMed] [Google Scholar]
- 5.Yeates KO, Armstrong K, Janusz J, et al. Long-term attention problems in children with traumatic brain injury. J Am Acad Child Adolesc Psychiatry. 2005;44:574–584. doi: 10.1097/01.chi.0000159947.50523.64. [DOI] [PubMed] [Google Scholar]
- 6.Yeates KO, Gerhardt CA, Bigler ED, et al. Peer relationships of children with traumatic brain injury. J Int Neuropsychol Soc. 2013;19:518–527. doi: 10.1017/S1355617712001531. [DOI] [PubMed] [Google Scholar]
- 7.Yeates KO, Bigler ED, Abildskov T, et al. Social competence in pediatric traumatic brain injury: from brain to behavior. Clin Psychol Sci. 2014;2:97–107. [Google Scholar]
- 8.Prigatano GP, Gupta S. Friends after traumatic brain injury in children. J Head Trauma Rehabil. 2006;21:505–513. doi: 10.1097/00001199-200611000-00005. [DOI] [PubMed] [Google Scholar]
- 9.Eccles JS, Midgley C, Wigfield A, et al. Development during adolescence. Am Psychol. 1993;48:90–101. doi: 10.1037//0003-066x.48.2.90. [DOI] [PubMed] [Google Scholar]
- 10.Seidman E, French SE. Developmental trajectories and ecological transitions: a two-step procedure to aid in the choice of prevention and promotion interventions. Dev Psychopathol. 2004;16:1141–1159. doi: 10.1017/s0954579404040179. [DOI] [PubMed] [Google Scholar]
- 11.Yeates KO, Bigler ED, Dennis M, et al. Social outcomes in childhood brain disorder: a heuristic integration of social neuroscience and developmental psychology. Psychol Bull. 2007;133:535–556. doi: 10.1037/0033-2909.133.3.535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ganesalingam K, Sanson A, Anderson V, et al. Self-regulation and social and behavioral functioning following childhood traumatic brain injury. J Int Neuropsychol Soc. 2006;12:609–621. doi: 10.1017/S1355617706060796. [DOI] [PubMed] [Google Scholar]
- 13.Dennis M, Simic N, Gerry Taylor H, et al. Theory of mind in children with traumatic brain injury. J Int Neuropsychol Soc. 2012;18:908–916. doi: 10.1017/S1355617712000756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Crick NR, Dodge KA. A review and reformulation of social information-processing mechanisms in children’s social adjustment. Psychol Bull. 1994;115:74–101. [Google Scholar]
- 15.Heverly-Fitt S, Rubin KH, Dennis M, et al. Investigating a proposed model of social competence in children with traumatic brain injuries. J Pediatr Psychol. 2016;41:235–243. doi: 10.1093/jpepsy/jsv085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Teasdale G, Jennett B. Assessment of coma and impaired consciousness. A practical scale. Lancet. 1974;2:81–84. doi: 10.1016/s0140-6736(74)91639-0. [DOI] [PubMed] [Google Scholar]
- 17.Williams DH, Levin HS, Eisenberg HM. Mild head injury classification. Neurosurgery. 1990;27:422–428. doi: 10.1097/00006123-199009000-00014. [DOI] [PubMed] [Google Scholar]
- 18.Wade SL, Taylor HG, Walz NC, et al. Parent-child interactions during the initial weeks following brain injury in young children. Rehabil Psychol. 2008;53:180–190. doi: 10.1037/0090-5550.53.2.180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schwartz D, Dodge KA, Pettit GS, et al. Friendship as a moderating factor in the pathway between early harsh home environment and later victimization in the peer group. Dev Psychol. 2000;36:646–662. doi: 10.1037/0012-1649.36.5.646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Walz NC, Yeates KO, Wade SL, et al. Social information processing skills in adolescents with traumatic brain injury: relationship with social competence and behavior problems. J Pediatr Rehabil Med. 2009;2:285–295. doi: 10.3233/PRM-2009-0094. [DOI] [PubMed] [Google Scholar]
- 21.Manly T, Anderson V, Nimmo-Smith I, et al. The differential assessment of children’s attention: the test of everyday attention for children (TEA-Ch), normative sample and ADHD performance. J child Psychol Psychiatry. 2001;42:1065–1081. doi: 10.1111/1469-7610.00806. [DOI] [PubMed] [Google Scholar]
- 22.Wechsler D. WISC-IV Administration Manual. San Antonio, TX: Pearson Assesment; 2003. [Google Scholar]
- 23.Rogerson PA. Statistical Methods for Geography. London, England: Sage; 2001. [Google Scholar]
- 24.Hayes AF, Preacher KJ. Statistical mediation analysis with a multicategorical independent variable. Br J Math Stat Psychol. 2014;67:451–470. doi: 10.1111/bmsp.12028. [DOI] [PubMed] [Google Scholar]
- 25.Tortura CMW, Green AE, Karver MS, et al. Multiple informants in the assessment of psychological, behavioral, and academic correlates of bullying and victimization in middle school. J Adolesc. 2009;32:193–211. doi: 10.1016/j.adolescence.2008.04.005. [DOI] [PubMed] [Google Scholar]
- 26.Goodman R, Meltzer H, Bailey V. The strengths and difficulties questionnaire: a pilot study on the validity of the self-report version. Eur Child Adolesc Psychiatry. 1998;7:125–130. doi: 10.1007/s007870050057. [DOI] [PubMed] [Google Scholar]
- 27.Anderson VA, Anderson P, Northam E, et al. Relationships between cognitive and behavioral measures of executive function in children with brain disease. Child Neuropsychol. 2002;8:231–240. doi: 10.1076/chin.8.4.231.13509. [DOI] [PubMed] [Google Scholar]
- 28.Max JE, Schachar RJ, Levin HS, et al. Predictors of secondary attention-deficit/hyperactivity disorder in children and adolescents 6 to 24 months after traumatic brain injury. J Am Acad Child Adolesc Psychiatry. 2005;44:1041–1049. doi: 10.1097/01.chi.0000173292.05817.f8. [DOI] [PubMed] [Google Scholar]
- 29.Dooley JJ, Anderson V, Hemphill SA, et al. Aggression after pediatric traumatic brain injury: a theoretical approach. Brain Inj. 2008;22:836–846. doi: 10.1080/02699050802425444. [DOI] [PubMed] [Google Scholar]
- 30.Schwartz D, McFadyen-Ketchum SA, Dodge KA, et al. Peer group victimization as a predictor of children’s behavior problems at home and school. Dev Psychopathol. 1998;10:87–99. doi: 10.1017/s095457949800131x. [DOI] [PubMed] [Google Scholar]