Abstract
Background
Sphenoethmoidal sinus mucocele causing uniocular progressive vision loss is a rare entity and was first described by Bery in 1985. It is generally diagnosed in its advanced stage when the patients develop subjective ophthalmic symptoms.
Case
A 43-year-old male presented to our institute for further evaluation and treatment of progressive visual deterioration in his left eye. The patient complained of visual impairment in his left eye for the past three months, in the form of a dark area in his left side of the visual field.
Observations
Magnetic resonance imaging (MRI) revealed a large expansile lesion in the left sided posterior ethmoidal air cells, abutting on the left optic nerve and displacing it in the region of the orbital apex. The patient underwent an urgent endoscopic sinus surgery by an Ear-Nose-Throat surgeon which resulted in stable visual acuity in the sixth postoperative month.
Conclusions
Sphenoethmoidal mucocele can cause irreversible blindness. Progressive vision loss with a neurological visual field defect should raise a high index of suspicion and computed tomography and MRI are to be performed to confirm the diagnosis. Collaboration between radiologists, ENT specialists, and ophthalmologists is essential for treating such cases.
Keywords: sphenoethmoidal mucocele, compressive optic neuropathy, visual field defect, endoscopic sinus surgery
Background
Sphenoethmoidal mucocele can cause irreversible blindness. Progressive vision loss with a neurological visual field defect should raise suspicion and computed tomography (CT) and magnetic resonance imaging (MRI) imaging are to be performed to confirm the diagnosis. Collaboration between radiologists, Ear-Nose-Throat (ENT) specialists, and ophthalmologists is essential for treating such cases.
A paranasal sinus mucocele is an encapsulated mass within a sinus containing mucoid secretions with desquamated epithelium and causing distension of the sinus walls. It is mostly found in the frontal and ethmoidal sinus and less commonly in the sphenoid sinus. Sphenoethmoidal sinus mucocele causing uniocular progressive vision loss is a rare entity and only a few reports are available in ophthalmic literature since its first description by Bery in 1989.1–5 This disease is most commonly diagnosed in its advanced stage because patients tend to seek examination only when they develop subjective ophthalmic symptoms.6 Early endoscopic surgical intervention may result in visual improvement.6 We herein report a rare case of sphenoethmoidal mucocele causing unilateral, painless progressive visual loss with immediate stabilization of vision following surgery.
Case
A 43-year-old man was referred to our institution in November 2008 for further evaluation and treatment of progressive visual deterioration out of retrobulbar neuritis in the left eye in spite of diagnosis and treatment with intravenous methylprednisolone at another medical centre. He complained of visual impairment in the left eye for the past three months, in the form of a dark area in his left side of the visual field. His medical and family history was unremarkable.
Observation
On examination, his visual acuity was 20/20 in the right eye and 20/30 in the left eye. Ocular movements were normal but relative afferent pupillary defect was present in the left eye. Fundus examination revealed generalized optic disc pallor, a well demarcated disc margin, and dilated retinal venules in the left eye (Figure 1). Computerized visual field analysis detected gross loss of threshold sensitivity except in the inferonasal quadrant where some sensitivity was retained (Figure 2). Extinguished visual-evoked potential (VEP) response was recorded in the left eye (Figure 3), while the right eye was clinically normal. Urgent MRI disclosed a large expansile T2 hyperintense lesion in the left sided posterior ethmoid air cells encroaching the adjacent sphenoid sinus (Figure 4). On T1-weighted images the lesion showed significant hyperintensity (Figure 5). The rest of the sphenoid sinus also contained mixed intensity components expressing hyperintense and hypointense signals. The lesion was abutting on the left optic nerve which was displaced in the region of orbital apex with narrowing of the superior orbital fissure. Depending upon the clinical and investigation findings, left compressive optic neuropathy caused by left sphenoethmoidal mucocele was diagnosed and the patient underwent urgent endoscopic sinus surgery. Marsupialization of the mucocele was performed under general anesthesia, in which the anterior and interior walls (septum) of the mucocele were removed. Pathological examination confirmed diagnosis of a mucocele. At the sixth month postoperative follow up, vision was stable with persistent disc pallor (Figure 6). Humphrey field analysis detected paracentral scotoma (30-2 tests; Figure 7) in left eye. MRI revealed minimal residual collection of fluid in the mucocele (Figure 8), however there was no compression to the optic nerve.
Figure 1.

Fundus photo revealing generalized optic disc pallor, well demarcated disc margin and dilated retinal venules in the left eye.
Figure 2.

Computerized visual field analysis showing a neurological field defect in the left eye.
Figure 3.

Flat visual-evoked potential response in the left eye.
Figure 4.
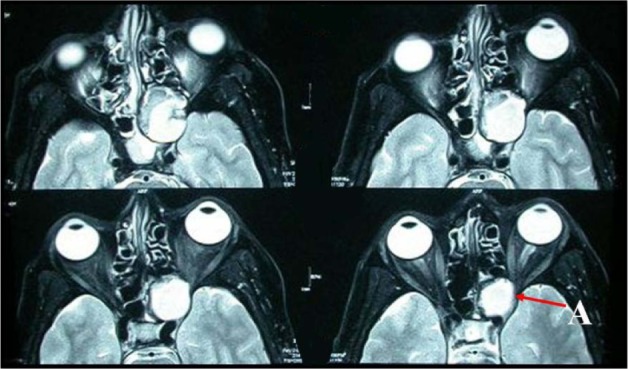
Preoperative serial axial magnetic resonance imaging shows large T2 weighted hyperitense lesion at the sphenoedmoidal region compressing and displacing the left optic nerve at the orbital apex (A) and intracranial extension.
Figure 5.

Preoperative axial T1 weighted image showing significant hyperintensity of the sphenoethmoidal mucocele. Sphenoidal sinus showing mixed intensity. Compression of the orbital apex and optic nerve is predominantly seen (A).
Figure 6.

Fundus photo showing the generalize pallor of the optic disc.
Figure 7.

Humphrey field analysis showing paracentral scotoma in left eye (30-2 test).
Figure 8.

Magnetic resonance imaging showing minimal residual collection of fluid in the mucocele (arrow).
Discussion
Sphenoethmoidal sinus mucocele is a rare cause of unilateral vision loss and blindness. Both genders are equally affected without any age predominance.1–7 Clinical examination and imaging (CT and MRI) are the bases of diagnosis. Clinical manifestations of sphenoethmoidal mucoceles are usually related to sinus expansion and extension of the lesion beyond the confinement of the sinus. The extension of the lesion usually follows the path of least resistance.
The presenting signs and symptoms are variable. If complication occurs, the most frequently reported findings are headache (89%), decreased visual acuity (57%), abducent or oculomotor palsies (56%), and exophthalmos (25%).7 Optic neuropathy is a well known complication of paranasal sinusitis and mucoceles.7,8 Different levels of vision loss including blindness can occur secondary to optic nerve dysfunction. One eye involvement is common particularly along with mucocele in the posterior paranasal sinus.2
There is a double mechanism involved in the development of visual loss caused by a mucocele.7,9 A gradual loss of vision is caused by circulatory disorders of the optic nerve due to pressure affect of the mucocele. Because the vascular supply of the optic nerve in the optic canal is limited and less dense than it is in other regions, this is a site where the optic nerve is susceptible to vascular compromise.10 On the other hand, a rapid loss of vision occurs from spread of infection and/or inflammation from the mucocele to the optic nerve.10
We presented a case of progressive deterioration of vision, neurological visual field defect, and VEP abnormality of the left eye. MRI findings showed left sphenoethmoidal mucocele causing compression of the left superior orbital fissure, orbital apex, and displacement of the same sided optic nerve which led to confirmation of the diagnosis. Our case had atypical presentation because other presenting common features like headache, abducent or oculomotor nerve palsies, or exophthalmos were absent. As a result of this diagnostic dilemma, the patient received intravenous methylprednesolone without any result in another medical centre. Along with the above findings, generalized disc pallor and mild venous stasis support the compressive theory of vision loss by the sphenoethmoidal mucocele. Thus, transnasal endoscopic surgical decompression is the standard surgical management of such cases and was carried out by an ENT surgeon for our patient. In the postoperative period, there was no further loss of vision.
Sphenoethmoidal sinus mucoceles can cause bilateral or even irreversible blindness and overall surgical prognosis may not be good.5 Ophthalmologists must be alert to this diagnosis. Progressive vision loss in one eye with a neurological visual field defect should raise a high index of suspicion and CT and MRI imaging need to be performed to confirm the diagnosis. Close collaboration between radiologists, ENT specialist, and ophthalmologists is essential for treating such cases.
Acknowledgments/disclosure
The authors thank Dr T Das and Dr N Medhi. The authors report no conflicts of interest in this work.
References
- 1.Nugent GR, Sprinle P, Bloor BM. Sphenoid sinus mucoceles. J Neurosurg. 1970;32:443–451. doi: 10.3171/jns.1970.32.4.0443. [DOI] [PubMed] [Google Scholar]
- 2.Tseng CC, Ho CY, Kao SC. Ophthalmic manifestations of paranasal sinus mucoceles. J Chin Med Assoc. 2005;68:260–264. doi: 10.1016/S1726-4901(09)70147-9. [DOI] [PubMed] [Google Scholar]
- 3.Stankiewicz JA. Sphenoid sinus mucocele. Arch Otolaryngol Head Neck Surg. 1989;115:735–740. doi: 10.1001/archotol.1989.01860300089024. [DOI] [PubMed] [Google Scholar]
- 4.Lochrl TA, Leopold DA. Spheno-ethmoidal mucoceles presenting with bilateral visual compromise. Am Otol Rhinolaryngol. 2000;109:608–610. doi: 10.1177/000348940010900615. [DOI] [PubMed] [Google Scholar]
- 5.Levy J, Monos T, Puterman M. Bilateral consecutive blindness due to sphenoid sinus mucocele with unilateral partial recovery. Can J Ophthalmol. 2005;40:506–508. doi: 10.1016/S0008-4182(05)80015-8. [DOI] [PubMed] [Google Scholar]
- 6.Moriyama H, Hesaka H, Tachibana T, Honda Y. Mucoceles of ethmoid and sphenoid sinus with visual disturbance. Arch Otolaryngol Head Neck Surg. 1992;118:142–146. doi: 10.1001/archotol.1992.01880020034012. [DOI] [PubMed] [Google Scholar]
- 7.Di Girolamo S, Cannizzaro P, Picciotti P, Nardi C. Ophthalmoplegia and ptosis as onset symptoms of an isolated primary mucocele of the sphenoid sinus. J Oral Maxillofac Surg. 2002;60:1500–1502. doi: 10.1053/joms.2002.36142. [DOI] [PubMed] [Google Scholar]
- 8.Chawla HS, Goodwin JA, Ticho BH, Feist RM. Orbital and sinus inflammation with secondary optic neuropathy. Ann Ophthalmol. 1991;23:231–233. [PubMed] [Google Scholar]
- 9.Shimo-Oku M, Miyazaki S, Shiraki K, Sagimoto T, Sotari H. Optic nerve involvement in posterior paranasal sinus disease. Neurophthalmology. 1989;9:147–155. [Google Scholar]
- 10.Hiratsuka Y, Hotta Y, Yui A, Nakayasu K, Kanai A, Yamakawa T. Rhinogenic optic neuropathy cause bilateral loss of light perception. Br J Ophthalmol. 1998;82:99–100. doi: 10.1136/bjo.82.1.99. [DOI] [PMC free article] [PubMed] [Google Scholar]


